Abstract
Early detection of undiagnosed diabetes, hypertension or hyperlipidemia through screening could reduce healthcare costs resulting from disease complications. To date, despite ample research on the factors linked to the uptake of community health screening programs, little attention has been directed at delayed or incomplete follow-up after positive outcomes are identified in community screening tests. This study aimed to investigate the socioeconomic and behavioral factors that influence non-compliance with recommendations for primary care physician referrals, following community-based screening for diabetes, hypertension and hyperlipidemia. A parallel mixed-methods study was conducted. For quantitative data, we performed multivariable analysis on community-based chronic disease screening data. The qualitative component involved semi-structured interviews with individuals with both non-compliance and compliance with referral recommendations. Thematic data analysis was undertaken using the Theoretical Domains Framework (TDF). The quantitative analysis showed that older age (OR = 0.92, 95%CI [0.89–0.96]), non-Chinese ethnicity (OR = 0.24; 95% CI [0.08–0.44]) and residing in 5-room public/ private housing (OR = 0.40; 95% CI [0.14–0.74]) were associated with lower odds of non-compliance with referral recommendations. Thematic analysis identified multiple behavioral-level determinants acting as enablers or barriers within 7 TDF domains: awareness of health risks after receiving screening results, self-management orientation and behavioral control, fear of formal diagnosis and concerns about healthcare cost, optimistic belief driven by the lack of symptoms, interpersonal relationship and social obligations, aversion to medication, communication at the result collection and sense of uncertainty regarding self-scheduling of appointment. Findings provide valuable implications for the development of interventions aimed at improving adherence to referral recommendation. Future endeavors should include culturally sensitive outreach, evidence-based information dissemination, family-centered education, positive public health messaging, brief counseling during result collection and an opt-out appointment system to enhance follow-up care.
Similar content being viewed by others
Introduction
Growing evidence suggests that high fasting plasma glucose, high blood pressure, and elevated low-density lipoproteins, collectively referred to as metabolic syndrome, are modifiable risk factors for increased cardiovascular disease (CVD) events1,2,3. These three metabolic syndromes are the leading causes of mortality and morbidity worldwide, accounting for a substantial proportion of deaths and disability-adjusted life years (DALYs). According to the International Diabetes Federation, diabetes alone was responsible for an estimated 6.7 million deaths in 2021 and played a significant role in complications such as kidney failure, lower limb amputation, and visual impairment4. Moreover, a report from the World Health Organization indicated that CVD-related deaths attributed to hypertension and hyperlipidemia accounted for an estimated 17.9 million deaths, positioning it as the leading cause of death worldwide5. These disease burdens underscore the critical need for early diagnosis to address their shared underlying roots and mitigate the cumulative health risks they pose. As a result, it is crucial to implement effective prevention strategies to reduce the burden of these diseases.
Against this backdrop, many jurisdictions introduced community-based screenings in an effort to prevent disease progression and slow debilitating health outcomes11. While facility-based screenings can conveniently leverage existing resources, the substantial patient demand for curative services and the geographical placement of screening sites may serve as deterrents to participation especially among community-dwelling residents12. On the other hand, community-based screenings not only foster early disease detection to enable timely interventions but may also promote health equity by reaching underserved populations who may face barriers to accessing traditional healthcare facilities13,14. Beyond their clinical benefits, community health screening programs offer valuable opportunities for health education and empowerment, encouraging individuals to take an active role in their well-being15. By engaging with communities directly, these screenings facilitate a collaborative approach to healthcare, strengthening the social fabric and contributing to improved health outcomes on a broader scale.
Despite the positive effects outlined in community health screening programs, an issue that warrants attention is the suboptimal follow-up that often ensues. For example, in US and Netherlands, compliance rates for referral following a chronic disease screening in primary care were 63% and 86% respectively16. In Singapore where this study was conducted, one in four who were screened for either hypertension, hyperlipidemia or hyperglycemia and received a referral recommendation did not return for a doctor’s follow-up17. Failing to adhere to recommended follow-up care and treatment plans significantly increases the risk of disease progression and complications associated with chronic conditions. Low engagement in the recommended healthcare regimen may also result in poorly managed blood pressure, cholesterol levels, and blood sugar, thereby exacerbating the susceptibility to cardiovascular events, organ damage, and other severe health repercussions18,19,20. These findings stressed that while community-based initiatives are effective in identifying health concerns at an early stage, subsequent steps in ensuring comprehensive care and treatment for those detected with conditions may fall short, signaling an urgent need for targeted interventions to improve the adherence rates to follow-up care.
In the literature, extensive research has elucidated the factors influencing the uptake of community screening programs21,22,23. Barriers such as limited access to healthcare facilities, lack of awareness about available services, and financial constraints can impede follow-up effort24,25. However, an underexplored aspect exists within the realm of follow-up processes subsequent to these screenings. While past studies have investigated the challenges of referrals, their primary focus has often been on referrals from primary care settings to specialist clinics16,26,27. This lack of research underscores the need for a better understanding of the factors influencing post-screening behaviors, particularly in cases where ‘abnormal’ screening outcomes are observed. Undertaking community-based health screening requires substantial investment. If the targeted individuals fail to derive benefits from screenings, the investment in healthcare resources remains suboptimal28. Furthermore, poor follow-up can result in unnecessary disease progression and complications, which have a profound impact on an individual’s quality of life29. Hence, understanding the determinants of non-compliance is crucial for augmenting the effectiveness of community health screening programs.
The escalating prevalence of diabetes, hypertension, and hyperlipidemia on a global scale has transformed these conditions into pressing public health concerns30,31,32. As these chronic diseases place a significant burden on healthcare systems and contribute to a substantial portion of preventable morbidity and mortality, it is imperative to delve into the determinants of non-compliance and compliance with referral recommendations. Therefore, this study aimed to investigate the socioeconomic and behavioral factors that influence non-compliance with recommendations for primary care physician referrals following community-based screening for diabetes, hypertension and hyperlipidemia.
Methods
Setting
This study was conducted in Singapore, a multi-ethnic city-state in Southeast Asia. In Singapore, one in three deaths is attributed to diabetes, hypertension and high total cholesterol33. To mitigate the burden of chronic diseases, the government has stepped up efforts to conduct routine chronic disease screening, namely Screen for Life’, for hypertension, hyperlipidemia or diabetes mellitus in the community34. Individuals at risk of developing hypertension or hyperlipidemia were given a letter containing screening results in person at the community center or via postal mail and requested that they make an appointment with a primary care physician for further checkup. To encourage them to comply with referral recommendations, the SingHealth cluster implemented an additional measure; nurse practitioners reached out to these individuals, checked referral compliance and explained the potential risks associated with delayed appointments.
Study design
The study employed a mixed methods approach in which qualitative and quantitative data were collected and analyzed in parallel35. The quantitative data assessed socioeconomic factors and certain limited behavioral factors, while the qualitative data was obtained though semi-structured interviews with a subset of the quantitative data participants, aiming to elicit in-depth information about behavioral determinants influencing decisions on non-compliance/compliance. In the discussion section of the study, narrative integration was conducted to synthesize the quantitative and qualitative data, allowing for a more holistic understanding of the research findings. For qualitative data, we used the Theoretical Domains Framework (TDF)36. TDF was chosen because it provides sufficient breadth to analyze a wide range of cognitive, social, affective and environmental influences on behaviors (i.e., non-compliance). The TDF comprises 14 validated domains which include (1) knowledge, (2) skills, (3) social/professional role and identity, (4) beliefs about capabilities, (5) optimism, (6) beliefs about consequences, (7) reinforcement, (8) intentions, (9) goals, (10) memory, attention and decision processes, (11) environmental context and resources, (12) social influences, (13) emotion and (14) behavioral regulation.
Sampling and recruitment
Quantitative component
SingHealth, the largest public health cluster in Singapore, administers the national health screening program. One of the study team members overseeing the screening program (LL) facilitated the acquisition of screening dataset spanning from 2016 to 2019. During this period, a total of 1,625 screening cases were observed. We screened the cases according to the following eligibility criteria: (1) an abnormal screening outcome for diabetes, high blood pressure or high blood cholesterol as recorded by a physician in charge of community screening; (2) previously undiagnosed (i.e., not told by a doctor that they have the disease); (3) received a primary care physician referral recommendation; and (4) received follow-up calls by a nurse for up to 6 months.
We collected a set of independent variables for our study. Socioeconomic variables included age, gender, ethnicity, marital status, educational attainment, monthly household income, employment status, residential housing type (as a proxy for socioeconomic status) and whether individuals have a personal family doctor. Behavioral data included smoking status, engagement in physical activity. We also collected data on whether immediate family members formally diagnosed with diabetes, hypertension or hyperlipidemia. The selection of these variables was guided by existing literature. Previous research has indicated that factors such as income, education, and place of residence37 are associated with participation in screening tests. Another study found that age, marital status, income level, education, socioeconomic status, smoking and engagement in exercise can influence the uptake of screenings38. To categorize average monthly income, we utilized our dataset’s 25th percentile (below $2,000), median range ($4,000-$5,900) and 75th percentile ($6,000 and above) as cutoffs. This categorization aligns with local studies, which have also used thresholds of < SGD$2,000 to define low monthly income and ≥ SGD$6,000 to define high monthly income39,40. For smoking status, we adopted categorization of current smoker and ex-smoker or nonsmoker, as employed in previous research41. Our categorization for housing type was adapted from prior research42,43,44.
Qualitative component
The qualitative component utilized the same cohort as quantitative component to approach eligible participants by telephone. We employed purposive sampling based on compliance status and age to ensure a range of experiences relevant to our research aim. We recruited both compliant and non-compliant individuals to gain insight into how various behavioral factors influenced their behavior. This approach allowed us to better understand the specific factors enabling or hindering individual’s decisions regarding compliance. In-depth interviews with individuals were conducted. Written informed consent was obtained prior to the interviews. A semi-structured interview guide was developed. Topics included experience regarding the collection of screening results and physician follow-up recommendations that were relayed by on-site staff, reasons for compliance or non-compliance with the recommendation and experience of nurse follow-up calls (Supplementary material 1). Interviews were conducted by an interviewer trained in qualitative research methods and lasted 30–60 min. The interviews were audio-recorded and transcribed verbatim. This study was approved by the SingHealth Centralized Institutional Review Board (CIRB: 2019–2229).
Data analysis
Quantitative component
Descriptive summary statistics were presented as counts and percentages were used to describe the different sociodemographic composition between the compliant and non-compliant group. Pearson’s Chi-squared test of independence and Student’s t-test were employed to determine if specific sociodemographic factors differ between two groups for categorical and continuous variables. We performed bivariable and multivariable logistic regression models to compute the crude odds ratio and adjusted odds ratio respectively to examine the association between compliance status and socioeconomic characteristics. Variables in the multivariable logistic regression model were chosen based on their Variance Inflation Factor (VIF) values, with those having a VIF score of ≤ 5 being designated as independent variables to assess multicollinearity. To improve model fit, we performed a stepwise backward elimination procedure, with a p-value more than or equal to 0.1 as the significance level for variable removal. Statistical analyses were performed using IBM SPSS Statistics (Version 27). A p-value of less than 0.05 was considered statistically significant.
Qualitative component
We adopted both inductive and deductive approaches in data analysis. Inductive thematic analysis was performed involving immersion in the data, coding, repeated sorting, and comparison. Each transcript was coded line by line to create code components. Each component was compared with other components to ensure that they were mutually exclusive. Following iterative comparisons of components, they were grouped into categories and subthemes, which were then continually refined and classified while accounting for deviations. Categories and subthemes were subsequently mapped to the components of the TDF to systematically identify factors influencing compliance. All transcripts were independently coded by two coders (SY, HG). Discrepancies were resolved through an iterative consensus process. We used NVivo 12 for data management and coding. All methods were performed in accordance with relevant guidelines and regulations45.
Results
Characteristics of participants
Quantitative component
During the data collection period, 1,625 individuals completed the screening. Out of these, 528 individuals met the inclusion criteria resulting in the final sample for analysis (Supplementary material 2). The mean age was 60 years old. Around 60% were female, 89% were Chinese and 78% were married. Half of the individuals were in the workforce, and 62% completed secondary school or a higher level of education. A small proportion (7%) were current smokers while 71% reported routinely participating in physical activities. In terms of compliance with referral recommendations, nearly 70% of individuals were non-compliant (Table 1). Of note, only age was significantly different between the two groups (p < 0.05).
Qualitative component
We approached a total of 38 individuals, and 26 agreed to participate in the interviews. Reasons for the decline included being busy or lacking interest in participation. Data saturation was reached at 23 interviews, with no new categories and sub-themes emerging under or outside the TDF domains relevant to non-compliance/compliance with referral recommendations during subsequent interviews. To achieve point of information redundancy, three more interviews were conducted beyond data saturation. The age of participants spanned from 41 to 74, with a mean age of 56 years. The majority were Chinese (84%) and married (80%) (Table 2).
Factors associated with non-compliance/compliance
Quantitative component
A summary of socioeconomic and behavioral factors associated with non-compliance with physician referral recommendation is found in Table 3. At the bivariable level, older people (OR=0.96; 95% CI [0.95-0.98]) had lower odds of being non-compliant. Furthermore, non-Chinese (OR=0.49; 95% CI [0.25-0.97]) had lower odds of being non-compliant compared to Chinese. At the multivariable level, analyses revealed that after controlling for all covariates in the model, age (OR = 0.92, 95%CI [0.89–0.96]) and ethnicity (OR=0.24; 95% CI [0.08-0.44]) remained negatively associated with non-compliance amongst the participants. Meanwhile, housing type was also found to have a negative association with non-compliance, with individuals in 5-room public or private housing (OR=0.40; 95% CI [0.14-0.74]) had lower odds of being non-compliant compared to those residing in 1- to 2-room public housing (Table 3).
Qualitative component
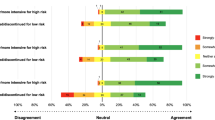
Our thematic analysis revealed several important behavioral factors acting as enablers or barriers to compliance under various TDF domains. By and large, out of 14 domains of TDF, seven domains were relevant to understanding behavioral determinants of non-compliance/compliance (Fig. 1).
Knowledge
One of the issues surrounding compliance was the awareness of health risks associated with undiagnosed conditions. Individuals who complied with the physician referral recommendation understood their personal risk and the need for follow-up. On the other hand, those who declined to comply with the recommendation generally lacked awareness of their health risks. Some participants offered a fatalistic view that justified their inaction or a passive approach to health.
“Because I found out [from screening] that my blood pressure is high, I should go and get more checkup… Since I knew that, I wanted to see what the doctor would recommend.” (#2, compliant)
“I know how I am doing. It is not about my cholesterol or the food I eat; it is something to do with my genetics. So, no matter what I try, things won’t really change.” (#P11, non-compliant)
Belief about capabilities
There was a consistent pattern within the data regarding beliefs of capabilities acting as either an enabler or barrier to compliance behaviors. Believing that undiagnosed diabetes, hypertension or hyperlipidemia could be prevented significantly influenced the willingness to visit a physician. This perceived behavioral control appeared to foster a sense of autonomy and prompted compliance. Conversely, for individuals with non-compliance, compensatory strategies such as perceptions of personal control reduced the perceived necessity of visiting a physician.
“I felt I could do something about this [high cholesterol]. So that made me want to see the doctor. But I told the doctor I wanted to manage it myself. I want to see if my condition gets better in a few months or a year without medical treatment.” (#P11, non-compliant)
“I didn’t see [a doctor] because I wanted to handle things on my own, I started making changes to my lifestyle. I am trying to exercise more and watch what I eat. I am sure my cholesterol has gotten better since the last time [screening].” (#P24, non-compliant)
Belief about consequences and emotions
Regardless of the compliance status, participants commonly appraised whether there would be positive or negative consequences of visiting a physician. Although anxiety about a formal diagnosis prevailed for both groups, a “peace of mind” or desire for early assurance encouraged individuals with compliance to make an appointment with a physician. They believed that a physician visit would be important for their future health outcomes. In contrast, the sense of fear of confirming the diagnosis and its associated future healthcare cost was a powerful barrier among those with non-compliance. Anticipating that they may have other chronic conditions notably reduced the likelihood of a physician visit.
“After seeing the [screening] results about my blood pressure, I got worried about having a stroke. I thought it would be better to see a doctor just to be safe.” (#P17, compliant)
“I always have this worry that if I visit the clinic and get thorough testing, I am afraid I can find out lot of other health issues, you know, then it feels like there is no end to it.” (#P25, non-compliant)
Optimism
Optimism, which could be unrealistic, played a key role in hindering non-compliance. This optimism was grounded in their belief that illness is always symptomatic. The lack of bodily symptoms influenced their perceptions that they were not at risk and thus did not feel the need for further actions.
“It wasn’t like very high, ridiculously high or high to worry about. It’s just that blood pressure is on the high side, nothing more. If it becomes extremely serious, I will definitely go immediately.” (#P24, non-compliant)
“I think the key point is I am doing well, you see. I feel great, so why should I spend the time and money to go through another health check?” (#P3, non-compliant)
Social roles and influences
The TDF describes social influences as the interpersonal processes that can change the way a person feels or behaves. Social support and expectations were found to be both enablers and barriers. Individuals with compliance described that family members were a powerful influence on their decision to make an appointment with the physician. Receiving multiple calls from a nurse also engendered a sense of moralization to drive these individuals to do the “right thing.” On the other hand, for individuals with non-compliance, social roles became the common factor affecting the decision to delay compliance with the referral recommendation. They described that their own healthcare needs were secondary to work commitments or childcare demands.
“The nurse called me several times telling me to go for a follow-up. I thought it was not nice to turn them down repeatedly. My daughter had been observing the situation and said why didn’t you go? That’s when I decided to schedule an appointment.” (#P7, compliant)
“I’m aware that my blood pressure might be high. But I haven’t been able to see the doctor because I’m busy, I have to take care of my son. I will plan to see the doctor when I have some free time in the future.” (#P23, non-compliant)
Reinforcement
The perceived belief that prescribed medications could reduce one’s risk and prevent further deterioration acted as a reinforcement to motivate individuals to comply with the recommendation. Conversely, a strong aversion to medications was a key barrier reinforcing their decision not to make a visit to a primary care clinic.
“I understand that this thing can be managed by taking necessary medications and staying active. That’s why I quickly visited the doctor at the polyclinic and got some prescriptions” (#P20, compliant)
“[I chose not to go] because taking a pill wouldn’t solve the root issue. The medication only controls symptoms, it doesn’t tackle the real problem. If you rely on medication too much, maybe you will have kidney problems down the line.” (#P11, non-compliant)
External context and resources
The system of reminder calls by the nurse to follow up with primary care physicians was an enabler for individuals with compliance. In contrast, miscommunication with community screening staff at the point of result collection served as a main barrier to compliance. Additionally, non-compliant participants reported that self-scheduling for an appointment was a challenge for them.
“I was really glad that they [the nurse] got in touch with me; it felt like they cared about me and my health. That’s what pushed me to go see a doctor.” (#P4, compliant)
“On the day that results were given out, there was no mention of needing to consult a doctor, so I thought everything was fine. The staff mentioned my [lab] results were okay.” (#P11, non-compliant)
“If they had scheduled an appointment, I would have definitely done the follow up. Since they left the choice of whether to or where to go up to me, I found it difficult to make a decision.” (#P11, non-compliant)
Discussion
Adherence to referral recommendations subsequent to community health screening is vital in order to ensure early detection and well-timed management for persons with undiagnosed diabetes, high blood pressure or high blood cholesterol. While the quantitative data revealed some socioeconomic and behavioral determinants, interviews provided behavioral nuances and contexts leading to decisions on non-compliance/compliance. These two sets of results combined to offer a fuller understanding of why a segment of individuals with undiagnosed conditions opted against follow-up despite the need to consult a medical professional to understand their health risks and manage them in a timely manner.
Our quantitative findings suggest that some socioeconomic factors such as younger age, Chinese ethnicity and residing in less affordable housing were associated with non-compliance. Although no straightforward comparison is possible due to sparse literature on this topic, it has been generally recognized that people of older age, being married, and higher education are more likely to participate in preventive health screening than their counterparts21,46,47. In addition, overseas studies corroborate that younger age and types of neighborhoods were key determinants of non-adherence to follow-up appointments with both primary and specialist care. For instance, Cristel et al. observed a reduced likelihood of compliance with specialist care referrals among patients residing in socioeconomically disadvantaged urban areas and those aged between 18 and 44 years26. In a separate study, Adrian et al. noted a tendency among patients aged 18 to 39 years to forgo general practitioner consultations for confirming screening results48. Our finding also revealed an intriguing observation that non-Chinese individuals (i.e., Malays and Indians) exhibited a greater tendency toward compliance in comparison to the Chinese population. This finding stands in stark contrast with the finding from a previous study, which indicated that Malays were less likely to attend health screening compared with the Chinese23. The difference in outcomes can be explained by the timing of the two studies. Our study was conducted after the implementation of strategic initiatives designed to engage and support the Malay and Indian community49,50,51. As a result, it is reasonable to assume that the higher compliance rates among non-Chinese individuals in our study could potentially be linked to the successful approach that considers ethnic disparities when addressing health issues among different ethnic groups. These findings, together with ours, indicate the need for tailored outreach efforts for particular segments of the population, such as younger age groups and individuals with low socioeconomic status. In addition, given Singapore’s diverse ethnic makeup, it is imperative to continue developing tailored outreach and education initiatives that incorporate culturally sensitive materials and multilingual resources, to further enhance accessibility and health literacy among different ethnic groups52. Lastly, effective policies should be formulated to facilitate collaboration and partnerships with local community organizations, recognizing their pivotal role in reaching out to residents and potentially serving as key facilitators in ensuring ongoing follow-up after health screenings53,54.
The quantitative analysis reveals that health behaviors such as current smoking and physical activity did not show a significant association with non-compliance decisions. This contrasts with a previous study that found positive effects of health behaviors on the acceptance of health screenings.56 This finding may be explained by the fact that the majority of our participants, irrespective of their compliance status, were non- or ex-smokers (92%) and engaged in regular physical activity (72%). Our interview data further indicates that many non-compliant individuals declined referral recommendations because they believed their self-management efforts were sufficient and strongly preferred personal control (belief about capabilities). Consequently, they did not perceive the need for a physician follow-up. However, it is worth noting that maintaining motivation to sustain healthy behaviors and revert early stages of a condition can be a challenge, as supported by existing literature57,58. Future intervention may benefit from providing evidence-based information on disease progression through various channels (e.g., national health agencies, expert testimonials) to enhance awareness of the importance of physician referrals.
Within the TDF framework, we identified seven domains relevant to non-compliance/compliance behaviors. One key determinant was social roles and influences, which acted as both a barrier and an enabler. While the support received from family members could encourage individuals, social obligations and relationships often hindered them from prioritizing their health over other competing social demands. This finding resonates with existing literature that interpersonal dynamics and role expectations significantly influence health-seeking behaviors59,60,61. Although our quantitative analysis did not show a direct influence of family members’ chronic diseases on non-compliance behavior, we noted that 55% (201 out of 360) of family members of non-compliant individuals had previously been diagnosed with chronic diseases. Given that family history represents an important non-modifiable risk factor for conditions like hypertension and diabetes62, it becomes imperative to develop family-centered education initiatives and support networks aimed at fostering mutual support thereby improving compliance behavior.
From our qualitative analysis, it became apparent that belief of consequences and emotions, such as the fear of formal diagnosis and its associated healthcare cost, were important determinants of referral compliance. Although concerns about healthcare costs can be addressed through counseling of available subsidies and financial support, what has been deficient was addressing emotions, particularly when it is combined with optimism, such as low illness perceptions. This means that there is a scope to incorporate interventions targeting psychological barriers and enablers. Behavioral research suggests that over-emphasis on health risks triggers fear, while undermining risks increases blind optimism and diminishes motivation63,64. Therefore, a public health message on referrals should be framed to highlight the positive consequences, such as reassurance for negative results and potential positive health outcomes, and at the same time, raise awareness of anticipated regret if individuals opt not to adhere to the referral recommendations.
Another notable finding from interviews is related to the external context and resources that have implications for system-based improvements. Contrary to existing literature, our research shows that participants value reminders, facilitating compliance65. However, inadequate communication at the point of result collection appears to be one of the main factors influencing compliance. Hence, integrating “teachable moment” brief education and counseling at the point of result collection could be considered to increase the attention of the target audience and ensure an educated decision in the midst of uncertainty66. This brief education is most beneficial to those with limited knowledge and strong aversion to medications (reinforcement), as identified by our study, and it should also address practical support to overcome unique barriers. Although knowledge alone may not result in behavior, it can inform beliefs, which in turn affect more proximal factors of behavior change like intentions and readiness, as shown in behavioral health theories67. Similarly, aversion to medications could be addressed by brief communication with individuals at the result collection, offering them a broader spectrum of choices to manage their health conditions while explaining the potential benefits of prescribed medicines. Optimization of primary care referral programs after screening is critical; as many non-compliant participants cited confusion related to scheduling an appointment with a primary care provider, prescheduling of appointments or an opt-out appointment system can be considered to improve compliance with recommendations as shown in other studies68,69. Healthier SG, a recent national initiative aimed at enrolling residents in their preferred family clinic for long-term personalized care, may offer a potential solution to the challenges associated with scheduling follow-up appointments70.
Our study has several strengths. Using both administrative data and theory-informed empirical interviews, the study comprehensively assessed the factors influencing non-compliance with physician referral recommendations. The TDF domains allowed us to systematically evaluate the determinants of behavior through a well-developed theoretical underpinning, which can facilitate evidence-based links to behavior change techniques. A recent systematic review of TDF applied literature highlighted the notable deficiency of non-Western studies, and therefore this study will make a meaningful contribution to the body of literature71. Limitations of this study include a skewed sample of the qualitative component with disproportionately more male and Chinese participants, and thus it is possible that we fail to capture distinct perspectives from female and other ethnic groups. Further research is warranted to understand the unique determinants among individuals from culturally diverse and minority backgrounds. Another potential limitation is that our qualitative data may not encompass all 14 domains of the TDF. However, we identified seven key domains as the most critical factors influencing non-compliance/compliance behavior through careful mapping of qualitative data. As this study was conducted in Singapore, an urban city-state, our findings may not be transferrable to rural and remote settings.
Conclusions
Community health screenings serve as a vital initial step in detecting potential health issues, but their true impact hinges on individuals taking an initiative to follow through with physician referral recommendations based on their screening results. Our study shed light on key socioeconomic factors, including lower socioeconomic status, younger age, and Chinese ethnicity, which influence non-compliance behavior. At the same time, behavioral factors such as sense of personal control, awareness of health risks, optimistic outlook, social demands, fear of confirming a diagnosis, and systemic challenges play a pivotal role in shaping individuals’ decisions regarding non-compliance/compliance. Our mixed-methods approach had provided a complementary view of the key determinants and valuable implications for the development of interventions aimed at addressing modifiable factors and improving adherence to referral recommendations. Future endeavors should include targeted and culturally sensitive outreach efforts, evidence-based information dissemination, family-centered educational programs, framing public health messages to emphasize positive outcomes of actions, the incorporation of brief education and counseling during result collection and the implementation of an opt-out appointment system. These strategies could collectively contribute to a more effective approach to promoting follow-up care and ultimately improving health outcomes.
Data availability
The datasets generated during the study are available from the corresponding author upon reasonable request.
References
Arnett, D. K. et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American college of Cardiology/American heart association task force on clinical practice guidelines. Circulation 140, e596–e646. https://doi.org/10.1161/cir.0000000000000678 (2019).
Rawshani, A. et al. Mortality and cardiovascular disease in type 1 and type 2 diabetes. N. Engl. J. Med. 376, 1407–1418. https://doi.org/10.1056/NEJMoa1608664 (2017).
Cai, X. et al. Association between prediabetes and risk of all cause mortality and cardiovascular disease: updated meta-analysis. BMJ 370, m2297. https://doi.org/10.1136/bmj.m2297 (2020).
Federation, I. D. Diabetes around the world in 2021, https://diabetesatlas.org/#:~:text=Diabetes%20around%20the%20world%20in%202021%3A&text=Diabetes%20is%20responsible%20for%206.7,over%20the%20last%2015%20years. (2021).
Organization, W. H. Cardiovascular Diseases, https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (2021).
Petrie, J. R., Guzik, T. J. & Touyz, R. M. Diabetes, hypertension, and cardiovascular disease: clinical insights and vascular mechanisms. Can. J. Cardiol. 34, 575–584. https://doi.org/10.1016/j.cjca.2017.12.005 (2018).
Leon, B. M. & Maddox, T. M. Diabetes and cardiovascular disease: Epidemiology, biological mechanisms, treatment recommendations and future research. World J. Diabetes 6, 1246–1258. https://doi.org/10.4239/wjd.v6.i13.1246 (2015).
Athyros, V. G. et al. Diabetes and lipid metabolism. Hormones (Athens) 17, 61–67. https://doi.org/10.1007/s42000-018-0014-8 (2018).
Ohishi, M. Hypertension with diabetes mellitus: physiology and pathology. Hypertens Res. 41, 389–393. https://doi.org/10.1038/s41440-018-0034-4 (2018).
Zhai, Z. et al. The hypertension and hyperlipidemia status among type 2 diabetic patients in the community and influencing factors analysis of glycemic control. Diabetol. Metab. Syndr. 15, 73. https://doi.org/10.1186/s13098-023-01013-0 (2023).
Berger, J. S., Jordan, C. O., Lloyd-Jones, D. & Blumenthal, R. S. Screening for cardiovascular risk in asymptomatic patients. J. Am. College Cardiol. 55, 1169–1177. https://doi.org/10.1016/j.jacc.2009.09.066 (2010).
Chien, S. Y., Chuang, M. C. & Chen, I. P. Why people do not attend health screenings: factors that influence willingness to participate in health screenings for chronic diseases. Int. J. Environ. Res. Public Health 17, https://doi.org/10.3390/ijerph17103495 (2020).
Soltani, S. et al. Community-based cardiovascular disease prevention programmes and cardiovascular risk factors: a systematic review and meta-analysis. Public Health 200, 59–70. https://doi.org/10.1016/j.puhe.2021.09.006 (2021).
Timm, L. et al. Early detection of type 2 diabetes in socioeconomically disadvantaged areas in Stockholm—comparing reach of community and facility-based screening. Glob. Health Action 13, 1795439. https://doi.org/10.1080/16549716.2020.1795439 (2020).
Mooney, L. A. & Franks, A. M. Impact of health screening and education on knowledge of coronary heart disease risk factors. J. Am. Pharm. Assoc. 2003(51), 713–718. https://doi.org/10.1331/JAPhA.2011.10127 (2011).
Forrest, C. B., Shadmi, E., Nutting, P. A. & Starfield, B. Specialty referral completion among primary care patients: results from the ASPN Referral Study. Ann. Fam. Med. 5, 361–367. https://doi.org/10.1370/afm.703 (2007).
Lai, L. in The Straits Times.
Khatib, R. et al. Patient and healthcare provider barriers to hypertension awareness, treatment and follow up: a systematic review and meta-analysis of qualitative and quantitative studies. PLoS One 9, e84238. https://doi.org/10.1371/journal.pone.0084238 (2014).
Adu, M. D., Malabu, U. H., Malau-Aduli, A. E. O. & Malau-Aduli, B. S. Enablers and barriers to effective diabetes self-management: A multi-national investigation. PLoS One 14, e0217771. https://doi.org/10.1371/journal.pone.0217771 (2019).
Brunner-La Rocca, H. P. et al. Challenges in personalised management of chronic diseases-heart failure as prominent example to advance the care process. Epma J. 7, 2. https://doi.org/10.1186/s13167-016-0051-9 (2015).
AshaRani, P. V. et al. Factors influencing uptake of diabetes health screening: a mixed methods study in Asian population. BMC Public Health 22, 1511. https://doi.org/10.1186/s12889-022-13914-2 (2022).
Rollet, Q., Tron, L., De Mil, R., Launoy, G. & Guillaume, É. Contextual factors associated with cancer screening uptake: A systematic review of observational studies. Prev. Med. 150, 106692. https://doi.org/10.1016/j.ypmed.2021.106692 (2021).
Venkataraman, K. et al. Determinants of individuals' participation in integrated chronic disease screening in Singapore. J. Epidemiol. Commun. Health (1979-) 70, 1242–1250 (2016).
Zimolzak, A. J. et al. Why test results are still getting “lost” to follow-up: a qualitative study of implementation gaps. J. Gen. Intern. Med. 37, 137–144. https://doi.org/10.1007/s11606-021-06772-y (2022).
Callen, J. L., Westbrook, J. I., Georgiou, A. & Li, J. Failure to follow-up test results for ambulatory patients: a systematic review. J. Gen. Intern. Med. 27, 1334–1348. https://doi.org/10.1007/s11606-011-1949-5 (2012).
van Dijk, C. E. et al. Compliance with referrals to medical specialist care: patient and general practice determinants: a cross-sectional study. BMC Family Practice 17, 11. https://doi.org/10.1186/s12875-016-0401-7 (2016).
Patel, M. P. et al. Closing the referral loop: an analysis of primary care referrals to specialists in a large health system. J. Gen. Intern. Med. 33, 715–721. https://doi.org/10.1007/s11606-018-4392-z (2018).
Michaud, T. L. et al. Costing a population health management approach for participant recruitment to a diabetes prevention study. Trans. Behav. Med. 11, 1864–1874. https://doi.org/10.1093/tbm/ibab054 (2021).
Association, A. D. Standards of medical care in diabetes—2022 abridged for primary care providers. Clin. Diab. 40, 10–38. https://doi.org/10.2337/cd22-as01 (2022).
Pirillo, A., Casula, M., Olmastroni, E., Norata, G. D. & Catapano, A. L. Global epidemiology of dyslipidaemias. Nat. Rev. Cardiol. 18, 689–700. https://doi.org/10.1038/s41569-021-00541-4 (2021).
Mills, K. T., Stefanescu, A. & He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 16, 223–237. https://doi.org/10.1038/s41581-019-0244-2 (2020).
Animaw, W. & Seyoum, Y. Increasing prevalence of diabetes mellitus in a developing country and its related factors. PLoS One 12, e0187670. https://doi.org/10.1371/journal.pone.0187670 (2017).
National Health Survey, https://www.moh.gov.sg/docs/librariesprovider5/resources-statistics/reports/national-population-health-survey-2021-report.pdf (2021).
Screen for Life, https://hpb.gov.sg/healthy-living/preventive-health/screenforlife (2019).
Creswell, J. W. & Plano Clark, V. L. Designing and conducting mixed methods research 3rd edn. (Sage, 2017).
Atkins, L. et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement. Sci. 12, 77. https://doi.org/10.1186/s13012-017-0605-9 (2017).
Finkelstein, M. M. Preventive screening. What factors influence testing? Can. Family Phys. 48, 1494–1501 (2002).
Lin, S.-J. Factors influencing the uptake of screening services for breast and cervical cancer in Taiwan. J. R. Soc. Prom. Health 128, 327–334. https://doi.org/10.1177/1466424007092802 (2008).
Teo, E., Lew, P. & Foo, C. Public perceptions of obesity and bariatric surgery in Singapore: a pilot study. Singapore Med. J. 53, 104 (2012).
Sabanayagam, C. et al. Prevalence of diabetes mellitus, glycemic control, and associated factors in a Malay population in Singapore. Asia Pacific J. Public Health 21, 385–398 (2009).
Sabanayagam, C., Shankar, A., Saw, S. M., Tai, E. S. & Wong, T. Y. The association between socioeconomic status and overweight/obesity in a Malay population in Singapore. Asia Pacific J. Public Health 21, 487–496 (2009).
Zheng, Y. et al. Prevalence and risk factors of diabetic retinopathy in migrant Indians in an urbanized society in Asia: the Singapore Indian eye study. Ophthalmology 119, 2119–2124. https://doi.org/10.1016/j.ophtha.2012.04.027 (2012).
Tan, G. S. et al. Ethnic differences in the prevalence and risk factors of diabetic retinopathy: the Singapore epidemiology of eye diseases study. Ophthalmology 125, 529–536. https://doi.org/10.1016/j.ophtha.2017.10.026 (2018).
Ong, S. Y. et al. Visual impairment, age-related eye diseases, and cognitive function: the Singapore Malay eye study. Arch. Ophthalmol. 130, 895–900. https://doi.org/10.1001/archophthalmol.2012.152 (2012).
Tong, A., Sainsbury, P. & Craig, J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 19, 349–357. https://doi.org/10.1093/intqhc/mzm042 (2007).
Du, B. & Mu, Y. The relationship between health changes and community health screening participation among older people. Front Public Health 10, 870157. https://doi.org/10.3389/fpubh.2022.870157 (2022).
Chien, S. Y., Chuang, M. C., Chen, I. P. & Yu, P. H. Primary drivers of willingness to continue to participate in community-based health screening for chronic diseases. Int. J. Environ. Res. Public Health 16, https://doi.org/10.3390/ijerph16091645 (2019).
Fianu, A. et al. Usefulness of home screening for promoting awareness of impaired glycemic status and utilization of primary care in a low socio-economic setting: a follow-up study in Reunion Island. Int. J. Health Policy Manag. 11, 2208–2218, https://doi.org/10.34172/ijhpm.2021.114 (2022).
Baker, J. New workgroup set up to improve health of minority ethnic groups, <https://www.channelnewsasia.com/singapore/new-workgroup-set-up-improve-health-minority-ethnic-groups-308291> (2021).
Baker, J. in Channel News Asia (Singapore, 2021).
PT, W. in Today (Singapore, 2022).
Lim, W. Y., Ma, S., Heng, D., Bhalla, V. & Chew, S. K. Gender, ethnicity, health behaviour & self-rated health in Singapore. BMC Public Health 7, 184. https://doi.org/10.1186/1471-2458-7-184 (2007).
Barker, S. L. et al. Community-engaged healthcare model for currently under-served individuals involved in the healthcare system. SSM Popul Health 15, 100905. https://doi.org/10.1016/j.ssmph.2021.100905 (2021).
Zahner, S. J., Kaiser, B. & Kapelke-Dale, J. Local partnerships for community assessment and planning. J. Public Health Manag. Pract. 11, 460–464. https://doi.org/10.1097/00124784-200509000-00016 (2005).
Fianu, A. et al. Usefulness of home screening for promoting awareness of impaired glycemic status and utilization of primary care in a low socio-economic setting: a follow-up study in Reunion Island. Int. J. Health Policy Manag. 11, 2208–2218, https://doi.org/10.34172/ijhpm.2021.114 (2021).
Lin, S. J. Factors influencing the uptake of screening services for breast and cervical cancer in Taiwan. J. R. Soc. Promot. Health 128, 327–334. https://doi.org/10.1177/1466424007092802 (2008).
Yoon, S., Wee, S., Loh, D. H. F., Bee, Y. M. & Thumboo, J. Facilitators and barriers to uptake of community-based diabetes prevention program among multi-ethnic Asian patients with prediabetes. Front. Endocrinol. (Lausanne) 13, 816385, https://doi.org/10.3389/fendo.2022.816385 (2022).
Yoon, S., Kwan, Y. H., Phang, J. K., Tan, W. B. & Low, L. L. Personal goals, barriers to self-management and desired mhealth application features to improve self-care in multi-ethnic asian patients with type 2 diabetes: a qualitative study. Int. J. Environ. Res. Public Health 19, https://doi.org/10.3390/ijerph192215415 (2022).
Chan, C. K. Y. et al. Social support and self-care outcomes in adults with diabetes: The mediating effects of self-efficacy and diabetes distress. Results of the second diabetes MILES—Australia (MILES-2) study. Diab. Res. Clin. Pract. 166, 108314, https://doi.org/10.1016/j.diabres.2020.108314 (2020).
Schram, M. T., Assendelft, W. J. J., van Tilburg, T. G. & Dukers-Muijrers, N. H. T. M. Social networks and type 2 diabetes: a narrative review. Diabetologia 64, 1905–1916. https://doi.org/10.1007/s00125-021-05496-2 (2021).
de Wit, M., Trief, P. M., Huber, J. W. & Willaing, I. State of the art: understanding and integration of the social context in diabetes care. Diabetic Med. 37, 473–482. https://doi.org/10.1111/dme.14226 (2020).
Li, A. L., Peng, Q., Shao, Y. Q., Fang, X. & Zhang, Y. Y. The interaction on hypertension between family history and diabetes and other risk factors. Sci. Rep. 11, 4716. https://doi.org/10.1038/s41598-021-83589-z (2021).
Weinstein, N. D. Unrealistic optimism about susceptibility to health problems. J. Behav. Med. 5, 441–460. https://doi.org/10.1007/bf00845372 (1982).
Lerner, J. S., Li, Y., Valdesolo, P. & Kassam, K. S. Emotion and decision making. Ann. Rev. Psychol. 66, 799–823. https://doi.org/10.1146/annurev-psych-010213-115043 (2015).
Nielsen, K. D., Dyhr, L., Lauritzen, T. & Malterud, K. You can’t prevent everything anyway: a qualitative study of beliefs and attitudes about refusing health screening in general practice. Fam. Pract. 21, 28–32. https://doi.org/10.1093/fampra/cmh107 (2004).
Rodriguez-Gutierrez, R., Lipska, K. J. & McCoy, R. G. Intensive glycemic control in type 2 diabetes mellitus—a balancing act of latent benefit and avoidable harm: a teachable moment. JAMA Internal. Med. 176, 300–301. https://doi.org/10.1001/jamainternmed.2015.8320 (2016).
Kelly, M. P. & Barker, M. Why is changing health-related behaviour so difficult?. Public Health 136, 109–116. https://doi.org/10.1016/j.puhe.2016.03.030 (2016).
Bunten, A., Porter, L., Gold, N. & Bogle, V. A systematic review of factors influencing NHS health check uptake: invitation methods, patient characteristics, and the impact of interventions. BMC Public Health 20, 93. https://doi.org/10.1186/s12889-019-7889-4 (2020).
Begum, S., Povey, R., Ellis, N. & Gidlow, C. A systematic review of recruitment strategies and behaviour change techniques in group-based diabetes prevention programmes focusing on uptake and retention. Diabetes Res. Clin. Pract 166, 108273. https://doi.org/10.1016/j.diabres.2020.108273 (2020).
Healthier SG, https://www.healthiersg.gov.sg/
Dyson, J. & Cowdell, F. How is the Theoretical Domains Framework applied in designing interventions to support healthcare practitioner behaviour change? A systematic review. Int. J. Qual. Health Care 33, https://doi.org/10.1093/intqhc/mzab106 (2021).
Acknowledgements
We would like to thank the participants who provided valuable insights for the study.
Funding
This research was supported by the National Research Foundation, Singapore under its AI Singapore Programme (AISG Award No.: AISG-GC-2019–001-2A). This research is also supported by the Ministry of Education Academic Research Fund Tier 1 (Award No: 2022-moet1-0005).
Author information
Authors and Affiliations
Contributions
The concept for the study was developed by S.Y. and L.L.L. H.G., J.K.P. and Y.H.K. collected the data. S.Y. and H.G. analyzed the data. S.Y. wrote the first draft, and all authors contributed and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yoon, S., Goh, H., Phang, J.K. et al. Socioeconomic and behavioral determinants of non-compliance with physician referrals following community screening for diabetes, hypertension and hyperlipidemia: a mixed-methods study. Sci Rep 13, 20554 (2023). https://doi.org/10.1038/s41598-023-47168-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-47168-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.