Abstract
The neutrophil to lymphocyte ratio (NTLR) and absolute lymphocyte count (ALC) recovery are prognostic across many cancers. We investigated whether NLTR predicts SBRT success or survival in a metastatic sarcoma cohort treated with SBRT from 2014 and 2020 (N = 42). Wilcox Signed Rank Test and Friedman Test compare NTLR changes with local failure vs. local control (N = 138 lesions). Cox analyses identified factors associated with overall survival. If local control was successful, NLTR change was not significant (p = 0.30). However, NLTR significantly changed in patients with local failure (p = 0.027). The multivariable Cox model demonstrated higher NLTR before SBRT was associated with worse overall survival (p = 0.002). The optimal NTLR cut point was 5 (Youden index: 0.418). One-year overall survival in SBRT metastatic sarcoma cohort was 47.6% (CI 34.3%–66.1%). Patients with an NTLR above 5 had a one-year overall survival of 37.7% (21.4%–66.3%); patients with an NTLR below 5 had a significantly improved overall survival of 63% (43.3%–91.6%, p = 0.014). Since NTLR at the time of SBRT was significantly associated with local control success and overall survival in metastatic sarcoma treated with SBRT, future efforts to reduce tumor inhibitory microenvironment factors and improve lymphocyte recovery should be investigated.
Similar content being viewed by others
Introduction
Sarcomas are a group of rare mesenchymal tumors that account for less than 1% of adult solid malignancies, but represent 21% of pediatric solid malignancies1. While the incidence is low relative to other malignancies, their biological heterogeneity and relative treatment resistance have made sarcomas challenging to treat2. Sarcomas can be divided into soft tissue sarcomas and primary bone tumors (e.g. osteosarcoma and Ewing sarcoma). Advances in sarcoma staging and therapy have led to survival improvements in both classes of sarcomas as well as improved risk-stratification3. For example, the 5-year survival in rhabdomyosarcoma has improved from around 50 to 70%4. Advancements in chemotherapy have improved prognosis in patients with low grade tumors. However, the success of surgery, radiotherapy, and chemotherapy capable of treating advanced metastatic disease is low5,6. Many patients present with high-grade histopathological features, and up to 25% of patients present with distant metastasis3,4. The current standard of care for most sarcomas is a combination of chemotherapy and local control that includes surgical resection and/or radiotherapy. Radiation is typically reserved for unresectable disease, when surgical morbidity could limit function, or when metastases are present7. There is an unmet need for more data to improve quality of cancer care and survival8.
Stereotactic body radiation (SBRT) is a relatively new advancement in radiotherapy that uses image guidance to precisely deliver high doses of ablative radiation in fewer fractions compared to traditional dose regimens. While contemporary indications for SBRT are rapidly expanding, it is most commonly used to treat inoperable early stage non-small cell lung cancer, prostate cancer, unresectable pancreatic cancer, pulmonary and hepatic metastases, and metastases to the spine or brain via a stereotactic radiosurgery approach9. Some sarcomas are relatively radioresistant and would theoretically benefit from the high biologically equivalent doses (BED) accompanying SBRT regimens. A multi-institutional phase II trial showed a 95% rate of lesion-specific local control at 6 months and improved progression free survival (PFS) and OS in patients with unresectable metastatic sarcoma treated with SBRT10. While local control with SBRT is encouraging, careful consideration of the therapeutic window must be applied as the higher fractional doses of radiation from SBRT increase the risk of developing late complications in normal tissue. A retrospective analysis of 31 patients found similarly high rates of local control and minimal toxicity, with only 1 out of 31 patients experiencing a late grade 3 radiation related toxicity11. SBRT has typically been reserved as salvage therapy for treatment resistant disease, so its role in primary treatment remains unknown, but has been investigated on a large cohort in a completed Children’s Oncology Group clinical trial in patients with metastatic Ewing sarcoma (NCT02306161).
Radiation therapy induces DNA damage through direct interaction and generation of reactive oxygen species. Tumor cells that survive the direct toxicity can express new antigens that may be recognized by the host immune system16. After radiation induced cell death of cancer cells, neutrophils and lymphocytes are actively recruited to the tumor site17. Given the interactions between radiation and the immune system, there may be a promising role for immunotherapy and radiotherapy synergism in the treatment of malignancy. SBRT, rather than conventional radiotherapy, may especially be synergistic with the patient’s immune system because it causes less lymphocyte depletion18. In pediatric osteosarcoma and Ewing sarcoma, improved absolute lymphocyte count (from either lymphocyte resilience or earlier recovery of lymphocytes post chemotherapy) has demonstrated survival benefits19,20,21,22. If the immune system is a critical part of the radiation efficacy, it would be helpful to have biometrics that help characterize the state of one’s immune system prior to SBRT.
Currently, there is no gold standard biomarker or biometric that can be used to assess how a patient’s immune system may respond to radiation. The NTLR is a promising candidate that has been correlated with survival in many malignancies including sarcoma before surgery23 and after chemotherapy24. Elevated pretreatment NTLR have been associated with poorer prognosis in both solid and hematological malignancies25,26,27,28. In soft tissue sarcoma, it has been associated with poorer survival and increased risk of distant metastasis29. Lymphopenia is also a prognostic factor in advanced sarcomas30.
While the literature suggests that NTLR will likely be prognostic across cancer diagnoses, it has not been studied in this population of metastatic sarcoma patients treated with SBRT. In this study, we show how NTLR changes over the SBRT treatment course and optimize a NTLR cutoff score to stratify patients with metastatic sarcoma into high and low risk survival groups. Furthermore, we demonstrate high NTLR was associated with a significantly worse prognosis and local failure after SBRT in patients with metastatic sarcoma.
Methods
Cohort
This study was approved by the Cleveland Clinic Institutional Review Board (IRB) as a single-institution registry of patients with metastatic sarcoma diagnosed between 2014 and 2020 treated with SBRT. After discussion of indications, risks, benefits, and alternatives, all patients or legal guardians provided written informed consent for SBRT as part of standard clinical care. No additional blood samples were obtained, therefore this was not considered an interventional study requiring additional informed consent for additional research blood samples as per IRB guidelines for a retrospective study. All research was performed in accordance with relevant guidelines and regulations. Included patients had histologically confirmed sarcoma including clear cell sarcoma, desmoplastic small round cell tumor, Ewing sarcoma, myxoid liposarcoma, osteosarcoma, rhabdomyosarcoma, undifferentiated pleomorphic small round blue cell sarcoma, and synovial sarcoma with at least one metastatic lesion treated with SBRT. CBC with differential data was collected by retrospective chart review at time points prior to SBRT, after SBRT, in follow-up, and at time of progression.
Treatment
Patients with histopathologic diagnosis of sarcoma were treated with SBRT defined as a fractional dose of ≥ 5 Gy delivered in five or fewer fractions to site(s) of metastatic disease. The intent of therapy -usually either definitive for oligo-metastatic disease or palliative for durable local control of metastases—as well as the specific dose and fractionation regimen were determined at the discretion of the treating physician. Technical details of SBRT technique based on lesion location have been described previously11,31.
Laboratory investigations
For each lesion treated with SBRT, complete blood count (CBC) data before and after SBRT treatment and in follow up were recorded. Since CBC is not routinely measured immediately before or after treatment, we included values within 3 months of treatment. We also recorded CBC parameters collected within 3 months after any local failure. We calculated a neutrophil to lymphocyte ratio by dividing absolute neutrophil count by absolute lymphocyte count. Friedman Test was used to assess changes in NTLR through SBRT therapy in failed lesions (comparing before SBRT vs after SBRT vs after local recurrence). Wilcox signed rank was used to compare NTLR in locally controlled lesions before SBRT versus after SBRT. These nonparametric statistical methods were chosen over linear regression methods due to the non-normality of the data and limited time points for comparison of the dependent variables.
Imaging
Patients received routine post-treatment imaging follow-up with CT, MRI, or PET to assess for local control. Local tumor failure was defined as recurrence of tumor at treatment site as determined by enlarged lesion on CT, MRI, or PET scan and/or interpretation of the radiologist and tumor board members.
Univariate and multivariate analysis of effects on survival
For each patient, the pretreatment CBC parameters within 3 months of SBRT was averaged and included with averaged values with other clinically relevant variables such as concurrent chemotherapy, Karnofsky Performance Status (KPS), and age in univariate Cox regression models to analyze their impact on overall survival. Overall survival was defined as time to death or last follow up from first treatment date. A selection criterion of p < 0.15 from the univariate model was used to determine the variables for the multivariate model. This was done because a small number of covariates was more appropriate for the small population size. Age, mean biologic equivalent dose across treatments, KPS, and NTLR were selected for the multivariate model.
A smoothed time-dependent ROC curve calibrated to 24 months of survival was used to generate an optimal cut point for NTLR32. Each patient’s NTLR was the average of their NTLR values prior to each SBRT treatment session. Optimal cut point to stratify patients into high and low risk groups was determined by the NTLR that maximized the Youden index, defined as the sum of sensitivity and specificity minus one. The Kaplan Meier method was used to calculate rates of overall survival. We compared the overall survival for these two groups using the log-rank test. All data were stored in a secure RedCap registry, and all analyses were performed in R (version 3.6.3)33.
Results
In total, there were 42 patients with 138 lesions that met criteria for the study as detailed in Table 1. The median age at diagnosis was 21 years with a range of 4 to 47 years. The median pretreatment NTLR for the cohort was 5.3. Twenty-five out of 42 patients had confirmed death, and the median clinical follow up time for surviving patients was 24 months and median imaging follow up time was 7.7 months.
Details about all individual lesions (n = 138) were recorded in our registry (Table 2). Most sarcomas treated with SBRT were osteosarcoma or Ewing sarcoma (84/138), and the remaining were soft tissue sarcomas. Lesions received 22.2–140 Gy with a median dose of 40 Gy (most common regimen was 8 Gy × 5 fractions) with biological equivalent dose from 66.7 Gy to 419 Gy with a median dose of 117 Gy, using an alpha/beta ratio of 3. Most patients receiving SBRT were also receiving concurrent systemic therapy (79/138, 57%). A total of 34/138 (25%) lesions experienced local recurrence. Figure 1 demonstrates the change in neutrophil to lymphocyte ratio over time. Median NTLR for sarcoma patients with controlled lesions before and after SBRT were very similar: 5.0 (IQR: 2.7 – 13.4) and 4.8 (IQR: 2.3 – 9.4), respectively. In patients experiencing local recurrence, the median NTLR for before and after SBRT was lower [3.3 (IQR: 2.2–5.0) and 3.5 (IQR: 3.0–6.1), respectively], and at time of local failure was higher [5.6 (IQR: 3.8 – 5.9)]. For locally controlled lesions, there was no significant difference in NTLR between the before and after SBRT groups (p = 0.30). For lesions that experienced recurrence, there was a significant difference in NTLR amongst the three groups (before, after SBRT and at recurrence: p = 0.027).
Table 3 Cox proportional hazards regression analyses for overall survival in our patient population. Higher mean radiotherapy BED (HR: 0.99; 95% CI: 0.98 to 1.00) and higher patient KPS (HR: 0.91; 95% CI: 0.87 to 0.96) were significant protective factors for overall survival whereas higher average pretreatment neutrophil count (HR: 1.24; 95% CI: 1.06 to 1.45) and higher average pretreatment NTLR (HR: 1.11; 95% CI: 1.04 to 1.19) were significantly associated with poorer survival in the univariate model. In the multivariable model, only worse KPS (HR: 0.91; 95% CI: 0.86 to 0.96) and higher average pretreatment NTLR (HR: 1.14; 95% CI: 1.05 to 1.24) were significantly associated with overall survival.
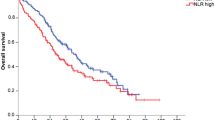
Fig. 2 demonstrates the time-dependent ROC curve calibrated to 24 months drawn to assess the optimal cutoff for stratifying high versus low risk groups based on NTLR. The optimal pre-SBRT NTLR cut point value was determined to be 5.033, which was rounded down to 5 and used for stratification into high risk and low risk groups. 24 patients (57%) were in the low risk NTLR category (< 5). Kaplan–Meier estimates for overall survival were calculated as shown in Fig. 3. Patients with a high NTLR (≥ 5) had significantly worse survival (p = 0.014). Patients with an NTLR ≥ 5 had a 1-year survival of 37.7% (95% CI: 21.4%–66.3%), while patients with an NTLR < 5 had a 1-year survival of 63% (95% CI: 43.3%–91.6%). 1-year survival in the entire cohort was 47.6% (95% CI: 34.3%–66.1%).
Kaplan–Meier curve comparing overall survival by NTLR ratio. Patients with an NTLR above 5 (red bottom line, n = 22) had a 1-year survival of 37.7% (95% CI: 21.4%–66.3%), while patients with an NTLR below 5 (teal, top line; n = 17) had a significantly improved 1- year survival of 63% (95% CI: 43.3%–91.6%, p = 0.014). 2-year survival was reduced to 18.8% (95% CI: 7.08% to 50.2%) for the high NTLR group and remained unchanged at 63% (95% CI: 43.3%–91.6%, p = 0.014) for the low NTLR group.
Discussion
Our study demonstrated for the first time a significant correlation between increased NTLR and poor local control and significantly worse overall survival in high-risk metastatic sarcoma patients undergoing SBRT. These findings are consistent with the prior observations in non-small cell lung cancer34. Interestingly, patients with lesions with more durable local control after SBRT correlated with a higher baseline NTLR compared to those with lesions that had local failure. However, NTLR in those with lesions that were locally controlled remained stable after therapy and survival seemed to plateau. Among patients experiencing local failure, the NTLR increased slightly after SBRT and then increased significantly after confirmed sarcoma recurrence. These findings suggest that a rising NTLR may be a more sensitive biometric of impending recurrence than absolute elevation of baseline NTLR.
However, absolute NTLR was associated with a significantly worse survival outcome in patients with metastatic sarcoma treated with SBRT. High pretreatment NTLR was associated with poor survival in the multivariable Cox proportional hazards model controlled for age, dose, and KPS. We also calculated a cutoff NTLR value of 5 to risk-stratify patients with metastatic sarcoma into high risk and low risk groups. An elevated NTLR could reflect either inflammation associated with advancing disease, impaired lymphocyte numbers or resilience (i.e. associated with a low ANC); either of these immune parameters would be expected to affect the tumor inhibitory microenvironment and be associated with local failure15.
In oropharyngeal cancer, an association between loco-regional recurrence and elevated NTLR has been observed35. In the setting of early stage NSCLC patients treated with SBRT, an elevated NTLR predicted for worse survival, but there was no correlation with local control34. This study did not assess changes in NTLR over time, but only evaluated pretreatment variables collected within 2 months of SBRT. Our analysis did not yield a statistical association between time to local recurrence and NTLR prior to treatment in a Kaplan–Meier model; however, our findings may be limited by the sample size of our study.
NTLR may become a useful biometric to study during immunotherapy with radiation, especially SBRT. The potential synergy between radiotherapy and immunotherapy is a growing area of research interest15. While radiation can result in temporary immunosuppression, it can assist the immune system long term by reducing tumor burden via direct cytotoxicity and exposing neoantigens to the immune system. The induction of neoantigens by radiotherapy and subsequent immunization against those neoantigens have been demonstrated in prostate cancer36. SBRT in particular has been demonstrated to stimulate the cellular immune response through enhanced T cell activity, increased antigen presentation, and release of inflammatory cytokines37. SBRT mediated damage of one tumor site can lead to systemic activation of the immune system against neoantigens present in other tumor sites leading to an abscopal effect, which has been demonstrated in some clinical settings37.
An elevated neutrophil count can be observed in chronic inflammatory conditions, including cancer. Tumor production of cytokines such as IL-1 and IL-6 can induce neutrophilia, with higher circulating neutrophil counts at baseline theoretically corresponding with an increased burden of disease38. It has also been shown that increased absolute neutrophil count (ANC) has the potential to suppress cytotoxic T lymphocyte function39. The relative lymphopenia associated with high NTLR may be associated with a poorer host immune response against tumor antigens and thus a poorer prognosis. T cells are necessary for checkpoint inhibition therapies and the anti-cancer cellular therapies using CAR-T and CAR-NK40. Taken together, an elevated NTLR suggests an increased burden of disease and an impaired immune response, both of which are poor prognostic factors. In the context of cancer therapy, we believe NTLR is a relevant biomarker for assessing potential immune responsiveness following radiotherapy and a useful metric for risk-stratification.
Our study has several limitations. Since this study is retrospective, it is difficult to ascertain the time course of exactly when SBRT alters the NTLR biometric. Given the disease rarity and relatively recent implementation of SBRT for treatment of metastatic sarcoma, the small sample size of the cohort still represents a large series of SBRT treated lesions11. Additionally, most sarcoma patients undergoing SBRT were heavily pre-treated with systemic therapies, a factor that likely affected the bone marrow and circulating lymphocytes. Although treatments such as granulocyte colony stimulating factor (G-CSF) could confound results, no one in our SBRT cohort received concurrent G-CSF during or immediately after SBRT.
In conclusion, high NTLR at the time of SBRT treatment was prognostic for significantly worse overall survival of patients undergoing SBRT for metastatic sarcoma. A rise in NTLR was also seen at time of local progression. The NTLR biometric may have implications for future sarcoma treatment, pre-and post-SBRT sarcoma surveillance, and future sarcoma and SBRT clinical trial design warranting further investigation.
Data availability
Anonymized datasets recorded and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SBRT:
-
Stereotactic Body Radiation Therapy
- NTLR:
-
Neutrophil to Lymphocyte Ratio
- CBC:
-
Complete Blood Count
- KM:
-
Kaplan–Meier
- HR:
-
Hazard Ratio
- KPS:
-
Karnofsky Performance Status
- BED:
-
Biological Effective Dose
- UV:
-
Univariate
- MR:
-
Multivariate
References
Burningham, Z., Hashibe, M., Spector, L. & Schiffman, J. D. The epidemiology of sarcoma. Clin. Sarcoma Res. 2(1), 14. https://doi.org/10.1186/2045-3329-2-14 (2012).
Skubitz, K. M. & D’Adamo, D. R. Sarcoma. Mayo. Clin. Proc. 82(11), 1409–1432. https://doi.org/10.4065/82.11.1409 (2007).
Bosma, S. E. et al. Easy-to-use clinical tool for survival estimation in Ewing sarcoma at diagnosis and after surgery. Sci. Rep. 9(1), 11000. https://doi.org/10.1038/s41598-019-46721-8 (2019).
Williams, R. F., Fernandez-Pineda, I. & Gosain, A. Pediatric sarcomas. Surg. Clin. North Am. 96(5), 1107–1125. https://doi.org/10.1016/j.suc.2016.05.012 (2016).
Oyama, R. et al. Generation of novel patient-derived CIC- DUX4 sarcoma xenografts and cell lines. Sci. Rep. 7(1), 4712. https://doi.org/10.1038/s41598-017-04967-0 (2017).
Subbiah, V. et al. Evaluation of novel targeted therapies in aggressive biology sarcoma patients after progression from US FDA approved therapies. Sci. Rep. 6, 35448. https://doi.org/10.1038/srep35448 (2016).
Sangkhathat, S. Current management of pediatric soft tissue sarcomas. World J. Clin. Pediatr. 4(4), 94–105. https://doi.org/10.5409/wjcp.v4.i4.94 (2015).
Subbiah, V. The next generation of evidence-based medicine. Nat. Med. 29(1), 49–58. https://doi.org/10.1038/s41591-022-02160-z (2023).
Chang, B. K. & Timmerman, R. D. Stereotactic body radiation therapy: A comprehensive review. Am. J. Clin. Oncol. 30(6), 637–644. https://doi.org/10.1097/COC.0b013e3180ca7cb1 (2007).
El-Bared, N., Wong, P. & Wang, D. Soft tissue sarcoma and radiation therapy advances, impact on toxicity. Curr. Treat. Options Oncol. 16(5), 19. https://doi.org/10.1007/s11864-015-0335-7 (2015).
Parsai, S. et al. Multiple site SBRT in pediatric, adolescent, and young adult patients with recurrent and/or metastatic sarcoma. Am. J. Clin. Oncol. 44(3), 126–130. https://doi.org/10.1097/coc.0000000000000794 (2021).
Gonzalez, H., Hagerling, C. & Werb, Z. Roles of the immune system in cancer: From tumor initiation to metastatic progression. Genes Dev. 32(19–20), 1267–1284. https://doi.org/10.1101/gad.314617.118 (2018).
Havel, J. J., Chowell, D. & Chan, T. A. The evolving landscape of biomarkers for checkpoint inhibitor immunotherapy. Nat. Rev. Cancer 19(3), 133–150. https://doi.org/10.1038/s41568-019-0116-x (2019).
Rizvi, N. A. et al. Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science 348(6230), 124–8. https://doi.org/10.1126/science.aaa1348 (2015).
Sellars, M. C., Wu, C. J. & Fritsch, E. F. Cancer vaccines: Building a bridge over troubled waters. Cell 185(15), 2770–2788. https://doi.org/10.1016/j.cell.2022.06.035 (2022).
Park, B., Yee, C. & Lee, K. M. The effect of radiation on the immune response to cancers. Int. J. Mol. Sci. 15(1), 927–943. https://doi.org/10.3390/ijms15010927 (2014).
McKelvey, K. J., Hudson, A. L., Back, M., Eade, T. & Diakos, C. I. Radiation, inflammation and the immune response in cancer. Mamm. Genome. 29(11–12), 843–865. https://doi.org/10.1007/s00335-018-9777-0 (2018).
Wild, A. T. et al. Lymphocyte-sparing effect of stereotactic body radiation therapy in patients with unresectable pancreatic cancer. Int. J. Radiat. Oncol. Biol. Phys. 94(3), 571–579. https://doi.org/10.1016/j.ijrobp.2015.11.026 (2016).
Moore, C. et al. Prognostic significance of early lymphocyte recovery in pediatric osteosarcoma. Pediatr Blood Cancer 55(6), 1096–1102. https://doi.org/10.1002/pbc.22673 (2010).
Anderson, P. Predicting and facilitating survival of pediatric cancer patients: The ALC story. Pediatr. Blood Cancer 55(6), 1041–1042. https://doi.org/10.1002/pbc.22715 (2010).
De Angulo, G. et al. Early lymphocyte recovery as a prognostic indicator for high-risk Ewing sarcoma. J. Pediatr. Hematol. Oncol. 29(1), 48–52. https://doi.org/10.1097/MPH.0b013e31802d3e3e (2007).
DuBois, S. G., Elterman, K. & Grier, H. E. Early lymphocyte recovery in Ewing sarcoma. J. Pediatr. Hematol. Oncol. 29(5), 351–352. https://doi.org/10.1097/MPH.0b013e3180590627 (2007).
Idowu, O. K., Ding, Q., Taktak, A. F., Chandrasekar, C. R. & Yin, Q. Clinical implication of pretreatment neutrophil to lymphocyte ratio in soft tissue sarcoma. Biomarkers 17(6), 539–544. https://doi.org/10.3109/1354750X.2012.699554 (2012).
Skubitz, K. M., Domingo-Musibay, E., Lindgren, B. R. & Cheng, E. Y. Prospective trial of neutrophil/lymphocyte ratio and other blood counts as biomarkers of survival among patients with high-grade soft tissue sarcomas treated with pegylated liposomal doxorubicin and ifosfamide. Cancers Basel 14(14), 3419. https://doi.org/10.3390/cancers14143419 (2022).
Gago-Dominguez, M. et al. Neutrophil to lymphocyte ratio and breast cancer risk: analysis by subtype and potential interactions. Sci. Rep. 10(1), 13203. https://doi.org/10.1038/s41598-020-70077-z (2020).
Guan, Y. et al. Revealing the prognostic landscape of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in metastatic castration-resistant prostate cancer patients treated with abiraterone or enzalutamide: A meta-analysis. Prostate Cancer Prostatic Dis. 23(2), 220–231. https://doi.org/10.1038/s41391-020-0209-3 (2020).
Sebastian, N. et al. Pre-treatment neutrophil-lymphocyte ratio is associated with overall mortality in localized non-small cell lung cancer treated with stereotactic body radiotherapy. Radiother. Oncol. 134, 151–157. https://doi.org/10.1016/j.radonc.2019.01.032 (2019).
Porrata, L. F. et al. Peripheral blood absolute lymphocyte/monocyte ratio recovery during ABVD treatment cycles predicts clinical outcomes in classical Hodgkin lymphoma. Blood Cancer J. 3(4), e110. https://doi.org/10.1038/bcj.2013.8 (2013).
Chan, J. Y. et al. Biological significance and prognostic relevance of peripheral blood neutrophil-to-lymphocyte ratio in soft tissue sarcoma. Sci. Rep. 8(1), 11959. https://doi.org/10.1038/s41598-018-30442-5 (2018).
Ray-Coquard, I. et al. Lymphopenia as a prognostic factor for overall survival in advanced carcinomas, sarcomas, and lymphomas. Cancer Res. 69(13), 5383–5391. https://doi.org/10.1158/0008-5472.CAN-08-3845 (2009).
Parsai, S. et al. Spine radiosurgery in adolescents and young adults: early outcomes and toxicity in patients with metastatic Ewing sarcoma and osteosarcoma. J. Neurosurg. Spine 29, 1–8. https://doi.org/10.3171/2019.9.SPINE19377 (2019).
Beyene, K. M. & El Ghouch, A. Smoothed time-dependent receiver operating characteristic curve for right censored survival data. Stat. Med. 39(24), 3373–3396. https://doi.org/10.1002/sim.8671 (2020).
R Development Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2017.
Shaverdian, N. et al. Pretreatment immune parameters predict for overall survival and toxicity in early-stage non-small-cell lung cancer patients treated with stereotactic body radiation therapy. Clin. Lung Cancer 17(1), 39–46. https://doi.org/10.1016/j.cllc.2015.07.007 (2016).
Young, C. A. et al. The prognostic role of the neutrophil-to-lymphocyte ratio in oropharyngeal carcinoma treated with chemoradiotherapy. Clin. Med. Insights Oncol. 8, 81–86. https://doi.org/10.4137/cmo.S15476 (2014).
Nesslinger, N. J. et al. Standard treatments induce antigen-specific immune responses in prostate cancer. Clin. Cancer Res. 13(5), 1493–1502. https://doi.org/10.1158/1078-0432.Ccr-06-1772 (2007).
Popp, I., Grosu, A. L., Niedermann, G. & Duda, D. G. Immune modulation by hypofractionated stereotactic radiation therapy: Therapeutic implications. Radiother. Oncol. 120(2), 185–194. https://doi.org/10.1016/j.radonc.2016.07.013 (2016).
Rosales, C. Neutrophil: A cell with many roles in inflammation or several cell types?. Rev. Front. Physiol. 9(113), 113. https://doi.org/10.3389/fphys.2018.00113 (2018).
Petrie, H. T., Klassen, L. W. & Kay, H. D. Inhibition of human cytotoxic T lymphocyte activity in vitro by autologous peripheral blood granulocytes. J. Immunol. 134(1), 230–234 (1985).
Basar, R., Daher, M. & Rezvani, K. Next-generation cell therapies: The emerging role of CAR-NK cells. Blood Adv. 4(22), 5868–5876. https://doi.org/10.1182/bloodadvances.2020002547 (2020).
Acknowledgements
The authors appreciate efforts of care coordinators in Pediatric Oncology (Shauna Sartoski and Alyssa Bauer) to assist pediatric and young adult patients getting SBRT. We also acknowledge generous support from The Cleveland Clinic Sarcoma program, Velosano, and the Little Warriors Foundation. Additionally, we acknowledge support from NIH grant R37 CA244613, NIH grant U54 (Radiation Oncology Biology Integration Network), and the American Cancer Society through their Research Scholar Grant.
Author information
Authors and Affiliations
Contributions
Conception and design: M.E., S.T., P.S., B.J., H.A.; Data collection: M.E. S.E., S.T., P.S., H.A., S.J.G., C.T., C.S., A.L., A.P.M., Z.S., T.M., T.S., J.S., Q.P., M.A.; Data analysis and interpretation: M.E. S.E., R.C., S.T., H.A.; Manuscript writing: M.E.S.E., S.T., H.A., A.P.M.; Final approval of manuscript: All Authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Somasundaram, E., Anderson, P.M., Smile, T.D. et al. Neutrophil to lymphocyte ratio (NTLR) predicts local control and overall survival after stereotactic body radiotherapy (SBRT) in metastatic sarcoma. Sci Rep 13, 19256 (2023). https://doi.org/10.1038/s41598-023-46476-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-46476-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.