Abstract
Circulating tumor HPV DNA (ctHPV16) assessed in liquid biopsy may be used as a marker of cancer in patients with HPV-associated oropharyngeal cancer (HPV + OPC). Factors influencing the initial ctHPV16 quantity are not well recognized. In this study we aimed to establish what factors are related to the level of ctHPV16 at the time of diagnosis. 51 patients (37 men and 14 women, median age of 57 years old) with HPV + OPC prior to definitive treatment were included. ctHPV16 was measured by qPCR. Tumor and nodal staging were assessed according to AJCC8. Blood derived factors included squamous cell carcinoma antigen (SCC-Ag), serum soluble fragment of cytokeratin 19 (CYFRA 21-1), C-reactive protein (CRP), albumin level (Alb), neutrophils (Neut), thrombocytes (Plt) and lymphocyte (Lym) count, Neut/Lym ratio were assessed. The volumes of the primary tumor (TV) and involved lymph nodes (NV) were calculated using MRI, CT or PET-CT scans. Data were analysed using parametric and nonparametric methods. Variables for multivariable linear regression analysis were chosen based on the results from univariable analysis (correlation, univariable regression and difference). There were 9 (18%), 10 (19%) and 32 (63%) patients who had TV and NV assessed in MRI, CT or PET respectively. Primary tumor neither as T-stage nor TV was related to ctHPV16 level. Significant differences in the ctHPV16 between patients with high vs low pain (P = 0.038), NV (P = 0.023), TV + NV (P = 0.018), CYFRA 21-1 (P = 0.002), CRP (P = 0.019), and N1 vs N3 (P = 0.044) were observed. ctHPV16 was significantly associated with CYFRA 21-1 (P = 0.017), N stage (P = 0.005), NV (P = 0.009), TV + NV (P = 0.002), CRP (P = 0.019), and pain (P = 0.038). In univariable linear regression analysis the same variables predicted ctHPV16 level. In multivariable analyses, CYFRA 21-1 and CRP (both as categorical variables) were predictors of ctHPV16 level even above NV. ctHPV16 at presentation is driven by tumor volume measured mostly by N. CYFRA 21-1 and CRP are additional factors related to ctHPV16 prior to the treatment.
Similar content being viewed by others
Introduction
The number of patients suffering from HPV-associated oropharyngeal cancer (HPV + OPC) is increasing 1,2,3. Despite a better treatment response for HPV + OPC patients compared to non-HPV-associated head and neck cancers, no treatment de-escalation has been approved 4 and nearly 25% of patients experience treatment failure 5,6. Circulating tumor HPV DNA (ctHPV16) in plasma has been shown to be a highly accurate real-time biomarker of HPV + OPC, reflecting the presence, absence and changes in cancer burden across time 7,8,9,10,11 not only in the relation to the volume of disease but probably also to dynamics of tumor cell proliferation and mechanisms of cell death due 12. ctHPV16 may be used as a promising biomarker for early detection of HPV + OPC 9,13,14, to support monitoring of treatment response during therapy 11,13,15,16 and shortly after its completion 17 but also during surveillance to indicate disease recurrence 18,19. In such cases, the initial amount of ctHPV16 as a reference value may be of clinical significance 11,20. Some datasets suggests that higher amount of initial ctHPV may be a positive prognostic factor, while others have found no association, or even the opposite relationship21. Little is known about factors which are linked to initial ctHPV16 level although recent work suggest nodal volume may be a driving force 22. In this study we examined selected tumor and patient related factors together with blood biomarkers in the relation to the amount of ctHPV16 at presentation.
Material and methods
Patient characteristics
Patients admitted to National Research Institute of Oncology, Gliwice Branch, Poland due to HPV + OPC between 2012 and 2022 were retrospectively analysed. The group consisted of 55 patients with HPV + OPC with ctHPV16 assessed at diagnosis and computerized tomography (CT), magnetic resonance imaging (MRI) or 18F-fluorodeoxyglucose positron emission tomography (PET-CT) scan acquisition prior to treatment. Four patients were excluded from analysis due to missing data, leaving a sample size of 51. There were 37 men and 14 women with a median age of 57 years (IQR: 49–63). Stage of primary tumor (T) and involved lymph nodes (N) were assessed according to AJCC8. Primary symptoms of disease were based on clinical interview with the patient via the medial record.
Blood derived factors included squamous cell carcinoma antigen (SCC-Ag), serum soluble fragment of cytokeratin 19 (CYFRA 21-1), C-reactive protein (CRP), albumin level (Alb), neutrophils (Neut), thrombocytes (Plt) and lymphocyte (Lym) count, Neut/Lym ratio based on routine clinical results were assessed. The concentration of SCC-Ag was determined by chemiluminescent microparticle immunoassay (CMIA), using analyzer Alinity I and commercial kit analyzer from Abbott Laboratories (Abbott Park, IL, USA). The concentration of CYFRA 21-1 was determined by means of the electrochemiluminescence immunoassay method (ECLIA) using the Roche Diagnostics (Basel, Switzerland) reagent kits and Cobas e801 analyzer. Serum CRP and albumin concentrations were measured by immunonephelometric technique, using a Siemens reagent kit and a Atelica nephelometer. The lymphocyte-to-monocyte ratio was calculated using automated complete blood cell count (CBC) data obtained by dividing the lymphocyte-to-monocyte count. A Sysmex XN 2000 analyzer machine was used for automated CBC.
For descriptive statistics, see Table S1 and S2 in the supplementary materials. Written informed consent was required from all participating patients.
Informed consent was taken from all participants. Institutional Review Board Statement: The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Bioethics Committee at Maria Sklodowska‑Curie National Research Institute of Oncology Gliwice Branch (protocol KB/430‑24/19 date of approval 11 March 2019).
Detection of HPV16 in plasma
Peripheral blood (12 mL) was collected in K3EDTA tubes (Becton–Dickinson, Franklin Lakes, NJ, USA). Plasma was separated within an hour by double centrifugation at 300 × g and 1000 × g, both at 4 °C for 10 min. DNA was extracted (according to the manufacturer’s instructions) from 1 mL of plasma using the Genomic Mini AX Body Fluids Kit (A&A Biotechnology, Gdynia, Poland). PCR reactions were performed using the Bio-Rad CFX96 qPCR instrument (Bio-Rad Laboratories, Hemel Hempstead, UK). Each measurement consisted of a standard curve of three dilutions of a plasmid construct containing the HPV16 and TERT genome, a negative control, and a sample. The amplification of TERT (human telomerase reverse transcriptase) was used for measurement of the total cell-free DNA in blood. The obtained copies of ctHPV16 were calculated according to the amount of plasma that was taken for DNA extraction (copies/ml) − viral load (VL). ctHPV16 VL in plasma was expressed as a log10 of copy number of HPV16 DNA per 1 mL (log10 viral load, log10 VL). After conversion of the values to log10, the range between 0.4 and 5.9 were obtained with a normal distribution. The measured ctHPV16 as a viral load (VL) of HPV16-DNA in plasma was expressed as a log10 of copy number of HPV16 DNA/ml.
The assessment of the tumor volume
The volume of primary tumor (TV) and involved lymph nodes (NV) of the neck were calculated independently. MRI examinations were performed with a 1.5 T and 3 T field induction apparatus. TV and NV were calculated in T1-w DCE (T1-weighted dynamic contrast enhancement) after intravenous administration of a paramagnetic contrast agent.
PET-CT examinations were performed after intravenous administration of 18F-Fluorodeoxyglucose (18F FDG). The CT examination was performed using the spiral technique with the reconstruction of 3 mm layers without providing contrast iv. The metabolic tumor volume (MTV) of the lesions was counted at 30%, 40% and 50% of the maximum normalized uptake (SUV) and additionally with an SUV cut-off threshold of 2.5.
Computed tomography (CT) volumes were calculated on contrast-enhanced images. The areas of the primary tumor and lymph nodes with a metastatic image were segmented after contrast agent administration.
Statistical analysis
Categorical variables were summarized as frequencies and percentages. Continuous data were shown as median values with interquartile ranges (25% to 75%, IQR 25–75) and mean values with standard deviation/min/max ranges, unless otherwise stated. For exact descriptive statistics, see Table S1 and S2 in the supplementary materials.
Predictive mean matching was used to replace missing data with use of mice package (v. 3.15.0) 23. Table S3 in supplementary materials represents the amount of missing data per patient that was included or excluded from the study.
Data were analysed using parametric and nonparametric methods depending on distribution and homogeneity of variance. Normality of distribution was tested using the Shapiro–Wilk test. To evaluate the difference in VL level the one-way analysis of variance (ANOVA with Duncan’s adjustment for pairwise comparisons) and Student's t-test was performed with d Cohen effect size calculation. The correlation with VL was investigated using stats package (v. 3.6.2) 24 (Pearson’s, Spearman's rank or Point biserial correlation was applied accordingly).
Visualizations was prepared with the ggplot2 (v. 3.4.0) 25 and corrplot package (v. 0.92) 26.
The following variables were assessed with VL as continuous and as categorical variables: TV, NV, combined TV and NV (TV + NV), SCC, age, symptoms duration (time to diagnosis − TtDGN) and CYFRA 21-1. Categorization was made according to median value.
In order to assess predictor(s) of VL level a univariable and multivariable linear regression analysis was performed with reduction in a stepwise manner. Models were compared on the basis of AIC (Akaike's Information Criterion). Analysis were performed using AICcmodavg (v. 2.3-1) 27, tidyverse (v. 1.3.0) 25,28, ggpubr (v. 0.5.0) 29, and MASS package (v. 7.3-58.1) 30.
Variables for multivariable analysis were chosen based on the results from univariable analysis (correlation, regression and difference). Full report can be found in Table S6 in Supplementary Material.
All analyses were performed using the R environment for statistical computing version 4.1.3 "One Push-Up" released on 10 March 2022 (R Foundation for Statistical Computing, Vienna, Austria, http://www.r-project.org). A two-sided P value < 0.05 was considered statistically significant, and a P value < 0.10 was considered close statistical significance. The Benjamini–Hochberg correction was applied to account for multiple testing, where a q-value of < 0.05 was considered statistically significant. Since the correction did not alter the inference, q-values are reported accordingly in the Supplementary Materials.
Results
Nine (18%), 10 (19%) and 32 (63%) patients had TV and NV assessed by MRI, CT or PET respectively.
In univariable analysis there was no difference in ctHPV16 level by median age, sex, disease symptoms or smoking status (Table 1; Supplementary materials, Table S4). However, pain was associated with ctHPV16 level (P = 0.038, d = 0.613). Primary tumor neither as T-stage nor TV (Table 1 and S4) was related to ctHPV16. On the contrary, involved regional nodes were related to VL with a significant difference in VL for N1 patients vs N3 patients (P = 0.044, d = 0.857; Table 1).
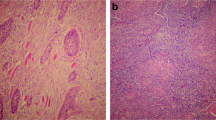
To assess how selected tumor- and patient-related factors together with blood biomarkers affect ctHPV16, a correlation analysis was performed. VL was significantly correlated with CYFRA 21-1 median (both as continues and as categorical variable: rho = 0.331, P = 0.017 and r = 0.417, P = 0.002 accordingly), N stage (rho = 0.386, P = 0.005), NV (both as continues and as categorical variable: rho = 0.360, P = 0.009 and r = 0.331, P = 0.018 accordingly), TV + NV (both as continues and as categorical variable: rho = 0.424, P = 0.002 and r = 0.316, P = 0.024), CRP level as categorical variable (r = 0.327, P = 0.019), and pain (r = − 0.291, P = 0.038) (Fig. 1). The complete report on correlation between VL and analysed variables is given in supplementary materials (Table S4; Fig. S1).
Next, variables were divided according to median values and related to VL.
Significant difference in VL was observed between patients with median/below median and above median of NV (P = 0.023, d = 0.703), TV + NV (P = 0.018, d = 0.827), CYFRA 21-1 (P = 0.002, d = 0.917) and CRP (P = 0.019, d = 0.694). Significant difference in VL was also observed, between patients with and without pain (P = 0.038, d = 0.613) (Fig. 2; Table 1).
CYFRA 21-1 and TV + NV both, as continuous and as categorical variable, N, pain, NV, and CRP as a categorical variable and TV as continues variable appeared to be a significant predictors of VL level (Table S5 in the Supplementary Material).
For multivariable analysis variables: pain, N, NV_CAT (NV as a categorical variable), CYFRA_CAT, and CRP_CAT (CYFRA 21-1 and CRP as a categorical variable accordingly) were divided into groups. Group I consisted of variables related to tumor and patient (pain, N, NV_CAT) and Group II consisted of variables related to biochemical biomarkers (CYFRA_CAT, CRP_CAT). From the group I NV as categorical variable (Table 2; Table S7) and all of the variables from the group II came as significant predictors of ctHPV16 level (Table 3; Table S8). Full assessment report can be found in Table S6.
Discussion
The detection of HPV sequences in the total cell free DNA in the blood of patients with HPV + OPC has become the basis of ctHPV assays as a tumor-derived biomarker 31,32,33. The amount of viral DNA could be described as a VL which is the number of viral particles per millilitre of the blood. Importantly, ctHPV levels, do not always correlate with the clinical stage of the cancer. For patients with HPV + OPC, VL is strongly, positively correlated with tissue VL − tVL (tVL) and the probability of detecting ctHPV in the blood increases with the increase of tVL 10. Cao et al. reported that the low tVL could be one of the contributors influencing the inability to detect ctDNA in the blood at baseline 20. Chera et al. found that patients with low baseline ctHPV (</= 200 copies/mL) in the blood had a significantly lower tVL than patients with high baseline ctHPV (> 200 copies/mL) 13. Understanding what clinical factors may influence ctHPV levels is critical for understanding the role of ctHPV in prognostication and treatment monitoring.
Certain populations of cancer cells may produce various amount of ctHPV. Moreover, distinct mechanisms influence ctDNA release which can be early or delayed. The kinetics of releasing ctHPV depends not only on the type of cancer cell but also external cytotoxic factors. Further, cell death mechanisms seem to be relevant as well. Cellular senescence contrary to immediate apoptotic death or necrosis may change the kinetics of ctDNA delaying ctDNA release 12. Furthermore, the structure of tumor including vascularity, perfusion, or hypoxia may also be confounding factors affecting the shedding rate of ctDNA 34.
A common features of HPV + OPC is a small primary tumor and higher volume nodal involvement, compared to non-HPV-associated OPC, and nearly all patients with HPV + OPC present with lymph node metastases 2,35,36,37. Thus, the questions remains what are the primary factors driving ctHPV.
While analysing primary tumor as a T-stage we did not find any correlation with ctHPV. This is in concordance with other reports. Chera et al. found even that patients with T3-T4 tumor stage of HPV + OPC had significantly lower baseline levels of ctHPV than patients with T2 tumor, suggesting that larger tumor size may be associated with lower rates of ctHPV release 13. Further analysis revealed that the level of baseline ctHPV may relate to HPV integration within the host genome, with more integrated cases having lower baseline ctHPV. Dahlstrom et al. reported no relationship between pretreatment serum ctHPV level and T-stage 38. In another study Cao et al. found no correlation between T-stage and ctHPV even if metabolic volume of primary tumor was taken into account 20. The lack of correlation between T-stage and ctHPV may be also the result of T-classification that reflects more the area of cancer infiltration and involvement of surrounding structures than the volume of the tumor. This difference between dimension and volume increases in cubic relation and is more meaningful for larger tumors. Also for patients with cervical cancer the relation between stage of disease and ctHPV16 was not obvious with significant difference between stage I and II but not between II and III or II and IV stage 7.
Contrary to primary tumor, we found significantly lower ctHPV levels in N1 tumors vs N3. Between stage N1 and N2 the difference was not significant. This discrepancy may be explained by staging features in AJCC 8th. N2 staging involves patients with metastatic lymph nodes on contralateral or both sides of the neck, independent of its dimension. Although 8th staging edition tried to better stratify HPV + OPC, it is not focused on tumor quantity. Due to this, besides T and N classification we also radiologically estimated the TV and NV what may more accurately reflect the quantify of tumor. For combined TV and NV, the median volume over 56.64 cm3 reflected significantly higher level of ctHPV. As previously mentioned, Dahlstrom et al. found that pretreatment ctHPV increased with increasing N category and was significantly higher while accounting stage of disease (combined T and N category) 38. Retting et al. considered diameter of primary tumor and involved nodes according to dimensions based on standard contrast-enhanced CT. They reported strong association of N stage with ctHPV while only a weak association with clinical T stage. Notably, in this set of patients T0 presented the highest ctHPV. Also the size of the largest cervical lymph node presented a stronger association with ctHPV than size of the primary tumor 22. Results of functional imaging also indicated that ctHPV is related more to NV than to TV. Cao et al. also found that pretreatment ctHPV was significantly correlated with NV, nodal poorly perfused subvolumes and high cellular subvolume of involved nodes defined from MRI. Authors suggested that cellularly dense nodal burden may dominate in the releasing of tumor DNA 20. Retting et al. reported only moderated association between metabolic activity in both primary tumor, nodes and ctHPV, although increasing SUVmax in involved lymph nodes was related to progressive increase of ctHPV 22.
Additional adverse clinical risk factor as smoking also may influence the relation between ctHPV and tumor burden. Chera et al. found that patients with more than 10 tobacco package per year had lower baseline ctHPV level despite T4 tumor stage 13. Hashida et al. reported that patients with ≥ 20 pack-years had significantly lower ctHPV 39. Mazurek et al. found that particularly high tVL was found in non-smoking women 10. This may suggest that in patients with HPV + OPC smoking, as an additional risk factor is responsible more for advanced disease rather than HPV and that prognosis based on pretreatment ctHPV in such patients may be of questionable value.
Significant correlation between ctHPV and levels of CYFRA 21-1 and CRP in the blood was found in our patients. CYFRA 21-1 is the serum soluble fragment of cytokeratin 19 and is a part of cytoskeleton of epithelial cell. CYFRA 21-1 is released by epithelium-derived cancer cells while proliferating. In some reports the correlation between CYFRA 21-1 and tumor growth, stage of disease, involved lymph nodes 40 or distant metastases 41 has been found. However, an inverse correlation between CYFRA 21-1 and the grade of tumor has been also reported 42. Little is known about CYFRA 21-1 in patients with HPV + OPC. Rudhart et al. did not find significant differences of the CYFRA 21-1 serum concentration for patients with HPV-associated and not associated tumors prior to treatment; however over 40% of patients in this group had unknown HPV status 43. Despite some uncertainties of CYFRA 21-1 as a marker of active tumor, we found that the median value of CYFRA 21-1 significantly separated patients in our group according to ctHPV, suggesting that CYFRA 21-1 may reflect higher proliferation of tumor cells.
Serum C-reactive protein (CRP) is a marker of inflammation and is elevated in response to tissue damage or infection. CRP level is also correlated with both tumor and nodal stage and histopatological differentiation of the tumor. Our results showed that patients with median CRP value over 2.03 mg/l had significantly higher ctHPV level. Husuan Ho et al. found that in the group of patients with pharyngolaryngeal carcinoma CRP level was significantly related to maximal SUV of involved nodes but not primary tumor 44. Johnson-Obaseki et al. 45 reported that CRP level was significantly higher in the patients with HPV + OPC but contrary results were described by Xiao et al. 46. The elevation of CRP also arises from the host immune responses to tumor growth with elevated inflammatory cytokines, especially Il-6 44. Our results confirm that ctHPV is significantly related to the level of both CYFRA 21-1 and CRP. The clinical utility of the assessment of these markers in patients with HPV + OPC and its potential prognostic or predictive value require however further investigation.
HPV DNA can be found as both, integrated and episomal states in cancer cells. Traditionally, episomal HPV has been felt to correlate with a favourable prognosis while integrated tumors were felt to have adverse tumor genomic feature 39,47. Lower initial level of ctHPV DNA has been reported to be associated with clinically higher-risk disease and also with greater likelihood of HPV integration, which represents adverse tumor genomic features 13. Recently, a more complex understanding of HPV genome states has emerged. Rossi et al. showed novel mechanism for HPV16 to cause cancer without integration through aberrant episomal replication, forming rearranged, mutated, and multimer episomes 48.
Finally, it should be noticed that in patients with no pain as clinical symptom of cancer, ctHPV was significantly higher. Explanation of this remain to be elucidated especially due to the assumption that the level of ctHPV seems to be related to lymphovascular invasion 22 and invasive component usually is responsible for the pain. This effect however might be less pronounced for HPV-associated primaries less likely to display ulceration or necrosis or nodal disease that is generally more clustered and cystic than for HPV-not associated tumors usually presenting ill-defined borders and invading into neighbouring muscle 49. There is also the general observation that patients with HPV-associated tumor usually are in better general performance status being less fatigue and less devastated by cancer disease that their counterparts with HPV-not associated tumors 46.
This study has several limitations. The study is retrospective, which may lead to data inaccuracies. Other doubts may be related to three distinct methods of tumor volume assessment. Despite of this, to our knowledge, the present study is the first to investigate correlation between volume of the primary tumor, lymph nodes and ctHPV. The significant correlation between tumor markers like CYFRA 21-1 or CRP and ctHPV has also not been previously described.
Conclusions
Our results indicate that ctHPV16 at presentation is driven by tumor volume measured mostly by N what is in concordance with other data suggesting nodal disease as the main determinant of this marker. CYFRA 21-1 and CRP are additional factors related to ctHPV16 prior to the treatment. This data contribute to the growing body of literature leading to a better understanding of the factors that influence ctHPV levels at diagnosis, which could help identify distinct subpopulations of patients with HPV + OPC for prognostication and stratification.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Gillison, M. L., Chaturvedi, A. K., Anderson, W. F. & Fakhry, C. Epidemiology of human papillomavirus-positive head and neck squamous cell carcinoma review. J. Clin. Oncol. 33(29), 3235–3242 (2015).
Wittekindt, C., Wagner, S., Bushnak, A., Prigge, E. S., von Knebel Doeberitz, M., & Würdemann, N., et al. Increasing incidence rates of oropharyngeal squamous cell carcinoma in germany and significance of disease burden attributed to human papillomavirus. Cancer Prev. Res. 12, 375–382 (2019).
Mehanna, H. et al. Prevalence of human papillomavirus in oropharyngeal and nonoropharyngeal head and neck cancer-systematic review and meta-analysis of trends by time and region. Head Neck 35, 747–755 (2013).
Bates, J. E. & Steuer, C. E. HPV as a carcinomic driver in head and neck cancer: A de-escalated future?. Curr. Treat Options Oncol. 23(3), 325–332 (2022).
Bledsoe, T. J. et al. Oropharyngeal squamous cell carcinoma with known human papillomavirus status treated with definitive chemoradiotherapy: Patterns of failure and toxicity outcomes. Radiat. Oncol. 8, 174 (2013).
Huang, S. H. et al. Natural course of distant metastases following radiotherapy or chemoradiotherapy in HPV-related oropharyngeal cancer. Oral Oncol. 49(1), 79–85 (2013).
Jeannot, E. et al. Circulating human papillomavirus DNA detected using droplet digital PCR in the serum of patients diagnosed with early stage human papillomavirus-associated invasive carcinoma. J. Pathol. Clin. Res. 2, 201–209 (2016).
Reder, H. et al. Plasma cell-free human papillomavirus oncogene E6 and E7 DNA predicts outcome in oropharyngeal squamous cell carcinoma. J. Mol. Diagnost. 22, 1333–1343 (2020).
Siravegna, G. et al. Cell free HPV DNA provides an accurate and rapid diagnosis of HPV-associated head and neck cancer. Clin. Cancer Res. 28(4), 719–727 (2022).
Mazurek, A. M. et al. Detection of circulating HPV16 DNA as a biomarker in the blood of patients with human papillomavirus-positive oropharyngeal squamous cell carcinoma. Head Neck. 41, 632–641 (2019).
O’Boyle, C. J. et al. Cell-free human papillomavirus DNA kinetics after surgery for human papillomavirus-associated oropharyngeal cancer. Cancer 128(11), 2193–2204 (2022).
Rostami, A. et al. Senescence, necrosis, and apoptosis govern circulating cell-free DNA release kinetics. Cell Rep. 31(13), 107830 (2020).
Chera, B. S. et al. Rapid clearance profile of plasma circulating tumor HPV type 16 DNA during chemoradiotherapy correlates with disease control in HPV-associated oropharyngeal cancer. Clin. Cancer Res. 25, 4682–4690 (2019).
Rettig, E. M. et al. Detection of circulating tumor human papillomavirus DNA before diagnosis of HPV-positive head and neck cancer. Int. J. Cancer 151(7), 1081–1085 (2022).
Inukai, D. et al. Pathological and virological studies of p16-positive oropharyngeal carcinoma with a good response to neoadjuvant chemotherapy. Microorganisms 8(10), 1497 (2020).
Naegele, S. et al. Detection and monitoring of circulating tumor HPV DNA in HPV-associated sinonasal and nasopharyngeal cancers. JAMA Otolaryngol. Head Neck Surg. 149(2), 179–181 (2023).
Rutkowski, T. W. et al. Circulating HPV16 DNA may complement imaging assessment of early treatment efficacy in patients with HPV-positive oropharyngeal cancer. J. Transl. Med. 18(1), 167 (2020).
Chera, B. S. et al. Plasma circulating tumor HPV DNA for the surveillance of cancer recurrence in HPV-associated oropharyngeal cancer. J. Clin. Oncol. 38, 1050–1058 (2020).
Berger, B. M. et al. Detection of occult recurrence using circulating tumor tissue modified viral HPV DNA among patients treated for HPV-driven oropharyngeal carcinoma. Clin. Cancer Res. 28(19), 4292–4301 (2022).
Cao, H. et al. Quantitation of human papillomavirus DNA in plasma of oropharyngeal carcinoma patients. Int. J. Radiat. Oncol. Biol. Phys. 82(3), e351–e358 (2012).
Cao, Y. et al. Early HPV ctDNA kinetics and imaging biomarkers predict therapeutic response in p16+ oropharyngeal squamous cell carcinoma. Clin. Cancer Res. 28(2), 350–359 (2022).
Rettig, E. M. et al. Association of pretreatment circulating tumor tissue-modified viral HPV DNA with clinicopathologic factors in HPV-positive oropharyngeal cancer. JAMA Otolaryngol. Head Neck Surg. 148(12), 1120–1130 (2022).
van Buuren, S. & Groothuis-Oudshoorn, K. mice: Multivariate imputation by chained equations in R. J. Stat. Softw. 45(3), 1–67 (2011).
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2022). https://www.R-project.org/
Wickham, H. ggplot2: Elegant Graphics for Data Analysis (Springer-Verlag, 2016).
Wei, T, & Simko, V. R package 'corrplot': Visualization of a Correlation Matrix (Version 0.92) (2021) https://github.com/taiyun/corrplot
Mazerolle, M. J. AICcmodavg: Model selection and multimodel inference based on (Q)AIC(c). R package version 2.3-1 (2019). https://cran.r-project.org/package=AICcmodavg
Wickham, H. et al. Welcome to the tidyverse. J. Open Source Softw. 4(43), 1686. https://doi.org/10.21105/joss.01686 (2019).
Alboukadel Kassambara. ggpubr: 'ggplot2' Based Publication Ready Plots. R package version 0.4.0. 2020; Available from: https://CRAN.R-project.org/package=ggpubr
Venables, W. N. & Ripley, B. D. Modern Applied Statistics with S 4th edn. (Springer, 2002).
van Ginkel, J. H. et al. Cell-free nucleic acids in body fluids as biomarkers for the prediction and early detection of recurrent head and neck cancer: A systematic review of the literature. Oral Oncol. 75, 8–15 (2017).
Keller, L., Belloum, Y., Wikman, H. & Pantel, K. Clinical relevance of blood-based ctDNA analysis: Mutation detection and beyond. Br J Cancer. 124, 345–358 (2021).
Swiecicki, P. L., Brennan, J. R., Mierzwa, M., Spector, M. E. & Brenner, J. C. Head and Neck Squamous Cell Carcinoma Detection and Surveillance: Advances of Liquid Biomarkers. Laryngoscope. 129, 1836–1843 (2019).
Wan, J. C. M. et al. Liquid biopsies come of age: towards implementation of circulating tumour DNA. Nat Rev Cancer. 17, 223–238 (2017).
Setton, J. et al. A multi-institution pooled analysis of gastrostomy tube dependence in patients with oropharyngeal cancer treated with definitive intensity-modulated radiotherapy. Cancer. 121(2), 294–301 (2015).
Keane, F. K. et al. Changing prognostic significance of tumor stage and nodal stage in patients with squamous cell carcinoma of the oropharynx in the human papillomavirus era. Cancer. 121(15), 2594–2602 (2015).
Ward, M. J. et al. Staging and treatment of oropharyngeal cancer in the human papillomavirus era. Head Neck. 37(7), 1002–1013 (2015).
Dahlstrom, K. R. et al. Circulating human papillomavirus DNA as a marker for disease extent and recurrence among patients with oropharyngeal cancer. Cancer. 121(19), 3455–3464 (2015).
Hashida, Y. et al. Prognostic significance of human papillomavirus 16 viral load level in patients with oropharyngeal cancer. Cancer Sci. 112(10), 4404–4417 (2021).
Niemann, A.M., Paulsen, J.J., Lippert, B.M., Henze, E., Gorogh, T. & Gottschlich, S. Cyfra21-1 in patients with head and neck cancer. In J. A. Werner, B. M. Lippert & H. H. Rudert eds. Head and Neck Cancer: Advances in Basic Research 529–537 (Elsevier, 1996).
Maass, J. D. et al. Cyfra 21-1: A serological help for detection of distant metastases in head and neck cancer. Anticancer Res. 20, 2241–2243 (2000).
Doweck, I., Barak, M., Uri, N. & Greenberg, E. The prognostic value of the tumor marker Cyfra 21-1 in carcinoma of the head and neck and its role in early detection of recurrent disease. Br. J. Cancer 83, 1696–1701 (2000).
Rudhart, S. A. et al. Clinical relevance of CYFRA 21–1 as a tumour marker in patients with oropharyngeal squamous cell carcinoma. Eur. Arch. Otorhinolaryngol. 277(9), 2561–71 (2020).
Chen, H. H. et al. Pre-treatment levels of C-reactive protein and squamous cell carcinoma antigen for predicting the aggressiveness of pharyngolaryngeal carcinoma. PLoS ONE 8(1), e55327 (2013).
Johnson-Obaseki, S. et al. C-reactive protein in HPV-positive and HPV-negative oropharyngeal cancer. Otolaryngol. Head Neck Surg. 160(3), 494–501 (2019).
Xiao, C. et al. Associations among human papillomavirus, inflammation, and fatigue in patients with head and neck cancer. Cancer 124(15), 3163–70 (2001).
Nulton, T. J., Kim, N. K., DiNardo, L. J., Morgan, I. M. & Windle, B. Patients with integrated HPV16 in head and neck cancer show poor survival. Oral Oncol. 80, 52–55 (2018).
Rossi, N. M. et al. Extrachromosomal amplification of human papillomavirus. Cancer Res. 83(11), 1768–1781 (2023).
Salzillo, T. C. et al. Advances in imaging for HPV-related oropharyngeal cancer: Applications to radiation oncology. Semin. Radiat. Oncol. 31(4), 371–388 (2021).
Author information
Authors and Affiliations
Contributions
Study concepts: TWR, AMM, MK. Study design: TWR, BBB. Data acquisition: AH, JMK, UK, EC, PP, AdA, MS, MK. Quality control of data and algorithms: AH, AMM, KDR, KG. Data analysis and interpretation: TWR, AJC, AMM. Statistical analysis: AJC. Manuscript preparation: TWR, AJC, MK. Manuscript editing: AMM, IŁ. Manuscript review: KS, DLF.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kentnowski, M., Cortez, A.J., Mazurek, A.M. et al. Determinants of the level of circulating-tumor HPV16 DNA in patients with HPV-associated oropharyngeal cancer at the time of diagnosis. Sci Rep 13, 21226 (2023). https://doi.org/10.1038/s41598-023-48506-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-48506-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.