Abstract
Gallbladder stones (GS) is associated with an increased risk of cardiovascular disease. However, the relationship between cholecystectomy for GS and acute coronary syndrome (ACS) is unknown. We investigated the ACS risk in patients with GS and its association with cholecystectomy. Data from the Korean National Health Insurance Service-National Sample Cohort from 2002 to 2013 was extracted. Overall, 64,370 individuals were selected through a 1:3 propensity score matching. Patients were stratified into two groups for comparison: the gallstone group, GS patients with or without cholecystectomy; and the control group, patients without GS or cholecystectomy. The gallstone group exhibited a higher risk of ACS than the control group (hazard ratio [HR], 1.30; 95% confidence interval [CI] 1.15–1.47; P < 0.0001). In the gallstone group, individuals without cholecystectomy had a higher risk of ACS development (HR: 1.35, 95% CI 1.17–1.55, P < 0.0001). Patients with GS with diabetes, hypertension, or dyslipidemia, had a higher risk of developing ACS than GS patients without the metabolic diseases (HR: 1.29, P < 0.001). The risk did not significantly differ after cholecystectomy compared to those without GS (HR: 1.15, P = 0.1924), but without cholecystectomy, the risk of ACS development was significantly higher than control group (1.30, 95% CI 1.13–1.50, P = 0.0004). Among patients without above metabolic disorders, cholecystectomy was still associated with increased ACS risk in the gallstone group (HR: 2.93, 95% CI 1.27–6.76, P = 0.0116). GS increased the risk of ACS. The effect of cholecystectomy on ACS risk differs according to the presence or absence of metabolic disorders. Thus, the decision to perform cholecystectomy for GS should consider both the ACS risk and the underlying disorders.
Similar content being viewed by others

Introduction
GB stones (GS) are a very common benign gall bladder disease1,2,3. GS and acute coronary syndrome (ACS) share a number of common risk factors, and previous studies have found that the incidence of ACS was higher in people with gallstones4,5,6,7. Zheng et al. analyzed the relationship between a history of GS and the risk of incident ACS in 3 large prospective US cohorts (n = 269,142 participants)6. They found that a history of GS was associated with a 23% (15–33%) increase in ACS risk6. Olaiya et al. further reported that patients with GS had an elevated risk of ACS (hazards ratio [HR], 1.42; 95% CI 1.28–1.58).5 ACS remains the leading cause of death worldwide. Despite substantial improvements in ACS prevention and treatment, the social and economic burden remains significant and continues to increase8. Thus, the association between GS and ACS could be a matter of interest in the prevention and management of ACS.
Cholecystectomy is one of the most frequently performed surgical procedures worldwide, and is considered safe in patients with GS. Even though the association between GS and ACS has been reported a number of times, few studies have observed an association between cholecystectomy and the risk of ACS, and their results are contradictory9,10. Chen et al. showed that cholecystectomy could decrease the risk of ACS10, and Norberto et al. reported that patients undergoing cholecystectomy had an increased prevalence of risk factors for ACS9,11. The outcomes of each study could be contentious as differences in baseline characteristics were not considered in this analysis. As there are other risk factors for ACS, such as hypertension, diabetes mellitus, and hyperlipidemia, we believe that the effects of cholecystectomy on ACS should be analyzed according to the underlying medical conditions.
We sought to investigate the association between GS and cholecystectomy and the risk of ACS according to the underlying medical conditions by conducting a nationwide population-based cohort study to explore the association between cholecystectomy and ACS.
Results
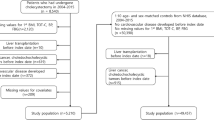
The baseline characteristics of the study population are presented in Table 1. A total of 64,370 individuals (47.8% men and 52.2% women) were selected for the study. Of these, 20.3% (n = 13,069) with GS were classified in the gallstone group, and 79.7% (n = 51,301) in the control group did not have GS. Among the patients with GS, 20.7% (n = 2706) underwent cholecystectomy, while 79.3% (n = 10,363) did not.
Among the study population, individuals with GS had a higher prevalence of diabetes (34.5% vs. 25.5%, P < 0.0001), hypertension (48.2% vs. 41.6%, P < 0.0001), and dyslipidemia (42.9% vs. 33.4%, P < 0.0001) than those without GS. Furthermore, in the gallstone group, the prevalence of the following diseases was slightly higher among patients who underwent cholecystectomy: diabetes (36.0% vs. 34.2%, P < 0.0001), hypertension (49.7% vs. 47.9%, P < 0.0001), and dyslipidemia (43.7% vs. 42.7%, P < 0.0001) (Supplementary Table 1).
Of the total study population, 2.0% (n = 1,279) had ACS. The GS group contained 2.7% (n = 357) ACS patients, while the control group contained 1.8% (n = 922). Furthermore, in the gallstone group, 3.8% (n = 103) underwent cholecystectomy and had ACS, whereas 2.5% (n = 254) did not undergo cholecystectomy but developed ACS. Regarding chronic conditions, 27.4% (n = 17,610), 43.0% (n = 27,667), and 35.3% (n = 22,748) of patients had diabetes, hypertension, and dyslipidemia, respectively, in whom the incidence rates of ACS were 4.0% (n = 702), 4.0% (n = 1109), and 3.8% (n = 863), respectively (Table 1).
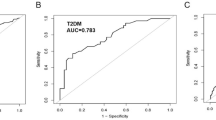
Kaplan–Meier analysis showed that the GS group was at a higher risk of developing ACS regardless of cholecystectomy (Fig. 1, P < 0.0001). Table 2 shows the results of the Cox proportional hazard model using HRs between the variables and ACS. The GS group exhibited a higher risk of developing ACS than the control group (HR:1.30, 95% CI 1.15–1.47, P < 0.0001). Individuals with GS had a higher risk of ACS (HR: 1.30, 95% CI 1.15–1.47, P < 0.0001) compared to the control group. Regarding cholecystectomy in the GS group, individuals who did not undergo cholecystectomy had a statistically higher risk of ACS development (HR: 1.35, 95% CI 1.17–1.55, P < 0.0001) compared to the control group, while the risk did not significantly differ after cholecystectomy compared to the control group (HR: 1.21, 95% CI 0.98–1.48, P = 0.0755).
We further investigated the association between GS and ACS according to diabetes, hypertension, and dyslipidemia (Tables 2 and 3). Diabetes (HR:1.29, 95% CI 1.15–1.45, P < 0.0001), hypertension (HR:3.74, 95% CI 3.14–4.47, P < 0.0001), and dyslipidemia (HR:1.98, 95% CI 1.75–2.24, P < 0.0001) (Table 2) were all associated with a higher risk of ACS development in this study. GS was also associated with the development of ACS in patients with metabolic diseases. The presence of GS increased the risk of ACS in those with metabolic diseases (diabetes HR:1.38, 95% CI 1.18–1.63, P < 0.0001; hypertension HR:1.23, 95% CI 1.08–1.41, P = 0.0023; dyslipidemia HR:1.22, 95% CI 1.05–1.41, P = 0.0106) (Table 3). The risk of developing ACS increased with the presence of diabetes, hypertension, and dyslipidemia in patients with GS compared to those without GS (HR:1.29, 95% CI 1.14 – 1.47, P < 0.0001).
The gallstone group was subdivided into two groups according to cholecystectomy. The impact of cholecystectomy on ACS differed according to the type of metabolic disease. In patients with diabetes, hypertension, or dyslipidemia, the gallstone groups who did not undergo cholecystectomy had a higher risk of ACS development than those who underwent cholecystectomy (diabetes HR:1.44, 95% CI 1.20–1.73, P < 0.0001; hypertension HR:1.26, 95% CI 1.08–1.47, P = 0.0031; dyslipidemia HR:1.31, 95% CI 1.10–1.55, P = 0.0019) (Table 3). Among the gallstone group diagnosed with any of the three diseases, those who did not undergo cholecystectomy showed a higher risk of ACS development than those who underwent cholecystectomy (HR,1.30; 95% CI 1.13–1.50; P = 0.0004). In contrast, in patients without the three diseases, cholecystectomy was associated with a higher risk of ACS development (HR:2.93, 95% CI 1.27–6.76, P = 0.0116).
Discussion
Previous studies have reported that the presence of GS is associated with an increased risk of ACS. Our results verified this and additionally showed that patients without cholecystectomy for GS are associated with an increased risk of ACS compared to the control group. Interestingly, the effects of cholecystectomy for GS on the risk of ACS differed depending on the underlying metabolic disease. When cholecystectomy was performed on patients with GS with an underlying metabolic disease, such as hypertension, diabetes, or hyperlipidemia, the risk of ACS was not significantly different compared to those without GS, but this trend was reversed in the GS group without underlying metabolic disease. In patients without all three diseases (diabetes, hypertension, and dyslipidemia), cholecystectomy was still associated with an increased risk of ACS than the control group. However, when the diseases were considered individually, the presence or absence of diabetes alone was not associated with an increased risk of ACS after cholecystectomy. These findings imply that when cholecystectomy is planned for GS, underlying metabolic diseases should be considered to reduce the risk of ACS.
Previous studies and our results have shown a significantly increased risk of ACS among patients with GS4,5,7,12. Patients with GS frequently have risk factors for ACS, which could explain the increased risk of ACS. Our subgroup analysis showed that GS was associated with an even higher risk of ACS in patients with diabetes, hyperlipidemia, and hypertension. Therefore, patients with gallstones were at increased risk of developing ACS not simply because they already had other risk factors, but because the presence of GS itself posed a risk.
Age, obesity, body mass index, low serum high-density lipoprotein cholesterol levels, diabetes mellitus, inadequate physical inactivity, and excessive alcohol use have all been identified as ACS risk factors7. These are also shared risk factors for GS, which could explain the increased risk of ACS in the GS group13. The formation of gallstones is thought to be caused primarily by biliary cholesterol supersaturation caused by metabolic abnormalities in the liver and the subsequent physico-chemical imbalance of cholesterol solubility in bile4,14,15. The term “ACS” refers to a group of conditions characterized by a sudden decrease in blood flow to the heart, such as unstable angina, non-ST elevation myocardial infarction, and ST elevation myocardial infarction.
The association between GS and ACS is easily understood but is unpredictable with cholecystectomy. The previous studies have reported varied effects of cholecystectomy on the risk of ACS. Chen et al. investigated the effect of cholecystectomy on the subsequent risk of ACS in patients with GS10. The cumulative incidence of ACS was lower in patients with GS who underwent cholecystectomy than in those who did not. In contrast, Norberto et al. analyzed the relationship between cholecystectomy for GS and risk factors for ACS. Multivariate analysis revealed that the cholecystectomy group had a higher incidence of metabolic risk variables for ACS than the control group. Patients who underwent cholecystectomy exhibited a higher incidence of risk factors for ACS regardless of age, sex, or body mass index9. In terms of patients’ baseline characteristics, the study by Chen et al. had a higher proportion of patients with metabolic illnesses than the study by Norberto et al. This suggests that the effect of cholecystectomy on the risk of ACS may differ depending on the underlying presence of metabolic diseases. Our results prove that the above-mentioned hypothesis is most likely to be true. In patients with metabolic diseases, not undergoing cholecystectomy was associated with a higher risk of ACS than the control group, but the risk did not significantly differ after cholecystectomy compared to the control group. Among patients without metabolic disorders, cholecystectomy was still associated with increased ACS risk in the GS group compared to the control group. These findings should be verified in future studies.
Although the treatment of asymptomatic gallstone patients is not generally recommended, current treatment strategies for symptomatic gallstone patients require surgical treatment. Following cholecystectomy, the gallbladder reservoir decreases, resulting in the continuous release of hepatic bile into the duodenum lumen16. As a result, the bile acid pool circulates more quickly, exposing enterohepatic organs and, eventually, peripheral tissues to a larger flow of bile acids during the diurnal cycle fasting periods17. Few studies have investigated the serum lipid profiles of individuals who underwent laparoscopic cholecystectomy. They showed that lipid and bile acid metabolisms are functionally linked18. There have been several hypotheses suggesting that cholecystectomy affects the lipid profile, which in turn affects the risk of ACS19,20. However, the results of previous studies cannot fully explain our findings, therefore, more research on the mechanism is required.
On the other hand, we also regard the mechanistic link between gallstones and cardiovascular disease that is associated with the gut microbiome. Patients with gallstones exhibit a distorted secretion of bile acids that play a crucial role in regulating gut microbiota21. Dysbiosis of gut microbiota may influence various host functions associated with cardiovascular risk22,23,24. Previous studies have reported that metabolites produced by gut microbiota, such as trimethylamine N-oxide and L-carnitine, inhibit bile acid transporters and promote atherosclerosis and cardiovascular risk25,26. Proteobacteria has been found to be linked to a wide range of metabolic disturbances, including an increased risk of obesity and cardiovascular disease27,28. Cholecystectomy alters bile flow to the intestine and can, therefore, modify the bidirectional interactions between bile acids and the intestinal microbiota29.
This study had several limitations First, the analysis was based on health insurance claim data reported with ICD-10 diagnostic codes; therefore, potential covariates, such as health behavior factors, drug prescription or laboratory test results were not included in this study. Due to a lack of clinical and laboratory data, there are still problems with diagnosis accuracy and failure to account for risk variables for gallstone disease. We adjusted all data for CCI, which provides information on the severity of an individual’s health conditions. In the future, we plan to investigate the relationship between metabolic disease and cholecystectomy using the same data from the Korea National Health and Nutrition Examination Survey. Second, the characteristics, including the number and size of gallstones, which are important factors related to gallstone surgery and prognosis, could not be investigated in this study. This aspect should be recognized as a limitation of epidemiological studies based on health insurance claims data. This study aimed to provide comprehensive information using a large-scale epidemiological study, and it was the largest large-scale study to examine the effect of cholecystectomy on ACS in patients with gallstones to date.
In conclusion, GS was associated with an increased risk of ACS. When cholecystectomy was performed for GS in patients with underlying metabolic diseases, the risk of ACS was not significantly different from that in patients without GS. When cholecystectomy is planned, its effect on the risk of ACS should be considered. Further validation in a large prospective cohort study and elucidation of the underlying mechanisms are needed.
Methods
In this study, we used data from the Korean National Health Insurance Service National Sample Cohort (NHIS-NSC). The NHIS is the universal health insurance service in Korea, under which all citizens are enrolled, as such, all Korean citizens’ claims data are included in the NHIS database. The NHIS-NSC data contains 2.2% of the entire Korean population, selected using a systematic stratified random sampling method. Data were collected over 11 years from 2002 to 2013. The International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10), was used for the health insurance claim data.
The final study population of 64,370 individuals was selected after applying 2 years of wash-out periods to detect newly diagnosed patients with ACS or GS. Of the total study population, 13,069 patients with GS were stratified to the gallstone group, while 51,301 individuals without GS were designated as the control group. To establish the case and control groups, a 1:3 propensity score matching of age, sex, and year was performed. The matched individuals shared the same index date as the case group, taking the diagnosis date as their follow-up start date.
GS and ACS were defined using the ICD-10 codes. K80.0, K80.1, and K80.2 defined GS, while I20.0 (unstable angina) and I21 (AMI) defined ASC. Once an individual was diagnosed with one of these ICD codes, they were categorized as patients. Patients with GS were further subdivided into those who underwent cholecystectomy and those who did not. As covariate variables, sex, age, region, income level, occupational status, disability, diabetes, hypertension, dyslipidemia, Charlson comorbidity index (CCI), and cohort entry year were examined. The age group was divided into 10-year intervals from the 20 s to the 80 s. None of the individuals were aged over 89 years. The regions were divided into three groups: the capital area (Seoul), metropolitan area (Busan, Daegu, Daejeon, Gwangju, Incheon, and Ulsan), and rural areas (Gyeonggi, Gangwon, Chungcheongbuk, Chungcheongnam, Jeollabuk, Jeollanam, Gyeongsangbuk, Gyeongsangnam, and Jeju). Diabetes (E10, E11, E12, E13, and E14), hypertension (I10, I11, I12, I13, I14, and I15), and dyslipidemia (E78) were defined using the ICD-10 codes.
Descriptive statistics for each variable of ACS are presented. Chi-square tests were used to test the differences in variables and incidence of ACS at baseline. Kaplan–Meier curves and log-rank test were applied to investigate the association between GS and ACS, along with survival time. The multivariate Cox proportional hazard model was employed to estimate the adjusted hazard ratios (HRs) and 95% confidence intervals (CI). The analyses investigated the associations between variables and ACS, considering survival time. All analyses were performed using SAS software (version 9.4; SAS Institute, Cary, North Carolina, USA).
Ethical approval and informed consent
The study used de-identified secondary health insurance claim data collected and distributed by NHIS under the government Ministry of Health and Welfare. As the data is available upon request to NHIS (www.nhis.or.kr), the study received a waiver of Ethical approval from Yonsei University Health System, Severance Hospital, Institutional Review Board (Wavier approval number: 4-2021-1375). Moreover, the informed consent was waived as the data is provided by NHIS. The waiver was approved based as Enforcement Rules Of The Bioethics and Safety Act, Republic of Korea [Article 15 (Deliberation on Human Subjects Research Projects)(1) A person who intends to conduct a human subjects research project shall prepare a research plan and submit it for deliberation by the competent IRB before commencing such human subjects research project. (2) Notwithstanding paragraph (1), a research project may be exempted from deliberation by the competent IRB, if a risk to human subjects of research and the general public is insignificant and the research project meets the standards prescribed by Ordinance of the Ministry of Health and Welfare after deliberation by the National Committee].
Data availability
Deidentified individual participant data are available upon request to Korean National Health Insurance Sharing Service at https://nhiss.nhis.or.kr/.
Abbreviations
- ACS:
-
Acute coronary syndrome
- CCI:
-
Charlson comorbidity index
- GS:
-
Gall stone
- HR:
-
Hazards ratio
- CI:
-
Confidence interval
- NHIS-NSC:
-
Korean National Health Insurance Service National Sample Cohort
References
Froutan, Y. et al. Gallstone disease founded by ultrasonography in functional dyspepsia: prevalence and associated factors. Int. J. Clin. Exp. Med. 8, 11283–11288 (2015).
Shaffer, E. A. Epidemiology of gallbladder stone disease. Best Pract. Res. Clin. Gastroenterol. 20, 981–996. https://doi.org/10.1016/j.bpg.2006.05.004 (2006).
Housset, C., Chretien, Y., Debray, D. & Chignard, N. Functions of the gallbladder. Compr. Physiol. 6, 1549–1577. https://doi.org/10.1002/cphy.c150050 (2016).
Fairfield, C. J., Wigmore, S. J. & Harrison, E. M. Gallstone disease and the risk of cardiovascular disease. Sci. Rep. https://doi.org/10.1038/s41598-019-42327-2 (2019).
Olaiya, M. T., Chiou, H. Y., Jeng, J. S., Lien, L. M. & Hsieh, F. I. Significantly increased risk of cardiovascular disease among patients with gallstone disease: a population-based cohort study. Plos One 8, e76448 (2013).
Zheng, Y. et al. Gallstones and risk of coronary heart disease: prospective analysis of 270 000 men and women from 3 US cohorts and meta-analysis. Arterioscler. Thromb. Vasc. Biol. 36, 1997–2003. https://doi.org/10.1161/ATVBAHA.116.307507 (2016).
Fan, L. L., Chen, B. H. & Dai, Z. J. The relation between gallstone disease and cardiovascular disease. Sci. Rep. 7, 15104. https://doi.org/10.1038/s41598-017-15430-5 (2017).
Lozano, R. et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet 380, 2095–2128. https://doi.org/10.1016/S0140-6736(12)61728-0 (2012).
Chavez-Tapia, N. C. et al. Association between cholecystectomy for gallstone disease and risk factors for cardiovascular disease. Ann. Hepatol. 11, 85–89. https://doi.org/10.1016/S1665-2681(19)31490-5 (2012).
Chen, C. H., Lin, C. L. & Kao, C. H. The effect of cholecystectomy on the risk of acute myocardial infarction in patients with gallbladder stones. Postgrad. Med. 133, 209–216. https://doi.org/10.1080/00325481.2020.1846964 (2021).
Chen, Y. S., Wu, S. D. & Tian, Y. Cholecystectomy as a risk factor of metabolic syndrome: from epidemiologic clues to biochemical mechanisms. Lab. Invest. 98, 7–14. https://doi.org/10.1038/labinvest.2017.95 (2018).
Fairfield, C., Wigmore, S. & Harrison, E. Gallstone disease and the risk of cardiovascular disease: systematic review and meta-analysis of observational studies. Brit. J. Surg. 105, 47–47 (2018).
Huang, J. J. et al. The association between gallstone disease (GSD) and the incidence of prediabetes and type 2 diabetes mellitus (type 2 DM): a prospective cohort study. Int. J. Diabetes Dev. C 40, 40–46. https://doi.org/10.1007/s13410-019-00748-9 (2020).
Lammert, F. et al. Gallstones. Nat. Rev. Dis. Primers 2, 16024. https://doi.org/10.1038/nrdp.2016.24 (2016).
Portincasa, P., Moschetta, A. & Palasciano, G. Cholesterol gallstone disease. Lancet 368, 230–239. https://doi.org/10.1016/s0140-6736(06)69044-2 (2006).
Amigo, L. et al. Cholecystectomy increases hepatic triglyceride content and very-low-density lipoproteins production in mice. Liver Int. 31, 52–64. https://doi.org/10.1111/j.1478-3231.2010.02361.x (2011).
Hylemon, P. B. et al. Bile acids as regulatory molecules. J. Lipid Res. 50, 1509–1520 (2009).
Kuipers, F., Bloks, V. W. & Groen, A. K. Beyond intestinal soap–bile acids in metabolic control. Nat. Rev. Endocrinol. 10, 488–498. https://doi.org/10.1038/nrendo.2014.60 (2014).
Sergeev, I., Keren, N., Naftali, T. & Konikoff, F. M. Cholecystectomy and biliary sphincterotomy increase fecal bile loss and improve lipid profile in dyslipidemia. Dig. Dis. Sci. 65, 1223–1230. https://doi.org/10.1007/s10620-019-05823-z (2020).
Krondl, A., Vavrinkova, H. & Michalec, C. effect of cholecystectomy on the role of the gall bladder in fat absorption. Gut 5, 607–610. https://doi.org/10.1136/gut.5.6.607 (1964).
Berr, F., Pratschke, E., Fischer, S. & Paumgartner, G. Disorders of bile acid metabolism in cholesterol gallstone disease. J. Clin. Invest. 90, 859–868. https://doi.org/10.1172/jci115961 (1992).
Wang, Z. et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature 472, 57–63. https://doi.org/10.1038/nature09922 (2011).
Vinjé, S., Stroes, E., Nieuwdorp, M. & Hazen, S. L. The gut microbiome as novel cardio-metabolic target: the time has come!. Eur. Heart J. 35, 883–887. https://doi.org/10.1093/eurheartj/eht467 (2014).
Tang, W. H. et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N. Engl. J. Med. 368, 1575–1584. https://doi.org/10.1056/NEJMoa1109400 (2013).
Koeth, R. A. et al. Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat. Med. 19, 576–585. https://doi.org/10.1038/nm.3145 (2013).
Charach, G. et al. The association of bile acid excretion and atherosclerotic coronary artery disease. Therap. Adv. Gastroenterol. 4, 95–101. https://doi.org/10.1177/1756283x10388682 (2011).
Wu, T. et al. Gut microbiota dysbiosis and bacterial community assembly associated with cholesterol gallstones in large-scale study. BMC Genom. 14, 669. https://doi.org/10.1186/1471-2164-14-669 (2013).
Carey, M. C. & Mazer, N. A. Biliary lipid secretion in health and in cholesterol gallstone disease. Hepatology 4, 31s–37s. https://doi.org/10.1002/hep.1840040806 (1984).
Keren, N. et al. Interactions between the intestinal microbiota and bile acids in gallstones patients. Environ. Microbiol. Rep. 7, 874–880. https://doi.org/10.1111/1758-2229.12319 (2015).
Funding
This work was supported by the National Research Foundation of Korea(NRF) grant funded by the Korea government(MSIT) (No. 2022R1F1A1062794).
Author information
Authors and Affiliations
Contributions
Conceptualization: H.S.L., J.H.J., M.J.C. and J.Y.P. Data curation: W.C. and S.I.J.; Formal analysis: W.C., and S.I.J.; Investigation: H.S.L., W.C., J.H.J., M.J.C., S.B., S.W.P., S.Y.S., S.I.J. and J.Y.P.; Methodology: W.C., and S.-I.J.; Validation: S.W.P. and S.Y.S.; Wiring: H.S.L., W.C., S.-I.J. and J.Y.P.; Supervision: S.I.J., J.Y.P. All author reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chae, W., Lee, H.S., Jo, J.H. et al. Impact of cholecystectomy on acute coronary syndrome according to metabolic condition: a nationwide population-based cohort study. Sci Rep 13, 7300 (2023). https://doi.org/10.1038/s41598-023-33440-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-33440-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.