Abstract
Although the placement of an intraventricular catheter remains the gold standard method for the diagnosis of intracranial hypertension (ICH), the technique has several limitations including but not limited to its invasiveness. Current noninvasive methods, however, still lack robust evidence to support their clinical use. We aimed to estimate, as an exploratory hypothesis generating analysis, the discriminative power of four noninvasive methods to diagnose ICH. We prospectively collected data from adult intensive care unit (ICU) patients with subarachnoid hemorrhage (SAH), intraparenchymal hemorrhage (IPH), and ischemic stroke (IS) in whom invasive intracranial pressure (ICP) monitoring had been placed. Measures were simultaneously collected from the following noninvasive methods: optic nerve sheath diameter (ONSD), pulsatility index (PI) using transcranial Doppler (TCD), a 5-point visual scale designed for brain Computed Tomography (CT), and two parameters (time-to-peak [TTP] and P2/P1 ratio) of a noninvasive ICP wave morphology monitor (Brain4Care[B4c]). ICH was defined as a sustained ICP > 20 mmHg for at least 5 min. We studied 18 patients (SAH = 14; ICH = 3; IS = 1) on 60 occasions with a mean age of 52 ± 14.3 years. All methods were recorded simultaneously, except for the CT, which was performed within 24 h of the other methods. The median ICP was 13 [9.8–16.2] mmHg, and intracranial hypertension was present on 18 occasions (30%). Median values from the noninvasive techniques were ONSD 4.9 [4.40–5.41] mm, PI 1.22 [1.04–1.43], CT scale 3 points [IQR: 3.0], P2/P1 ratio 1.16 [1.09–1.23], and TTP 0.215 [0.193–0.237]. There was a significant statistical correlation between all the noninvasive techniques and invasive ICP (ONSD, r = 0.29; PI, r = 0.62; CT, r = 0.21; P2/P1 ratio, r = 0.35; TTP, r = 0.35, p < 0.001 for all comparisons). The area under the curve (AUC) to estimate intracranial hypertension was 0.69 [CIs = 0.62–0.78] for the ONSD, 0.75 [95% CIs 0.69–0.83] for the PI, 0.64 [95%Cis 0.59–069] for CT, 0.79 [95% CIs 0.72–0.93] for P2/P1 ratio, and 0.69 [95% CIs 0.60–0.74] for TTP. When the various techniques were combined, an AUC of 0.86 [0.76–0.93]) was obtained. The best pair of methods was the TCD and B4cth an AUC of 0.80 (0.72–0.88). Noninvasive technique measurements correlate with ICP and have an acceptable discrimination ability in diagnosing ICH. The multimodal combination of PI (TCD) and wave morphology monitor may improve the ability of the noninvasive methods to diagnose ICH. The observed variability in non-invasive ICP estimations underscores the need for comprehensive investigations to elucidate the optimal method-application alignment across distinct clinical scenarios.
Similar content being viewed by others
Introduction
Intracranial hypertension (ICH) is a frequent and critical complication after acute brain injury1,2. Intracranial pressure (ICP) measurement is considered the standard of care to guide therapy in patients with potential ICH3, although there is no definitive evidence supporting the usefulness of ICP monitoring to improve patient outcomes4.
Despite several limitations of the invasive method for monitoring ICP (ICPi)5, a noninvasive method (ICPni) that meets all the requirements to replace it is still not available6. Recently, either the association of noninvasive methods7 or the creation of new ICPni monitoring techniques has renewed the interest in these technologies8,9,10.
In this context, in this study we evaluated the correlation between ICPi and four noninvasive methods: a noninvasive waveform pulse morphology (P2/P1 ratio and Time-To-Peak [TTP) (Brain4care9,11 technology), the optic nerve sheath diameter (ONSD)12, pulsatility index (PI) by transcranial Doppler (TCD)13, and a five-item visual scale assessed by brain computed tomography (CT)6,14. Additionally, as an exploratory hypothesis generating analysis, we assessed the discriminant ability of these noninvasive methods to detect ICH.
Methods
We conducted a prospective study of patients with acute ischemic (IS) or hemorrhagic stroke (HS) requiring ICPi monitoring due to the risk of ICH. We included patients admitted to a neurocritical care unit (neuro-ICU) of a tertiary hospital, aged 18 years or older, diagnosed at admission with IS or HS (subarachnoid and intraparenchymal hemorrhage) who required ICPi monitoring with the placement of external ventricular drainage (EVD). We excluded patients with chronic neurological diseases (demyelinating or neuromuscular disease), past medical history of diseases associated with high ICP (e.g., chronic hydrocephalus, benign intracranial hypertension), those under ICP monitoring other than intraventricular (e.g., subdural or epidural), or with suspected brain death. There was no direct public or private funding for this study, except for the availability of the device and the technical support given by Brain4care Inc. This study protocol was approved by our local Ethics Committee and registered at clinicaltrials.gov under number NCT05121155. All patients’ legal representative signed an informed consent form.
Patient monitoring
All patients received the standard ICU continuous hemodynamic monitoring, which consisted of invasive blood pressure assessment through the radial artery, continuous electrocardiography, and pulse oximeter. Except for the CT scan, all tests were performed simultaneously, at least five minutes after EVD closure. ICP was assessed through a catheter inserted into the ventricle and connected to a pressure transducer placed at the level of the external auditory meatus and connected to a drainage system (Codman, Johnson and Johnson Medical Ltd., Raynham, MA, USA). Blood flow velocities were measured using TCD (DWL, Doppler BOXx, Compumedix, Germany) by a selected group of experienced certified operators. Insonation was standardized by positioning a 2 MHz pulsed low-frequency ultrasound probe in the temporal window for insonation of the M1 and M2 portions of the middle cerebral artery (MCA) at a depth of 45–55 mm bilaterally to measure the pulsatility index (PI), with one measurement on each side. PI was calculated automatically using the formula:
Optic nerve sheath ultrasound (ONSUS) was performed exclusively by the principal investigator using an US device with a 13–6 MHz linear probe with ocular presets (Samsung Mysono U6, EUA). Three measurements were made on each side (six measurements per patient). The final sheath value was the average of these six measurements. The probe was leaned against the upper eyelid with the eyes closed and caudally and medially angled until the optic nerve was visualized as a linear hypoechoic structure with well-defined margins posterior to the eyeball. The probe was never leaned against the patient’s cornea or conjunctiva. All images were collected on an axial/transverse axis for uniformity. The sheath was measured 3 mm behind the retina.
All CT measurements were made within 24 h of the other methods and assessed by certified neuroradiologists to detect the ICH signs described in Table 1. CT readers were blinded to ICPi measurements.
The Braincare sensor (Braincare Monitor 2000 and Braincare ICPNI sensor [BcSsNI2000], Braincare Corp, USA) was positioned on the patient’s scalp without shaving, surgical incision, or trepanation after EVD closure. The Braincare Analytical System acquired ICP wave morphology through a strain sensor that, when in contact with the patient’s skin on the skull, can detect and monitor subtle bone deformations caused by ICP changes. These ICP oscillations generate pulse waves corresponding to the ICPi monitoring9,11. The pulse waveform was monitored throughout the session time. The device digitized, filtered, and amplified all recordings, which were later transferred to a computer for analysis. Brain4care® monitor results were accessed by professionals blinded to the results of the other noninvasive methods and the absolute ICPi value. Patients were monitored for at least 30 min. The ICPni waveform parameters calculated were the P2/P1 ratio and the time-to-peak (TTP). Calculations were performed using the B4c morphology after artifact exclusion. The mean pulse wave was used to calculate P1 and P2 peak amplitudes, with the peak arterial pressure wave being used to define P1 in case of disagreement15. The amplitude was obtained by detecting the highest point of these peaks and subtracting the initial ICPni wave value. P2/P1 ratio was calculated by dividing the amplitude of these two points. TTP is the time between wave onset and its maximum peak. The averaged values of P2/P1 and TTP were obtained from the entire recording (Fig. 1).
Waveform analysis of the Brain4care Monitor. (A): normal waveform (P1 > P2 and short TTP). (B): abnormal waveform (P2 > P1 and longer TTP). P2/P1 ratio: the ratio between the amplitudes of peaks P2 and P1; TTP: time to peak, defined as the time, from the start of the pulse, at which the ICP waveform reaches its highest peak. The shaded line represents the confidence interval of the 1-min monitoring.
Data analysis
Qualitative variables were expressed as absolute (n) and relative (%) frequencies, and quantitative variables were expressed as mean ± standard deviation, medians, minimum, and maximum values.
Repeated measures correlation (rmcorr) was used to assess the relationship between noninvasive methods and the absolute ICP value16. The intraclass correlation coefficient (ICC) was used to analyze the agreement between sides in the TCD and the ONSD measurements. Receiver operator characteristic (ROC) curves for repeated measures were constructed for each method to define the cutoff points of the noninvasive techniques, considering the presence or absence of ICH (mean ICP greater than 20 mmHg) as the reference standard17. The area under the curve (AUC) was used to describe the discriminatory power of the methods, and the Youden index was used to define the cutoff point for each method. Binary logistic regression models for repeated measures using generalized estimated equations were used to analyze how these methods related to ICH jointly. The results were presented as odds ratio (OR) and their respective 95% confidence intervals (CI95%). ICH was considered the dependent variable, and noninvasive methods as the independent variables. Statistical analysis was performed using the JAMOVI software (version 1.8.1.).
Ethics approval and consent to participate
This study protocol was approved by our local Ethics Committee at https://plataformabrasil.saude.gov.br under number 03843118.0.0000.5505 and registered at clinicaltrials.gov under number NCT05121155. All patients’ legal representative signed an informed consent form. The research performed in accordance with the Declaration of Helsinki.
Results
Population description
Of the 30 patients with invasive ICP monitoring admitted to our Neuro-ICU between March 2019 and March 2020 (pre-COVID-19), 18 met our inclusion and exclusion criteria (Fig. 2), with a total of 60 monitoring sessions regarding all methods described in this study. Fifty-one monitoring sessions were from patients with subarachnoid hemorrhage (SAH), two from patients with IS, and seven from patients with intraparenchymal hemorrhage (IPH). SAH etiology was 100% aneurysmal, IPH was 100% hypertensive, and the two IS were cardioembolic. Table 2 shows the clinical characteristics of the patients.
ICP wave morphology—Brain4care method
The mean time of invasive and noninvasive monitoring with Brain4Care (B4c) was 45 min (35–60 min), with a mean of 3.290 waves per monitoring (IC 2.080–4.310), totaling 197.400 B4c waves distributed in 2.495 min. In 30% (18 out of 60) of the monitoring sessions, the mean ICP was higher than 20 mmHg. The morphological characteristics of B4c waves are described in Table 3.
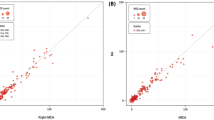
The mean B4c P2/P1 ratio correlated with the absolute ICP value (r = 0.35, p < 0.001). The correlation between the mean TTP and the mean ICP was also significant (r = 0.35, p < 0.001). The mean B4c P2/P1 ratio showed a sensitivity of 100%, specificity of 45.5%, positive predictive value (PPV) of 36.8%, and negative predictive value (NPV) of 100% to predict ICH, with a cutoff value of 1.06. TTP showed a sensitivity of 85.7%, specificity of 50.0%, PPV of 35.3%, and NPV of 91.7% to predict ICH, with a cutoff value of 0.199. The AUC was 0.79 (Fig. 3A) for the mean P2/P1 and 0.69 for the mean TTP to predict ICH. (Fig. 3B).
ROC curves of the noninvasive methods. (A) mean P2/P1 (B) mean TTP. (C) mean ONSD D) PI of TCD, (E) Sum of CT, (F) Combination of B4c and TCD. Abbreviations: B4C: Brain4care monitor; CT: Computerized Tomography; P2/P1: P2/P1 ratio; ONSD: Optic Nerve Sheath Diameter; PI: Pulsatility Index, TTP: Time-to-Peak; TCD: Transcranial Doppler.
Optic nerve sheath Ultrasonography
A total of 360 measurements were performed on 60 separate monitoring sessions. The mean ONSD was 4.93 mm (CI 3.57–7.70). The mean ONSD was 5.69 (CI 4.82–6.42) in sessions in which patients had ICH and 4.55 (CI 4.33–4.77) mm in sessions in which ICP was below 20 mmHg (p = 0.006). The mean ONSD difference between sides was 0.06 mm. The intraclass correlation coefficient (ICC) for assessing agreement between the right and left eye was high (0.92, CI 95% 0.87–0.96), suggesting a small side-to-side variation. The correlation between the mean ONSD value and the mean ICP was weak (r = 0.29, p = 0.01). The AUC for diagnosing ICH was 0.69 for the mean ONSD. With a cutoff of 5.2 mm, the sensitivity was 71.4%, the specificity was 70.4%, the PPV was 43.5%, and the NPV was 88.6% (Fig. 3C).
Transcranial Doppler
The 18 patients underwent 60 monitoring sessions, with 120 PI measurements (one measurement on each side). The mean PI on both sides was 1.22 (minimum 0.785, maximum 3.33). The mean difference between sides in the same patient was 0.12 (CI95% 0.08–0.16). The ICC for assessing agreement between the right and left PI was high (0.88, CI95% 0.83–0.91), suggesting slight side-to-side variation. The mean PI in patients with and without ICH was 1.09 and 1.45, respectively (p = 0.002). The correlation between mean PI and mean ICP was moderate (r = 0.62, p < 0.001). The mean PI showed an AUC of 0.75 to diagnose ICH. With a PI threshold of 1.28, the sensitivity was 78.6%, the specificity was 77.3%, the PPV was 50.0%, and the NPV was 91. 7%. (Fig. 3D). We performed a sensitivity analysis using only the time that overlapped between TCD and the B4c and found consistent results.
Brain CT scan
Overall, 55 of 60 (91.6%) CTs showed at least one radiological sign suggestive of ICH. CTs in which patients did not have ICH showed a median of two findings (minimum 0 and maximum 3), and a median of three findings (minimum 2 and maximum 5) when patients had ICH (p = 0.05). The correlation between the sum of CT findings and the mean ICP was weak (r = 0.21, p = 0.03). The AUC of the ROC curve of the sum of CT for ICH was 0.644 (Fig. 3E). Finding a signal on CT showed a sensitivity of 100%, a specificity of 16.6%, a PPV of 34%, and a NPV of 100% for detection of ICH.
Summary of the findings of the individual methods
Table 4 summarizes the correlation between noninvasive methods and ICP and the AUC values of the ROC curve with a defined cutoff value.
Logistic regression model for repeated measures
After multivariate analysis, only three of the variables described remained statistically significant: Mean B4C TTP, mean PI, and mean optic nerve sheath (ONS). The ROC curve of the sum of the three methods had an AUC of 0.861. The details are presented in Table 5. Comparing the aggregate accuracy of only two methods at a time the best combination (pair) of methods was B4c and TCD, with a ROC curve with an AUC of 0.802 (Fig. 3F).
Discussion
We found that the noninvasive methods used to evaluate the presence of ICH showed a wide range of correlation with ICP, from weak to moderate. Conversely, the discriminatory power of all four methods was moderate to high. When combined, B4c and TCD showed the best diagnostic ability.
The B4C wave morphology showed adequate performance, with a moderate correlation with ICP. The parameter P2/P1 was better than TTP in predicting ICH in the univariate analysis, although only TTP remained significant in the multivariate analysis. It is known that morphological changes in the ICP waveform precedes ICH18,19,20. Consequently, P2/P1 and TTP could be altered even before the onset of ICH depending on the intracranial compliance19. This could explain, at least in part, why some patients had abnormal P2/P1 and TTP but normal ICP value, justifying physiologically its moderate correlation to the ICP value and to predict ICH. This hypothesis is supported by a study that studied 38 patients with traumatic brain injury (TBI) and found an abnormal P2/P1 ratio in several patients with no ICH21. Another recent study analyzed the association between noninvasive wave morphology and intracranial compliance (ICC)22. A total of 36 patients with ICPi monitoring underwent an intracranial volume infusion test while monitored with TCD. Three methods were used to evaluate the ICC: a) a mathematical fluid model, b) an assessment of cerebral arterial blood volume changes, and c) the ratio of the amplitude of pulse wave P2/P1 peaks. All methods showed a strong and positive correlation with ICC. The P2/P1 ratio showed a correlation of 0.94 with ICC. Another recent study by Ballestero et al.23 aiming to assess the ICP waveform parameters on their ability to predict IH and functional prognosis evaluated 22 TBI patients simultaneously with B4C sensor and ICPi. The findings unveiled a robust non-linear correlation between ICPi and non-invasively derived nICPW waveforms, despite the presence of a moderate linear Pearson's correlation. However, the non-invasive parameters did not exhibit any association with patient outcomes or IH. This study used extended monitoring periods, a concept that, while interesting, may introduce certain limitations24. Considering the sensor's mechanical nature and its direct contact with the skull's surface, continuous monitoring in the context of an intensive care unit's daily operations could be susceptible to disruptions caused by patient movement or handling. Such factors could potentially undermine the precision of the assessments. In contrast, our study opted for a briefer monitoring duration, accompanied by vigilant oversight. This approach aligned more effectively with the device's current capabilities15.
In our study, ONSD showed worse results than expected compared to the previous literature. The initial studies25 showed a cutoff of 4.8 mm, with a sensitivity of 96%, specificity of 94%, and AUC = 0.98. Several other investigators corroborated these initial findings with cutoff points ranging from 4.8 to 5.2 mm26,27,28,29. A meta-analysis30 confirms that ONSD > 5.00 mm presents a sensitivity of 99% and specificity of 73%, including six studies with 352 patients with an AUC of 0.981. These encouraging results have been challenged by other investigators, who found a very weak correlation between the ONSD and the ICPi in patients with SAH31,32. A possible loss of the elastic properties of the ONS acutely distended due to very high ICP during aneurysmal rupture might be a possible explanation for the poor correlation of ICP and ONSD in patients with SAH. Hansen et. al explored the elastic properties of the ONS using human optic nerve preparations isolated from autopsies and used progressive pressure increases to show that moderate ICP increases allowed reversible sheath changes. However, when the pressure increase was equal to or greater than 45 mmHg, there was hysteresis, i.e. no return to the baseline diameter33. This is clearly relevant in SAH since ICP may rise to 100 mmHg during aneurysmal rupture both in humans and in experimental models, which is one of the reasons for the initial loss of consciousness some patients experience34,35.
The literature using TCD to predict ICH can be divided into three groups: predictions based on the PI, those based on the estimation of noninvasive cerebral perfusion pressure, and those using mathematical models. The published studies showed an accuracy for ICH prediction ranging from 0.62 to 0.92 (AUC)36. Bellner et al. evaluated 82 patients with distinct etiologies (SAH, TBI, and others) and reported an excellent ICC with ICP (R2 = 0.938) with the formula: ICP: 10.93 X PI—1.28. No other study has been able to replicate their results with such accuracy37,38,39,40,41. In our study, TCD showed the best correlation with ICP (r = 0.62) and the second-best ROC curve, with an AUC of 0.75, when corrected for its classic confounding variables such as vasospasm, fever, and anemia, keeping its significance after the multivariate analysis. Recently, a prospective, international, multicenter, unblinded, diagnostic accuracy study recruited two hundred and sixty-two patients in 16 international intensive care units. ICPi measurements (reference test) were compared to simultaneous ICPtcd measurements42 (index test) at three different timepoints: before, immediately after and 2 to 3 h following ICPi catheter insertion. The results showed an elevated NPV (ICP > 20 mmHg = 91.3%, > 22 mmHg = 95.6%, > 25 mmHg = 98.6%), indicating high discriminant accuracy of ICPtcd in excluding IH43.
In our study, we used the only CT scale created for ICH detection, which was developed in the original study by Miller et al.44 and later adapted by Rajajee et al.14 (Table 1). Miller evaluated 160 patients with Traumatic Brain Injury using ICPi monitoring to investigate if the five criteria observed predicted ICH. Although the binary logistic regression showed no significance, all factors were statistically significant in the linear regression. Based on this previous study, Rajajee et al. evaluated 65 patients diagnosed with SAH, TBI, intraparenchymal HS, and tumor. As in our study, most patients had at least one of the described signs (91.6% in our study and 77% in the cited study) related to ICH. The sensitivity of the original study to detect ICH with at least one radiological sign was 77% (CI95% 46–95%), specificity was 29% (17–45%), PPV was 24% (CI95% 12–40%), and NPV 81% (CI95% 54–96%). Such findings corroborate our results, with high sensitivity and NPV and low specificity and PPV for ICH prediction.
Only one previous publication evaluated the ability of multiple noninvasive methods to estimate ICH7. A total of 100 patients were evaluated (TBI = 30; SAH = 47; HS = 23) with invasive monitoring associated with ONSD, TCD (PI and ICP estimation formula [eICP]), and Pupillary Neurological Index (NPI) by automated pupillometry. All four methods showed moderate correlation with ICPi (ONSD, r = 0.54; PI, r = 0.50; eICP, r = 0.61; NPI, r = − 0.41, with p < 0.001 for all methods). The AUC to predict ICH was 0.78 for ONSD, 0.85 for PI, 0.86 for eICP, and 0.71 for NPI. With the combination of techniques, the highest AUC was 0.91 (0.84–0.97) with the combination of ONS and eICP. In a subgroup analysis, patients with SAH showed higher correlation with pupillometry (r = -0.77) and eICP (r = 0.88), and moderate correlation with ONS (r = 0.61) and PI (r = 0.53). The AUC to predict ICH in this subgroup was 0.78 for ONSUS, 0.79 for PI, 0.68 for eICP, and 0.70 for NPI. This study corroborates the concept that noninvasive techniques exhibit a satisfactory ICP correlation and a reasonable predictive accuracy for ICH particularly enhanced when multiple methods are employed in concert. In the whole group of patients, TCD and ONSD was the best combination, while in the SAH subgroup, NPI and TCD showed the best performance for ICH prediction. In our study, the combination of TCD and B4C had the best accuracy. We acknowledge the existence and importance of other relevant noninvasive methods besides the ones discussed in this paper and further discussion can be found elsewhere2,5,6.
Our study presents some limitations. First, it is a single-center study with few subjects (n = 18), although the number of measurements was reasonable (n = 60). Second, the time between admission and assessment varied among patients, as well as the interval between measurements in the same patient and among patients. Third, PaCO2 was not universally monitored as a confounding variable. Furthermore, the ONSD and TCD examiners were not blinded to the ICP measures. Finally, the correlations we observed between the various methods and ICP were characterized by modest to moderate strengths. This pattern is likely attributable to each method gauging distinct surrogates or proxies of intracranial hypertension, rather than directly quantifying ICP itself.
Conclusion
In conclusion, this exploratory study with noninvasive methods showed various degrees of correlation with ICP and discriminatory power for the diagnosis of ICH. The noninvasive wave morphology monitor and TCD (PI) had the best performances both isolated and combined. The multimodal combination of such indices may increase the ability to noninvasively identify and manage ICH. The observed diversity in estimated ICP through non-invasive measurements underscores the need for additional investigations to define the appropriateness of specific methods more precisely within distinct clinical scenarios.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ICH:
-
Intracranial hypertension
- SAH:
-
Subarachnoid hemorrhage
- IPH:
-
Intraparenchymal hemorrhage
- IS:
-
Ischemic stroke
- ICPi:
-
Invasive intracranial pressure
- ONS:
-
Optic nerve sheath
- ONSD:
-
Optic nerve sheath diameter
- ONSUS:
-
Optic nerve sheath ultrasound
- PI:
-
Pulsatility index
- TCD:
-
Transcranial Doppler
- CT:
-
Computed tomography
- TTP:
-
Time-to-peak
- B4c:
-
Brain4Care
- ICP:
-
Intracranial pressure
- ICPni:
-
Noninvasive intracranial pressure method
- HS:
-
Hemorrhagic stroke
- neuro-ICU:
-
Neurocritical care unit
- EVD:
-
External ventricular drainage
- MCA:
-
Middle cerebral artery
- ICC:
-
Intraclass correlation coefficient
- ROC:
-
Receiver operator characteristic
- AUC:
-
Area under the curve
- OR:
-
Odds ratio
- CC:
-
Cerebral compliance
- TBI:
-
Traumatic brain injury
- ICC:
-
Intracranial compliance
References
Heldt, T., Zoerle, T., Teichmann, D. & Stocchetti, N. Intracranial pressure and intracranial Elastance monitoring in Neurocritical care. Annu. Rev. Biomed. Eng. 21, 523–549 (2019).
Evensen, K. B. & Eide, P. K. Measuring intracranial pressure by invasive, less invasive or non-invasive means: Limitations and avenues for improvement. Fluids Barriers CNS Int 17(1), 1–33. https://doi.org/10.1186/s12987-020-00195-3 (2020).
Carney N, Totten AM, Reilly CO, et al. Guidelines for the management of severe traumatic brain injury 4th edition. (2016)
Chesnut, R. M. et al. A trial of intracranial-pressure monitoring in traumatic brain injury. N. Engl. J. Med. 367(26), 2471–2481 (2012).
Nag, D. S., Sahu, S., Swain, A. & Kant, S. Intracranial pressure monitoring: Gold standard and recent innovations. World J. Clin. Cases 7(13), 1535–1553 (2019).
de Moraes, F. M. & Silva, G. S. Noninvasive intracranial pressure monitoring methods: A critical review. Arq. Neuropsiquiatr. 79(5), 437–446 (2021).
Robba, C. et al. Multimodal non-invasive assessment of intracranial hypertension: An observational study. Crit. Care 24(1), 1–10 (2020).
Cabella, B. et al. Validation of a new noninvasive intracranial pressure monitoring method by direct comparison with an invasive technique. Acta Neurochir. Suppl. 122, 93–96 (2016).
de Moraes, F. M. et al. Waveform morphology as a surrogate for ICP monitoring: A comparison between an invasive and a noninvasive method. Neurocrit. Care Int. https://doi.org/10.1007/s12028-022-01477-4 (2022).
Harary, M., Dolmans, R. G. F. & Gormley, W. B. Intracranial pressure monitoring—review and avenues for development. Sens. Switz. 18(2), 3–7 (2018).
Brasil, S. et al. A novel noninvasive technique for intracranial pressure waveform monitoring in critical care. J. Personal. Med. 11(12), 1302 (2021).
Price, D. A. et al. Review of non-invasive intracranial pressure measurement techniques for ophthalmology applications. British J. Ophthalmol. 104(7), 887–892 (2020).
Bellner, J. et al. Transcranial Doppler sonography pulsatility index (PI) reflects intracranial pressure (ICP). Surg. Neurol. 62(1), 45–51 (2004).
Rajajee, V., Vanaman, M., Fletcher, J. J. & Jacobs, T. L. Optic nerve ultrasound for the detection of raised intracranial pressure. Neurocrit. Care 15(3), 506–515 (2011).
Andrade, R. D. A. P. et al. A Nanometer resolution wearable wireless medical device for Non invasive intracranial pressure monitoring. IEEE Sens. J 21(20), 22270–22284 (2021).
Bakdash, J. Z. & Marusich, L. R. Repeated measures correlation. Front. Psychol. 7(8), 456 (2017).
Liu, H. & Wu, T. Estimating the area under a receiver operating characteristic (ROC) curve for repeated measures design Honghu Liu 1 and Tongtong Wu 2. J. Stat. Softw. 8(12), 1–18 (2003).
Eide, P. K. & Sorteberg, W. Association among intracranial compliance, intracranial pulse pressure amplitude and intracranial pressure in patients with intracranial bleeds. Neurol. Res. 29(8), 798–802 (2007).
Eide, P. K. The correlation between pulsatile intracranial pressure and indices of intracranial pressure-volume reserve capacity: Results from ventricular infusion testing. J. Neurosurg. 125(6), 1493–1503 (2016).
Wagshul, M. E., Eide, P. K. & Madsen, J. R. The pulsating brain: A review of experimental and clinical studies of intracranial pulsatility. Fluids Barriers CNS 8(1), 1–23 (2011).
Fan, J. Y., Kirkness, C., Vicini, P. & Burr, R. M. P. Intracranial pressure waveform morphology and intracranial adaptive capacity. Am. J. Crit. Care 6, 545–556 (2008).
Kazimierska, A. et al. Compliance of the cerebrospinal space: comparison of three methods. Acta Neurochirurgica. 163, 1979–1989 (2021).
Ballestero, M. et al. Can a new noninvasive method for assessment of intracranial pressure predict intracranial hypertension and prognosis?. Acta Neurochir. Wien 165(6), 1495–1503 (2023).
Brasil S, Godoy DA. A new noninvasive method can effectively assess intracranial compliance. Letter to the Editor. Acta Neurochir. (Wien). (2023)
Hansen, H. C. & Helmke, K. Validation of the optic nerve sheath response to changing cerebrospinal fluid pressure: Ultrasound findings during intrathecal infusion tests. J. Neurosurg. 87(1), 34–40 (1997).
Geeraerts, T. et al. Ultrasonography of the optic nerve sheath may be useful for detecting raised intracranial pressure after severe brain injury. Intensive Care Med. 33(10), 1704–1711 (2007).
Kimberly, H. H., Shah, S., Marill, K. & Noble, V. Correlation of optic nerve sheath diameter with direct measurement of intracranial pressure. Acad. Emerg. Med. 15(2), 201–204 (2008).
Geeraerts, T., Merceron, S., Benhamou, D., Vigué, B. & Duranteau, J. Non-invasive assessment of intracranial pressure using ocular sonography in neurocritical care patients. Intensiv. Care Med. 34(11), 2062–2067 (2008).
Soldatos, T. et al. Optic nerve sonography in the diagnostic evaluation of adult brain injury. Crit. Care 12(3), 1–7 (2008).
Kim, S. E., Hong, E. P., Kim, H. C., Lee, S. U. & Jeon, J. P. Ultrasonographic optic nerve sheath diameter to detect increased intracranial pressure in adults: A meta-analysis. Acta Radiol. 60(2), 221–229 (2019).
Zoerle, T. et al. Optic nerve sheath diameter is not related to intracranial pressure in subarachnoid hemorrhage patients. Neurocrit. Care Int. https://doi.org/10.1007/s12028-020-00970-y (2020).
Bäuerle, J., Niesen, W. D., Egger, K., Buttler, K. J. & Reinhard, M. Enlarged optic nerve sheath in aneurysmal subarachnoid hemorrhage despite normal intracranial pressure. J. Neuroimag. 26(2), 194–196 (2016).
Hansen, H. C., Lagrèze, W., Krueger, O. & Helmke, K. Dependence of the optic nerve sheath diameter on acutely applied subarachnoidal pressure—An experimental ultrasound study. Acta Ophthalmol. 89(6), 528–532 (2011).
Rouanet, C. & Silva, G. S. Aneurysmal subarachnoid hemorrhage: Current concepts and updates. Arq. Neuropsiquiatr. 77(11), 806–814 (2019).
Prunell, G. F. et al. Experimental subarachnoid hemorrhage: Subarachnoid blood volume, mortality rate, neuronal death, cerebral blood flow, and perfusion pressure in three different rat models. Neurosurgery 52(1), 165–176 (2003).
Cardim, D. et al. Non-invasive monitoring of intracranial pressure using transcranial Doppler ultrasonography: Is it possible?. Neurocrit. Care 25(3), 473–491 (2016).
De Riva, N. et al. Transcranial doppler pulsatility index: What it is and what it isn’t. Neurocrit Care 17(1), 58–66 (2012).
Zweifel, C. et al. Reliability of the blood flow velocity pulsatility index for assessment of intracranial and cerebral perfusion pressures in head-injured patients. Neurosurgery. 71(4), 853–861 (2012).
Figaji, A. A., Zwane, E., Fieggen, A. G., Siesjo, P. & Peter, J. C. Transcranial Doppler pulsatility index is not a reliable indicator of intracranial pressure in children with severe traumatic brain injury. Surg. Neurol. Int. 72(4), 389–394. https://doi.org/10.1016/j.surneu.2009.02.012 (2009).
Behrens, A. et al. Transcranial doppler pulsatility index: Not an accurate method to assess intracranial pressure. Neurosurgery 66(6), 1050–1057 (2010).
Hanlo, P. W. et al. Value of transcranial Doppler indices in predicting raised ICP in infantile hydrocephalus—A study with review of the literature. Child’s Nerv. Syst. 11(10), 595–603 (1995).
Rasulo, F. A. et al. The accuracy of transcranial Doppler in excluding intracranial hypertension following acute brain injury: A multicenter prospective pilot study. Crit. Care 21(1), 1–8 (2017).
Rasulo, F. A. et al. Transcranial Doppler as a screening test to exclude intracranial hypertension in brain-injured patients: the IMPRESSIT-2 prospective multicenter international study. Crit. Care. 1, 1–2. https://doi.org/10.1186/s13054-022-03978-2 (2022).
Miller, M. T. et al. Initial head computed tomographic scan characteristics have a linear relationship with initial intracranial pressure after trauma. J. Trauma. Inj. Infect. Crit. Care 56(5), 967–973 (2004).
Acknowledgements
We would like to thank Prof. Eduardo Leite Vieira Costa for the assistance regarding the repeated correlations and ROC curves.
Funding
Brain4care provided the monitor and a fee for the translation of this article.
Author information
Authors and Affiliations
Contributions
We confirm that authorship requirements have been met and the final manuscript was approved by all authors. Conception and Design of the work: F.M.M., F.G.R.F., F.E.A.C.N., G.S.S. Acquisition of data: F.M.M., E.A., E.R., F.C.D.B., M.M., R.A.V., J.B.C.A. Interpretation of data: F.M.M., F.G.R.F., F.E.A.C.N., G.S.S. Drafted and revised the work: F.M.M., G.S.S. We confirm that all authors have agreed both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. We confirm adherence to ethical guidelines and indicate ethical approvals (IRB) and use of informed consent, as appropriate.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de Moraes, F.M., Adissy, E.N.B., Rocha, E. et al. Multimodal monitoring intracranial pressure by invasive and noninvasive means. Sci Rep 13, 18404 (2023). https://doi.org/10.1038/s41598-023-45834-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-45834-5
This article is cited by
-
ICP wave morphology as a screening test to exclude intracranial hypertension in brain-injured patients: a non-invasive perspective
Journal of Clinical Monitoring and Computing (2024)
-
Noninvasive neuromonitoring in acute brain injured patients
Intensive Care Medicine (2024)
-
Noninvasive Intracranial Pressure Monitoring: Are We There Yet?
Neurocritical Care (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.