Abstract
Molluscum contagiosum presenting as a periorbital region abscess is unusual. The virus generally causes a self-limiting localized disease in children. Presentation as an abscess has been reported mainly in immunocompromised patients. We performed a retrospective study of ten children treated for Molluscum contagiosum infection presenting as periorbital abscess. Data investigated included age, immunocompetence, systemic antibiotic treatment, clinical findings, and histopathology. All children were immunocompetent. Bacterial cultures taken in six of the ten children were positive in two. Seven patients received oral antibiotics before presentation but required IV antibiotics on admission. One patient received IV antibiotics only. All antibiotic treatment had very limited effect. Two patients had no antibiotic treatment. CT imaging in one case where orbital cellulitis was suspected showed no significant intraorbital findings with anterior involvement only. Nine out of ten children had surgery and intra-operative cryotherapy at our center with immediate improvement and recovery. One child whose parents initially refused surgical excision had initial limited clinical improvement of periorbital swelling with antibiotics. However, the lesions were excised shortly following discharge from our hospital at another medical center with a complete cure. Molluscum is a cause of periorbital abscess in immunocompetent children which should be part of the differential diagnosis in periorbital/adnexal infection. Antibiotic treatment has a limited effect, and the abscess is most likely a virally triggered reaction. Surgical excision and intra-operative cryotherapy are curative of the disease in our experience.
Similar content being viewed by others
Introduction
Molluscum contagiosum is a common benign viral infection seen commonly in children. The disease is caused by a double stranded DNA virus of the Poxviridae family. Molluscum infects the human epidermis causing dome-shaped papules with an average diameter of 3–5 mm1,2. The infection is transmitted by contact with infected people or contaminated objects1. Several studies have shown a greater prevalence and higher number of lesions in patients with atopic dermatitis3,4 that may be explained by the immunologic changes and an impaired skin barrier in this disease. Molluscum is typically more severe with larger and more disseminated lesions in immunocompromised patients1.
In immunocompetent patients, lesions regress spontaneously over time in most cases1,2,3,4,5. Spontaneous regression of Molluscum lesions is generally accompanied by signs of inflammation including perilesional erythema5.
The diagnosis of Molluscum is based on physical examination with observation of the typical umbilicated papules. Dermatoscopy can aid diagnosis in some cases by identifying the punctiform, radial, or “mixed flower” patterns of the lesion vasculature6. The definitive diagnosis is made by biopsy and histopathology2.
Molluscum lesions may spontaneously resolve without treatment. While most cases resolve within six to nine months, some may persist for years7.
Periocular Molluscum lesions frequently affect the eyelid margins or the area near the palpebral aperture and may cause secondary unilateral follicular conjunctivitis or superficial punctate keratitis8.
Although periocular lesions may be self-limited with no need for intervention beyond conservative management, it is important to understand that the disease can also take an aggressive form. In some cases, eczematous reactions, pruritus, pain, discomfort, superinfection and hypersensitivity may appear9. Several reports and studies have suggested different therapies including topical, systemic and surgical interventions.
There are few reports of Molluscum presenting as periorbital abscess or eyelid cellulitis10,11. However, in one large series of 578 cases from all over the body including the head and neck, abscesses were present in about 11% of the patients12. It is not specified in that paper how many cases of abscesses were from the head and neck region or how many abscesses were in children. Abscesses are considered to be caused by discharge of Molluscum bodies to the dermis and the consequent release of proinflammatory cytokines with complement pathway activation. This is thought to induce a neutrophil reaction and abscess formation13,14. Our case series involves ten pediatric cases of aggressive Molluscum infection in immunocompetent children presenting as abscesses of the eyelid and anterior orbit. This would suggest that infections of the eyelids and periorbita caused by Molluscum could be more common than previously accepted in young children and clinical examination should always exclude it as a cause.
Methods
We performed a retrospective review of ten pediatric patients suffering from eyelid Molluscum with abscess formation treated or examined at Emek Medical Center in Israel.
The study was permitted by the Emek Medical Center (EMC) ethics committee review board. Methods were carried out in accordance with relevant guidelines and regulations. Experimental protocols were approved by the EMC ethics committee review board. Waiver of informed consent was permitted by EMC ethics committee review board as the research was retrospective and anonymous, and information is not sensitive in nature presenting no threat to the rights and welfare of research subjects. Necessary informed consent was obtained from all parents or legal guardians for publication of identifying information and images.
Each patient presented with classical Molluscum lesions of the face and various parts of the body in addition to deep eyelid and orbital abscesses. Data including age, immunocompetence, treatment with antibiotics at the period of presentation, clinical findings and follow-up, histopathology, and bacterial culture results were reviewed.
All cases had a complete blood count and there was no leucopoenia or any irregularity implying immunodeficiency. All cases had normal development and weight gain. In Israel it is mandatory to check every woman during pregnancy for HIV. In addition, all newborns are screened by a mandatory blood test for SCID (Severe Combined Immunodeficiency). Every case in our cohort was screened negatively for any history of immunodeficiency, including the data discussed above, in addition to negative history of any symptoms, admissions or treatments connected to immunodeficiency. None of the children have systemic atopies. The cases were not screened for HIV as there was no medical indication.
Results
A total of ten cases of periorbital abscess and eyelid cellulitis caused by Molluscum contagiosum in immunocompetent children were included in our cohort (Table 1). Age ranged between 1 and 9 years old. There were seven boys and three girls, and all cases were admitted to hospital because of worsening signs and symptoms of infection despite antibiotic treatment given in eight of the ten cases. No similar adult cases presented, and this clinical picture was only seen in children. CT imaging was carried out in one out of ten cases, but there was no significant intraconal involvement of the abscess (Fig. 1).
The children presented with large, expanding lesions and cellulitis of the eyelids and periorbita, which were concerning (Fig. 2).
There was localized pain and periorbital swelling with erythema, and in all cases, there were characteristic lesions on other parts of the body including the face, ears, trunk, arms, and genitalia. None of the children presented with restricted eye movements, severe orbitopathy, or clinical signs of serious disseminated infection such as fever, chills, nausea, vomiting, or diarrhea.
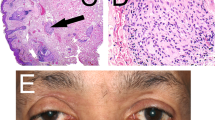
Blood analysis was normal in all but two of the cases, which showed lymphocytosis and neutrophilia. Although cultures were taken in six of the children, no bacteria were isolated in four of these cases. Two children had positive bacterial isolates (case 3 with Staphylococcus and case 6 with Heamophilus). Despite a negative bacterial culture, the child whose parents initially refused surgical excision of the Molluscum clinically improved with IV antibiotics, while the children with positive cultures had very limited clinical improvement with IV antibiotics. All ten children continued to surgical excision despite antibiotics. Histopathology demonstrated Molluscum in all nine of the ten patients who had surgery at our center, confirming the clinical diagnosis (Fig. 3). The tenth child underwent operation at another center and there is no histopathological confirmation of the clinical diagnosis.
Treatment with oral antibiotics or local antibiotic ointment was ineffective in all relevant cases. IV antibiotic therapy was ineffective in all but one case, where cellulitis was reduced in the eyelids, although the Molluscum lesion remained smoldering and were excised one week later at another facility. In all patients receiving antibiotic treatment, there was a limited effect only. Surgical excision of the viral lesions gave immediate resolution and cure (Fig. 4).
In all nine cases operated in our center, there was a substantial amount of characteristic white viral tissue, and surprisingly less pus than expected. The lesions invaded through the septum into the anterior orbital fat causing orbital edema and cellulitis.
All children recovered rapidly, and all signs and symptoms completely disappeared within a week of follow-up.
Discussion
This case series of Molluscum periocular/adnexal abscess is distinctive in that it includes exclusively immunocompetent children only. There were no adult cases. Most cases in the literature of Molluscum with abscess formation are reported in children with immunodeficiency or HIV infection whereas all of our cases were immunocompetent15,16,17. Alrajeh et al. reported a case of an ulcerating eyelid Molluscum infection in an immunocompetent child that was surgically treated with complete cure11. We also had positive bacterial cultures in some cases as opposed to most of the literature, which describes positive bacterial culture mostly in immunocompromised patients. All children in our case series underwent surgery giving immediate improvement and cure of the disease. Published case series generally describe Molluscum in populations of all ages and include the whole body. One large case series described the presentation of abscesses in approximately 11% of Molluscum in their cohort, although they did not specify how many abscesses involved the head and neck or periocular region specifically12. Their cohort included patients of all ages. They estimated that only about 40% of Molluscum cases with abscess were clinically diagnosed. It would seem that the abscesses are virally induced. Molluscum with abscess was easily diagnosed clinically in all of our pediatric cases due to additional characteristic lesions elsewhere on the body. The abscesses can initially be misdiagnosed as bacterial abscesses when in fact they are actually virally induced reactive abscesses most probably caused by proinflammatory cytokines and complement pathway activation13,14. Some lesions may have had secondary bacterial infiltration from scratching, but this is unlikely to be the cause of the deep inflammatory infectious reaction observed. Broad-spectrum antibiotics had minimal effect on the abscesses in the cases where bacterial cultures were positive, and no cases had clinical systemic signs or symptoms. Surgical excision has an immediate curative effect, and although coverage with antibiotic may be indicated, its effect is limited at best in our experience.
Early periocular Molluscum literature described the disease in immunosuppressed patients, correlating indirectly with CD4 count. Molluscum, however, is most commonly seen in immunocompetent pediatric patients1. While aggressive Molluscum lid abscess is known to present in immunosuppressed patients15,16,17, its presentation in the immunocompetent pediatric population is typically less severe than in our cases2. It is possible, but unlikely, that the novel presentation of Molluscum with abscess, as in our cases, represents a new Molluscum virus variant. This hypothesis would need to be assessed by genetic testing in future presentations of the disease. Characteristic small, self-resolving papules are found in most immunocompetent children, as opposed to our case series, where Molluscum presented as painful, persistent, and aggressive periocular abscesses. Örnek et al. have already suggested the differential diagnosis of periocular infection in children should always include Molluscum, a diagnosis that can sometimes be evasive18.
Co-infection has been previously reported mainly in immunosuppressed patients15,16,17, although we think it is likely that the bacterial infection is mostly insignificant in immunocompetent cases such as ours. However, due to the gravity of complications that can occur with a periorbital abscess, it is very difficult not to give antibiotic cover to these children.
From our experience, it is likely that CT or MRI orbital imaging in immunocompetent children is unnecessary before surgery in cases of Molluscum abscess, as they do not penetrate into the intraconal fat space.
It has been well established that surgical removal or cryodestruction of the viral core are highly effective modes of treatment for Molluscum9,18,19,20. Periorbital Molluscium abscess has the potential to cause significant morbidity and therefore timely surgical intervention is probably the best mode of management even when antibiotic treatment has begun. We suggest that in these cases surgery should be scheduled as soon as possible.
Data availability
The dataset generated and analyzed during the current study is not publicly available, as we accessed patient information through the hospital database. The hospital database is not publicly available and is protected by privacy laws. Data can be made available from the corresponding author on reasonable request.
References
Chen, X., Anstey, A. V. & Bugert, J. J. Molluscum contagiosum virus infection. Lancet. Infect. Dis 13(10), 877–888 (2013).
Rosner, M. & Zloto, O. Periocular molluscum contagiosum: Six different clinical presentations. Acta Ophthalmol. 96(5), e600–e605 (2018).
Kakourou, T. et al. Molluscum contagiosum in Greek children: A case series. Int. J. Dermatol. 44(3), 221–223 (2005).
Osio, A. et al. Clinical characteristics of molluscum contagiosum in children in a private dermatology practice in the greater Paris area, France: A prospective study in 661 patients. Dermatology (Basel, Switzerland) 222(4), 314–320 (2011).
Vermi, W. et al. Spontaneous regression of highly immunogenic Molluscum contagiosum virus (MCV)-induced skin lesions is associated with plasmacytoid dendritic cells and IFN-DC infiltration. J. Investig. Dermatol. 131(2), 426–434 (2011).
Vázquez-López, F. et al. Dermoscopic semiology: Further insights into vascular features by screening a large spectrum of nontumoral skin lesions. Br. J. Dermatol. 150(2), 226–231 (2004).
van der Wouden, J. C. et al. Interventions for cutaneous molluscum contagiosum. Cochrane Database Syst. Rev. 5(5), CD004767 (2017).
Mutalik, S. D. & Rasal, Y. D. Successful use of oral acyclovir in ophthalmic molluscum contagiosum. Indian Dermatol. Online J. 10(4), 456–459 (2019).
Brown, J. et al. Childhood molluscum contagiosum. Int. J. Dermatol. 45(2), 93–9 (2006).
Örnek, K., Onaran, Z. & Koçak, M. Giant eyelid molluscum contagiosum presenting as preseptal cellulitis. J. Paediatr. Child Health 50(12), 1036. https://doi.org/10.1111/jpc.12530 (2014).
Alrajeh, M., Alessa, D., Maktabi, A. M. & AlAlsheikh, O. Eyelid molluscum contagiosum presenting as a giant solitary ulcerating mass. Saudi J. Ophthalmol. Off. J. Saudi Ophthalmol. Soc. 32(4), 338–340. https://doi.org/10.1016/j.sjopt.2018.01.005 (2018).
Cribier, B., Scrivener, Y. & Grosshans, E. Molluscum contagiosum: Histologic patterns and associated lesions. A study of 578 cases. Am. J. Dermatopathol. 23(2), 99–103. https://doi.org/10.1097/00000372-200104000-00003 (2001).
Takematsu, H. & Tagami, H. Proinflammatory properties of molluscum bodies. Arch. Dermatol. Res. 287(1), 102–106. https://doi.org/10.1007/BF00370727 (1994).
Brandrup, F. & Asschenfeldt, P. Molluscum contagiosum-induced comedo and secondary abscess formation. Pediatr. Dermatol. 6(2), 118–121. https://doi.org/10.1111/j.1525-1470.1989.tb01008.x (1989).
Schwartz, J. J. & Myskowski, P. L. Molluscum contagiosum in patients with human immunodeficiency virus infection. A review of twenty-seven patients. J. Am. Acad. Dermatol. 27(4), 583–588. https://doi.org/10.1016/0190-9622(92)70226-6 (1992).
Biswas, J., Therese, L., Kumarasamy, N., Solomon, S. & Yesudian, P. Lid abscess with extensive molluscum contagiosum in a patient with acquired immunodeficiency syndrome. Indian J. Ophthalmol. 45, 234–236 (1997).
Boudreau, S. et al. Dermal abscesses with Staphylococcus aureus, cytomegalovirus and acid-fast bacilli in a patient with acquired immunodeficiency syndrome (AIDS). J. Cutaneous Pathol. 15(1), 53–57. https://doi.org/10.1111/j.1600-0560.1988.tb00517.x (1988).
Gonnering, R. S. & Kronish, J. W. Treatment of periorbital Molluscum contagiosum by incision and curettage. Ophthalmic Surg. 19(5), 325–327 (1988).
Meza-Romero, R., Navarrete-Dechent, C. & Downey, C. Molluscum contagiosum: An update and review of new perspectives in etiology, diagnosis, and treatment. Clin. Cosmet. Investig. Dermatol. 12, 373–381. https://doi.org/10.2147/CCID.S187224 (2019).
Leung, A., Barankin, B. & Hon, K. Molluscum contagiosum: An update. Recent Patents Inflamm. Allergy Drug Discov. 11(1), 22–31. https://doi.org/10.2174/1872213X11666170518114456 (2017).
Acknowledgements
All authors have participated in (a) conception and design, or analysis and interpretation of the data; (b) drafting the article or revising it critically for important intellectual content; and (c) approval of the final version. This manuscript has not been submitted to, nor is under review at, another journal or other publishing venue. The authors have no affiliation with any organization with a direct or indirect financial interest in the subject matter discussed in the manuscript.
Author information
Authors and Affiliations
Contributions
M.M.S. conducted data collection through a retrospective chart review, finding and summarizing relevant patient cases, and contributed to writing the manuscript. J.G. searched relevant literature, assisted with chart review, and wrote the original manuscript. O.L. assisted with retrospective chart review of relevant patient cases, data extraction, and contributed to reviewing and editing the manuscript. J.K. provided Molluscum histological images and analysis. D.B. was the mentor who initiated the paper, supervised every step of the research effort, and was involved with writing and editing the manuscript. M.M.S. and J.G. contributed equally, and should both be listed as first authors. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mor-Shaham, M., Gutovitz, J., Levinkron, O. et al. Molluscum contagiosum presenting as periorbital abscess in immunocompetent children. Sci Rep 13, 18059 (2023). https://doi.org/10.1038/s41598-023-45320-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-45320-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.