Abstract
For pre-operative osteoarthritis (OA) patients with varus knee, previous studies showed inconsistent results. Therefore, we conducted this study to better identify the association of Hospital for Special Surgery (HSS) score and mechanical alignment. 44 patients (51 knees) with constitutional varus knee caused by combined deformities (LDFA (lateral distal femoral angle) > 90°and MPTA (medial proximal tibial angle) < 85°)) were selected and analyzed with a mean follow-up period of 14 months after total knee arthroplasty (TKA). From January 2015 to December 2016, patients were collected consecutively after primary TKA. After filtering, fifty-one knees (44patients) were analyzed with a mean follow-up period of 14 months. All patients were divided into two groups based on post-operative hip-knee-ankle (HKA) acute angle: varus mechanical alignment (VMA) group (HKA < − 3°) and neutral mechanical axis (NMA) group (− 3° ≤ HKA ≤ 3°). 30 knees were included in the NMA group, and 21 knees in the VMA group. Comparisons of HSS between NMA group and VMA group were performed. After adjusting for age and Body Mass Index (BMI) confounders, Compared with NMA group, the HSS score in VMA group decreased by 0.81 units (95% CI, − 3.37 to 1.75) p = 0.5370). For pre-operative constitutional varus knee caused by combined deformities in chinese populations, no significant association between post-operative lower limb mechanical alignment and HSS score was found.
Similar content being viewed by others
Introduction
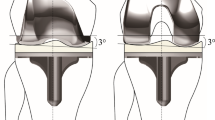
Generally, achieving a post-operative neutral lower limb mechanical alignment within 3° is regarded as a golden standard in total knee arthroplasty (TKA) for a long time, which is widely regarded being associated with optimal clinical function. Mechanical alignment principle demands that tibial and femoral cuts are perpendicular to the mechanical axis of the tibia and femur in the coronal plane, respectively1. Based on this principle, the neutral mechanical alignment in the coronal plane is defined as or characterized by hip-knee-ankle (HKA) acute angle of 0° ± 3°(mean and standard deviation)2,3,4.
The Hospital for Special Surgery (HSS)score 5 which was proposed by American Hospital in 1976 consists of the following six parts: pain (30 points), function (22 points), range of motion (18points), muscle strength (10points), knee flexion deformity(10points), and stability (10points). When the patients walk with the help of the crutches or there are varus deformity or valgus deformity in their knee-joints, these points will be reduced accordingly. HSS scoring system6 emphasizes pain, function and range of motion, which is well known for its high degree of inter-observer correlation7. The clinical function score is a reflection of the satisfaction score. Dissatisfaction is the patients’ unsatisfied state or attitude; which consist of discontent; displeased, or a particular reason or feeling of displeasure or disappointment. It is estimated that 20% of elderly osteoarthritis patients (about 60 million people) in the United States will need surgery by 20208 . However, about 20% of patients are not satisfied with clinical outcome of TKA 9,10,11. Therefore, even a small promotion of satisfaction could have a substantial impact on patients who are performed with TKA.
Constitutional varus knee was characterized by the physiologic mechanical axis is 3° varus or more12, which takes a big proportion in medial OA patients13. Although many studies have explored the association between post-operative mechanical alignment and clinical outcomes in pre-operative varus knee populations, it is worth noting that previous studies showed inconsistent results14,15,16. Some studies14,16 found that TKA performed in patients with pre-operative varus deformity had superior clinical outcomes when the lower limb mechanical alignment was left in residual varus, while another studies17,18,19 found that post-operative varus mechanical alignment has no significant effect on patient’s clinical outcomes compared with the neutral mechanical alignment. And the majority of patients in above studies were Europeans or Americans who previously had varus knees, and their results may not be generalized to other populations with different lifestyles or disease.
Therefore, we conducted a retrospective study in Chinese populations to better identify the association of post-operative mechanical alignment and HSS score after primary TKA of patients suffering from constitutional varus knee that caused by combined deformities.
Methods
Demographics
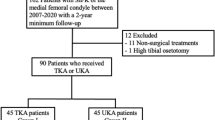
From January 2015 to December 2016, a doctor who was not involved in the surgery consecutively collected clinical data in this research. The target are patients suffering from constitutional varus knee that caused by combined femoral and tibial deformities before surgery 12 was consecutively collected. To get accurate experimental data, patients with bone on bone were excluded in this study. Each patient is selected according to the following inclusion and exclusion criteria. The inclusion criteria encompasses following points: (1) unilateral medial end-stage OA ((Kellgren-Lawrence grade) K/L grade III or IV) and contralateral knee joints with cartilage loss less than 50% (K/L grade 0–II); (2) bilateral medial end-stage OA patients (K/L grade III). The exclusion criteria includes five points: (1) rheumatoid or inflammatory arthritis; (2) external joint deformity; (3) posttraumatic; (4) abnormal condition caused by diseases (such as Paget’s or rickets etc.); (5) inappropriate preoperative or post-operative radiographs. 53 patients (78 knees) met above standard totally. After filtering, 44 patients (51 knees) who met inclusion criteria underwent follow-up (Fig. 1). 3 patients who met inclusion criteria could not participate in the experiment because post-operative radiographs were not available (n = 3). 4 patients were lost during follow-up (n = 4); 2 patient's radiographs did not meet Paley's criteria (n = 2). This study have got the informed consent of all patients. Ethical approval was granted by the Chinese PLA General Hospital medical ethics committee (S-2018-018-01). All experiments were performed in accordance with relevant guidelines and regulations.
Radiographic evaluation
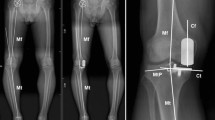
Pre-operative and post-operative full-length standing radiographs were collected and measured according to Paley’s criteria using the Mimics medical imaging programme (version 16.0; Materialise, Leuven, Belgium) with an accuracy within 0.1 mm20. All patients stood barefoot with the patellae pointed straight ahead20 during radiographic scan. The criteria of the femoral and tibial mechanical axis defined by Cooke et al21 was adopted in this study.
LDFA
The LDFA is the lateral angle that formed by the mechanical axis of the femur and the knee joint line of the femur in the coronal plane.
MPTA
The MPTA is the medial angle which formed by the mechanical axis of the tibia and the knee joint line of the tibia in the coronal plane.
HKA
The HKA angle was defined as the included angle between the femoral mechanical axis and the tibial mechanical axis22,23 (Fig. 2). This acute angle was expressed as a deviation from 0° with a negative value for varus knee and positive value for valgus knee.
Clinical evaluation
Pre-operative and post-operative knee functional scores were calculated using the HSS scale24. The patients’ baseline characteristics included age, BMI and follow-up time. The maximum range of motion of the knee was measured by a goniometer at 12 months after surgery.
Statistical analysis
Comparative statistical analyses between VMA group and NMA group after TKA were performed in SPSS software 22.0 (SPSS, Chicago, IL) with the independent sample t test, a p value < 0.05 was adopted. These measured parameters were summarized by the mean and standard deviation.
Results
General observations
There was no significant difference in baseline characteristics regarding age, BMI and Follow-up time, which are shown in Table 1. For all patients, there are significant differences between pre-operative and post-operative HSS score, MPTA, LDFA, HKA angles, respectively. (Fig. 3A,B). In general, the HSS score were improved from 48.23 ± 10.34 points before surgery to 86.71 ± 4.49 points at the final follow-up examination (p < 0.05).
Pre-operative and post-operative comparison between two groups
Post-operative LDFA in NMA group was larger than VMA group (90.87° ± 2.13° vs 94.06° ± 2.60°), there was a significant statistical difference between the two groups (p = 0.001). Meanwhile, Post-operative MPTA in NMA group was larger than VMA group (89.81° ± 1.54° vs 88.78° ± 1.79°), there was a significant difference between the two groups (p = 0.038). For NMA group, the Mean and standard deviation of HKA was 1.80° ± 1.03°, for the VMA group, the Mean and standard deviation (11.53° ± 4.15°) were more than three and two times larger than those of NMA group. A significant difference was detected between the two groups (p < 0.05). No significant differences were observed in HSS score between NMA group and VMA group (87.29 ± 3.41 vs 86.30 ± 5.13) after operation (p < 0.05) (Fig. 4).
Discussion
Previous studies14,15 showed inconsistent results, a retrospective study was conducted to better identify the association between mechanical alignment and post-operative HSS score after primary TKA in this study. The most important finding of the current study was that we found no significant association between post-operative lower limb mechanical alignment and HSS score for patients in Chinese with pre-operative constitutional varus knee caused by combined deformities. .
Experimental results on the association between mechanical alignment and HSS score in this research is consistent with previous studies 15,22,25,26. Michael et al22 proved that leaving varus knees in residual varus will not improve clinical outcomes in a retrospective review of 361 primary TKAs. Dominique et al. 27 also found there were similar clinical outcomes for neutral or varus alignment. Richard et al.26 concluded that there was no correlation between post-operative lower limb mechanical alignment and clinical outcomes for patients with pre-operative varus deformity. However, the previous research objects were Europeans or Americans who previously had varus knees. Here, the patients in Chinese with pre-operative constitutional varus knee caused by combined deformities were selected, and a new evidence was provided in this study.
For these OA patients with constitutional varus knee, there are many intraoperative difficulties and post-operative complications if applying neutral mechanical axis method. Firstly, it widely needs to release medial soft tissue, including socket stripping insertion of medial soft tissue of the tibia17, stripping popliteal ligament, superficial medial collateral ligament and so on18. It is widely known that excessive release of the soft tissue may result in bleeding, knee instability. Secondly, by applying reduction osteotomy of tibial plateau, Dixon et al.19 corrected severe varus knee deformity and improved patients' Knee Society Clinical Rating System (KSS) score and activity level. However, along with the narrowing of the tibial plateau, the contact area of the tibial plateau is decreased, meanwhile the wear of artificial joints will be increased under the same loading circumstance. Moreover, tibial prosthesis cannot cover the lateral tibial margin after reduction osteotomy, which will increase the sinking risk of the tibial component, because spongy bone of lateral-medial tibial plateau resulted in a relative ingression to adapt tracking of femoral component. When there exists residual varus deformity during the operation, the above complications can be reduced. In addition, obtaining neutral mechanical axis among these patients is more difficult and time-consuming procedure, which requires more complex bone cuts and larger soft tissue releases. Sampath et al.28 also described the need for increased operative time to obtain neutral axis of the lower limb in severe varus knees. In this study, slight varus mechanical alignment of the lower limb after TKA can reduce the difficulty and save operative time for surgeon.
This study has several limitations. Firstly, this study was a retrospective. Second, in the case of proximal tibia and distal femur bone on bone, the parameters of normal knee joint was measured. However, according to Dargel’s result29, there was a positive correlation in morphometric data between two knees for one subject. At last, static lower limb mechanical axis was not associated with clinical results while dynamic axis may be a predictor of clinical performances after TKA, because Miller et al.30 found the standing mechanical axis after TKA was not enough to predict dynamic behavior of the lower limb during gait. Thus, a prospective study with large samples is required in the future.
Conclusion
For patients suffering from constitutional varus knee that caused by combined deformities among Chinese populations, we found no significant association between post-operative lower limb mechanical alignment and HSS score in our study. Slight varus mechanical alignment of the lower limb after TKA can reduce the difficulty and save operative time for surgeon.
References
Insall, J., Scott, W. N. & Ranawat, C. S. The total condylar knee prosthesis. A report of two hundred and twenty cases. J. Bone Jt. Surg. 61, 173–180 (1979).
Jeffery, R. S., Morris, R. W. & Denham, R. A. Coronal alignment after total knee replacement. J. Bone Jt. Surg. 73, 709–714 (1991).
Abdel, M. P. et al. Coronal alignment in total knee replacement: historical review, contemporary analysis, and future direction. Bone Jt. J. 96-B, 857 (2014).
Thienpont, E., Schwab, P. E. & Fennema, P. J. B. J. J. A systematic review and meta-analysis of patient-specific instrumentation for improving alignment of the components in total knee replacement. Bone Jt. J. 410, 1052–1061 (2014).
Insall, J. J. C. O. & Research, R. Rationale of the Knee Society clinical rating system. 248 (1989).
Davies, A. P. J. K. Rating systems for total knee replacement. Orthopedics 9, 261–266 (2002).
Bach, C. M. et al. Scoring systems in total knee arthroplasty. Bone Jt. J. 399, 184 (2002).
Walcott, B. P., Hanak, B. W., Caracci, J. R., Redjal, N. & Coumans, J. V. C. E. J. S. N. I. Trends in inpatient setting laminectomy for excision of herniated intervertebral disc: Population-based estimates from the US nationwide inpatient sample. Surg. Neurol. Int. 2, 7 (2011).
Bourne, R. B., Chesworth, B. M., Davis, A. M., Mahomed, N. N. & Charron, K. D. J. Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? 468, 57–63.
Robertsson, O., Dunbar, M., Pehrsson, T. r., Knutson, K. & Lidgren, L. J. A. O. Patient satisfaction after knee arthroplasty: A report on 27,372 knees operated on between 1981 and 1995 in Sweden. 71, 262–267.
Scott, C. E. H., Howie, C. R., MacDonald, D., Biant, L. C. J. J. o. B. & Volume, J. S. B. Predicting dissatisfaction following total knee replacement: A prospective study of 1217 patients. 92-B, 1253–1258.
Bellemans, J., Colyn, W., Vandenneucker, H. & Victor, J. The Chitranjan Ranawat award: Is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin. Orthop. Relat. Res. 470, 45–53. https://doi.org/10.1007/s11999-011-1936-5 (2012).
Vandekerckhove, P. et al. The relationship between constitutional alignment and varus osteoarthritis of the knee. Knee Surg. Sports Traumatol. Arthrosc. 25, 2873–2879. https://doi.org/10.1007/s00167-016-3994-4 (2017).
Vanlommel, L., Vanlommel, J., Claes, S. & Bellemans, J. Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg. Sports Traumatol. Arthrosc. 21, 2325–2330. https://doi.org/10.1007/s00167-013-2481-4 (2013).
Rames, R. D., Mathison, M., Meyer, Z., Barrack, R. L. & Nam, D. No impact of under-correction and joint line obliquity on clinical outcomes of total knee arthroplasty for the varus knee. Knee Surg. Sports Traumatol. Arthrosc. 26, 1506–1514. https://doi.org/10.1007/s00167-017-4507-9 (2018).
Nishida, K. et al. Remaining mild varus limb alignment leads to better clinical outcome in total knee arthroplasty for varus osteoarthritis. (2016).
Thienpont, E., Cornu, O., Bellemans, J. & Victor, J. Current opinions about coronal plane alignment in total knee arthroplasty: A survey article. Acta Orthop. Belg. 81, 471–477 (2015).
Morgan, S. S. et al. The influence of postoperative coronal alignment on revision surgery in total knee arthroplasty. Int. Orthop 32, 639–642. https://doi.org/10.1007/s00264-007-0391-0 (2008).
Shelton, T. J., Nedopil, A. J., Howell, S. M. & Hull, M. L. Do varus or valgus outliers have higher forces in the medial or lateral compartments than those which are in-range after a kinematically aligned total knee arthroplasty? Limb and joint line alignment after kinematically aligned total knee arthroplasty. Bone Jt. J. 99, 1319–1328. https://doi.org/10.1302/0301-620x.99b10.Bjj-2017-0066.R1 (2017).
Dror Paley, F. Principles of Deformity Correction (Springer, Berlin, 2002).
Derek, T., Cooke, V., Sled, E. A. & Scudamore, R. A. Frontal plane knee alignment: A call for standardized measurement. J. Rheumatol. 34, 1796–1801 (2007).
Meneghini, R. M., Grant, T. W., Ishmael, M. K. & Ziemba-Davis, M. Leaving residual varus alignment after total knee arthroplasty does not improve patient outcomes. J. Arthroplasty 32, S171–S176. https://doi.org/10.1016/j.arth.2017.02.064 (2017).
Nishida, K. et al. Remaining mild varus limb alignment leads to better clinical outcome in total knee arthroplasty for varus osteoarthritis. Knee Surg. Sports Traumatol. Arthrosc. 25, 3488–3494. https://doi.org/10.1007/s00167-016-4260-5 (2017).
Slupik, A. & Bialoszewski, D. Comparative analysis of clinical usefulness of the Staffelstein Score and the Hospital for Special Surgery Knee Score (HSS) for evaluation of early results of total knee arthroplasties. Preliminary report. Ortop. Traumatol. Rehabil. 9, 627–635 (2007).
Stucinskas, J. et al. Moderate varus/valgus malalignment after total knee arthroplasty has little effect on knee function or muscle strength. Acta Orthop. 86, 728–733 (2015).
Rames, R. D., Mathison, M., Meyer, Z., Barrack, R. L. & Nam, D. No impact of under-correction and joint line obliquity on clinical outcomes of total knee arthroplasty for the varus knee. Knee Surg. Sports Traumatol. Arthrosc. https://doi.org/10.1007/s00167-017-4507-9 (2017).
Saragaglia, D. et al. Influence of the post-operative axis on the clinical results of total knee replacement for severe varus deformities: Does a slight residual varus improve the results?. Int. Orthop. https://doi.org/10.1007/s00264-018-4092-7 (2018).
Sampath, S. A., Voon, S. H., Sangster, M. & Davies, H. The statistical relationship between varus deformity, surgeon’s experience, BMI and tourniquet time for computer assisted total knee replacements. Knee 16, 121–124. https://doi.org/10.1016/j.knee.2008.09.008 (2009).
Dargel, J., Feiser, J., Gotter, M., Pennig, D. & Koebke, J. Side differences in the anatomy of human knee joints. Knee Surg. Sports Traumatol. Arthrosc. 17, 1368–1376. https://doi.org/10.1007/s00167-009-0870-5 (2009).
Miller, E. J., Pagnano, M. W. & Kaufman, K. R. Tibiofemoral alignment in posterior stabilized total knee arthroplasty: Static alignment does not predict dynamic tibial plateau loading. J. Orthop. Res. 32, 1068–1074 (2014).
Author information
Authors and Affiliations
Contributions
Z.Z. and W.C. contributed equally, and they are co-first author. Z.J. and Y.Q. are co-corresponding author. W.C., Y.Q. and Z.J. provided the ideas of this study. Z.Z. collected the data and wrote the manuscript. Y.Z., X.W. and Z.C. analyzed the patientdata. G.Z., Q.Z. helped with the interpretation of data. P.W. made some contributions to the revision.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, Z., Chai, W., Zhao, G. et al. Association of HSS score and mechanical alignment after primary TKA of patients suffering from constitutional varus knee that caused by combined deformities: a retrospective study. Sci Rep 11, 3130 (2021). https://doi.org/10.1038/s41598-021-81285-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-81285-6
This article is cited by
-
Effect of knee joint weight change on knee function recovery and gait after total knee arthroplasty
BMC Musculoskeletal Disorders (2022)
-
Short-term outcomes of Oxford unicompartmental knee arthroplasty with coronal subluxation of the knee: a retrospective case–control study
Journal of Orthopaedics and Traumatology (2022)
-
Survival, functional outcome and satisfaction of first revision total knee arthroplasty at a mean eleven-year follow-up
European Journal of Orthopaedic Surgery & Traumatology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.