Abstract
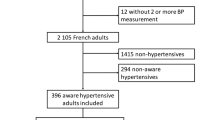
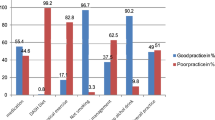
Suboptimal medication adherence is a major barrier to hypertension control in Kenya, especially among informal urban settlement areas (sometimes referred to as “slums”). The few studies that have specifically explored medication adherence among this population have received discordant results, implying that additional factors which influence medication adherence merit further investigation. This study explores the relationship between family support and medication adherence among people with hypertension in informal settlements in Nairobi, Kenya. We conducted a quantitative survey followed up by semi-structured qualitative interviews. The sampling frame comprised two health facilities in informal settlement areas of the Korogocho neighborhood and participants were recruited via convenience sampling. We performed multiple logistic regressions for quantitative data and thematic analysis for qualitative data. A total of 93 people participated in the survey (mean age: 57 ± 14.7, 66% female). Most participants reported high family support (82%, n = 76) and suboptimal medication adherence (43% by the Morisky Scale; 76% by the Hill-Bone Scale), with no significant associations between family support and medication adherence. During interviews, many participants reported they lacked health knowledge and education. We suggest that the lack of health knowledge among this population may have contributed to a failure for family support to meaningfully translate into improvements in medication adherence. Our results underscore the need for further research to improve hypertension control among this uniquely disadvantaged population, especially with respect to the possible mediating influence of health education on family support and medication adherence.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
References
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–23.
WHO. A global brief on hypertension—silent killer, global public health crisis. World Health Day. 2013. [cited 2021 Dec 3]. Available from: http://apps.who.int/iris/bitstream/10665/79059/1/WHO_DCO_WHD_2013.2_eng.pdf?ua=1
van de Vijver SJ, Oti SO, Agyemang C, Gomez GB, Kyobutungi C. Prevalence, awareness, treatment and control of hypertension among slum dwellers in Nairobi, Kenya. J Hypertens. 2013;31:1018–24.
Joshi MD, Ayah R, Njau EK, Wanjiru R, Kayima JK, Njeru EK, et al. Prevalence of hypertension and associated cardiovascular risk factors in an urban slum in Nairobi, Kenya: a population-based survey. BMC Public Health. 2014;14:1–0.
Hendriks ME, Wit FW, Roos MT, Brewster LM, Akande TM, De Beer IH, et al. Hypertension in sub-Saharan Africa: cross-sectional surveys in four rural and urban communities. PloS One. 2012;7:e32638.
Ongeti KW, Ogeng’o JA, Pulei AN, Olabu BO, Gakara CN Blood pressure characteristics among slum dwellers in Kenya. Glob Adv Res J Microbiol. 2013;2.
Jenson A, Omar AL, Omar MA, Rishad AS, Khoshnood K. Assessment of hypertension control in a district of Mombasa, Kenya. Glob Public Health. 2011;6:293–306.
Mohamed SF, Mutua MK, Wamai R, Wekesah F, Haregu T, Juma P, et al. Prevalence, awareness, treatment and control of hypertension and their determinants: results from a national survey in Kenya. BMC Public Health. 2018;18:1–0.
World Health Organization [WHO] (2003). Adherence to Long-Term Therapies. Evidence for Action. Available at: http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf [accessed 2 September, 2021].
Vrijens B, Antoniou S, Burnier M, de la Sierra A, Volpe M. Current situation of medication adherence in hypertension. Front Pharmacol. 2017;8:100.
Burnier M, Egan BM. Adherence in hypertension: a review of prevalence, risk factors, impact, and management. Circulation Res. 2019;124:1124–40.
Kuria NE, Reid A, Owiti P, Tweya H, Kibet CK, Mbau L, et al. Compliance with follow‐up and adherence to medication in hypertensive patients in an urban informal settlement in Kenya: comparison of three models of care. Tropical Med Int Health. 2018;23:785–94.
Hulzebosch A, Vijver SVD, Oti SO, Egondi T, Kyobutungi C. Profile of people with hypertension in Nairobi’s slums: a descriptive study. Globalization Health. 2015;11:26.
Nielsen JØ, Shrestha AD, Neupane D, Kallestrup P. Non-adherence to anti-hypertensive medication in low-and middle-income countries: a systematic review and meta-analysis of 92443 subjects. J Hum Hypertens. 2017;31:14–21.
UN-Habitat. The State of African Cities 2008: a Framework for Addressing Urban Challenges in Africa. Nairobi: UN Habitat; 2008.
UN-Habitat. The Challenge of Slums: Global Report on Human Settlements 2003. London: Earthscan; 2003.
Emina J, Beguy D, Zulu EM, Ezeh AC, Muindi K, Elung’ata P, et al. Monitoring of health and demographic outcomes in poor urban settlements: evidence from the Nairobi Urban Health and Demographic Surveillance System. J Urban Health. 2011;88 Suppl 2:S200–S218.
Faye O, Baschieri A, Falkingham J, Muindi K. Hunger and food insecurity in Nairobi’s slums: an assessment using IRT models. J Urban Health. 2011;88 Suppl 2:S235–S255.
Chambers EC, Duarte CS, Yang FM. Household instability, area poverty, and obesity in urban mothers and their children. J Healthc Poor Underserved. 2009;20:122–33.
Hill TD, Angel RJ. Neighborhood disorder, psychological distress, and heavy drinking. Soc Sci Med. 2005;61:965–75.
Kenya Healthcare Federation. Task Force Health Care. Kenyan: Kenyan Healthcare Sector: Opportunities for the Dutch Life Sciences & Health Sector, 2016.
Kimani S, Mirie W, Chege M, Okube OT, Muniu S. Association of lifestyle modification and pharmacological adherence on blood pressure control among patients with hypertension at Kenyatta National Hospital, Kenya: a cross-sectional study. BMJ Open. 2019;9:e023995.
Anand K, Shah B, Yadav K, Singh R, Mathur P, Paul E, et al. Are the urban poor vulnerable to non-communicable diseases? A survey of risk factors for non-communicable diseases in urban slums of Faridabad. Natl Med J India. 2007;20:115.
Olack B, Wabwire-Mangen F, Smeeth L, Montgomery JM, Kiwanuka N, Breiman RF. Risk factors of hypertension among adults aged 35-64 years living in an urban slum Nairobi, Kenya. BMC Public Health. 2015;15:1251.
Olalemi OE, Muyibi SA, Ladipo MM. Perceived Family Support and Medication Adherence amongst Hypertensive Outpatients in a Tertiary Hospital, Ibadan, Nigeria. West Afr J Med. 2020;37:481–9.
Chacko S, Jeemon P Role of family support and self-care practices in blood pressure control in individuals with hypertension: results from a cross-sectional study in Kollam District, Kerala. Wellcome Open Res. 2020;5:180.
Waari G, Mutai J, Gikunju J. Medication adherence and factors associated with poor adherence among type 2 diabetes mellitus patients on follow-up at Kenyatta National Hospital, Kenya. Pan Afr Med J. 2018;29:1–5.
Scheurer D, Choudhry N, Swanton KA, Matlin O, Shrank W. Association between different types of social support and medication adherence. Am J managed care. 2012;18:e461–7.
Ojo O, Malomo S, Sogunle P. Blood pressure (BP) control and perceived family support in patients with essential hypertension seen at a primary care clinic in Western Nigeria. J Fam Med Prim Care. 2016;5:569.
Costa Rdos S, Nogueira LT. Family support in the control of hypertension. Rev Lat Am Enferm. 2008;16:871–6.
Olowookere AJ, Olowookere SA, Talabi AO, Etonyeaku AC, Adeleke OE, Akinboboye OO. Perceived family support and factors influencing medication adherence among hypertensive patients attending a Nigerian tertiary hospital. Ann Tropical Med Public Health. 2015;8:241.
Mayberry LS, Osborn CY. Family support, medication adherence, and glycemic control among adults with type 2 diabetes. Diabetes care. 2012;35:1239–45. https://doi.org/10.2337/dc11-2103
Morisky DE, Green LW, Levine DM Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74.
Kim MT, Hill MN, Bone LR, Levine DM. Development and testing of the hill-bone compliance to high blood pressure therapy scale. Prog Cardiovasc Nurs. 2010;15:90–6.
Procidano ME, Heller K. Measures of perceived social support from friends and from family: three validation studies. Am J Community Psychol. 1983;11:1–24.
Muthuki EW, Nyamu DG, Karimi PN, Bosire KO Predictors of non-adherence to antihypertensive therapy in a rural health facility in Kenya. African J Pharmacol Ther. 2020 30;9.
Calderón-Larrañaga A, Diaz E, Poblador-Plou B, Gimeno-Feliu LA, Abad-Díez JM, Prados-Torres A. Non-adherence to antihypertensive medication: the role of mental and physical comorbidity. Int J Cardiol. 2016;207:310–6.
Tedla YG, Bautista LE Drug side effect symptoms and adherence to antihypertensive medication. Am J Hypertens. 2016;29:772–9.
Maddalena V, Cicero AFG, Maria Grazia P, Ada D, Eugenio C, Enrico S, et al. A prospective evaluation of persistence on antihypertensive treatment with different antihypertensive drugs in clinical practice. Vasc Health Risk Manag. 2007;3:999–1005.
Okumagba PO. Family support for the elderly in delta state of Nigeria. Studies on Home and Community. Science 2011;5:21–7. Apr 1
Miller TA, Dimatteo MR. Importance of family/social support and impact on adherence to diabetic therapy. Diabetes Metab Syndr Obes. 2013;6:421–6. https://doi.org/10.2147/DMSO.S36368
Lambert EV, Steyn K, Stender S, Everage N, Fourie JM. Cross-cultural validation of the hill-bone compliance to high blood pressure therapy scale in a South African, primary healthcare setting. Ethnicity Dis. 2006;16:286. Dec 1
Nashilongo MM, Singu B, Kalemeera F, Mubita M, Naikaku E, Baker A, et al. Assessing adherence to antihypertensive therapy in primary health care in Namibia: findings and implications. Cardiovascular drugs Ther. 2017;31:565–78. Dec
Denguir H, Yakdhane I, Gamra H, Zaabouti H. Validation of the Hill-Bone’s scale of compliance to high blood pressure therapy in his Tunisian version. Arch Cardiovascular Dis Suppl. 2019;11:101. Jan 1
Karademir M, Koseoglu IH, Vatansever K, Van Den Akker M. Validity and reliability of the Turkish version of the Hill–Bone compliance to high blood pressure therapy scale for use in primary health care settings. Eur J Gen Pract. 2009;15:207–11. Jan 1
Uchmanowicz I, Jankowska-Polańska B, Chudiak A, Szymańska-Chabowska A, Mazur G. Psychometric evaluation of the polish adaptation of the hill-bone compliance to high blood pressure therapy scale. BMC cardiovascular Disord. 2016;16:1–6.
Song Y, Han HR, Song HJ, Nam S, Nguyen T, Kim MT. Psychometric evaluation of hill-bone medication adherence subscale. Asian Nurs Res. 2011;5:183–8.
Pan J, Hu B, Wu L, Wang H, Lei T, Liu Z. The Translation, Reliability and Validity of the Chinese Version of the Hill–Bone Compliance to High Blood Pressure Therapy Scale in Adults with Hypertension. Patient preference adherence. 2020;14:1853.
Joshi MD, Ogola EN, Karari E. Adequacy of blood pressure control and level of adherence with antihypertensive therapy. East Afr Med J. 2009;86:499–506.
Ongaga, JK, 2019. Assessing Treatment Adherence In Hypertension Control Among Hypertensive Patients Post Health Education At Kenyatta National Hospital (Doctoral dissertation, University of Nairobi).
Wang Y, Lee J, Toh MP, Tang WE, Ko Y. Validity and reliability of a self‐reported measure of medication adherence in patients with type 2 diabetes mellitus in Singapore. Diabet Med. 2012;29:e338–44. Sep
Kumara WG, de Zoysa P, Balasuriya A, Fernando NF. Cross-cultural adaptation of the Morisky Green Levine medication adherence scale for use in patients with Ischaemic Heart Disease in Sri Lanka. J Postgrad Inst Med. 2020;7:1–7.
Val Jiménez A, Amorós Ballestero G, Martínez Visa P, Fernández Ferré ML, León SM. Descriptive study of patient compliance in pharmacologic antihypertensive treatment and validation of the Morisky and Green test. Aten Primaria. 1992;10:767–70.
Vural B, Acar ÖT, Topsever P, Filiz TM. Reliability and validity of Turkish version of modified Morisky scale. J Turkish Fam Phys. 2012;3:17–20.
Siqueira HH, Dalbem JS, Schiavini M, Silva PE, Costa TB, Leite PH, et al. Self-reported adherence among people with epilepsy in Brazil. Epilepsy Behav. 2020;103:106498. Feb 1
Yan LL, Gong E, Gu W, Turner EL, Gallis JA, Zhou Y, et al. Effectiveness of a primary care-based integrated mobile health intervention for stroke management in rural China (SINEMA): A cluster-randomized controlled trial. PLoS Med. 2021;18:e1003582 https://doi.org/10.1371/journal.pmed.1003582
Teshome DF, Demssie AF, Zeleke BM. Determinants of blood pressure control amongst hypertensive patients in Northwest Ethiopia. PloS One. 2018;13:e0196535. May 2
Tefera YG, Gebresillassie BM, Emiru YK, Yilma R, Hafiz F, Akalu H, et al. Diabetic health literacy and its association with glycemic control among adult patients with type 2 diabetes mellitus attending the outpatient clinic of a university hospital in Ethiopia. PloS One. 2020;15:e0231291.
Usman MN, Umar MD, Idris FA, Abdullahi Y. Medication adherence and its associated factors among hypertensive patients in a tertiary health facility in Minna, North central Nigeria. Archives of Clinical. Hypertension 2019;5:003–7.
Tandon S, Chew M, Eklu-Gadegbeku CK, Shermock KM, Morisky DE. Validation and psychometric properties of the 8-item Morisky Medication Adherence Scale (MMAS-8) in Type 2 diabetes patients in sub-Saharan Africa. Diabetes Res Clin Pract. 2015;110:129–36.
Kubo MN, Kayima JK, Were AJ, McLigeyo SO, Ogola EN. Factors associated with uncontrolled hypertension among renal transplant recipients attending nephrology clinics in Nairobi, Kenya. J Transpl. 2015;2015:746563.
Acknowledgements
We acknowledge our collaboration with the African Population and Health Research Center in Nairobi, Kenya. We acknowledge the contributions of our local collaborators in Kenya for their strong intellectual and logistic support during the fieldwork.
Funding
This research was funded by Duke Kunshan University.
Author information
Authors and Affiliations
Contributions
SX, SF, and LLY conceived the study design, drafted the study protocol, and obtained ethical approvals. CW and DW led the data collection and cleaning. SX and NP conducted data analysis, interpretation, and led the writing. NP, TO, MO, and XZ provided critical suggestions to the structure and writing of the manuscript. All authors approved the submission for the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was approved by the ethical committees of Duke Kunshan University, Africa Population Health Research Center (APHRC), and the Ethics and Scientific Research Committee of African Medical and Research Foundation (AMREF). Informed consent was obtained from each participant before they were involved in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xiong, S., Peoples, N., Østbye, T. et al. Family support and medication adherence among residents with hypertension in informal settlements of Nairobi, Kenya: a mixed-method study. J Hum Hypertens 37, 74–79 (2023). https://doi.org/10.1038/s41371-022-00656-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-022-00656-2