Abstract
The goal of this study was to investigate the impact of postoperative inclination of the joint line on clinical results after total knee arthroplasty (TKA) using a prosthesis with anatomical geometry. This study included 145 primary cruciate-retaining type of knee prosthesis with anatomical geometry. Three years postoperatively, clinical outcomes including the patient-reported outcomes (PROs) were recorded. Limb alignment was evaluated by the hip-knee-ankle (HKA) axis and inclination of the joint line was assessed by the joint line orientation angle (JLOA). Knees were divided into two groups according to the HKA: in-range (− 3 to 3°) and outlier group (< − 3° or > 3°) or the JLOA: in-range (2–4°) and outlier group (< 2° or > 4°), and clinical outcomes were compared between the groups. Postoperative Knee Society Function Score (KS-FS) was significantly higher in the HKA in-range group than the outlier group (p = 0.01). The Knee Society Knee Score and all subscales of the Knee injury Osteoarthritis Outcome Score were comparable between the groups. A multivariate analysis revealed a significant association between age at operation and postoperative KS-FS > of 80 points. Neither HKA in-range nor JLOA in-range were associated with the higher knee function. In conclusion, TKA-postoperative inclination of the joint line was not relevant to the short-term PROs. Treatment strategies that attempt to make joint line inclination in order to improve postoperative PROs should be avoided, and alignment goals such as kinematic alignment should be considered carefully.
Similar content being viewed by others
Introduction
Although the outcomes of total knee arthroplasty (TKA) are generally acceptable, approximately 20% of patients have some complaints and poor patient-reported outcomes (PROs) after TKA1,2,3. The reasons for dissatisfaction remain poorly understood. Failure to restore a physiological joint line has been suggested as a causative factor associated with the poor outcomes. In 2008, kinematically aligned (KA)-TKA was introduced as a surgical technique to reproduce the physiological joint line4. With KA-TKA, the femoral and tibial components are implanted to restore the physiological joint line to its constitutional state of individual patients. To date, many investigators have reported good clinical outcomes after KA-TKA5,6,7,8,9,10; however, the longevity of the polyethylene insert and survival of femoral and/or tibial components are still major concerns11,12. Considering these issues, restoration of the physiological joint line using a prosthesis with anatomical geometry through mechanically aligned (MA)-TKA may improve the PROs with maintaining the long-term survival.
The FINE total knee was developed in Japan and its clinical use began in 2001. It has unique design features that include an oblique 3° femorotibial joint line in both coronal and axial planes, conforming to anatomical geometry13. This feature allows reproduction of the physiological joint line by the osteotomy to be performed perpendicular to the mechanical axis. The patellofemoral geometry has patellar-friendly design and the round, all-polyethylene component is inset to the patella when resurfacing. When the FINE knee is implanted with mechanically neutral alignment, the forces on the insert should be even between the medial and lateral side. Besides, vitamin E is added to the polyethylene and the insert is produced through the direct compression molding method that allows to reduce backside wear of the polyethylene insert14. The insert has a minimum thickness of 5 mm on medial concave side that secures longevity of the implant.
Although restoration of the physiological joint line using a prosthesis with anatomical geometry would potentially improve the clinical outcomes including the PROs, the impact is not clear. The aim of this study was to investigate the impact of inclination of the joint line on clinical outcomes including PROs after TKA using a prosthesis with anatomical geometry. Our hypothesis was that patients with physiological inclination of the joint line after TKA would have better clinical outcomes including PROs than those without it.
Materials and methods
Patients
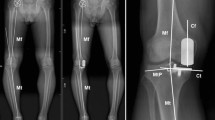
This study included 145 primary TKAs in 145 patients with osteoarthritis (OA) who received a cruciate-retaining type of the FINE total knee (Teijin-Nakashima Medical Co. Ltd., Okayama, Japan) (Fig. 1) at our hospital between February 2015 and February 2019. Exclusion criteria were patients with an impaired posterior cruciate ligament, bilateral TKAs, valgus knees < 170° of the femorotibial angle (FTA), flexion contracture of 30o or more, deformed femur or tibia following trauma, or dementia at the time of recording clinical scores.
The FINE total knee. The femoral condyle has an asymmetric shape and femorotibial joint line with an inclination of 3° both in coronal (left) and axial (right) planes. The medial and lateral condyle have different length of radii (medial larger than lateral), resulting in medially inclined joint line both in extension and flexion. The medial surface of the polyethylene insert has a convex curve while the lateral surface has a flat surface. The figure is reprinted with minor modifications from Fig. 1 in reference 13.
This study was approved by the institutional review board at our institution. All activities were performed in accordance with the ethical standards set forth in the Declaration of Helsinki, and a written informed consent was obtained from all patients who participated in this study.
Surgical procedures
All TKAs were performed by a single senior orthopedic surgeon (A.N) using the measured resection technique through the mid-vastus approach. Our goal was mechanically neutral alignment and surgeries were performed using conventional instruments. A distal femoral osteotomy was conducted perpendicular to the mechanical axis at a level 9–10 mm from the farthest point of the medial condyle, and the posterior condyle was osteotomized parallel to the surgical epicondylar axis. A tibial osteotomy subsequently was conducted perpendicular to the anatomical axis of the tibia. The resection level was 8–10 mm distal to the convex of the lateral plateau. Following osteotomy, soft tissue balance was checked both in extension and flexion using the knee balancer. When the minimum gap to implant the prosthesis was not obtained in medial side, the MCL was released from the tibial site or the pie-crust release was added. After no flexion contracture and good flexion angle in replacement with trial components was confirmed, the implants were fixed to the bone with cement. We basically replaced patellae but not for patients without osteoarthritic changes in patellofemoral joint or with small size of patellae. Patients were discharged three weeks after surgery when they were medically stable, with pain controlled by oral analgesics and when deemed by a physiotherapist to be mobilizing sufficiently to function safely at home.
Clinical evaluation
Clinical scores including flexion angle, Knee Society Knee Score (KSS), and Knee injury and Osteoarthritis Outcome Score (KOOS) were recorded preoperatively and three years postoperatively. Flexion angle was measured by a single observer (M.Y) using a goniometer with a patient laid on a flat table, and the maximum active flexion angle was recorded. Increase in the scores (postoperative-preoperative scores) also were recorded. The KSS, which consists of a knee score (KS-KS) and a function score (KS-FS), was used to objectively evaluate knee function15. In addition to the KSS, the Japanese KOOS, an instrument of confirmed validity and reliability for PROs based on its cross-cultural adaptation16, was used, but the sports subscale was not recorded.
Radiographic examinations for limb alignment and inclination of the joint line
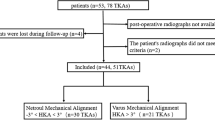
The limb alignment was evaluated by hip-knee-ankle (HKA) angle, which was measured using full-leg standing radiographs, and varus alignment was defined as positive. Knees were divided into two groups with the HKA: i.e., in-range (− 3 ~ 3°) and outlier groups (< − 3° or > 3°). Inclination of the joint line was evaluated by joint line orientation angle (JLOA) (Fig. 2), which is the angle formed between the joint line and a line parallel to the floor9,17,18,19,20. Medial inclination (medial side down and lateral side up) was defined as positive. The goal of the JLOA is considered to be 3° in the FINE based on its design concepts13. Therefore, knees were divided into two groups with the JLOA: i.e., in-range (2–4°) and outlier (< 2° or > 4°), and clinical outcomes were compared between the groups. Regarding the component alignment for individuals, our previous study has shown that there were no differences in coronal and sagittal alignment of the femoral and tibial components between the groups21.
Two independent observers (M.Y and A.N) measured the HKA and the JLOA twice, with a 2-month interval, using a subset of 20 cases. All measurements were performed using SYNAPSE-PACS software (FUJIFILM, Tokyo, Japan).
Statistical analysis
Intra-observer and inter-observer reliabilities were assessed using intra-class correlation coefficients (ICCs). ICCs were > 0.8 for all measurements. Based on these reliabilities, measurements performed by a single investigator (M.Y) were used in the analysis. A t-test was used to compare between the two groups. Prior to the t-test, we confirmed that each clinical score exhibited a normal distribution and there were no significant differences in the variance between the groups. A statistical power analysis was performed prior the study; based on a prespecified significance level of α < 0.05 and by assuming a medium effect size (= 0.5), the power required was estimated to be 0.8 by using G*Power 3. The estimated sample size was 64 patients. A multivariate logistic regression analysis was further performed to determine factors associated with postoperative KS-FS > of 80 points. Age, gender (male/female), BMI, Kellgren-Lawrence (K-L) grade, preoperative range of motion (ROM), postoperative ROM, preoperative femorotibial angle (FTA), postoperative FTA, patellar replacement (yes/no), HKA in-range (yes/no), and JLOA in-range (yes/no) were chosen as the explanatory variables. Prior to the multivariate analysis, multi-collinearity for the variables was validated, and we confirmed that variance inflation factor (VIF) of each variable was < 10. Results were expressed as the mean (standard deviation, SD). Data analyses were performed using SPSS software, version 28 (SPSS Inc., Chicago, IL, USA) and p-values < 0.05 were considered statistically significant.
Ethics approval and consent to participate
Approval for the study was received from the Institutional Review Board at Toho University Sakura Medical Center, and all patients gave their written consent to participate in this study. All activities were performed in accordance with the ethical standards set forth in the Declaration of Helsinki.
Results
Demographic data of the patients
The demographic data of the patients were shown in Table 1. There were 28 men and 117 women, with a mean age of 72.9 years (range: 48–89) at the time of surgery. The mean body mass index was 26.7 kg/m2. The mean FTA on a standing position was 184.4° (range: 172–206). The number of cases on the K-L classification22 were 7 for grade II, 29 for grade III, and 109 for grade IV. Ninety-seven patients (63.4%) received patellar replacement. Regardless of patellar replacement, neither anterior knee pain nor patellar clunk syndrome were observed during the period of this study.
Distribution of the knees according to postoperative limb alignment or inclination of the joint line
Among 145 knees analyzed, 81 knees (55.9%) were classified into the HKA in-range group and 64 knees (44.1%) were classified into the outlier group. Alternatively, 80 knees (55.2%) were classified into the JLOA in-range group and 65 knees (44.8%) were classified into the outlier group. The distribution of knees either with the HKA or the JLOA is shown in Fig. 3.
Distribution of the in-range and the outlier groups in a total of 145 knees. When the knees were classified according to the HKA axis, 81 knees (55.9%) were assigned to the in-range group (− 3 to 3°) (left, red bars), and 64 knees (44.1%) were assigned to the outlier group (< − 3° or > 3°) (left, blue bars). When classified according to the JLOA, 80 knees (55.2%) were assigned to the in-range group (2–4°) (right, red bars), and 65 knees (44.8%) were assigned to the outlier group (< 2° or > 4°) (right, blue bars). HKA: hip-knee-ankle; JLOA: joint line orientation angle.
Comparison of clinical outcomes between groups for postoperative limb alignment
Preoperative flexion angle, the KSS, and all subscales of the KOOS were comparable between the HKA in-range and outlier groups. Postoperatively, the KS-FS was significantly higher in the in-range group than the outlier group (p = 0.01). The KS-KS, all subscales of the KOOS, and the increase in the scores were comparable between the groups. (Table 2).
Comparison of clinical outcomes between groups for postoperative inclination of the joint line
Preoperative KSS and the KOOS subscales were comparable between JLOA in-range and outlier groups, but the preoperative flexion angle was significantly lower in the in-range group than the outlier. The postoperative flexion angle was comparable between the groups (in-range: 126.6°, outlier: 127.1°). The increase in flexion angle was more in the in-range group than the outlier. The KSS, all subscales of the KOOS, and the increase in the scores other than flexion angle were comparable between the groups (Table 3).
A multivariate analysis for identification of factor(s) associated with the postoperative KS-FS > of 80 points
Based on the results that the in-rage group for the HKA had a significantly higher score than the outlier group (Table 2), we performed a multivariate logistic analysis to identify factor(s) associated with the postoperative KS-FS > of 80 points. Among 11 explanatory variables, age at operation was significantly associated with the postoperative KS-FS > of 80 points, and neither HKA in-range nor JLOA in-range were associated with the higher knee function (Table 4).
Discussion
The association between postoperative mechanical axis alignment, often evaluated as HKA axis alignment, and clinical outcomes after mechanically aligned (MA)-TKA has been shown by a number of studies. Most studies stated that HKA axis malalignment was not associated with clinical outcomes13,23,24,25,26,27,28. Similar results were shown in the present study; the HKA in-range group did not have better clinical outcomes including flexion angle, the KSS, and all subscales of the KOOS than the outlier group. However, long-term clinical outcomes and implant survival are concerned in TKA with HKA axis malalignment. Kuroda et al. reported that immediate postoperative varus alignment and varus position of the femoral and tibial components were possible risk factors for varus progression in limb alignment in the long term after TKA29. Therefore, it is conceivable that the postoperative HKA axis should be targeted for in-range alignment even though it does not associate with clinical outcomes.
Inclination of the joint line after TKA has been discussed by many orthopedic surgeons. Several investigators have examined physiological inclination of the joint line in normal knees30,31,32,33,34,35,36. Moreland et al. first reported that inclination of the joint line relative to the tibial mechanical axis was 3.0° (right) and 2.6° (left) in young male volunteers 30. Nakano et al. reported that tibial plateau inclination was 85.6° (female) and 85.1° (male) in young Japanese participants36, which corresponds to 4.4° and 4.9° respectively, if inclination of the joint line was measured according to the method in the present study. These observations show physiological inclination of the joint line in normal knees and its racial or gender differences. Regarding the joint line inclination in OA knees, we have shown that the mean medial proximal tibial angle (MPTA) for elderly Japanese patients was 83.9°37, which corresponds to 6.1 degrees of inclination in the present study.
The FINE total knee was developed to reproduce physiological inclination of the joint line. The characteristic aspect of the FINE knee is to have 3° inclination of the medial femorotibial surface and anatomical geometry13. The expectation using this prosthesis was that patients with a JLOA close to 3° would have better clinical outcomes than those with a JLOA that deviated from 3°. A systematic review showed that the clinical outcomes of KA-TKA were comparable or superior to those of MA-TKA after a minimum 2-year follow-up. This review also showed that the JLOA in KA-TKA was relatively parallel to the floor compared to that in the native knee, and not oblique (medial side up and lateral side down) compared to that in MA-TKA9. In the present study, 55.2% of knees were classified to the in-range group with the JLOA, and 44.8% were classified to the outlier group. Although the goal of JLOA in the FINE knee is considered to be 3°, the in-range group did not have better clinical results including flexion angle, the KSS, and all subscales of the KOOS than the outlier group. Similar results have been shown by previous studies5,6,7,8,9,10. In this study, we showed that a half of patients got ‘in-range’ JLOA when the ‘in-range’ was defined between 2 and 4° with such limited range (Fig. 3); however, this does not mean that there are only 50% chances to get good alignment when performing TKA using our surgical technique. It remains to be argued whether the JLOA of 2–4° is adopted to ‘in-range’.
A recent classification for coronal plane alignment of the knee (CPAK) has simplified categorization of knee phenotypes based on two independent variables, constitutional (prearthritic) alignment, termed the arithmetic HKA, and joint line obliquity38. Sappey-Marinier et al., using the CPAK classification, investigated whether better clinical outcomes would be obtained in patients with a restored knee phenotype at 2 years follow-up after MA-TKA39. The results showed that only 18% of patients had restored constitutional knee phenotype, and neither restored obliquity nor arithmetic HKA was associated with clinical outcomes including flexion angle and the KSS. These observations suggest that performing MA-TKA resulted in most cases in a change of the preoperative knee phenotype, and restoration of the knee phenotype did not always lead to better clinical outcomes. As the clinical outcomes were short-term and physician-based alone, the mid- to long-term follow-up and the PROs will be required to evaluate the importance of restoration of the knee phenotype. The femoral rotational alignment is also likely to change when performing TKA in the concept to restore preoperative joint line inclination. The impact of postoperative inclination of the joint line in the femoral axial plane on clinical outcomes should be investigated in the future studies.
The multivariate logistic analysis revealed significant association between age at operation and postoperative KS-FS of > 80 points, and neither HKA in-range nor JLOA in-range were associated with the higher function (Table 4). These results demonstrate that younger age at surgery is important to obtain higher knee function and may suggest the alignment or joint line inclination to be targeted should not be limited in the narrow range regarding functional outcome in the short-term.
Recently, a wide distribution of femoral and tibial coronal alignment in normal knees has been identified40,41,42,43,44, which suggests the need for a more individualized approach in TKA40. Taken together with our results, reconstructing inclination of the joint line to a uniform angle, that is 3°, may not lead to an improvement in clinical outcomes. It might be a better surgical strategy to reproduce the inclination of the joint line to its constitutional state in each patient. Further investigation with mid- to long-term follow-ups will be required to demonstrate the impact of restoration of inclination of the joint line on clinical outcomes after TKA.
In this study we replaced patellae for 63.4% of patients, which might affect clinical outcomes including PROs. However, in the multivariate analysis patellar replacement was not associated with higher knee function (Table 4). A long-term follow-up will be necessary to evaluate the influence of patellar replacement on clinical outcomes.
There are some limitations to this study. First, the sample size was relatively small and the patients were recruited from a single institution. To establish the impact of postoperative joint line on clinical outcomes, more cases will be required from multiple institutions. Second, approximately 40% of patients did not receive patellar replacement, which could not be ignored when investigating the influence of other variables on postoperative outcomes. Third, inclination of the joint line was assessed by a coronal plane alone, and it should be also assessed by a sagittal plane in the future studies. Fourth, knees were divided into two groups (the HKA or JLOA in-range and outlier). Especially, it remains to be argued to set physiological inclination of the joint line at 2–4° of the JLOA.
In conclusion, neither TKA-postoperative inclination of the joint line nor limb alignment was relevant to the short-term PROs. Treatment strategies that attempt to make joint line inclination in order to improve postoperative PROs should be avoided, and alignment goals such as kinematic alignment should be considered carefully. Further investigation with mid- to long-term follow-ups will be required to show the impact of restoration of physiological inclination of the joint line on clinical outcomes after TKA.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Baker, P. N., van der Meulen, J. H., Lewsey, J. & Gregg, P. J. National Joint Registry for England and Wales. The role of pain and function in determining patient satisfaction after total knee replacement. Data from the National Joint Registry for England and Wales. J. Bone Jt. Surg. Br. 89, 893–900 (2007).
Clement, N. D., Macdonald, D. & Burnett, R. Predicting patient satisfaction using the Oxford knee score: Where do we draw the line?. Arch. Orthop. Trauma Surg. 133(5), 689–694 (2013).
Minns, R. J. The role of gait analysis in the management of the knee. Knee 12(3), 157–162 (2005).
Howell, S. M., Kuznik, K., Hull, M. L. & Siston, R. A. Results of an initial experience with custom-fit positioning total knee arthroplasty in a series of 48 patients. Orthopedics 31(9), 857–863 (2008).
Howell, S. M., Shelton, T. J. & Hull, M. L. Implant survival and function ten years after kinematically aligned total knee arthroplasty. J. Arthroplasty 33(12), 3678–3684 (2018).
Woon, J. T. K. et al. Outcome of kinematic alignment using patient-specific instrumentation versus mechanical alignment in TKA: a meta-analysis and subgroup analysis of randomised trials. Arch. Orthop. Trauma Surg. 138(9), 1293–1303 (2018).
Young, S. W. et al. The Chitranjan S. Ranawat Award: no difference in 2-year functional outcomes using kinematic versus mechanical alignment in TKA: a randomized controlled clinical trial. Clin Orthop Relat Res. 475(1), 9–20 (2017).
Laende, E. K., Richardson, C. G. & Dunbar, M. J. A randomized controlled trial of tibial component migration with kinematic alignment using patient-specific instrumentation versus mechanical alignment using computer-assisted surgery in total knee arthroplasty. Bone Jt. J. 101B(8), 929–940 (2019).
Lee, Y. S. et al. Kinematic alignment is a possible alternative to mechanical alignment in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 25(11), 3467–3479 (2017).
An, V. V. G., Twiggs, J., Leie, M. & Fritsch, B. A. Kinematic alignment is bone and soft tissue preserving compared to mechanical alignment in total knee arthroplasty. Knee 26(2), 466–476 (2019).
Teeter, M. G. et al. Varus tibial alignment is associated with greater tibial baseplate migration at 10 years following total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 26(6), 1610–1617 (2018).
Howell, S. M., Hodapp, E. E., Vernace, J. V., Hull, M. L. & Meade, T. D. Are undesirable contact kinematics minimized after kinematically aligned total knee arthroplasty? An intersurgeon analysis of consecutive patients. Knee Surg. Sports Traumatol. Arthrosc. 21(10), 2281–2287 (2013).
Nakajima, A. et al. Association between limb alignment and patient-reported outcomes after total knee arthroplasty using an implant that reproduces anatomical geometry. J. Orthop. Surg. Res. 13(1), 320. https://doi.org/10.1186/s13018-018-1030-8 (2018).
Lombardi, A. V. Jr., Ellison, B. S. & Berend, K. R. Polyethylene wear is influenced by manufacturing technique in modular TKA. Clin. Orthop. Relat. Res. 466, 2798–2805 (2008).
Insall, J. N., Dorr, L. D., Scott, R. D. & Scott, W. N. Rationale of the Knee Society clinical rating system. Clin. Orthop. Relat. Res. 248, 13–14 (1989).
Nakamura, N. et al. Cross-cultural adaptation and validation of the Japanese Knee Injury and Osteoarthritis Outcome Score (KOOS). J. Orthop. Sci. 16(5), 516–523 (2011).
Hutt, J., Masse, V., Lavigne, M. & Vendittoli, P. A. Functional joint line obliquity after kinematic total knee arthroplasty. Int. Orthop. 40(1), 29–34 (2016).
D’Amato, M., Kosse, N. M. & Wymenga, A. B. Restoration of pre-operative joint orientation and alignment does not affect KSS and KOOS 1 year after total knee arthroplasty. Knee Knee Surg. Sports Traumatol. Arthrosc. 29(10), 3170–3177 (2021).
Matsumoto, T. et al. Radiological and clinical comparison of kinematically versus mechanically aligned total knee arthroplasty. Bone Jt. J. 99B, 640–646 (2017).
Ji, H. M., Han, J., Jin, D. S., Seo, H. & Won, Y. Y. Kinematically aligned TKA can align knee joint to horizontal. Knee Surg Sports Traumatol Arthrosc. 24(8), 2436–2441 (2016).
Nfakajima, A. et al. Three-year clinical and radiological results of a cruciate-retaining type of the knee prosthesis with anatomical geometry developed in Japan. BMC Musculoskelet. Disord. 22(1), 241 (2021).
Kellgren, J. H. & Lawrence, J. S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 16(4), 494–502 (1957).
Abdel, M. P. et al. Effect of postoperative mechanical axis alignment on survival and functional outcomes of modern total knee arthroplasties with cement: a concise follow-up at 20 years. J. Bone Jt. Surg. Am. 100A(6), 472–478 (2018).
Hatayama, K., Terauchi, M., Saito, K. & Higuchi, H. Does residual varus alignment cause increasing varus laxity at a minimum of 5 years after total knee arthroplasty?. J. Arthroplasty. 32(6), 1808–1813 (2017).
Hooper, G., Rothwell, A. & Frampton, C. The low contact stress mobile-bearing total knee replacement: a prospective study with a minimum follow-up of ten years. J. Bone Jt. Surg. Br. 91B, 58–63 (2009).
Matziolis, G., Adam, J. & Perka, C. Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement. Arch. Orthop. Trauma Surg. 130(12), 1478–1491 (2010).
Slevin, O., Amsler, F. & Hirshmann, M. T. No correlation between coronal alignment of total knee arthroplasty and clinical outcomes: a prospective clinical study using 3D-CT. Knee Surg. Sports Traumatol. Arthrosc. 26(6), 1610–1617 (2017).
Stucinskas, J. et al. Moderate varus/valgus malalignment after total knee arthroplasty has little effect on knee function or muscle strength. Acta Orthop. 86(6), 728–733 (2015).
Kuroda, Y. et al. Varus deformity in the proximal tibia and immediate postoperative varus alignment result in varus progression in limb alignment in the ling term after total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 28, 3287–3293 (2020).
Moreland, J. R., Bassett, L. W. & Hanker, G. J. Radiographic analysis of the axial alignment of the lower extremity. J. Bone Jt. Surg. Am. 69(5), 745–749 (1987).
Hsu, R. W., Himeno, S., Coventry, M. B. & Chao, E. Y. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin. Orthop. Relat. Res. 255, 215–227 (1990).
Cooke, D. et al. Axial lower limb alignment: comparison of knee geometry in normal volunteers and osteoarthritis patients. Osteoarthritis Cartilage 5, 39–47 (1997).
Tang, W. M., Zhu, Y. H. & Chiu, K. Y. Axial alignment of the lower extremity in Chinese adults. J. Bone Jt. Surg. Am. 82A(11), 1603–1608 (2000).
Mullaji, A. B., Marawar, S. V. & Mittal, V. A comparison of coronal plane axial femoral relationships in Asian patients with varus osteoarthritic knees and healthy knees. J. Arthroplasty. 24(6), 861–867 (2009).
Hovinga, K. R. & Lerner, A. L. Anatomic variations between Japanese and Caucasian populations in the healthy young adult knee joint. J. Orthop. Res. 27, 1191–1196 (2009).
Nakano, N. et al. Coronal lower limb alignment in normal knees-a radiographic analysis of 797 normal knee subjects. Knee 23, 209–213 (2016).
Toguchi, K. et al. Predicting clinical outcomes after total knee arthroplasty from preoperative radiographic factors of the knee osteoarthritis. BMC Musculoskelet. Disord. 21(1), 9 (2020).
MacDessi, S. J., Griffiths-Jones, W., Harris, I. A., Bellemans, J. & Chen, D. B. Coronal plane alignment of the knee (CPAK) classification. Bone Jt. J. 103B(2), 329–337 (2021).
Sappey-Marinier, E. et al. Mechanical alignment for primary TKA may change both knee phenotype and joint line obliquity without influencing clinical outcomes: a study comparing restored and unrestored joint line obliquity. Knee Surg. Sports Traumatol. Arthrosc. https://doi.org/10.1007/s00167-021-06674-w (2021).
Hirschmann, M. T. & Behrend, H. Functional knee phenotypes: a call for a more personalized and individualized approach to total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 26(10), 2873–2874 (2018).
Hirschmann, M. T. et al. Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg. Sports Traumatol. Arthrosc. 27(5), 1394–1402 (2019).
Hirschmann, M. T. et al. Phenotyping the knee in young non-osteoarthritic knees shows a wide distribution of femoral and tibial coronal alignment. Knee Surg Sports Traumatol. Arthrosc. 27(5), 1385–1393 (2019).
Moon, Y. W., Park, J. H., Lee, S. S., Kang, J. W. & Lee, D. H. Distal femoral phenotypes in Asia varus osteoarthritic knees. Knee Surg. Sports Traumatol. Arthrosc. https://doi.org/10.1007/s00167-020-06131-0 (2020).
Hess, S. et al. Osteoarthritic and non-osteoarthritic patients show comparable coronal knee joint line orientation in a cross-sectional study based on 3D reconstructed CT images. Knee Surg. Sports Traumatol. Arthrosc. https://doi.org/10.1007/s00167-021-06740-3 (2021).
Funding
This study was supported by a Grant-in-Aid for Scientific Research of Japan Society for the Promotion of Science (20K09469 to A.N).
Author information
Authors and Affiliations
Contributions
M.Y. participated in the design of the study, performed the statistical analysis and drafted the manuscript. A.N. planed the design of the study, completed the manuscript. M.S. and Y.A. participated in the design of the study and performed statistical analyses. J.S. and M.N. participated in the design of the study and helped to draft the manuscript. K.Y., K.K. and S.T. collected patients’ clinical information and made a part of figures and tables. Y.A., T.S. and K.N. conceived of the study, participated in its design and coordination and helped to revise the manuscript. All authors read and approved the final manuscript. All patients gave their written consent to publish to report individual patient data.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yamada, M., Nakajima, A., Sonobe, M. et al. The impact of postoperative inclination of the joint line on clinical outcomes in total knee arthroplasty using a prosthesis with anatomical geometry. Sci Rep 13, 979 (2023). https://doi.org/10.1038/s41598-023-28182-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-28182-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.