Abstract
Brain metastasis in gastric cancer (GC) patients is a rare phenomenon that is associated with adverse clinical outcomes and poor survival rates. We conducted a retrospective cohort study to investigate the incidence, risk factors and prognostic factors of brain metastasis in GC patients. Data on sociodemographic and tumor characteristics of GC patients from 2010 to 2019 was extracted from the Surveillance, Epidemiology and End-Results (SEER) database. Descriptive statistics, multivariable logistic and Cox regression were applied on SPSS. Kaplan–Meier-Survival curves and ROC curves were constructed. A total of 59,231 GC patients, aged 66.65 ± 13.410 years were included. Brain metastasis was reported in 368 (0.62%) patients. On logistic regression, the risk of brain metastasis was significantly greater in males, patients aged < 60 years and patients having concurrent bone and lung metastasis. High grade and high N stage were significant risk factors for development of brain metastasis. Patients who had undergone surgery for the primary tumor were at reduced risk for brain metastasis (adjusted odds ratio 0.210, 95% CI 0.131–0.337). The median OS was 3 months in patients with brain metastasis and 17 months in patients without brain metastasis (p < 0.05). On Cox regression, Grade IV tumors and primary antral tumors were significant predictable parameters for poor prognosis. Overall Survival (OS) and Cancer-Specific Survival (CSS) were prolonged in patients who had undergone surgery. Brain metastasis in gastric cancer is associated with significantly worse survival. Employing large-scale screening for high-risk patients holds a promising impact to improve survival rates, but it must be accurately balanced with a comprehensive understanding of clinicopathological aspects for accurate diagnosis and treatment.
Similar content being viewed by others
Introduction
The World Health Organization ranks stomach cancer as the fifth most common form of cancer worldwide. According to the latest statistics by GLOBOCAN2020, gastric cancer remains the fourth-leading cause of death worldwide, accounting for 7.7% of cancer deaths, and is a significant contributor to global mortality and morbidity, particularly in men1. Being extremely aggressive and heterogeneous, gastric cancer poses a global public health risk2. It is a multifactorial disease brought on by a variety of genetic and environmental factors. Owing to the vague symptoms and lack of proper awareness and understanding of the disease, the cancer usually has a low survival rate. It is commonly detected after it has spread to one or more organs3. Despite rapid advancements in diagnostic and therapeutic options, fewer than 5% of patients survive more than 5 years after initial diagnosis4,5.
The brain is a common site of metastatic spread in several malignancies. According to Lemke et al., nearly 10% of all cancer patients develop brain metastasis at some point in the course of the disease6,7. This, however, is mostly dependent on the location of the first tumor, as a majority of brain metastases only involve the tumors of skin, breast, and lungs. As much as 4% of esophageal and colorectal cancers also metastasize to the brain. On the other hand, with an incidence of less than 1% (0.2–0.7%), the brain is a very uncommon site for metastasis in gastric cancer6. Gastric cancers spread more frequently to the liver (48%), peritoneum (32%), bones (12%) and lungs (15%)8,9.
Although brain metastasis is rare in cases of gastric cancer, it has an unfavourable prognosis globally and low survival rates. Patients are severely cachexic, and the median Overall Survival (OS) is reported to be 1.3–2.4 months, due to its detection at an advanced stage of the disease10,11,12. After a diagnosis of gastric cancer, the median time until brain metastasis is reported to be 12.3 months10. Most of these patients have their cancer already metastasized to bones, liver and lungs12. Although resecting the metastatic lesion significantly increases the patients' chances of survival, brain metastasis is usually very difficult to treat and resect10,11. Lin et al. identified size, tumor extension, T, and N stages as significant risk factors for metastatic spread to the brain13. Analysis of the Surveillance, Epidemiology and End-Results (SEER) registry from 1998 to 2004 revealed that age, sex, and the location of the primary stomach tumor all significantly predicted the prognosis of patients with metastatic gastric cancer14.
Despite the poor prognosis in patients who develop brain metastasis, there is limited literature which describes the risk factors for brain metastasis and the prognostic factors which influence survival. The available evidence consists primarily of reviews, case series and small-scale observational studies. Therefore, we undertook an analysis of data from the SEER database to correctly identify the risk factors as well as prognostic factors for brain metastasis in gastric carcinoma.
Methods
Data source
We extracted data for our retrospective cohort study from the SEER database, which is a data registry funded by the National Cancer Institute. We used the dataset Incidence-SEER 17 Regs Research Data, Nov 2021 Sub (2000–2019) to generate case listings14. Data on the metastatic spread to distant organs, including the brain, became available from 2010. Therefore, we used SEER*Stat 8.4.0.1 software to identify the pathologically diagnosed cases of gastric cancer from 2010 to 201915. We selected patients based on the following inclusion criteria: (1) diagnosis of gastric cancer (site recode ICD-O-3/WHO2008:C160-C169), (2) complete metastatic and survival information. Patients with cancer diagnosed during autopsy or through their death certificate and those with incomplete survival data were excluded.
Outcome variables
We collected information pertaining to gender, race, age at diagnosis, year of diagnosis, primary site, histology, tumor size, grade, TNM stage, distant organ metastasis, surgery of primary tumor, income, OS and Cancer-Specific Survival (CSS). The time interval between diagnosis of gastric cancer and death due to any cause was defined as OS. The time interval between diagnosis of gastric cancer and death due to gastric cancer was defined as CSS. Authorization was obtained from the SEER website and no additional ethical approval was required.
Statistical analysis
The sociodemographic and tumor characteristics of included patients were summarized using descriptive statistics. Comparisons were made between patients with and without brain metastasis using the chi-square test. Risk factors for brain metastasis in gastric cancer patients were discerned using logistic regression analysis. Receiver Operator Characteristics (ROC) curves were constructed and Areas Under the Curve (AUC) were computed to determine the diagnostic efficacy of multiple variables in predicting brain metastasis. Survival function estimation and comparison among patients with and without brain metastasis were performed using Kaplan–Meier estimates and the log-rank test. Variables that were associated with prognosis in gastric cancer patients with brain metastasis were identified using Cox proportional hazard regression. All statistical analysis was performed on SPSS version 26, and a p-value less than 0.05 was considered statistically significant.
Results
General data
A total of 59,231 patients with gastric cancer were enrolled in this study, including 35,889 (60.6%) males and 23,342 (39%) females. 70.9% of patients (n = 41,995) were Caucasians, 13.1% (n = 7776) were African American and 16% (9460) from other ethnicities. Metastasis to the brain was reported in 368 (0.62%) patients.
Characteristics of patients with or without metastasis
It was found that brain metastasis was significantly more common in patients aged younger than 60 years, males, Caucasians, patients with primary tumor site of the cardia, grade IV, unknown T stage, unknown N stage, patients with no previous surgery for primary tumor and in whom cancer had metastasized to other organs such as bone, liver and lung (P < 0.05). There was no significant association between income and histological type of tumor and brain metastasis (Table 1).
Univariable and multivariable logistic regression analysis of odds of gastric cancer brain metastasis
Univariable analysis results suggested that tumor site in stomach, race, age, gender, T stage, N stage, tumor grade, metastasis to bone, liver and lung, surgery of primary tumor, tumor size and histological type were significant independent risk factors for brain metastasis (P < 0.05), whereas income was not a significant risk factor for brain metastasis (P > 0.05) (Table 2).
All significant factors from the univariable analysis were entered in to the multivariable logistic regression model. Risk of brain metastasis was significantly lower in patients older than 60 years, compared to patients younger than 60 years (adjusted odds ratio [aOR] 0.680, 95% CI 0.547–0.846). Males were at a significantly higher risk of brain metastasis compared to females (aOR 1.294, 95% CI 1.017–1.647). Risk of brain metastasis was significantly greater in patients who had developed metastasis to lung (aOR 3.943, 95% CI 3.101–5.013) and bone (aOR 3.845, 95% CI 3.020–4.896). Patients with Grade II cancer (aOR 4.387, 95% CI 1.367–14.081), Grade III cancer (aOR 3.819, 95% CI 1.204–12.109), Grade IV cancer (aOR 7.961, 95% CI 2.049–30.921) and patients with unknown grade (aOR 5.420, 95% CI 1.704–17.238) were more likely to develop metastasis to brain as compared to patients with Grade I tumors. Patients who underwent surgery of primary tumor were at significantly lower risk of brain metastasis (aOR 0.210, 95% CI 0.131–0.337). Risk of brain metastasis was lesser in patients with primary tumor of antrum (aOR 0.267, 95% CI 0.158–0.452) and body (aOR 0.530, 95% CI 0.340–0.827), compared to cardia. Patients at N3 stage (aOR 2.527, 95% CI 1.548–4.127) and patients with unknown N stage (aOR 1.459, 95% CI 1.110–1.917) were at greater risk of brain metastasis, compared to patients at N1 stage. Patients who had undergone previous surgery for primary tumor were at lesser risk of developing brain metastasis as compared to patients who had not (aOR 0.210, 95% CI 0.131–0.337). Race, histology, liver metastasis, tumor size and T stage were not significant predictors of brain metastasis (Table 2).
Comparison of diagnostic efficacy of risk factors for gastric cancer brain metastasis
We constructed ROC curves to determine the diagnostic power of risk factors for brain metastasis in gastric cancer patients (Fig. 1). The AUC for different risk factors were compared. The results showed that the AUC for surgery was 0.704 (95% CI 0.684–0.724, p < 0.001), AUC for site was 0.557 (95% CI 0.523–0.590, p < 0.001); AUC for histological type of tumor was 0.515 (95% CI 0.487–0.544, p = 0.305); the AUC for grade was 0.570 (95% CI 0.542–0.598, p < 0.001); the AUC for tumor size was 0.638 (95% CI 0.610–0.666, p < 0.001); the AUC for gender was 0.557 (95% CI 0.529–0.586, p < 0.001); the AUC for T stage was 0.675 (95% CI 0.646–0.704, p < 0.001); the AUC for N stage was 0.619 (95% CI 0.590–0.649, p < 0.001); the AUC for age was 0.550 (95% CI 0.520–0.580, p = 0.001); the AUC for bone metastasis was 0.640 (95% CI 0.607–0.674, p < 0.001); the AUC for liver metastasis was 0.626 (95% CI 0.594–0.658, p < 0.001); the AUC for lung metastasis was 0.654 (95% CI 0.620–0.687, p < 0.001); the AUC for race was 0.550 (95% CI 0.522–0.578, p = 0.001); the AUC for income was 0.505 (95% CI 0.477–0.534, p = 0.721). Surgery of primary tumor was the best diagnostic predictor for brain metastasis.
Survival analysis
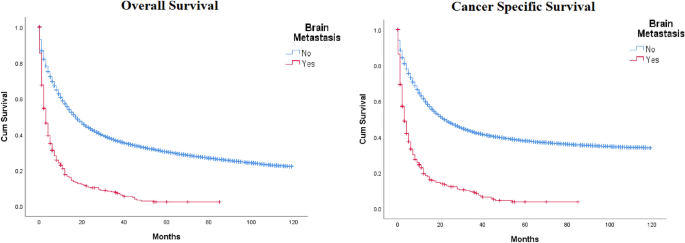
The median OS was 3.0 months (95% CI 2.449 ~ 3.551) in patients with brain metastasis and 17 months (95% CI 26.778 ~ 33.222) in patients without brain metastasis (p < 0.05) (Fig. 2). The 1, 2, and 4-year OS of patients with brain metastasis were 14.4%, 8.42%, and 1.62%, respectively. The 1, 2 and 4-year OS of patients without brain metastasis were 49%, 33%, and 17.96%, respectively. The median CSS of patients with brain metastasis was 3.0 months (95% CI 2.313 ~ 3.687). For patients without brain metastasis, the median CSS was 22 months (95% CI 21.397 ~ 22.603) (p < 0.05).
Univariable and multivariable analysis of factors affecting the prognosis of patients with brain metastasis in gastric cancer
Univariable Cox regression analysis of patients with brain metastasis showed that bone metastasis, no previous surgery, grade 4 tumor, unknown N stage and primary tumor of antrum, body, greater curvature and overlapping/non-specified site of primary tumor were significant predictors of worse OS (Tables 3, 4).
All significant factors from the univariable analysis were entered into the multivariable Cox regression model. Patients who underwent surgery of primary tumor had significantly better OS compared to patients who did not undergo surgery (adjusted hazard ratio [aHR] 0.452, 95% CI 0.269–0.758). Grade IV patients had a worse OS compared to patients with Grade I tumors (aHR 5.322, 95% CI 1.114–25.415). Patients with primary tumors of antrum (aHR 1.957, 95% CI 1.122–3.414) and greater curvature (aHR 2.339, 95% CI 1.238–4.422) had significantly worse OS compared to patients with primary tumor of cardia. Patients with unknown N stage had significantly worse OS compared to patients at N1 stage (aOR 1.372, 95% CI 1.026–1.834) (Table 3).
Univariable Cox regression analysis of patients with brain metastasis showed that bone metastasis, no surgery, grade IV tumor, unknown N stage and primary tumor of antrum, body, greater curvature and overlapping/non-specified site of primary tumor were significant predictors of worse CSS (Table 3).
All significant factors from the univariable analysis were entered into the multivariable Cox regression model. Patients who underwent surgery for primary tumor had significantly better CSS compared to patients who did not undergo surgery (aHR 0.458, 95% CI 0.268–0.781). Grade IV patients had a worse CSS compared to patients with Grade I tumors (aHR 5.287, 95% CI 1.106–25.268). Patients with primary tumors of antrum (aHR 1.858, 95% CI 1.045–3.302) had significantly worse CSS compared to patients with primary tumor of cardia. Patients with unknown N stage had significantly worse CSS compared to patients at N1 stage (aOR 1.390, 95% CI 1.027–1.881) (Table 3).
Discussion
Due to the known rarity of brain metastasis in gastric carcinoma patients, the risk factors and prognostic variables have yet to be clearly determined. Our results indicated a greater risk of brain metastasis in patients aged less than 60 years, those who had already developed lung and bone metastasis, patients with grade II, III, and IV cancer, and patients with N3 stage. In contrast, patients who underwent surgery for primary tumor and those with tumors involving antrum and body of stomach had a decreased risk of brain metastasis compared to patients who did not undergo surgery and those with tumors involving cardia of stomach, respectively. Surgery of primary tumor was the best diagnostic predictor for brain metastasis. The median OS and the median CSS were lower in patients with brain metastasis than in those without brain metastasis. Better OS and CSS were seen in patients who underwent surgery for primary tumor; whereas, OS and CSS were worse for patients with primary tumor of antrum and grade IV tumor.
Data from 59,231 patients with gastric carcinoma were included in our current study, and metastasis to the brain was reported in 0.62% of the patients. Our results are comparable to Qui et al. who analysed data of gastric carcinoma patients between the years 2010 and 2014 and reported 0.79% of their study population to have brain metastasis16. A study conducted by Lin et al. reported 0.39% of their study population of 18,752 gastric carcinoma patients to have brain metastasis12. The variations in the occurrence of brain metastasis can be due to multiple factors, including but not limited to, differences in the study population, treatment of choice, and the duration of treatment.
Existing literature shows gastric carcinoma to have a higher incidence of metastasising to the liver (16.82%), lungs (5.92%), and bone (5.08%)16. The observed distribution is in accordance with the path of spread of tumor cells, with metastasis being most commonly reported in the site closest to the stomach. Tumor cells from the stomach reach the liver through the portal veins, before spreading to the lungs and finally to the brain. The documented occurrence of brain metastasis could potentially be underestimated, as routine brain scans are not typically conducted during the evaluation of gastric cancer cases17. Moreover, owing to rapid disease progression and shorter survival time in many patients with brain metastasis, there is a lack of clinical information12. Thus, it may be safe to assume that the incidence of brain metastasis in gastric carcinoma patients is underestimated.
Other gastrointestinal cancers, especially colorectal and oesophageal are known to be more widely associated with brain metastasis, in comparison to gastric and pancreatic cancers. This difference may be due to different genetic makeups, as well as diverging mechanisms and routes of haematological dissemination6.
The risk of brain metastasis was lesser in patients with primary tumor of antrum but they had significantly worse OS compared to primary proximal tumors. Our findings are consistent with Qui et al. who report that metastasis was significantly more likely to occur in proximal stomach cancer compared to distal stomach cancer. Yang et al. also reported a survival benefit in tumors of gastric cardia compared to more distal locations13,16. However, according to another study, proximal tumors were reported to be larger, with deeper penetration of gastric wall, more frequent metastasis to lymph nodes and more advanced stage. Overall survival was worse in proximal gastric tumors18. The disparity in available literature warrants more extensive research into this matter.
As expected, patients with grade IV tumors had a worse OS and CSS compared to those with grade I tumors. This was consistent with the findings of Yang et al.13. Studies conducted on bone metastasis in gastric cancer patients also report a similar pattern of prognosis and overall survival3. Our study suggested a higher occurrence of brain metastasis in younger patients which may be attributed to the differences in lymph node involvement in different age groups. The proportion of gastric cancer patients with more than 15 lymph node metastases decreases significantly with age19. It should also be highlighted here that younger age was not a significant predictor of OS and CSS. A study on gastric carcinoma in young patients also reported similar results20.
In our study, the mean overall survival in patients with brain metastasis was 3 months, as opposed to 17 months in patients without brain involvement. This was consistent with the findings reported by Qui et al.16. Mean cancer survival was also significantly lesser in patients with brain metastasis (3 months versus 22 months). A lower survival rate correlates with the fact that brain metastasis from gastric cancer is a late event in the disease’s clinical course. Moreover, the existence of the blood–brain barrier hinders the maximal therapeutic effect of chemotherapeutic drugs, resulting in a poor prognosis21.
Among the various risk factors assessed in our analysis, surgery was seen to be the best diagnostic predictor for brain metastasis. Patients who underwent surgery had a significantly lower risk of developing brain metastasis and had a better OS compared to those who did not undergo surgery. However, once brain metastasis has occurred, various prognostic factors like performance status, number and site of metastases and dissemination to other organs, need to be considered before forming a treatment plan. It is known the aggressive nature of brain metastasis in gastric carcinoma warrants an aggressive treatment like neurosurgery, combined with stereotactic radiosurgery, palliative radiotherapy, and chemotherapy11.
This is the first SEER-based study to focus solely on brain metastasis in gastric cancer patients. Limitations of our analysis should be considered while interpreting the results. Despite a large study population, selection bias exists owing to the retrospective study design. Other important prognostic factors, like imaging, CEA and alkaline phosphatase levels, and various treatment regimens have not been studied. Data from SEER included reported cases of gastric carcinoma from 2010 to 2019; it may be argued that this provides an inadequate follow-up period. Furthermore, ethnicity and geographical factors, which are known risk factors for gastric cancer, have been not extensively studied.
In conclusion, the incidence of brain metastasis for gastric cancer patients is reported to be 0.62%. The presence of brain metastasis significantly reduces the overall and cancer-specific survival, and higher staging and grading are associated with a worse prognosis. Clinicians need to consider clinicopathological factors when deciding on diagnostic and treatment regimens. Further research, including other prognostic factors such as the number and site of brain metastases, various treatment options and a larger prospective cohort, is imperative.
Data availability
The datasets used and analysed during the current study available from the corresponding author on reasonable request.
References
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71(3), 209–249 (2021).
Gao, J. P., Xu, W., Liu, W. T., Yan, M. & Zhu, Z. G. Tumor heterogeneity of gastric cancer: From the perspective of tumor-initiating cell. World J. Gastroenterol. 24(24), 2567 (2018).
Xiaobin, C. et al. Analysis of related risk factors and prognostic factors of gastric cancer with bone metastasis: A SEER-based study. J. Immunol. Res. 2022, 3251051 (2022).
Brenner, H., Rothenbacher, D. & Arndt, V. Epidemiology of stomach cancer. Methods Mol Biol. 472, 467–477 (2009).
Rawla, P. & Barsouk, A. Epidemiology of gastric cancer: Global trends, risk factors and prevention. Prz. Gastroenterol. 14(1), 26–38 (2019).
Lemke, J. et al. Brain metastases in gastrointestinal cancers: Is there a role for surgery?. Int. J. Mol. Sci. 15(9), 16816 (2014).
Barnholtz-Sloan, J. S. et al. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J. Clin. Oncol. 22(14), 2865–2872 (2004).
Riihimäki, M., Hemminki, A., Sundquist, K., Sundquist, J. & Hemminki, K. Metastatic spread in patients with gastric cancer. Oncotarget. 7(32), 52307–52316 (2016).
York, J. E., Stringer, J., Ajani, J. A., Wildrick, D. M. & Gokaslan, Z. L. Gastric cancer and metastasis to the brain. Ann. Surg. Oncol. 6(8), 771–776 (1999).
Kasakura, Y., Fujii, M., Mochizuki, F., Suzuki, T. & Takahashi, T. Clinicopathological study of brain metastasis in gastric cancer patients. Surg Today. 30(6), 485–490 (2000).
Kraszkiewicz, M. & Wydmanski, J. Brain metastases from stomach cancer: The role of different treatment modalities and efficacy of palliative radiotherapy. Rep. Pract. Oncol. Radiother. 20(1), 32–37 (2014).
Lin, Z. et al. Prediction of distant metastasis and survival prediction of gastric cancer patients with metastasis to the liver, lung, bone, and brain: Research based on the SEER database. Ann. Transl. Med. 10(1), 16–16 (2022).
Yang, D. et al. Survival of metastatic gastric cancer: Significance of age, sex and race/ethnicity. J. Gastrointest. Oncol. 2(2), 77–84 (2011).
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence—SEER Research Data, 17 Registries, Nov 2021 Sub (2000–2019)—Linked To County Attributes—Time Dependent (1990–2019) Income/Rurality, 1969–2.
Surveillance Research Program. National Cancer Institute SEER*Stat software (www.seer.cancer.gov/seerstat) Version 8.4.0.1.
Qiu, M. Z. et al. Frequency and clinicopathological features of metastasis to liver, lung, bone, and brain from gastric cancer: A SEER-based study. Cancer Med. 7(8), 3662–3672 (2018).
Lohr, F., Pirzkall, A., Hof, H., Fleckenstein, K. & Debus, J. Adjuvant treatment of brain metastases. Semin. Surg. Oncol. 20(1), 50–56 (2001).
Pinto-de-Sousa, J., David, L., Seixas, M. & Pimenta, A. Clinicopathologic profiles and prognosis of gastric carcinomas from the cardia, fundus/body and antrum. Dig. Surg. 18(2), 102–110 (2001).
Ahmad, A., Khan, H., Cholankeril, G., Katz, S. C. & Somasundar, P. The impact of age on nodal metastases and survival in gastric cancer. J. Surg. Res. 202(2), 428–435 (2016).
Al-Refaie, W. B., Pisters, P. W. & Chang, G. J. Gastric adenocarcinoma in young patients: A population-based appraisal. Ann. Surg. Oncol. 25, 4547. https://doi.org/10.1200/jco20072518_suppl4547 (2007).
Daneman, R. & Prat, A. The blood–brain barrier. Cold Spring Harb. Perspect. Biol. 7(1), a020412 (2015).
Author information
Authors and Affiliations
Contributions
M.R., A.K., F.F. Conceptualization B.M., A.S., H.C. Methodology M.R., F.F. Formal analysis and investigation, prepared figures and tables. M.R., F.F., S.M., I.K., T.H. Original draft preparation A.K., A.I., R.A. Writing review and editing S.R., F.A., S.S. Supervision.
Corresponding author
Ethics declarations
Competing interests
Faiz Anwer reports personal fees from Bristol Myers Squibb as a speaker and fee from Janssen Pharmaceutical as an advisory board member, this fee was not related to the submitted work. Without receiving direct funding, served as the local principal investigator for Allogene Therapeutics, Celgene, GlaxoSmithKline, and Bristol Myers Squibb; has a consulting or advisory role for Seattle Genetics, Incyte Corporation Speakers’ Bureau, Company: Incyte Corporation; receives travel and accommodations expenses from Seattle Genetics, Incyte; receives honoraria from Incyte, Company: Seattle Genetics; and received research funding from Seattle Genetics, Company: Celgene, Acetylon Pharmaceuticals, Millennium, Astellas Pharma and AbbVie; and reports no other potential conflicts of interest for this work. The other authors report no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rehman, M.E.U., Kulsoom, A., Faraz, F. et al. Analysis of risk factors and prognostic factors of brain metastasis in gastric cancer: a surveillance, epidemiology and end-results database study. Sci Rep 13, 18664 (2023). https://doi.org/10.1038/s41598-023-46109-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-46109-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.