Abstract
The purpose of this cross-sectional study was to examine the association between ultra-processed foods (UPFs) intake and lipid profile in Iranian people. The study was performed on 236 individuals with the age range of 20–50 years in Shiraz, Iran. Food intakes of the participants were evaluated using a 168-item food frequency questionnaire (FFQ) which was previously validated in Iranian populations. In order to estimate the ultra-processed foods intake, classification of NOVA food group was used. Serum lipids including total cholesterol (TC), triglyceride (TG), high density lipoprotein cholesterol (HDL-C) and low density lipoprotein cholesterol (LDL-C) were measured. The results showed that mean of age and body mass index (BMI) of the participants were 45.98 years and 28.28 kg/m2, respectively. Logistic regression was used to evaluation the relation between UPFs intake and lipid profile. Higher UPFs intake was associated with increased OR of TG and HDL abnormality in both crude (OR 3.41; 95% CI 1.58, 7.34; P-trend = 0.001 and OR 2.99; 95% CI 1.31, 6.82; P-trend = 0.010) and adjusted models (OR 3.69; 95% CI 1.67, 8.16; P-trend = 0.001 and OR 3.38 95% CI 1.42, 8.07; P-trend = 0.009). But, there were no association between UPFs intake and other indices of lipid profile. Also, we found significant associations between UPFs intake and dietary nutrient profiles. In conclusion, UPFs consumption could worsen the nutritional profile of the diet and lead to negative changes in some indices of the lipid profile.
Similar content being viewed by others
Introduction
Dyslipidemia is defined as any lipid abnormality including elevated total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C) and triglycerides (TG), and declined high-density lipoprotein cholesterol (HDL-C)1. Prevalence of hypertriglyceridemia, hypercholesterolemia, high non-HDL, and low HDL in Iranian adults are 28%, 26.7%, 39.5,% and 69.2% respectively2.
Abnormalities of lipid profile are associated with many clinical outcomes such as type 2 diabetes and cardiovascular diseases (CVDs). It is also the main cause of more than half of the cases of congenital heart disease and more than four million deaths annually3. There is a complex interaction between genetic factors and several environmental factors such as smoking, sedentary lifestyle, and socioeconomic situation as determinants of lipid profile4. Particularly taking foods rich in calories, carbohydrates, sodium, cholesterol, trans and saturated fatty acids are related to the high concentration of TC and LDL-C. On the other hand, consumption of polyunsaturated fatty acids, vegetables, dietary fibers, milk, and dairy products could decrease the risk of dyslipidemia5.
Nova classification system by considering physical, biological, chemical properties of the foods, also the additives for food manufacturing, classifies foods into different groups, including unprocessed and minimally processed food, processed culinary ingredients, processed foods and ultra-processed foods. UPFs are intrinsically fatty, sugary or salty, high calorie, and poor in protein, dietary fiber, micronutrients, and other bioactive compounds, and usually contain no or small amount of whole foods6,7. UPFs contain soft drinks; sweets like chocolate, candies, ice cream, biscuits and cakes; packaged leaves of bread; nugget and sticks, margarine, pastries; pre-prepared food dishes, and many other products8.
Evidence also showed that high consumption of UPFs is potentially related to the high rate of obesity and related comorbidities9. Assessment of UPFs’ effects on lipid profiles and upcoming diseases is an ongoing debate. Most studies reported a positive association of UPFs intake with lipid abnormalities, altered blood lipid factors varies in the studies. While, some reported association between UPFs intake with elevated TG and lower HDL-C10,11,12, others reported positive association of UPFs consumption with high LDL and total cholesterol13,14. As UPFs production and consumption have increased extremely during the last decades, comprehending their potential effects on human health has become a major concern in health care systems. The purpose of this cross-sectional study was to examine the association between UPFs intake and lipid profile in Iranian adults. In addition, as secondary outcomes, we examined the association of UPFs consumption with the intake of food subgroups, macronutrients, and some of the micronutrients. To the best of our knowledge, no previous study has investigated the association between UPFs intake and lipid profile in Iranian adults.
Methods
Study population
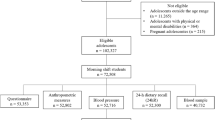
This cross-sectional study was performed on 236 individuals with the age range of 20–50 years who were selected by cluster random sampling in health care centers of Shiraz-Iran (Fig. 1). For this purpose, Shiraz was divided in four clusters and one health care center was randomly selected in each cluster. Study sample size was calculated by the following formula, in which α = 0.01, β = 0.10 and r = ± 0.25.
Prerequisites for participating in this study were no history of chronic diseases and no adherence to any special diet (The detailed of this study have been previously published15,16). Written consent form was signed by all participants. The protocol of this study was authorized by Shiraz University of Medical Sciences (IR.SUMS.REC.1394.S146).
Dietary assessment
Food intakes of the participants were evaluated by a 168-item food frequency questionnaire (FFQ) which was previously validated in Iranian populations17. The FFQ was filled out based on family food intakes and data was changed to gram. For computing energy, and nutrients intakes we used NUTRITIONIST IV (version 7.0; N-Squared Computing, Salem, OR, USA).
To estimate the ultra-processed foods intake, classification of NOVA food group was used8,18. Accordingly, total daily consumption of some foods and beverages items were considered as ultra-processed food (including: packaged breads, buns, confectionaries, pastries and sweets, ice cream, biscuits, cakes, soft drinks, industrial fruit drinks, sweetened milk-based beverages, margarine, sauces, dressings, processed meats, fries, and salty snacks19). To define the contribution of every food group to overall consumption of ultra-processed foods, the mean daily intake of every 9 subgroups of ultra-processed foods (dairy products, non-dairy beverages, margarine and sauces, cakes and cookies, chips and snacks, breads, fast foods and meats, sweets and others) was divided by daily consumption of ultra-processed foods, then multiplied by 100.
Biochemical assessments
Serum lipids including TC, TG, HDL-C and LDL-C were measured in blood samples (5 cm3) taken from the participants commercially accessible enzyme kits (Pars Azmoon, Tehran, Iran).
Socio-demographic and anthropometric assessments
Sex, age, smoking habit and alcohol intake were evaluated by using a questionnaire. Also we used International Physical Activity Questionnaire (IPAQ)20 to assess physical activity level of the participants. Anthropometric indices [weight (kg), waist circumference (cm) and height (cm)] were measured. Then, according to weight and height, BMI was calculated.
Statistical analysis
All analysis was done using SPSS for windows (version 20.0, SPSS Inc. Chicago IL, USA). The level of significance was P-value < 0.05. Normal distribution of the variables was checked by Kolmogorov–Smirnov test. The relationship between quantitative variables and qualitative variables was evaluated by analysis of variance test and Chi-square test respectively. Crude and adjusted models of logistic regression were used to evaluate the relation between UPFs score with anthropometric index and lipid profile. In adjusted models, the effects of age, energy intake, physical activity, BMI, sex and smoking history were controlled. We dichotomized lipid profile and anthropometric indices then LDL-C more than 130 mg/dL, HDL-C less than 40 mg/dL for male and 50 mg/dL for female, TC more than 200 mg/dL, TG more than 150 mg/dL, non-HDL more than 130 and WC more than 88 cm for female and 102 for male were considered as abnormal16,21,22,23,24.
Ethical approval
The present study was approved by The Research Ethics Committee of Shiraz University of Medical Sciences, Shiraz, Iran (IR.SUMS.REC.1394.S146).
Use of human participants
All experiments were performed in accordance with relevant guidelines and regulations.
Informed consent
All participants singed informed consent form.
Results
As shown in Table 1, mean age and BMI of study population were 45.97 years and 28.28, respectively kg/m2. Also, 58.90% of the study participants were female. According to Table 2 there was no significant difference between age, weight, height, BMI, waist circumference, WHR, TC, LDL, HDL, Non-HDL, physical activity, sex, smoking habits, alcohol intake history and education of the participants in the first and last tertile of UPFs, intake, but the difference was significant for mean of serum TG (P = 0.015).
Compared to the first tertile, individuals in the last tertile of UPFs intake had higher consumption of energy (P = 0.008), carbohydrate (P = 0.028), fat (P = 0.002), cholesterol (P = 0.023), SFA (P = 0.004), MUFA (P = 0.001), PUFA (P = 0.005), vitamin B12 (P = 0.013) and vitamin C (P = 0.027). But, we observed no significant association between intake of vitamin B6, B9, C, calcium, magnesium, zinc and selenium with UPFs intake (Table 3).
As presented in Table 4, participants in the last tertile of UPFs intake had significantly higher intakes of processed and red meat (P = 0.007) and breads (P = 0.022), also lower intake of margarine and sauces (P < 0.001). There were no differences in non-dairy beverages, cookies and cakes, dairy products, potato chips and salty snacks, sweets and other food items intakes among the UPFs tertiles.
We found that, higher UPFs intake was associated with increased OR of serum TG and HDL abnormality in both crude (OR 3.41; 95% CI 1.58, 7.34; P-trend = 0.001 and OR 2.99; 95% CI 1.31, 6.82; P-trend = 0.010) and adjusted model (OR 3.69; 95% CI 1.67, 8.16; P-trend = 0.001 and OR 3.38 95% CI 1.42, 8.07; P-trend = 0.009) (Table 5).
Discussion
We found that higher intake of UPFs was associated with elevated lipid profile abnormality including TG and HDL. In terms of other blood lipids such as TC, LDL and non-HDL, while they were not significantly associate with UPFs intake, all were higher in last tertile of UPFs intake.
In agreement with our study, Lima et al. reported that higher UPFs consumption was associated with higher TG and lower HDL-C levels25. Furthermore, a large cohort of older adults in Spain found the same results10, and a systematic review and meta-analysis resulted in a negative association between UPFs consumption and HDL-cholesterol levels12. On the other hand, a cross-sectional study on Ecuadorian adolescents showed that dietary patterns consisted of processed foods were associated with an increased level of LDL and cholesterol13. Also, a longitudinal study in Brazil on preschool children found that intake of UPFs was a predictor of higher total cholesterol and LDL cholesterol but not HDL and TG probably because effects of food habits on serum LDL and total cholesterol in children are stronger than its effects on other dyslipidemia markers14.
We found a strong association between the dietary contribution of UPFs and the dietary content of energy, carbohydrates, fat, cholesterol, and SFAs. Moreover, intake of MUFAs and PUFAs increased parallel to UPFs consumption, probably due to high fat content of the UPFs.
With regard to anthropometric indices, although WC and WHR were not significantly associated with UPFs intake, participants in the last tertile of UPFs had higher mean of WC and WHR. Findings of some cohort studies, indicated that higher UPFs intake was associated with greater adiposity accumulation, higher BMI, weight gain and incidence of obesity26,27,28. Besides, another cohort study on overweight and obese participants aged 55–75 years reported that higher UPFs intake was associated with higher age-related increase in visceral and overall adiposity29. Another similar study also showed a positive association between UPFs intake and the incidence of abdominal obesity in adults30. A systematic review and meta-analysis and a multi-national cohort study also reported positive associations between higher consumption of UPFs and general and abdominal obesity12,31. We assume that our opposite findings is due to the high mean of our participants’ weight, WHR, and WC.
UPFs are often calorie-dense, contain large amounts of fats, saturated fats, trans fats, sodium, and simple sugars with high glycemic index and contain no or small amount of fibers, vitamins, minerals, or other bioactive compounds which naturally exist in fresh foods, so they are nutritionally unbalanced32.
Several mechanisms have been suggested to explain the adverse effects of UFPs on lipid profile and health. First of all, due to their intrinsic palatability, overconsumption of UPFs may result in physiological disruption of hunger and satiety patterns33,34,35,36. Besides, energy-dense foods usually contain high amounts of free sugar and trans fats which enhance lipogenesis, and decrease fatty acids oxidation which lead to their aggregation in tissues and blood circulation and elevated LDL level37. Furthermore, partially hydrogenated vegetable oils content of UPFs contain trans fatty acids which have adverse impacts on lipid profile. In addition, scientific evidence support the hypothesis that the interacting effects of substances produced through the high-heat processing of oils, determine their health effects38. Heat processing also causes degradation of food substances and formation of furans in UPFs39. Higher intake of UPFs increase exposure to phthalates which is used in the packing process and could transfer to food40. The accumulation of phthalates, bisphenols, furans, and their metabolites may ultimately lead to lower HDL-c and elevated TG levels through disruption of endocrine functions41,42. Evidence has shown that urinary concentration of phthalates and their metabolites was positively associated with TG and negatively associated with LDL levels43.
On the other hand, the impact of carbohydrates on lipid profile also depends on their sources and processing methods. While consumption of free sugar elevates serum TG, whole grains intake decreases TC, LDL and TG levels44. Consumption of minimally-processed whole grains such as oatmeal, instead of highly processed refined grains may improve lipid profile45.
Our study has some limitations as follows: First, because of the nature of the cross-sectional study, we were not able to assess causal correlations between UPFs intake and lipid profile. In the second place, the study was done in Shiraz city, so it should be generalized to other Iranian adults with caution. Ultimately, although we have removed the effects of some confounders in our analysis, there may be some others which have not been recognized in this study.
In conclusion, our results showed significant associations between ultra-processed foods intake and dietary nutrient profiles which resulted in dyslipidemia as a risk factor for chronic diseases. Findings of the present study highlight a necessity for more evidence, particularly longitudinal, to define the effect of UPFs on lipid profiles.
Data availability
Data available on request from the corresponding author.
References
Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation 106, 3143–3421 (2002).
Aryan, Z. et al. The prevalence, awareness, and treatment of lipid abnormalities in Iranian adults: Surveillance of risk factors of noncommunicable diseases in Iran 2016. J. Clin. Lipidol. 12, 1471-1481.e1474. https://doi.org/10.1016/j.jacl.2018.08.001 (2018).
World Health Organization. Quantifying selected major risks to health. The World Health Report 2002; Reducing risks, promoting healthy life (World Health Organization, 2002).
Haskell, W. L. Cardiovascular disease prevention and lifestyle interventions: Effectiveness and efficacy. J. Cardiovasc. Nurs. 18, 245–255. https://doi.org/10.1097/00005082-200309000-00003 (2003).
Song, S. J., Paik, H. Y., Park, M. & Song, Y. J. Dyslipidemia patterns are differentially associated with dietary factors. Clin. Nutr. 35, 885–891. https://doi.org/10.1016/j.clnu.2015.06.002 (2016).
Barry, M. P. et al. Towards unified and impactful policies to reduce ultra-processed food consumption and promote healthier eating. Lancet Diabetes Endocrinol. 9, 462–470. https://doi.org/10.1016/S2213-8587(21)00078-4 (2021).
Ebner, P., Frank, K., Christodoulou, A. & Davidou, S. How are the processing and nutrient dimensions of foods interconnected? An issue of hierarchy based on three different food scores. Int. J. Food Sci. Nutr. 73, 770–785 (2022).
Monteiro, C. A. et al. Ultra-processed foods: What they are and how to identify them. Public Health Nutr. 22, 936–941. https://doi.org/10.1017/S1368980018003762 (2019).
Cordova, R. et al. Consumption of ultra-processed foods associated with weight gain and obesity in adults: A multi-national cohort study. Clin. Nutr. 40, 5079–5088 (2021).
Donat-Vargas, C. et al. High consumption of ultra-processed food is associated with incident dyslipidemia: A prospective study of older adults. J. Nutr. 151, 2390–2398. https://doi.org/10.1093/jn/nxab118 (2021).
Lima, L. R. et al. Association between ultra-processed food consumption and lipid parameters among adolescents. Cien Saude Colet 25, 4055–4064. https://doi.org/10.1590/1413-812320202510.24822018 (2020).
Pagliai, G. et al. Consumption of ultra-processed foods and health status: A systematic review and meta-analysis. Br. J. Nutr. 125, 308–318. https://doi.org/10.1017/s0007114520002688 (2021).
Ochoa-Avilés, A. et al. Dietary intake practices associated with cardiovascular risk in urban and rural Ecuadorian adolescents: A cross-sectional study. BMC Public Health 14, 939. https://doi.org/10.1186/1471-2458-14-939 (2014).
Rauber, F., Campagnolo, P. D., Hoffman, D. J. & Vitolo, M. R. Consumption of ultra-processed food products and its effects on children’s lipid profiles: A longitudinal study. Nutr. Metab. Cardiovasc. Dis. 25, 116–122. https://doi.org/10.1016/j.numecd.2014.08.001 (2015).
Kohansal, A. et al. Association between plant and animal proteins intake with lipid profile and anthropometric indices: A cross-sectional study. Nutr. Health https://doi.org/10.1177/02601060221104311 (2022).
Borazjani, M., Nouri, M., Venkatakrishnane, K., Najafi, M. & Faghih, S. Association of plant-based diets with lipid profile and anthropometric indices: A cross-sectional study. Nutr. Food Sci. 52, 830–842 (2022).
Mirmiran, P., Esfahani, F. H., Mehrabi, Y., Hedayati, M. & Azizi, F. Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public Health Nutr. 13, 654–662. https://doi.org/10.1017/s1368980009991698 (2010).
Monteiro, C. A. et al. The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 21, 5–17. https://doi.org/10.1017/s1368980017000234 (2018).
Jafari, F. et al. Ultra-processed food intake and risk of colorectal cancer: A matched case-control study. Nutr. Cancer 75, 532–541. https://doi.org/10.1080/01635581.2022.2125990 (2023).
Biernat, E., Stupnicki, R., Lebiedziński, B. & Janczewska, L. Assessment of physical activity by applying IPAQ questionnaire. Phys. Educ. Sport 52, 46–52. https://doi.org/10.2478/v10030-008-0019-1 (2008).
Salcedo-Cifuentes, M., Belalcazar, S., Acosta, E. Y. & Medina-Murillo, J. J. Conventional biomarkers for cardiovascular risks and their correlation with the Castelli Risk Index-Indices and TG/HDL-C. Archivos de Medicina (Manizales) 20, 11–22 (2020).
Huang, P. L. A comprehensive definition for metabolic syndrome. Dis. Model. Mech. 2, 231–237. https://doi.org/10.1242/dmm.001180 (2009).
Wongcharoen, W., Sutthiwutthichai, S., Gunaparn, S. & Phrommintikul, A. Is non-HDL-cholesterol a better predictor of long-term outcome in patients after acute myocardial infarction compared to LDL-cholesterol? A retrospective study. BMC Cardiovasc. Disord. 17, 10. https://doi.org/10.1186/s12872-016-0450-9 (2017).
Lotfi, M. et al. Plant-based diets could ameliorate the risk factors of cardiovascular diseases in adults with chronic diseases. Food Sci. Nutr. 11, 1297–1308 (2022).
Lima, L. R. et al. Association between ultra-processed food consumption and lipid parameters among adolescents. Ciência Saúde Coletiva 25, 4055–4064 (2020).
Beslay, M. et al. Ultra-processed food intake in association with BMI change and risk of overweight and obesity: A prospective analysis of the French NutriNet-Santé cohort. PLoS Med. 17, e1003256. https://doi.org/10.1371/journal.pmed.1003256 (2020).
Li, M. & Shi, Z. Ultra-processed food consumption associated with overweight/obesity among Chinese adults—Results from China Health and Nutrition Survey 1997–2011. Nutrients 13, 2796 (2021).
Mendonça, R. D. et al. Ultra-processed food consumption and the incidence of hypertension in a Mediterranean cohort: The Seguimiento Universidad de Navarra Project. Am. J. Hypertens. 30, 358–366 (2017).
Konieczna, J. et al. Contribution of ultra-processed foods in visceral fat deposition and other adiposity indicators: Prospective analysis nested in the PREDIMED-Plus trial. Clin. Nutr. 40, 4290–4300 (2021).
Sandoval-Insausti, H. et al. Ultra-processed food consumption is associated with abdominal obesity: A prospective cohort study in older adults. Nutrients 12, 2368 (2020).
Cordova, R. et al. Consumption of ultra-processed foods associated with weight gain and obesity in adults: A multi-national cohort study. Clin. Nutr. (Edinburgh, Scotland) 40, 5079–5088. https://doi.org/10.1016/j.clnu.2021.08.009 (2021).
Mehta, K. et al. Marketing foods to children through product packaging: Prolific, unhealthy and misleading. Public Health Nutr. 15, 1763–1770 (2012).
de Graaf, C. J. A. Effects of snacks on energy intake: An evolutionary perspective. Appetite 47, 18–23 (2006).
Garber, A. K. & Lustig, R. H. Is fast food addictive?. Curr. Drug Abuse Rev. 4, 146–162 (2011).
Lissner, L. et al. Television habits in relation to overweight, diet and taste preferences in European children: The IDEFICS study. Eur. J. Epidemiol. 27, 705–715 (2012).
Parks, E. J., Skokan, L. E., Timlin, M. T. & Dingfelder, C. S. Dietary sugars stimulate fatty acid synthesis in adults. J. Nutr. 138, 1039–1046 (2008).
Chong, M. F., Fielding, B. A. & Frayn, K. N. Mechanisms for the acute effect of fructose on postprandial lipemia. Am. J. Clin. Nutr. 85, 1511–1520 (2007).
Astrup, A. et al. Saturated fats and health: A reassessment and proposal for food-based recommendations: JACC state-of-the-art review. J. Am. Coll. Cardiol. 76, 844–857 (2020).
Seok, Y. J. et al. Furan in thermally processed foods—A review. Toxicol. Res. 31, 241–253. https://doi.org/10.5487/tr.2015.31.3.241 (2015).
Milošević, N. et al. Could phthalates exposure contribute to the development of metabolic syndrome and liver disease in humans?. Environ. Sci. Pollut. Res. 27, 772–784. https://doi.org/10.1007/s11356-019-06831-2 (2020).
Golestanzadeh, M., Riahi, R. & Kelishadi, R. Association of exposure to phthalates with cardiometabolic risk factors in children and adolescents: A systematic review and meta-analysis. Environ. Sci. Pollut. Res. 26, 35670–35686. https://doi.org/10.1007/s11356-019-06589-7 (2019).
Srour, B. & Touvier, M. Ultra-processed foods and human health: What do we already know and what will further research tell us?. EClinicalMedicine 32, 100747. https://doi.org/10.1016/j.eclinm.2021.100747 (2021).
Milošević, N. et al. Could phthalates exposure contribute to the development of metabolic syndrome and liver disease in humans?. Environ. Sci. Pollut. Res. Int. 27, 772–784. https://doi.org/10.1007/s11356-019-06831-2 (2020).
Hollænder, P. L., Ross, A. B. & Kristensen, M. Whole-grain and blood lipid changes in apparently healthy adults: A systematic review and meta-analysis of randomized controlled studies. Am. J. Clin. Nutr. 102, 556–572 (2015).
Juul, F., Vaidean, G. & Parekh, N. Ultra-processed foods and cardiovascular diseases: Potential mechanisms of action. Adv. Nutr. (Bethesda, MD) 12, 1673–1680. https://doi.org/10.1093/advances/nmab049 (2021).
Author information
Authors and Affiliations
Contributions
M.N., S.E., M.M., M.R., N.O. and M.N.; Contributed to data collection and writing the first draft. M.N.; Contributed to all data and statistical analysis, and interpretation of data. S.F.; Contributed to the research concept, supervised the work and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nouri, M., Eskandarzadeh, S., Makhtoomi, M. et al. Association between ultra-processed foods intake with lipid profile: a cross-sectional study. Sci Rep 13, 7258 (2023). https://doi.org/10.1038/s41598-023-34451-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-34451-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.