Abstract
Neurological manifestations of coronavirus disease 2019 (COVID-19) have been frequently described. In this prospective study of hospitalized COVID-19 patients without a history of neurological conditions, we aimed to analyze their prevalence and prognostic value based on established, standardized and objective methods. Patients were investigated using a multimodal electrophysiological approach, accompanied by neuropsychological and neurological examinations. Prevalence rates of central (CNS) and peripheral (PNS) nervous system affections were calculated and the relationship between neurological affections and mortality was analyzed using Firth logistic regression models. 184 patients without a history of neurological diseases could be enrolled. High rates of PNS affections were observed (66% of 138 patients receiving electrophysiological PNS examination). CNS affections were less common but still highly prevalent (33% of 139 examined patients). 63% of patients who underwent neuropsychological testing (n = 155) presented cognitive impairment. Logistic regression models revealed pathology in somatosensory evoked potentials as an independent risk factor of mortality (Odds Ratio: 6.10 [1.01–65.13], p = 0.049). We conclude that hospitalized patients with moderate to severe COVID-19 display high rates of PNS and CNS affection, which can be objectively assessed by electrophysiological examination. Electrophysiological assessment may have a prognostic value and could thus be helpful to identify patients at risk for deterioration.
Similar content being viewed by others
Introduction
Since the first outbreak of coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), affections of the human central (CNS) and peripheral nervous system (PNS) have been repeatedly described. The most frequently encountered neurological manifestations are fatigue, myalgia, taste and/or smell impairment and headache1.
A recent meta-analysis reported at least one neurological manifestation in one-third of patients with COVID-19 and an association with mortality in patients ≥ 60 years1. In line with this, an individual patient data (IPD) meta-analysis on hospitalized COVID-19 patients with neurological complications revealed that these patients were more likely to die within 30 days than hospitalized COVID-19 patients in general2. Importantly, neurological complications may not only manifest as overt symptoms, but also as subtle presentations3.
However, some studies included patients with preexisting neurological conditions4,5,6,7,8, did not report how previous neurological diseases were handled9, or only included patients with neurological affections2. Therefore, conclusions regarding SARS-CoV-2 specific effects are limited. Further, definition of and diagnostic criteria for neurological manifestations in COVID-19 oftentimes remain unreported and are not standardized1. Lastly, some studies rely on patient-reported outcomes only10,11. Electrophysiological characterization of both PNS and CNS function to objectify the reported symptoms and to detect subclinical symptoms in larger cohorts is still missing.
Evoked potentials and nerve conduction studies (NCS) including the blink reflex (BR) as a marker of brainstem function and the sympathetic skin response (SSR) as a marker of autonomous nervous system (ANS) function represent well-established, non-invasive methods to objectively investigate neuronal function. In a case series we found that these measures, as well as neuropsychological outcomes, can be markedly impaired during and directly after COVID-1912. In line with this, a recent study found subclinical abnormalities in NCS two to six months after pneumonia due to SARS-CoV-213.
In this study, we extended our multimodal approach to a large cohort of previously neurologically healthy hospitalized patients with COVID-19, which we investigated during the acute infection. Early identification of critical patients is crucial to guide clinical decision making and allocation of limited resources. We therefore aimed to analyze the extent and prevalence of neurological deficits using established, standardized and objective methods and to identify potential biomarkers of prognostic value. Since there is no research on the prevalence rates of CNS and PNS affections based on standard electrophysiological assessments (EA) yet, analyses were of exploratory nature.
Methods
Participants
Hospitalized patients with COVID-19 were recruited between May 2020 and March 2022 at the University Hospital Duesseldorf, Germany, to participate in the PROGNOSE study. Inclusion criterion was an ongoing infection with SARS-CoV-2, confirmed by real-time reverse-transcription polymerase chain reaction. Here, we only focus on patients with symptoms of COVID-19. Exclusion criteria were: (1) pregnancy, (2) previous or ongoing neurological conditions with possible influence on the study readouts, and (3) age < 18 years.
Patients with neurological preconditions that only affected some assessments (e.g., dementia) were excluded only for confounded investigations (e.g., neuropsychology). Study participation did not influence the clinical treatment, which was performed according to the best medical care available at the time of examination.
Ethics approval and consent to participate
The study was approved by the ethical committee of the medical faculty of the Heinrich-Heine-University Düsseldorf (Study-Number 2020-979) and carried out in accordance with the declaration of Helsinki. Informed written consent was provided prior to participation by the patient or, in case of inability to consent, by relatives and post-hoc by the patient.
Neurological and clinical assessment and laboratory markers
Since there is no COVID-19 specific score for classification of neurological symptoms and disability yet, the following established disability scores were adjusted to the COVID-19 pathology and determined by neurological examination: (1) Expanded Disability Status Scale (EDSS) based on the following Functional Systems (FS): brainstem, pyramidal, cerebral, cerebellar, sensory14, (2) Modified Rankin Scale15, (3) INCAT disability score16, (4) Barthel Index17. All scores are described in detail in the Supplementary Methods. The clinical status of the patient at the time of examination was assessed by the WHO clinical progression scale (WHO score), documenting disease severity from 0 (uninfected) to 10 (dead)18.
Blood samples were collected as part of the clinical routine during or shortly after admission, and the following laboratory markers were analyzed: C-reactive protein, urea, lymphocytes, procalcitonin, troponin, ferritin, lactate dehydrogenase, and D-dimers. At admission, the level of consciousness was assessed by the Glasgow Coma Scale19.
Neuropsychological assessment
The neuropsychological assessment consisted of the Montreal Cognitive Assessment (MoCA, version 7)20 as a screening battery for mild cognitive impairment and the Symbol Digit Modalities Test (SDMT)21 as a measure of information processing speed (IPS). Delirium was assessed using the 4 ‘A’s Test22 and Confusion Assessment Method for use in intensive care unit (ICU) patients23. MoCA and SDMT scores were transformed into demographically adjusted z-scores (see Supplementary Methods)24,25. In case of language barriers, neuropsychological assessment was limited to the SDMT or cancelled.
Electrophysiological assessment
The EA included NCS of the right tibial, sural and ulnar nerves, BR of the bilateral ocular orbicular muscle, SSR, and motor and somatosensory evoked potentials (MEP/SSEP) to/from all extremities. If the right side could not be assessed in the NCS (e.g., due to an intravenous line) or patients specifically reported symptoms on the left side requiring clinical examination, the left side was measured instead. MEP were recorded from bilateral tibialis anterior and 1st dorsal interosseus muscles. Supramaximal stimuli of bilateral medial and tibial nerves with at least 200 averages were used for SSEP, recording responses at the poplitea/Erb’s point, C5/T12 and Cp/Cz, respectively.
All measurements were carried out with a Nihon Kohden Neuropack X1 (Nihon Kohden Corporation, Tokyo, Japan) and Ag–AgCl surface electrodes (28 × 20 mm [MEP, SSR, and NCS]/ 20 × 15 mm [BR], Ambu, Ballerup, Denmark) and subdermal needle electrodes (SSEP/12 × 0.4 mm, Ambu, Ballerup, Denmark) were used for recordings. MEP were evoked by single pulse transcranial magnetic stimulation via a standard circular coil (90 mm outer diameter, The Magstim Company Ltd., Whitland, UK) connected to a Magstim 200 (The Magstim Company Ltd., Whitland, UK).
All EA were evaluated based on the clinical norms of the University Hospital Düsseldorf (Supplementary Tables S1–S5) and affections were classified into PNS, CNS, and ANS (multiple selection possible).
PNS affection was defined as any abnormality in the NCS (distal motor latency [DML], F-wave latency, compound muscle action potential [CMAP], sensory nerve action potential [SNAP], motor/sensory conduction velocity [mCV/sCV]) or the following abnormalities in the BR: (1) R1, iR2 and cR2 exclusively delayed on one side, or (2) R1 and iR2 delayed on one side and cR2 delayed on the other side. Axonal pathology was defined as a reduction in CMAP/SNAP amplitude, whereas demyelinating pathology was defined as a reduction in mCV/sCV or prolongation of DML or F-wave latency.
CNS affection was defined as (1) reduced N20 and/or P40 in the SSEP and normal peripheral response (defined as normal N10 in the SSEP, if available, or as normal latency measured in the NCS), (2) increased central motor conduction time (CMCT) in the MEP, (3) increased cortical latency in the MEP and normal peripheral response (measured in the NCS), (4) delayed R1 exclusively on one side in the BR, (5) delayed R2 exclusively on one side in the BR, 6) delayed R2 on both sides in the BR.
ANS affection was defined as pathological latencies in the SSR. Please refer to Supplementary Tables S1–S5 for applied cut-offs for each assessment.
Statistical analyses
Since the primary goal of the study was to investigate the unknown prevalence of (sub)clinical neurological affections, sample size was based on the number of patients willing to participate rather than statistical power calculation.
Clinical and demographic differences between surviving and deceased patients were assessed by Fisher’s exact test for categorical data and Mann–Whitney-U-test for continuous variables with non-normal distribution. P-values < 0.05 were considered significant. Prevalence rates were calculated using crosstabulations (1) considering all patients, including those with missing data, and (2) including only patients who underwent the respective assessments. Exploratively, statistical analyses were repeated excluding patients with diabetes mellitus (DM) as the most prevalent potential confounding factor.
The relationship between abnormalities in the EA and death was assessed by Firth logistic regression models. Firth logistic regression models were also calculated for all predictive parameters for the patient’s outcome of the 4C Deterioration Model and 4C Mortality Score26,27, as well as for the WHO score18, sedation, and the Modified Rankin Scale15. Due to the exploratory nature of the study, we did not correct for multiple testing.
To avoid confounding influences of sedation, regression analyses were repeated excluding sedated patients. Further, age and sex were included as potentially confounding factors. All analyses were repeated using the raw data of the EA as independent factor.
Probabilities of mortality were estimated using Kaplan–Meier analysis and Cox proportional hazard models were used to compare the probability of death between patients with and without pathological findings in the EA. Again, analyses were conducted separately for the whole sample and, subsequently, only for non-sedated patients.
All analyses were conducted using R Studio (version 2021.09.1 + 372), except for Kaplan–Meier analysis and Cox proportional hazard models which were conducted using IBM SPSS Statistics (version 26).
Results
Sample characteristics
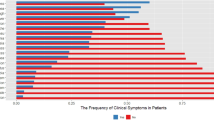
Out of 1243 SARS-CoV-2 positive patients who were assessed for eligibility at the University Hospital Duesseldorf, 184 with definite COVID-19 and without a history of neurological diseases could be enrolled in the study (Fig. 1). Descriptive statistics are presented in Table 1 and individual data for each assessment are provided in Supplementary Figure S1. Compared to surviving patients, patients who died were significantly older, treated longer in the hospital, required ICU treatment and oxygen therapy more frequently, were more often comatose and more severely ill at the time of examination, as indicated by significantly higher WHO scores18. On average, they were also examined two days later after admission. Oxygen saturation and lymphocyte counts at admission were higher in survivors, while urea, C-reactive protein, procalcitonin, lactate dehydrogenase, and D-dimer concentrations were higher in the deceased group. More deceased than surviving patients suffered from the original virus variant.
Prevalence rates of abnormalities
Table 2 displays the neurological characteristics of all patients. PNS pathology occurred in a majority (66%) of all patients that underwent EA with slightly more sensible than motor affections (sensible: 59%, motor: 54%) of both axonal and demyelinating nature (axonal: 58%, demyelinating; 58%). Excluding patients with DM, prevalence rates of PNS affection remained equally high (64%, Supplementary Figure S2). Also taking into account patients who did not receive EA, the prevalence rate remained as high as 50%.
CNS pathology occurred less frequently but was still highly prevalent, affecting 33% of patients undergoing CNS assessment. Including patients who did not receive CNS testing, the prevalence rate was 25%.
ANS pathology occurred least frequently, affecting 25% of those electrophysiologically examined and 16% of the total sample.
Eight patients were comatose, impeding most neurological investigations. In the remaining patients, brainstem and pyramidal functions were most frequently affected. Half of those patients undergoing neurological and electrophysiological assessment presented with subclinical manifestations, which were detectable in the EA but not by the neurological examination (EDSS < 1). Further, most of the clinical symptoms detected in the neurological examination did not have a corresponding finding in the EA. This was also true investigating the single FS separately, with exception of the tests for coordination of the cerebellar FS, in which most clinical symptoms were associated with pathology in the NCS.
Figure 2 illustrates the number of pathological findings in the different EA in relation to the number of enrolled participants and conducted EAs. It shows that EA revealed pathological findings in most patients and that most affections of the CNS and ANS were accompanied by PNS affection.
Frequencies of different nervous system affections in relation to each other, conducted electrophysiological assessments, and enrolled patients. This figure illustrates the results of the electrophysiological assessment. It shows the number of patients with pathological findings in the central, peripheral and autonomous nervous system in relation to each other, the number of conducted electrophysiological assessments, and the number of enrolled participants. The sizes of the ellipses are proportional to the number of affected participants and were estimated by the R package ‘eulerr’42. EA, Electrophysiological assessment; PNS, Peripheral nervous system; ANS, Autonomous nervous system; Patho, Any pathology in the EA.
Prevalence rates of abnormalities in the neuropsychological assessments
53% of the total sample and 63% of those undergoing cognitive assessment presented with impairment in the SDMT, MoCA or both (Table 2). No delirium was detected. Of those presenting with cognitive deficits, 36% were impaired in both tests, whereas 35% and 29% showed signs of impairment exclusively in the MoCA and SDMT, respectively.
Association between electrophysiological readouts and death
Among patients who underwent EA of the ANS, 55% of the deceased patients had pathological findings, compared to 28% of those surviving. Independent of the outcome, peripheral pathology occurred in most patients who underwent EA with slightly more affections in the group that passed away (75%Death, 65%Survival). CNS affections were equally distributed in 50% of the deceased and 46% of the surviving patients.
Separately analyzing the single assessments, the BR revealed pathological findings in the majority of deceased patients (67%), compared to 14% in survivors. The SSEP revealed a similar pattern with 75% and 31% pathological findings in the deceased and surviving group, respectively. NCS revealed high rates of affection in both groups (90%Death, 67%Survival) whereas the MEP was less frequently abnormal (57%Death, 32%Survival). Absolute frequencies of pathologies in the EA for both groups are presented in Supplementary Figure S2.
Logistic regression revealed independent associations of abnormalities in the BR, SSR, and SSEP with mortality. Odds ratios are presented in Fig. 3 and Table 3. Investigating the clinical status, sedation, and WHO scores ≥ 7 and ≥ 6 were strongly associated with death. Sedation is known to influence BR and SSR but not SSEP and, in line with this, the association with mortality lost significance for the BR and SSR when sedated patients were excluded, but remained significant for the SSEP. After including age and sex as covariates, no effects remained significant in unsedated patients (Supplementary Table 6).
Odds ratio of mortality. This figure shows the odds ratios of mortality (with 95% confidence interval) on the log scale. All scores refer to the time of examination if not indicated otherwise. Number of comorbidities were defined according to the extended Charlson comorbidity index26. No results for the Glasgow coma scale19 at admission are displayed because all patients achieved the highest possible score. See Table 3 for detailed statistics. CI, Confidence interval; adm, Score refers to the time of admission to the hospital; MRS, Modified Rankin Scale; WHO score, WHO clinical progression scale; PNS, Peripheral nervous system; CNS, Central nervous system; NCS, Nerve conduction studies; MEP, Motor evoked potentials; SSEP, Somatosensory evoked potentials; SSR, Sympathetic skin response; BR, Blink reflex.
Analysis of the raw data revealed significant associations between death and the N20 (mean of both sides of the body) as well as iR2 (left and right) not only in the total sample but also in the subsample of unsedated patients (Supplementary Figure S3). Excluding patients with a history of DM (n = 39) resulted in a subsample of only six deceased patients and associations of abnormalities in the EA with mortality lost significance (Supplementary Figure S4). However, the N20 and iR2 were still associated with death (Supplementary Figure S5).
Among the parameters already described to be predictive of the patient’s outcome26,27, significant associations with mortality were confirmed for oxygen saturation and need of oxygen therapy, C-Reactive protein, and age. However, the association of need of oxygen therapy lost significance after controlling for age and sex.
The Kaplan–Meier-Curves, Hazard Ratios and the number of remaining patients under observation for all EAs from the time of assessment until discharge are presented in Supplementary Figure S6, illustrating that death mostly occurred within 30 days of hospitalization.
Time-trend of pathologies
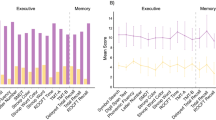
Due to the limited sample size, it was impossible to analyze the effects of factors such as virus variant, immunization status and treatment option on the presence of neurological affections. Although we could not statistically control for these factors during our analyses, the number of patients with CNS, PNS and cognitive affections in relation to the number of included patients and the number of vaccinated patients are presented in Fig. 4.
Time-trend of neurological manifestations. This figure shows the prevalence rates of central nervous system affection (red), peripheral nervous system affection (blue) and cognitive impairment (black) over time. The rate of vaccinated patients (dotted) and the predominant virus variant for each period are presented as well. Part A displays the prevalence rates based on the number of all included patients (N = 184). Part B displays the prevalence rates based only on the number of patients receiving the corresponding assessment(s). E.g., prevalence of cognitive impairment is based only on patients participating in neuropsychological assessment (N = 157). Please refer to Table 2 for overall prevalence rates and number of assessed patients. PNS, Peripheral nervous system; CNS, Central nervous system.
Discussion
We extensively investigated neurological function and cognitive performance in a large population of hospitalized patients with moderate to severe COVID-19 and report high prevalence rates of CNS and especially PNS affections during the acute phase of the infection in this cohort. In line with previous studies28, we also report high rates of cognitive impairment. More than half of the patients presented with cognitive impairment, which was evitable in below average performance in the MoCA and/or reduced IPS.
We present a detailed neurological profile based on objective and standardized assessments, classifying not only clinical symptoms but also subclinical pathologies. Further, we provide information to help identify patients who may be at greater risk for complications and may benefit from more aggressive and earlier treatment. Not only high WHO scores18, reflecting respiratory failure, are associated with an increased risk of mortality but also SSEP pathology was identified as an independent risk factor. Although this effect lost statistical significance after controlling for age and sex, this could be of high value for patient care and possibly even of psychosocial and economic relevance.
In contrast to previous results29, PNS affections were more common than CNS affections. However, our estimates may be biased by patients with previously undiagnosed polyneuropathy (PNP), e.g. due to DM, alcohol consumption, malnutrition or other risk factors of PNP, as we only excluded patients with a known history of PNP. Importantly, prevalence of PNS affection remained stable when excluding patients with DM, suggesting that PNS pathology may indeed occur as a consequence of COVID-19. Our results are also in accordance with previous studies reporting high prevalence rates of (sub)clincal PNS affections, even in patients with mild COVID-1930 and the subacute state31. However, most previous studies did not exclude patients with neurological conditions prior to COVID-19, thereby potentially overestimating PNS pathologies. Our study on patients without previous neurological affections, therefore adds important value to the current literature on neurological affections in patients with COVID-19.
The major limitation of our study is the lack of a control group. Our study was designed to include hospitalized patients with pneumonias of other origins as a control group. However, in the context of diverse measures to prevent the spread of SARS-CoV-2, the incidence of other pneumonias was very low and due to the exclusion criterion of confounding neurological disorders we could only include 13 of 91 approached control patients. Precluding meaningful comparison, we chose not to include these patients in the analyses. Thus, the reported affections cannot be considered specific for COVID-19 and need to be interpreted in the context of other factors associated with neurological manifestations, such as ICU treatment. ICU treatment is well known to be associated with neurological manifestations such as critical illness polyneuropathy or myopathy (CIP/CIM), but prevalence rates are strongly influenced by the studied population, time of assessment, risk factors and diagnostic criteria32. Thus, comparison with the prevalence rates found in our cohort of COVID-19 patients is difficult.
In patients with acute respiratory distress syndrome (ARDS), prevalence of ICU-acquired weakness, summarizing both CIP and CIM, ranges from 36% at hospital discharge to 60% following sedation33,34. Importantly, prevalence of PNS pathology in our subgroup of ICU patients exceeds the highest rate in ARDS (85.7% considering all ICU patients/ 90% considering all ICU patients that underwent PNS assessment). Further, the majority of our participants was not treated in the ICU and median time of hospitalization was rather short (8 days). In line with this, a study comparing clinical and electrophysiological data of patients with ICU-acquired weakness between patients with COVID-19 and other diseases reported significantly more CIP in the COVID-19 cohort35. Based on findings of a retrospective cohort study comparing neurological and psychiatric manifestations after COVID-19 and other respiratory tract infections, we further believe that our reported rates are higher than what could be expected from other infections36. Nonetheless, studies comparing neurological manifestations in hospitalized COVID-19 patients with hospitalized SARS-CoV-2 negative patients are urgently needed and already underway.
At the time of study initiation, evidence regarding neurological manifestations in patients with COVID-19 was scarce and limited to case series, prohibiting power-calculation. Therefore, our study has to remain descriptive in nature and deductions are limited to our study population and center. However, our center is representative of hospitals treating patients with COVID-19 in Germany.
Patients were recruited regardless of subjective (neurological) symptoms. It’s possible that those with subjective neurological complaints were more inclined to participate in our study, potentially inflating the prevalence rates of neurological affections. Unfortunately, selection bias is a well-known limitation of clinical research due to the voluntary nature of study participation. To avoid further bias in our prevalence rates, we do not only report prevalence rates based on the number of patients who received assessment of CNS/PNS function but also based on the number of all included patients. While the former may overestimate the ‘true’ rate, the latter is rather conservative and probably an underestimation. We, therefore, believe that the ‘true’ rate falls between the two estimates.
Further limitations are the lack of neuro(psycho)logical or even electrophysiological evaluation prior to the infection and the lack of ambulatory patients, who could not be investigated due to quarantine measures. Additionally, neuropsychological testing may have been influenced by factors, such as anxiety and depression, potentially linked to the pandemic in general but also to the hospitalization with COVID-19. Indeed, there had been a small increase in mental health symptoms during the first months of the pandemic, which did, however, decline over time37. Looking at the time-trend, rates of cognitive impairment remained high throughout the course of the pandemic despite immunization, more treatment options, less fatal virus variants, and decreasing levels of mental health symptoms. This suggests, that cognitive impairment occurred independent of these factors in our cohort. However, cross-sectional neuropsychological assessments can only inform about the cognitive performance in a specific situation and timepoint, while longitudinal assessments are needed to inform about the persistence of deficits. Indeed, longitudinal studies have shown, that cognitive deficits may persist up to one year after the acute infection38,39,40.
Confounding factors such as immunization status and variable treatment may have influenced our predictive measures. Importantly, however, we controlled for the most important confounding factor, namely preexisting neurological conditions, by strictly excluding patients with a previous history of neurological disorders. Even though this criterion drastically reduced our final cohort, this was the best procedure to prohibit further selection bias and to ensure that neurological affections detected in this study were unlikely present prior to COVID-19. Exploratory, we also controlled for age and sex in our predictive analyses. As expected, based on the well-known influence of age and sex, including these factors, dramatically decreased the predictive value of the neurological affections.
It would be interesting to compare the prevalence rate and prognostic value of the reported affections for different SARS-CoV-2 variants. The severity rates have decreased over time as a result of mutations of the virus, vaccinations and novel treatment options. With the limited number of cases of each variant in this study, it was impossible to control for these strong confounding factors to compare the effect of different SARS-CoV-2 variants, immunization status and treatment. However, we provide a graphical illustration of the number of patients with CNS, PNS and cognitive affections in relation to the number of included patients and the number of vaccinated patients. Although entirely descriptive, it suggests that neurological affections occurred less frequently during the course of the pandemic. Larger studies are needed to investigate the relevance of the virus variant, immunization status, treatment, and other factors.
Future studies should also include neuroimaging data to increase sensitivity of detecting possible CNS affections that may not be revealed by electrophysiological and neurological examination. Further, the prognostic relevance of sensitive laboratory measures of brain injury (e.g. blood neurofilament light chain protein (NfL) as a marker of neuroaxonal damage and nervous system involvement)41 should be taken into account. In a recent IPD meta-analysis, NfL levels were not only elevated in hospitalized COVID-19 patients without major CNS manifestations but also associated with poor clinical outcomes3. Although further investigations are warranted, these results indicate that overt neurological symptoms may merely represent the surface manifestations of a more complex and multifaceted underlying issue.
In conclusion, we report high rates of CNS and PNS affection in a cohort of hospitalized patients with moderate to severe COVID-19 during the acute infection, objectively assessed by electrophysiological examination. While somatosensory affections may have an independent prognostic value for mortality in the acute phase, affections of the PNS seem to occur very frequently. EA, notably SSEP, may be helpful in the clinical routine to identify patients at high risk for unfavorable outcomes and to allocate limited resources for the management of post-COVID-19 sequelae.
Data availability
Deidentified participant data, a data dictionary, and informed consent forms (German only) will be made available on request by researchers working in related fields three months after publication. Data will be provided by the corresponding author.
References
Misra, S. et al. Frequency of neurologic manifestations in COVID-19: A systematic review and meta-analysis. Neurology https://doi.org/10.1212/WNL.0000000000012930 (2021).
Singh, B. et al. Prognostic indicators and outcomes of hospitalised COVID-19 patients with neurological disease: An individual patient data meta-analysis. PLoS One 17(6), e0263595. https://doi.org/10.1371/journal.pone.0263595 (2022).
Abdelhak, A. et al. Prognostic performance of blood neurofilament light chain protein in hospitalized COVID-19 patients without major central nervous system manifestations: An individual participant data meta-analysis. J. Neurol. 270(7), 3315–3328. https://doi.org/10.1007/s00415-023-11768-1 (2023).
Bungenberg, J. et al. Long COVID-19: Objectifying most self-reported neurological symptoms. Ann. Clin. Transl. Neurol. https://doi.org/10.1002/acn3.51496 (2022).
Cervantes-Arslanian, A. M. et al. Neurologic manifestations of severe acute respiratory syndrome Coronavirus 2 infection in hospitalized patients during the first year of the COVID-19 pandemic. Crit. Care Explor. 4(4), e0686. https://doi.org/10.1097/CCE.0000000000000686 (2022).
Fleischer, M. et al. Observational cohort study of neurological involvement among patients with SARSCoV-2 infection. Ther. Adv. Neurol. Disord. 14, 1–14 (2021).
Haki, C., Demirci, H., Ayar, Y., Demir, C. & Caliskan, G. Neurological symptoms and diagnoses in patients hospitalized With COVID-19: Relationships with mortality. Neurologist 26(6), 237–243. https://doi.org/10.1097/NRL.0000000000000379 (2021).
Kleineberg, N. N. et al. Neurological symptoms and complications in predominantly hospitalized COVID-19 patients: Results of the European multinational Lean European Open Survey on SARS-Infected Patients (LEOSS). Eur. J. Neurol. 28(12), 3925–3937. https://doi.org/10.1111/ene.15072 (2021).
Mao, L. et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 77(6), 683–690. https://doi.org/10.1001/jamaneurol.2020.1127 (2020).
Kumar, J. et al. Long-term neurological impact of COVID-19. Cureus. 13(9), e18131. https://doi.org/10.7759/cureus.18131 (2021).
Goërtz, Y. M. J. et al. Persistent symptoms 3 months after a SARS-CoV-2 infection: The post-COVID-19 syndrome?. ERJ Open Res. https://doi.org/10.1183/23120541.00542-2020 (2020).
Groiss, S. J. et al. Prolonged neuropsychological deficits, central nervous system involvement, and brain stem affection after COVID-19-A case series. Front. Neurol. 11, 574004. https://doi.org/10.3389/fneur.2020.574004 (2020).
Koskderelioglu, A., Eskut, N., Ortan, P., Ozdemir, H. O. & Tosun, S. Visual evoked potential and nerve conduction study findings in patients recovered from COVID-19. Neurol. Sci. 43(4), 2285–2293. https://doi.org/10.1007/s10072-021-05816-9 (2022).
Kurtzke, J. F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 33(11), 1444–1452. https://doi.org/10.1212/wnl.33.11.1444 (1983).
van Swieten, J. C., Koudstaal, P. J., Visser, M. C., Schouten, H. J. & van Gijn, J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19(5), 604–607. https://doi.org/10.1161/01.STR.19.5.604 (1988).
Hughes, R. et al. Randomized controlled trial of intravenous immunoglobulin versus oral prednisolone in chronic inflammatory demyelinating polyradiculoneuropathy. Ann. Neurol. 50(2), 195–201. https://doi.org/10.1002/ana.1088 (2001).
Mahoney, F. I. & Barthel, D. W. Functional evaluation: The barthel index: A simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Md State Med. J. 14, 61–65 (1965).
Marshall, J. C. et al. A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect. Dis. 20(8), e192–e197. https://doi.org/10.1016/S1473-3099(20)30483-7 (2020).
Teasdale, G. & Jennett, B. Assessment of coma and impaired consciousness: A practical scale. The Lancet 304(7872), 81–83. https://doi.org/10.1016/S0140-6736(74)91639-0 (1974).
Nasreddine, Z. S. et al. The montreal cognitive assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 53(4), 695–699. https://doi.org/10.1111/j.1532-5415.2005.53221.x (2005).
Smith A. Symbol Digit Modalities Test (SDMT). (Western Psychological Services, 1982).
MacLullich A. The 4 'A's Test. Published October 30, 2014. Accessed July 7, 2022. www.the4at.com
Ely, E. W. et al. Evaluation of delirium in critically ill patients: Validation of the confusion assessment method for the intensive care unit (CAM-ICU). Crit. Care Med. 29(7), 1370 (2001).
Scherer, P., Baum, K., Bauer, H., Göhler, H. & Miltenburger, C. Normierung der brief repeatable battery of neuropsychological tests (BRB-N) für den deutschsprachigen Raum Anwendung bei schubförmig remittierenden und sekundär progredienten multiple-sklerose-patienten. Nervenarzt 75(10), 984–990. https://doi.org/10.1007/s00115-004-1729-0 (2004).
Thomann, A. E. et al. The montreal cognitive assessment: Normative data from a German-speaking cohort and comparison with international normative samples. J. Alzheimers Dis. 64(2), 643–655. https://doi.org/10.3233/JAD-180080 (2018).
Gupta, R. K. et al. Development and validation of the ISARIC 4C deterioration model for adults hospitalised with COVID-19: A prospective cohort study. The Lancet Respir. Med. 9(4), 349–359. https://doi.org/10.1016/S2213-2600(20)30559-2 (2021).
Knight, S. R. et al. Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO clinical characterisation protocol: Development and validation of the 4C mortality score. BMJ. 370, m3339. https://doi.org/10.1136/bmj.m3339 (2020).
Crivelli, L. et al. Changes in cognitive functioning after COVID-19: A systematic review and meta-analysis. Alzheimers Dement. https://doi.org/10.1002/alz.12644 (2022).
Guerrero, J. I. et al. Central and peripheral nervous system involvement by COVID-19: A systematic review of the pathophysiology, clinical manifestations, neuropathology, neuroimaging, electrophysiology, and cerebrospinal fluid findings. BMC Infect. Dis. 21(1), 515. https://doi.org/10.1186/s12879-021-06185-6 (2021).
Hanganu, A.-R. et al. Peripheral nervous system involvement associated with COVID-19. A systematic review of literature. PLoS One. 18(4), e0283827. https://doi.org/10.1371/journal.pone.0283827 (2023).
Taskiran-Sag, A. et al. Headache and cognitive disturbance correlate with ganglion cell layer thickness in patients who recovered from COVID-19. Clin. Neurol. Neurosurg. 217, 107263. https://doi.org/10.1016/j.clineuro.2022.107263 (2022).
Zink, W., Kollmar, R. & Schwab, S. Critical illness polyneuropathy and myopathy in the intensive care unit. Nat. Rev. Neurol. 5(7), 372–379. https://doi.org/10.1038/nrneurol.2009.75 (2009).
Fan, E. et al. Physical complications in acute lung injury survivors: A two-year longitudinal prospective study. Crit. Care Med. 42(4), 849–859. https://doi.org/10.1097/CCM.0000000000000040 (2014).
Bercker, S. et al. Critical illness polyneuropathy and myopathy in patients with acute respiratory distress syndrome. Crit. Care Med. 33(4), 711–715. https://doi.org/10.1097/01.ccm.0000157969.46388.a2 (2005).
Frithiof, R. et al. Critical illness polyneuropathy, myopathy and neuronal biomarkers in COVID-19 patients: A prospective study. Clin. Neurophysiol. 132(7), 1733–1740. https://doi.org/10.1016/j.clinph.2021.03.016 (2021).
Taquet, M., Geddes, J. R., Husain, M., Luciano, S. & Harrison, P. J. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: A retrospective cohort study using electronic health records. The Lancet Psychiatry. 8(5), 416–427. https://doi.org/10.1016/S2215-0366(21)00084-5 (2021).
Robinson, E., Sutin, A. R., Daly, M. & Jones, A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 296, 567–576 (2022).
Rass, V. et al. Neurological outcomes 1 year after COVID-19 diagnosis: A prospective longitudinal cohort study. Eur. J. Neurol. 29(6), 1685–1696. https://doi.org/10.1111/ene.15307 (2022).
Ferrucci, R. et al. One-year cognitive follow-up of COVID-19 hospitalized patients. Eur. J. Neurol. https://doi.org/10.1111/ene.15324 (2022).
Seeßle, J. et al. Persistent symptoms in adult patients 1 year after coronavirus disease 2019 (COVID-19): A prospective cohort study. Clin. Infect. Dis. 74(7), 1191–1198. https://doi.org/10.1093/cid/ciab611 (2022).
Abu-Rumeileh, S. et al. The multifaceted role of neurofilament light chain protein in non-primary neurological diseases. Brain 146(2), 421–437. https://doi.org/10.1093/brain/awac328 (2023).
Larsson J. in Area-Proportional Euler and Venn Diagrams with Ellipses [R Package Eulerr Version 6.1.1] (2021).
Acknowledgements
We would like to thank all patients for participating in the study and all colleagues of the involved departments for their support.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
C.Bal.—Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Validation, Writing—original draft. C.Ban.—Investigation, Writing—review & editing. M.B.—Investigation, Writing—review & editing. T.B.—Investigation, Writing—review & editing. P.B.—Investigation, Writing—review & editing. S.E.—Conceptualization, Writing—review & editing. T.F.—Investigation, Writing—review & editing. C.J.H.—Investigation, Writing—review & editing. E.H.—Data curation, Writing—review & editing. J.I.—Investigation, Writing—review & editing. C.J.—Investigation, Writing—review & editing. B.-E.O.J.—Resources, Writing—review & editing. T.L.—Resources, Writing—review & editing. D.K.M.—Resources, Writing—review & editing. I.-K.P.—Writing—review & editing. I.S.—Investigation, Writing—review & editing. K.S.—Investigation, Writing—review & editing. A.-K.T.—Investigation, Writing—review & editing. J.T.—Resources, Writing—review & editing. L.V.—Investigation, Writing—review & editing. C.V.—Investigation, Writing—review & editing. G.W.—Investigation, Writing—review & editing. A.S.—Resources, Writing—review & editing. S.G.M.—Resources, Writing—review & editing. S.J.G.—Conceptualization, Investigation, Methodology, Supervision, Writing—review & editing. P.A.—Conceptualization, Investigation, Methodology, Supervision, Writing—original draft.
Corresponding author
Ethics declarations
Competing interests
CBal, CBan, MB, TB, PC, SE, TF, SJG, CJH, EH, JI, CJ, TL, SGM, DKM, IS, KS, AKT, JT, LV, CV & GW have nothing to disclose. BEOJ reports research grants from Gilead, GSK, and Roche, travel support from Gilead, honoraria for lectures/presentations from Gilead, GSK, and Fresenius Medical Care, served on advisory boards for Gilead, and is an (unpaid) member of the COVRIIN expert group at the Robert-Koch-Institute. IKP reports research support from the German MS Society, Celgene, Novartis, Roche, and Teva, payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from Almirall, Biogen, BMS, Celgene, Genzyme, Janssen, Merck, Novartis, Roche, and Teva, and served on advisory boards for Biogen, BMS, Celgene, Janssen, Medscape, and Novartis. AS reports research grants from the German Research Foundation, consulting fees from Abbott and Medtronic Inc., and speaker honoraria from Abbott, Boston Scientific, Medtronic Inc., and Novartis. PA reports research grants, speaker honoraria and travel support from Allergan, Abbvie, Biogen, Janssen Cilag, Bristol Myers Squibb, Celgene, Sanofi/Genzyme, Ipsen, Merck, Merz, Novartis, Roche, Sanofi, and speaker honoraria from Lilly, Sandoz, Teva.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Balloff, C., Bandlow, C., Bernhard, M. et al. Prevalence and prognostic value of neurological affections in hospitalized patients with moderate to severe COVID-19 based on objective assessments. Sci Rep 13, 19619 (2023). https://doi.org/10.1038/s41598-023-46124-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-46124-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.