Abstract
Circulating tumor DNA (ctDNA) provides molecular information on tumor heterogeneity. The prognostic usefulness of ctDNA after first-line epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) are limited. Therefore, the present study evaluated ctDNA during osimertinib administration as a second-line or more setting to identify the relationship between EGFR mutation levels and outcomes in patients with advanced non-small cell lung cancer (NSCLC). Forty patients with EGFR T790M-positive NSCLC receiving osimertinib after prior EGFR-TKI treatment were registered. Plasma samples were collected at osimertinib pretreatment, after 1 month of treatment, and at the time of progressive disease (PD). ctDNA analysis was performed by digital polymerase chain reaction. The detection rate of copy numbers of exon 19 deletion, L858R, and T790M in plasma samples was significantly lower 1 month after osimertinib than at pretreatment, and significantly higher at PD than at 1 month, whereas that of C797S was significantly higher at PD than at 1 month. No statistically significant difference was observed in the copy numbers of exon 19 deletion, L858R, T790M, and C797S between complete response or partial response and stable disease or PD. The detection of T790M at PD after osimertinib initiation was a significant independent prognostic factor for predicting shorter prognosis, and the presence of major EGFR mutations at pretreatment and PD was closely linked to worse survival after osimertinib initiation. Molecular testing based on ctDNA is helpful for predicting outcomes of osimertinib treatment in T790M-positive NSCLC after previous EGFR-TKI treatment.
Similar content being viewed by others
Introduction
Molecular targeting agents are useful to improve the prognosis of patients with cancer with driver mutations1. Among patients with advanced non-small cell lung cancer (NSCLC), epidermal growth factor receptor (EGFR) mutation is identified as the predominant target, and EGFR tyrosine kinase inhibitor (TKI) administration is the standard treatment for patients with NSCLC harboring EGFR mutation. In particular, osimertinib, as a third-generation EGFR-TKI, is administered as a first-line treatment2, but it can also be effective for patients with previously treated NSCLC harboring T790M-positive EGFR mutation, based on the AURA3 trial3. If T790M is detected in progressive disease (PD) after first- or second-generation EGFR-TKI administration, osimertinib is applicable to such patients. However, approximately 25% of patients resistant to first- or second-generation EGFR-TKIs can receive osimertinib because of T790M-positive testing4. As the presence of T790M within tumor specimens cannot predict the outcome of osimertinib administration, the development of an useful predictor is required to distinguish responders from non-responders.
Recently, Ariyasu et al.5 evaluated the ratio of T790M to EGFR-activating mutations in cytological samples from 33 patients with NSCLC receiving osimertinib using droplet digital polymerase chain reaction (PCR) and found a significant correlation between the T790M ratio and the tumor reduction rate. In addition, the clearing of all EGFR mutations from the blood after osimertinib initiation significantly predicted its efficacy and outcome in 82 pretreated patients receiving osimertinib, and all clearing of T790M and sensitizing mutations is necessary for a positive predictor of osimertinib6.
The assessment of circulating tumor DNA (ctDNA) is a noninvasive strategy for cancer diagnosis; in particular, plasma ctDNA testing to examine sensitizing EGFR and T790M mutations was approved in 20157. EGFR and T790M plasma testing was evaluated using several techniques, such as PCR and next-generation sequencing. Although liquid biopsy is more feasible than tissue biopsy, there are some doubts about the sensitivity of its detection. Tumor tissue genotyping exhibits a high sensitivity and specificity for molecular analysis, but, yields a limitation about tumor availability and accessibility. The turnaround time for genetic analysis is longer than that for liquid biopsy. Thus, liquid biopsy could overcome these limitations because of faster turnaround time and less invasive procedure8. Digital PCR is a recently developed method. It has higher detection sensitivity than conventional PCR and has recently attracted attention for the detection of ctDNA9,10. However, a recent report analyzed extracted ctDNA using non-digital platforms (the cobas EGFR Mutation Test) and digital platforms (BEAMing dPCR), and demonstrated that both platforms yielded a high sensitivity for T790M mutation detection11. Non-digital platform by the cobas EGFR Mutation Test is also considered as comparable technology to digital PCR. In several studies, the ratio of T790M to EGFR-activating mutations in ctDNA, plasma pretreatment T790M level, and fraction of EGFR-mutant ctDNA in plasma have been reported to be potential markers of prognosis in patients receiving osimertinib12,13,14. However, there are no established markers to predict the outcome of osimertinib treatment in patients with T790M-positive EGFR mutation.
Based on this background, we conducted a prospective study to investigate the predictive markers of osimertinib in patients with T790M-positive EGFR-mutant NSCLC using digital PCR.
Results
Patient demographics
Patient demographics are shown in Table 1. Twenty-four patients had exon 19 deletion, 15 harbored L858R, and one patient presented with L861Q, as detected using the cobas method. Forty blood samples were collected from patients before osimertinib initiation, 36 blood samples were collected from patients 1 month after osimertinib administration, and 20 blood samples were collected from patients with PD after osimertinib treatment. Nine of the patients remained on osimertinib treatment without progression at the time of data cutoff, whereas 31 patients experienced PD. The median age was 69 (range, 33–85) years, and 28 (70.0%) patients were women. Thirty-one (77.6%) patients were never-smoker, 35 (87.5%) had a performance status (PS) score of 0–1, and all patients were classified as having adenocarcinoma histology. Thirty-four (85%) patients had stage III or IV disease, and 6 (15%) patients had postoperative recurrence.
EGFR mutation assessment in plasma circulating tumor DNA (ctDNA) samples
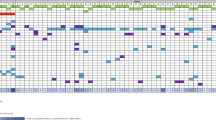
In a total of 40 patients, the detection rates for EGFR sensitizing mutations at baseline, 1 month and PD after osimertinib were 80.0% 27.8% (32/40), (10/36), and 85.0% (17/20), respectively. In the exon 19 deletion assay, the copy numbers detected in plasma samples at pretreatment, at 1 month, and at PD after osimertinib treatment ranged from 0 to 77.5 (positive rate, 42.5% [17/40]), from 0 to 0.59 (positive rate, 13.9% [5/36]), and from 0 to 13.15 copies/µL (positive rate, 45.0% [9/20]), respectively, demonstrating a significant difference between 1 month and PD (p = 0.003) (Fig. 1A). In the L858R assay, the copy numbers in the plasma sample at pretreatment, at 1 month, and at PD after treatment ranged from 0 to 134.7 (positive rate, 37.5% [15/40]), from 0 to 2.41 (positive rate, 13.9% [5/36]), and from 0 to 10.83 copies/µL (positive rate, 40.0% [8/20]), respectively, indicating a significant difference between 1 month and PD (p = 0.044) (Fig. 1B). The copy numbers detecting T790M ranged from 0 to 93.9 at pretreatment (positive rate, 60.0% [24/40]), from 0 to 0.45 at 1 month (positive rate, 13.9% [5/36]), and from 0 to 5.67 copies/µL (positive rate, 45.0% [9/20]). There was a significant difference in the copy numbers between pretreatment and 1 month (p = 0.028) and between 1 month and PD (p = 0.006) (Fig. 1C). The copy numbers of C797S ranged from 0 to 0.18 at pretreatment (positive rate, 12.5% [5/40]), from 0 to 0.09 at 1 month (positive rate, 11.1% [4/36]), and from 0 to 0.31 at PD (positive rate, 30.0% [6/20]), and those at PD were significantly higher than those at 1 month (p = 0.025) (Fig. 1D). Moreover, the positive rate of copy numbers of exon 19 deletion, L858R, and T790M in plasma samples were significantly lower at 1 month after osimertinib treatment than at pretreatment and PD, whereas that of C797S was significantly higher at PD than at 1 month (Fig. 2).
Distribution of epidermal growth factor receptor (EGFR) mutant-allele copy number in plasma samples before osimertinib (pretreatment), 1 month after its administration, and at progressive disease to its treatment, according to the EGFR mutation status of exon 19 deletion (A), exon 21 L858R (B), T790M (C), and C797S (D).
Association between plasma ctDNA and efficacy to osimertinib
Of the 40 patients, one achieved a complete response (CR), 24 had a partial response (PR), 11 had stable disease (SD), 3 displayed PD, and one had a non-evaluable lesion. The overall response rate (ORR) and disease control rate were 64.1% (25/39) and 92.3% (36/39), respectively. A comparison of the copy numbers based on the exon 19 deletion, L858R, T790M, and C797S between CR or PR (responders) and SD or PD (non-responders) was performed. However, there was no statistically significant difference in the copy numbers between them (Fig. A, online only). In addition, the positive rate of copy number did not differ significantly between responders and non-responders, except for exon 19 deletion at pretreatment (Fig. B, online only).
Survival analysis according to plasma ctDNA
The median PFS and OS were 13.1 months and 27.2 months, respectively. Twenty-five (62.5%) of the 40 patients experienced progression, and 19 (47.5%) patients died due to disease progression. Univariate and multivariate analyses were performed in all patients (Tables 2 and 3). Univariate analysis identified the detection of major EGFR mutation (exon 19 deletion and L858R) at pretreatment and detection of T790M at PD after osimertinib treatment for PFS (Table 2), and PS, brain metastasis, detection of major EGFR mutation at PD, and detection of T790M at PD after its treatment were considered significant predictors for OS (Table 3). Multivariate analysis confirmed that detection of major EGFR mutation at pretreatment and detection of T790M at PD were independent prognostic factors for predicting favorable PFS (Table 2), and detection of T790M at PD was identified as an independent factor for predicting worse OS (Table 3). Kaplan–Meier curves for PFS and OS according to the detection of major EGFR mutation and T790M are shown in Fig. 3A,B.
Kaplan–Meier curve according to major epidermal growth factor receptor (EGFR) mutation (A) and T790M (B) at pretreatment, 1 month, and progressive disease (PD) after osimertinib administration. Patients with detection of major EGFR mutation at pretreatment exhibited a significantly shorter progression-free survival (PFS) than those without it; moreover, there was significantly worse overall survival (OS) in patients with detection of major EGFR mutation at PD than those without it (A). Patients with T790M detection at PD yielded significantly worse PFS and OS than those without it (B).
Clinical efficacy on the ratio of T790M to major EGFR mutation
The clinical significance of the T790M/major EGFR mutation ratio at pretreatment was investigated, with a mean of 0.305 for CR/PR/SD and 0.185 for PD, without a significant difference (p = 0.632) (Fig. C1, online only). According to ROC analysis, the best cut-off value of the T790M/major EGFR mutation ratio was 0.727. No statistically significant difference in PFS and OS was observed between patients with T790M/major EGFR mutation ≥ 0.727 and < 0.727 (Fig. C2,C3, online only).
Discussion
This was a prospective observational study evaluating the prognostic significance of ctDNA, such as exon 19 deletion, L858R, T790M, and C797S EGFR mutations, in patients with previously treated NSCLC harboring T790M EGFR mutation who received osimertinib. The detection of ctDNA in plasma samples by digital PCR exactly reflected the change in exon 19 deletion, L858R, and T790M at 1 month and PD after osimertinib administration. We found that the detection of T790M at PD after osimertinib initiation was a significant independent prognostic factor for predicting worse OS, and that the detection of major EGFR mutations at pretreatment and T790M at PD also affected the outcome after osimertinib initiation. Currently, osimertinib is clarified as a first-line EGFR-TKI; thus, the frequency of its administration as a second-line or more lines is decreasing. However, the detection of blood samples using digital PCR is a noninvasive technique that is convenient for daily practice, and an improvement in the detection rate is warranted to realize the development of an optimal predictor.
The analysis of EGFR mutation in tissue and plasma from the AURA3 trial reported that the detection of plasma T790M was related to a larger baseline tumor size, and PFS after osimertinib (median, 12.5 vs. 8.3 months) was longer in patients with a cobas plasma T790M-negative status at pretreatment compared to those with a plasma T790M-positive status15. PFS in patients with NSCLC harboring T790M who received osimertinib tended to be worse in patients with high T790M copy number at pretreatment, as assessed by cell-free plasma DNA using digital, rather than those with low T790M copy number. Moreover, no significant difference in ORR was recognized according to T790M copy numbers16. Although another study also assessed the association between the utility of plasma T790M mutant copy number at pretreatment and the prognostic role of osimertinib using digital PCR, a high plasma T790M copy number was associated with worse PFS and OS compared to a low T790M copy number17. In addition, a high copy number of active EGFR mutations in plasma samples has been reported to be closely associated with poor outcomes after osimertinib treatment13. The results of these studies indicated that a high copy number of plasma T790M or activating EGFR mutations was a useful marker for predicting worse PFS in patients with NSCLC harboring positive EGFR T790M who were treated with osimertinib13,15,16,17. Ding et al.12 reported that high plasma T790M level at pretreatment was related to superior disease control in patients with NSCLC with advanced EGFR T790M treated with osimertinib. In our study, the detection of major plasma EGFR mutation (exon 19 deletion or L858R) at pretreatment could predict shorter PFS after osimertinib administration, but not plasma T790M copy number. Although previous studies have focused on the association between plasma EGFR mutation copy numbers and the efficacy of osimertinib at pretreatment, Sakai et al.18 evaluated the clinical significance of monitoring the ctDNA of EGFR-TKI-sensitizing mutations and EGFR T790M mutation in EGFR T790M-positive patients with NSCLC at pretreatment, on day 1 of treatment cycle 4 or 9, and at the diagnosis of PD using digital PCR. In their study, rebound of sensitizing EGFR mutation and T790M was observed at PD, and ctDNA monitoring for sensitizing EGFR mutation at four cycles was better for predicting the outcome after osimertinib18. We found that the detection rate of ctDNA by digital PCR significantly decreased 1 month after osimertinib initiation, and that the detection of plasma T790M at PD was closely associated with worse outcomes. Although ctDNA monitoring in the early phase after osimertinib may not be useful for prognostic prediction, the detection of major EGFR mutation at pretreatment is predictive of PFS after osimertinib based on previous studies.
Several studies have investigated the prognostic significance of the ratio of T790M to major EGFR mutation at baseline in patients with advanced EGFR T790M-positive NSCLC receiving osimertinib and reported that a higher ratio is closely related to tumor shrinkage and favorable survival13,19. Two researchers observed that the ratio was significantly higher in patients with CR/PR/SD than in those with PD13,19. In the present study, the ratio of T790M/major EGFR mutation at pretreatment could not predict the outcome or tumor shrinkage after osimertinib administration. A previous study confirmed that the amount of plasma T790M at pretreatment is not a reliable biomarker for tumor response and survival13,19. This finding is similar to the results of the present study. Although the absence of major EGFR mutation in plasma at pretreatment may be a significant surrogate marker for the outcome after osimertinib treatment, we believe that baseline T790M level is not closely associated with response and prognostic prediction.
Our study has some limitations. First, the sample size was small, which may have biased the results. Second, the current study focused on patients harboring the T790M EGFR mutation after first- or second-generation EGFR-TKI administration. Currently, osimertinib is frequently administered to patients with naive EGFR-TKIs. Therefore, our digital PCR technique should be examined as an exploratory investigation for a predictive marker of first-line osimertinib. Moreover, we defined a copy number of 0 (copies/µL) as the cut-off value for further investigation. The cut-off values of copy number are different according to individual studies; therefore, it is uncertain whether an optimal cut-off value is determined by digital PCR. Finally, we were unable to investigate the mechanisms of resistance to osimertinib, except for C797S. Resistance mechanisms, such as the bypass signaling pathway, PTEN loss, MET amplification, MYC amplification, and small cell lung carcinoma transformation, have been described in previous reports20,21,22. Since resistance to osimertinib is closely associated with many tumor mutations, it is difficult to identify specific markers.
In conclusion, the detection of plasma T790M at PD after osimertinib treatment is identified as a significant predictor of worse outcomes after osimertinib administration. The detection of major EGFR mutations during pretreatment and PD also affects the outcome after treatment. Further investigation using a large-scale sample is warranted to confirm the results of our study.
Methods
Patients
A total of 40 patients with advanced EGFR T790M-mutant NSCLC on PD after first- or second-generation EGFR-TKI administration were registered in a prospective, observational multicenter study from August 2016 to December 2019. The inclusion criteria in this study were as follows: age ≥ 20 years, cytologically or histologically confirmed NSCLC harboring EGFR mutations, PD after first- or second-generation EGFR-TKI (gefitinib, erlotinib, or afatinib) administration, and verified EGFR T790M mutation in liquid and/or tissue re-biopsy. Clinical data were extracted from the medical records. This study was conducted according to the international guidelines on Good Clinical Practice and the Declaration of Helsinki and was approved by the institutional ethics committee (Gunma University Hospital Clinical Research Review Board) on 4th of April, 2017. (Registration number: 1524) Written informed consent was obtained from all participating individuals.
Treatment and evaluation
All patients were treated with osimertinib 80 mg daily as a starting dose, with dose reductions or interruptions based on the clinician’s discretion because of PD or therapeutic toxicity. Physical examination, complete blood count, biochemical testing, and adverse events were measured according to the judgment of each chief physician. Any toxicity was graded based on the Common Terminology Criteria for Adverse Events version 4.0. Tumor response was examined according to the Response Evaluation Criteria in Solid Tumors version 1.123.
Blood sample collection and epidermal growth factor receptor (EGFR) mutation analysis
Peripheral blood samples (20 mL) were collected in ethylenediaminetetraacetic acid tubes before pretreatment, 1 month after osimertinib treatment, and at PD. The samples were centrifuged at 3000 rpm for 15 min at room temperature and stored at − 80 °C until analysis. ctDNA was isolated using a cfDNA Sample Preparation Kit (Roche Molecular Systems).
EGFR mutation testing using Cobas was performed according to the manufacturer’s protocol. Mutation analysis was performed by PCR using a Cobas z480 analyzer (Roche Molecular Systems).
Droplet digital PCR (Bio-Rad) was performed according to previously reported techniques8, and sensitizing EGFR mutations, EGFR T790M, and EGFR C797S were detected. The primers and probe for the detection of sensitizing EGFR mutations and EGFR T790M were provided by Bio-Rad using the QUANTSOFT analytical software package (Bio-Rad). Primers and probes for detecting EGFR C797S were obtained from Riken Genetics. In the present study, we did not analyze the detection of L861Q based in the ddPCR.
Statistical analyses
For statistical analyses, we used Student’s t-test and the χ2 test for continuous and categorical variables, respectively. The statistical significance level was set at p < 0.05. Progression-free survival (PFS) was defined as the time from the day of initial osimertinib treatment to either earlier that of disease progression or death. Overall survival (OS) was defined as the time from the day of initial osimertinib treatment to that of death from any cause. The Kaplan–Meier method was used to estimate survival as a function of time, and survival differences were analyzed using the log-rank test. Univariate and multivariate analyses according to different variables were performed using logistic regression analysis. In this study, a copy number of 0 (copies/µL) was defined as negative, and a copy number greater than 0 was defined as positive, according to previous investigation24. The predictive value of T790M/major EGFR mutation ratio at pretreatment was determined by receiver operating characteristic (ROC) curve analyses, which were used for PFS to identify an optimal cut-off value. All statistical analyses were performed using GraphPad Prism (version 8.0; GraphPad Software, San Diego, CA, USA) and JMP 14.0 (SAS Institute Inc., Cary, North Carolina, USA).
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Kris, M. G. et al. Using multiplexed assays of oncogenic drivers in lung cancers to select targeted drugs. JAMA 311, 1998–2006 (2014).
Soria, J. C. et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N. Engl. J. Med. 378, 113–125 (2018).
Mok, T. S. et al. Osimertinib or platinum-pemetrexed in EGFR T790M-positive lung cancer. N. Engl. J. Med. 376, 629–640 (2017).
Seto, T. et al. Real-world EGFR T790M testing in advanced non-small-cell lung cancer: A prospective observational study in Japan. Oncol. Ther. 6, 203–215 (2018).
Ariyasu, R. et al. High ratio of T790M to EGFR activating mutations correlate with the osimertinib response in non-small-cell lung cancer. Lung Cancer 117, 1–6 (2018).
Ebert, E. B. F. et al. Clearing of circulating tumour DNA predicts clinical response to osimertinib in EGFR mutated lung cancer patients. Lung Cancer 143, 67–72 (2020).
U.S. Food and Drug Administration. Medical Devices: Cobas EGFR Mutation Test v2—P150047. Available online. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?id=P150047
Rolfo, C. et al. Liquid biopsy for advanced NSCLC: A consensus statement from the international association for the study of lung cancer. J. Thorac. Oncol. 16, 1647–1662 (2021).
Kasahara, N. et al. Plasma epidermal growth factor receptor mutation testing with a chip-based digital PCR system in patients with advanced non-small cell lung cancer. Lung Cancer 106, 138–144 (2017).
Oxnard, G. R. et al. Noninvasive detection of response and resistance in EGFR-mutant lung cancer using quantitative next-generation genotyping of cell-free plasma DNA. Clin. Cancer Res. 20, 1698–1705 (2014).
Thress, K. S. et al. EGFR mutation detection in ctDNA from NSCLC patient plasma: A cross-platform comparison of leading technologies to support the clinical development of AZD9291. Lung Cancer 90, 509–515 (2015).
Ding, P. N. et al. Plasma pre-treatment T790M relative allelic frequency in patients with advanced EGFR-mutated non-small cell lung cancer predicts treatment response to subsequent-line osimertinib. Transl. Lung Cancer Res. 10, 1623–1634 (2021).
Del Re, M. et al. The amount of activating EGFR mutations in circulating cell-free DNA is a marker to monitor osimertinib response. Br. J. Cancer 119, 1252–1258 (2018).
Beagan, J. J. et al. Circulating tumor DNA analysis of EGFR-mutant non-small cell lung cancer patients receiving osimertinib following previous tyrosine kinase inhibitor treatment. Lung Cancer 145, 173–180 (2020).
Papadimitrakopoulou, V. A. et al. Epidermal growth factor receptor mutation analysis in tissue and plasma from the AURA3 trial: osimertinib versus platinum-pemetrexed for T790M mutation-positive advanced non-small cell lung cancer. Cancer 126, 373–380 (2020).
Buder, A. et al. Cell-free plasma DNA-guided treatment with osimertinib in patients with advanced EGFR-mutated NSCLC. J. Thorac. Oncol. 13, 821–830 (2018).
Li, J. Y. C., Ho, J. C. M. & Wong, K. H. T790M mutant copy number quantified via ddPCR predicts outcome after osimertinib treatment in lung cancer. Oncotarget 9, 27929–27939 (2018).
Sakai, K. et al. Predicting osimertinib-treatment outcomes through EGFR mutant-fraction monitoring in the circulating tumor DNA of EGFR T790M-positive patients with non-small cell lung cancer (WJOG8815L). Mol. Oncol. 15, 126–137 (2021).
Bordi, P. et al. From the beginning to resistance: Study of plasma monitoring and resistance mechanisms in a cohort of patients treated with osimertinib for advanced T790M-positive NSCLC. Lung Cancer 131, 78–85 (2019).
Oxnard, G. R. et al. Assessment of resistance mechanisms and clinical implications in patients with EGFR T790M-positive lung cancer and acquired resistance to osimertinib. JAMA Oncol. 4, 1527–1534 (2018).
Le, X. et al. Landscape of EGFR-dependent and -independent resistance mechanisms to osimertinib and continuation therapy beyond progression in EGFR-mutant NSCLC. Clin. Cancer Res. 24, 6195–6203 (2018).
Yang, Z. et al. Investigating novel resistance mechanisms to third-generation EGFR tyrosine kinase inhibitor osimertinib in non-small cell lung cancer patients. Clin. Cancer Res. 24, 3097–3107 (2018).
Eisenhauer, E. A. et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 45, 228–247 (2009).
Buder, A. et al. EGFR mutation tracking predicts survival in adanced EGFR-mutated non-small cell lung cancer patients treated with osimertinib. Transl. Lung Cancer Res. 9, 239–245 (2020).
Acknowledgements
The authors thank Yosuke Miura, Yukiko Suto, and Takayuki Asao for their assistance in preparing this manuscript. The authors also thank Editage (www.editage.jp) for the English language editing.
Funding
This study was funded by AstraZeneca. This work was supported by JSPS KAKENHI (Grant Number: JP19K16855).
Author information
Authors and Affiliations
Contributions
O.Y., N.K. and K.K.: study conception and manuscript preparation. O.Y., H.S., H.I., I.N., H.Y., M.I., K.T., M.U., H.T., D.O., Y.M., A.S. and A.M.: patient management. N.K., K.K., N.S., T.M., K.M., H.M. and H.K.: statistical analysis and patient data collection. O.Y., N.K. and K.K.: manuscript revision. All authors contributed and agreed with the content of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
KK, NK and NS have received research grants and a speaker honorarium from Nihon Medi-Physics Co., Ltd and AstraZeneca. OY, AM and HK has received research grants and a speaker honorarium from AstraZeneca. All other authors declare no potential conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yamaguchi, O., Kasahara, N., Soda, H. et al. Predictive significance of circulating tumor DNA against patients with T790M-positive EGFR-mutant NSCLC receiving osimertinib. Sci Rep 13, 20848 (2023). https://doi.org/10.1038/s41598-023-48210-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-48210-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.