Abstract
The knee joint center of rotation is altered in the absence of the anterior cruciate ligament, which leads to substantially higher variance in kinematic patterns. To overcome this, total knee arthroplasty (TKA) designs with a high congruency in the lateral compartment have been proposed. The purpose of this study was to analyze the influence of a lateral pivot TKA-design on in-vivo knee joint kinematics. Tibiofemoral motion was retrospectively addressed in 10 patients during unloaded flexion-extension and loaded lunge using single plane fluoroscopy. During the unloaded flexion-extension movement, the lateral condyle remained almost stationary with little rollback at maximum flexion. The medial condyle exhibited anterior translation during the whole flexion cycle. During the loaded lunge movement, a higher degree of rollback compared to the unloaded activity was observed on the lateral condyle, whereas the medial condyle remained almost stationary. The results showed a clear lateral pivot during the unloaded activity, reflective of the implant’s geometric characteristics, and a change to a medial pivot and a higher lateral rollback during the weight-bearing conditions, revealing the impact of load and muscle force. It remains unclear if the kinematics with a lateral TKA design could be considered as physiological, due to the limited knowledge available on native knee joint kinematics.
Similar content being viewed by others
Introduction
Though the survival rate in total knee arthroplasties (TKA) has improved1, a relevant number of patients (20%) remain unsatisfied with the outcome, regardless of specific TKA design features. Across most designs, postoperative knee pain persists without a distinct radiological or clinical reason2,3. One of the main known causes is non-physiological kinematics4. However, it remains under debate until what extent the surgical technique, such as soft-tissue balancing, and implant geometry, such as curved radii, have a direct influence on the knee joint kinematics5.
Despite various developments in TKA implant designs, which include fixed bearing, rotating platform, cruciate retaining and posterior stabilized geometries, it remains unclear which design is superior for achieving a physiological kinematics6,7,8. In particular, studies on the kinematics of symmetrical femoral component designs showed inconsistent femoral anterior-posterior (AP) translation during flexion, which also often report increased patellofemoral and anterior knee pain9,10,11,12. Furthermore, it has been suggested that such excessive AP motion could result in bony impingement between the femur and the posterior rim of the tibial insert13,14,15,16.
If a proper TKA component alignment as well as ligament balancing has been conducted, a proper soft tissue guidance of the knee replacement may be retained16,17,18,19. However, excessive ligament tensioning limits the extent of movement, while loose ligaments leads to knee joint instability20,21, both of which can be reasons for revision surgery22,23,24. Both instability and unbalanced ligament structures may lead to pronounced asymmetric polyethylene (PE) wear and thus, increased loosening rates24.
It has been reported that the native knee requires a specific degree of rollback of the lateral compartment coupled with a medial pivot25, which leads to an external axial rotation of the femur. This rollback is thought to be even more pronounced with increasing knee flexion angles to enable deep flexion without excessive shear forces acting at the patella or overloading the extensor mechanism25.
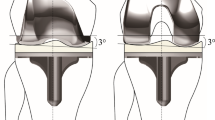
On the other hand, previous reports on the kinematics of healthy knees have shown a predominantly lateral pivot during low flexion activities such as walking and running26,27,28. In the absence of the anterior cruciate ligament (ACL), the center of rotation is altered from a medial to a lateral pivot, as reported by Yamaguchi and Isberg’s analysis of squats performed in ACL-deficient subjects29,30. In a similar analysis using fluoroscopy, Dennis and colleagues also reported an altered pivot as well as substantially higher variance in the pattern and magnitude of both AP translation and axial rotation31. In response, designs with high congruency in the lateral compartment have been developed and implemented in an attempt to overcome this. Such highly congruent lateral femoral condyle designs are consequently combined with a widened medial condyle to increase contact area and to minimize contact pressures32. Designs with this specific characteristics are named lateral pivoting designs.
Previous in vitro analyses of lateral pivoting designs have shown a change of the pivot position at 10 and 60 degrees of knee flexion33. Different reports on in vivo static analysis during kneeling and lunge activities have shown either a predominantly lateral pivot34,35 or a lateral rollback16,36. However, a comprehensive analysis of knee kinematics under weight-bearing or non-weight-bearing dynamic conditions in a set of TKA patients, particularly for demanding knee flexion activities, is currently lacking in the literature.
The purpose of this study was to analyze the influence of a lateral pivot TKA design on in vivo knee joint kinematics during knee flexion activities and to compare this to corresponding clinical data. Patients were analyzed at 2 years post-surgery to allow for a postoperative status that is not influenced by the current stage of rehabilitation. We hypothesized that kinematics in a TKA implant designed to exhibit a lateral pivot during the range of knee joint flexion would differ between loaded and unloaded knee flexion activities.
Materials and Methods
Patients
In a retrospective study, 10 subjects (66.1 years mean age (SD 6.1), 6 females, 33.2 mean BMI (SD 5.0)) were included for this analysis. All subjects were implanted with the 3D Knee™ fixed bearing cruciate retaining TKA design (DJO GLOBAL), which has an asymmetric femoral component design. This TKA exhibits high lateral congruency in extension, which decreases at higher flexion, as well as a widened medial condyle. Inclusion criteria were a primary diagnosis of osteoarthritis with a coronal deformity of <10°, as well as no previous open knee surgery. Patients were measured at 24 months post-surgery. The study was approved by the local ethics committee (Landesärztekammer Brandenburg, Germany, approval-Nr: S9 (A)/2016). All subjects provided written informed consent prior to participation. All investigations were performed in accordance with relevant guidelines/regulations.
Surgical technique
All surgeries were conducted under full general anesthesia, with standard pain management through blockades of the femoralis and ischiadicus nerves. A measured resection technique was applied and a constant tibia slope of 5° was maintained. The posterior cruciate ligament (PCL) was preserved and balanced with a spacer technique. All implants were fully cemented with reference to manufacturer guidelines. All surgeries were performed by the same surgeon, who was neither involved in data acquisition, data interpretation, nor preparation of the manuscript. Standard post-operative standard physiotherapy, pain treatment and clinical monitoring were conducted.
In vivo 3-D knee kinematics using single plane fluoroscopy
Single plane fluoroscopy analysis was conducted in all subjects using a Philips BV Pulsera device (Philips Medical Systems GmbH, Hamburg, Germany) to assess the tibiofemoral kinematics (30 Hz frame rate, 8 ms pulse width, beam energy 60 kVp, beam current 5 mA). Image resolution was 1024 × 1024 pixels with a 12-bit color depth. Additional images of a specially designed Perspex calibration box37 were collected to correct for image distortion.
All patients performed a single leg weight-bearing activity (lunge) and a single leg unloaded activity (flexion-extension) on the TKA limb to assess tibiofemoral knee kinematics under closed and open chain conditions, respectively. Special care was taken to clarify the activities to the subjects and to ensure correct performance during data collection.
During the lunge, both feet were at the same level but with the foot of the leg of interest positioned frontally to achieve a position of the knee to be analyzed as near as possible to the center of the image intensifier. The contralateral leg was in a more posterior position to avoid overlapping. The activity started at full extension and was conducted without a break until the maximal active possible knee flexion was achieved without help and was completed when full extension was reached again (Fig. 1).
The unloaded flexion-extension activity started also at full extension and was conducted without a break until maximal active possible flexion and finalize at full extension (Fig. 1). Three repetitions were collected during both activities. Considering the frame rate of 30 Hz and the varied duration of the activity (approximately 8–15 seconds), between 250 and 450 frames were collected during each repetition.
Clinical questionnaires
The following clinical questionnaires were collected: the Knee Society Score (KSS)38, consisting of the Knee Score (KS) and Function Score (FS)38, as well as Forgotten Joint Score (FJS)39, the High Flexion Knee Score (HFKS)40, and subjective patient postoperative satisfaction (10 points meaning maximal satisfaction with the prosthesis).
Data post-processing and analyses
The collected “Digital Imaging and Communications in Medicine” (DICOM) packages of every activity and repetitions were separated into single images. The images starting from maximal extension to maximal flexion were then used for fluoroscopic analysis. The 3D computer-aided-design (CAD) models of the femoral and tibial metallic components were registered to the fluoroscopic images as previously described41. Since single plane fluoroscopy is not a direct measurement method, the calculated joint kinematics depend highly on the accuracy of the CAD models42 and contour selection. In addition to the automatic contour detection method applied, manual corrections need to be conducted to select the relevant and also to discard the erroneous contour parts. The accuracy of the registration procedure has been analyzed previously under dynamic conditions with root mean square values of 0.2–0.6 mm for translations and 0.4–0.8 for rotations reported41.
The transformations after the registration procedure were used to reproduce the positions and orientations of the components using the AMIRA environment (Visage Imaging, Berlin, Germany). The origin of the tibial coordinate system was defined as the intersection of the tibia plateau with the tibia shaft axis, which also formed the Z-axis (pointing proximally), while the X-axis pointed right and the Y-axis anterior. The most distal points of the medial and lateral femoral condyles were determined and projected onto the tibia component plateau to generate a distal line43 (Fig. 2).
3-D Surface models of the total joint replacement implant. Upper left: distal lateral and medial condyle points (shortest distance between femur and tibia). Bottom left: most anterior tangency lateral and medial condyle points (shortest distance between femur and anterior frontal plane). Upper/bottom right, determination of the anterior-posterior translation with the medial/lateral distal and medial/lateral anterior tangency points respectively.
The axial rotation was defined as the angle between the distal line and the medio-lateral tibial axis. A frontal plane, perpendicular to the tibia plateau plane and positioned anteriorly, was used to determine the most anterior tangency medial and lateral femoral frontal points as a reference for the movement of the patella43 (Fig. 2). Both AP translations were expressed as the absolute values of the distal/anterior points relative to the origin of the tibial coordinate system. These values were resampled at 1° increments of knee flexion using linear interpolation to allow for determination of cohort means and standard deviations.
To analyze the relationship between kinematics and clinical outcomes, a correlation analysis was conducted between the FJS values and the AP translation at maximal achieved knee joint flexion for both the medial and lateral compartments.
Results
A clear variability in the initial position of the lateral and medial distal points can be observed in both activities in the extended position (Appendix Fig. 1).
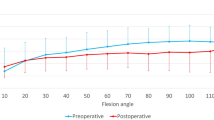
During the analysis of the flexion-extension activity, 7 subjects showed a relatively stationary position of the lateral condyle with additional little rollback at maximum flexion. On the other hand, the medial condyle continuously exhibited anterior translation during the whole flexion cycle in all patients (Appendix Fig. 1). In general, the subjects attained a high maximum flexion degree during this active non weight-bearing activity, with a flexion of 89.1 +/− 8.3° (mean +/−SD).
During the weight-bearing lunge, the lateral condyle showed a higher extent of rollback, which started approximately at mid-flexion, while the medial condyle remained stationary with additional anterior translation at approximately 50–60 degrees of flexion, although in less magnitude compared to the flexion-extension activity, (Appendix Fig. 1). Compared to the unloaded activity, less knee joint flexion could be reached by the subjects, with a flexion of 65.5 +/− 18.0°. The mean and standard deviations of the absolute values of this analysis are displayed in Table 1.
Considering the axial rotation, the initial anterior position of the medial, as well as the posterior position of the lateral distal points indicates an externally rotated position of the femoral component during extension. An increase of this external rotation was then identified in both measured activities with values at maximum flexion of 9.2 +/− 3.1° and 4.8 +/− 3.3° for the flexion extension and lunge respectively. A clear change of pivot from the medial compartment during the flexion-extension activity to the lateral compartment during the lunge activity could be observed (Fig. 3).
The medial and lateral anterior tangency points as reference of the movement towards the patella showed a continuous posterior translation of the lateral point in both activities. On the other hand, the medial point remained relatively stationary at the beginning of the unloaded flexion-extension activity, translating posteriorly at approximately 70° of knee joint flexion. While this posterior translation was relatively constant, although minor compared to the lateral point during lunge (Appendix Fig. 2). The mean and standard deviations of the absolute values of this analysis are displayed in Table 1.
Regarding the clinical questionnaires, a clear good passive flexion was observed in all subjects (mean: 133°, range: 125–145°) as well as a high subject’s satisfaction with the prosthesis (mean: 8.2, range: 5–10). A clear variability could be observed in the values of the FJS and HFKS. This information is collected in Table 2. The correlation analysis showed low correlation values (maximal R2 = 0.3478), however a tendency towards a reduced anterior position at high FJS values could be observed (Appendix Fig. 3).
Discussion
Tibiofemoral kinematics after TKA are determined by multiple factors such as patient-specific characteristics, surgical technique, soft-tissue balance, PCL strain, limb alignment, bearing design and femoral component geometry43. Inconsistent anterior translation of the femur in flexion has been previously observed in symmetrical femoral components, leading to a large variety of implants with their own advantages and limitations6,7,8. The analyzed implant in this study has a congruent lateral compartment with the aim to provide more AP stability and to prevent paradoxical motion in early and mid-flexion. On the other hand, the less conforming medial compartment aims to reduce the contact pressure and to drive femoral rollback32. Despite these targeted features, the analysis conducted in the present study shows different behavior during unloaded and loaded activities.
There is a clear anterior translation in the medial compartment during the unloaded flexion-extension accompanied by a relative stationary position, or pivoting, on the lateral compartment. This leads to the assumption that a knee joint kinematics reflective of the implant’s geometric characteristics takes place during this activity. However, during the loaded lunge activity, an anterior shift in the medial compartment is reduced and is accompanied by increased lateral rollback. If patients would have been able to achieve a higher knee joint flexion, this observed movement pattern may have been continued at higher knee flexion angles due to the progressively decreasing of the congruency. The lateral rollback observed is comparable to the reports on the same prosthesis design of previous studies. Posterior positions of the lateral condyle up to 7, 8, 9 and 15 mm have been also reported by Mikashima, Ginsel, Watanabe and Harman respectively16,34,35,36. However, such degrees of rollback were achieved in kneeling activities performed differently.
Importantly, a clear change of pivot was reported between the measured activities: while a clear lateral pivot was observed during the unloaded activities, a change towards a medial pivot was observed in the loaded lunge, likely due to the influence of muscle activation and axial load during closed chain activities44. Apart from this changed pivot, a clear external axial rotation of the femoral component relative to the tibia component was evident in both activities; however, the performance was location- and activity-dependent. The medial pivot during the loaded activity was coupled with an external rotation and a rollback of the lateral condyle, similar to the reports of Pinskerova and colleagues on healthy knees from extension to flexion25. However, the lateral pivot during the unloaded activity showed an external rotation coupled with an anterior sliding of the medial condyle. In contrast, this motion pattern has been observed in unconstrained TKA designs with up to 20% more prevalence of a lateral pivot during stair navigation15. It is also similar to the reports on healthy knees during walking and running26,27,28 and to the anterior translation of around 8 mm observed during knee flexion in the medial condyle of subjects with ACL deficient knees29.
The anterior shift of the medial condyle can be considered paradoxical and it has been shown that tibiofemoral roll-forward leads to increased patello-femoral contact forces4,45,46. However, the analysis of the anterior tangency points as reference of the movement towards the patella showed a shift towards posterior of the lateral and medial points, starting medially at 70° of knee joint flexion and continuously from extension to maximal flexion on the lateral compartment. This movement pattern could eventually leads to a relief of the patello-femoral contact force.
The clinical scores show the patients’ high satisfaction with the prosthesis and a tendency towards a reduced anterior position with high FJS values. However, the variability in the Forgotten Joint Score and the High Flexion Knee Score could be related to the limited sample size of analyzed patients. Possible causes of this variability could be the lack of controlled ligament tensioning as well as variable instrumentation.
The general variability observed in our clinical and fluoroscopic data could be related to different factors such as the patient’s level of activity, muscle weakness, body weight index, joint line angulation and loading conditions. Since a measured resection technique was applied during surgery and considering the actual knowledge about gap-balancing and controlled ligament tensioning, the clinical and kinematic performance could benefit from such specific approaches47,48.
This study is not free of limitations. First, it is a retrospective study design, which may include selection bias. Though patients were recruited from a single center, operated by single surgeon and treated under standardized protocols to provide comparability, bias may have impacted the findings. Second, only one design with the aforementioned geometric characteristics was analyzed within this study. Thus, any conclusion regarding other implant designs cannot be drawn. Third, pre-operative clinical data was not available, which weaken the interpretation of the post-operative outcome scores.
At 2 years post-surgery, the effect of weight bearing during high flexion activities appears to affect knee joint kinematics in this particular TKA implant. During the unloaded activity, the knee had a clear lateral pivot that was reflective of the implant’s geometric characteristics. Yet during the weight-bearing condition, there was a change to a medial pivot and a higher lateral rollback, which reveals the impact of load and muscle force. It remains unclear if the kinematics with a lateral TKA design could be considered as physiological, due to the limited knowledge available on native knee joint kinematics.
Data Availability
All relevant data are within the paper. Additional information associated with this article can be found at: https://osf.io/6a47x/?view_only=b9fd80cc7cff45a1bc64bd81aad574a8.
Change history
15 January 2020
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
Bonnin, M. P., Basiglini, L. & Archbold, H. A. What are the factors of residual pain after uncomplicated TKA? Knee Surg Sports Traumatol Arthrosc 19, 1411–1417, https://doi.org/10.1007/s00167-011-1549-2 (2011).
Maratt, J. D., Lee, Y. Y., Lyman, S. & Westrich, G. H. Predictors of Satisfaction Following Total Knee Arthroplasty. J Arthroplasty 30, 1142–1145, https://doi.org/10.1016/j.arth.2015.01.039 (2015).
Noble, P. C., Fuller-Lafreniere, S., Meftah, M. & Dwyer, M. K. Challenges in outcome measurement: discrepancies between patient and provider definitions of success. Clin Orthop Relat Res 471, 3437–3445, https://doi.org/10.1007/s11999-013-3198-x (2013).
Komistek, R. D. et al. In vivo comparison of femorotibial contact positions for press-fit posterior stabilized and posterior cruciate-retaining total knee arthroplasties. J Arthroplasty 17, 209–216 (2002).
Saffarini, M., Demey, G., Nover, L. & Dejour, D. Evolution of trochlear compartment geometry in total knee arthroplasty. Ann Transl Med 4, 1–6, https://doi.org/10.3978/j.issn.2305-5839.2015.12.53 (2016).
Bailey, O. et al. No clinical difference between fixed- and mobile-bearing cruciate-retaining total knee arthroplasty: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc 23, 1653–1659, https://doi.org/10.1007/s00167-014-2877-9 (2015).
Jiang, C. et al. Posterior Cruciate Ligament Retention versus Posterior Stabilization for Total Knee Arthroplasty: A Meta-Analysis. PloS one 11, 1–15, https://doi.org/10.1371/journal.pone.0147865 (2016).
Moskal, J. T. & Capps, S. G. Rotating-platform TKA no different from fixed-bearing TKA regarding survivorship or performance: a meta-analysis. Clin Orthop Relat Res 472, 2185–2193, https://doi.org/10.1007/s11999-014-3539-4 (2014).
Becher, C. et al. Posterior stabilized TKA reduce patellofemoral contact pressure compared with cruciate retaining TKA in vitro. Knee Surg Sports Traumatol Arthrosc 17, 1159–1165, https://doi.org/10.1007/s00167-009-0768-2 (2009).
Clary, C. W., Fitzpatrick, C. K., Maletsky, L. P. & Rullkoetter, P. J. The influence of total knee arthroplasty geometry on mid-flexion stability: an experimental and finite element study. J Biomech 46, 1351–1357, https://doi.org/10.1016/j.jbiomech.2013.01.025 (2013).
Donadio, J., Pelissier, A., Boyer, P. & Massin, P. Control of paradoxical kinematics in posterior cruciate-retaining total knee arthroplasty by increasing posterior femoral offset. Knee Surg Sports Traumatol Arthrosc 23, 1631–1637, https://doi.org/10.1007/s00167-015-3561-4 (2015).
Heyse, T. J. et al. Patellofemoral pressure after TKA in vitro: highly conforming vs. posterior stabilized inlays. Arch Orthop Trauma Surg 130, 191–196, https://doi.org/10.1007/s00402-009-0920-y (2010).
Banks, S. A., Harman, M. K., Bellemans, J. & Hodge, W. A. Making sense of knee arthroplasty kinematics: news you can use. The Journal of bone and joint surgery. American volume 85-A(Suppl 4), 64–72 (2003).
Banks, S. A. & Hodge, W. A. Implant design affects knee arthroplasty kinematics during stair-stepping. Clin Orthop Relat Res, 187–193 (2004).
Banks, S. A. & Hodge, W. A. 2003 Hap Paul Award Paper of the International Society for Technology in Arthroplasty. Design and activity dependence of kinematics in fixed and mobile-bearing knee arthroplasties. J Arthroplasty 19, 809–816 (2004).
Harman, M. K., Bonin, S. J., Leslie, C. J., Banks, S. A. & Hodge, W. A. Total knee arthroplasty designed to accommodate the presence or absence of the posterior cruciate ligament. Advances in orthopedics 2014, 178156, https://doi.org/10.1155/2014/178156 (2014).
Jacobs, W. C., Clement, D. J. & Wymenga, A. B. Retention versus removal of the posterior cruciate ligament in total knee replacement: a systematic literature review within the Cochrane framework. Acta orthopaedica 76, 757–768, https://doi.org/10.1080/17453670510045345 (2005).
Matziolis, G. et al. How much of the PCL is really preserved during the tibial cut? Knee Surg Sports Traumatol Arthrosc 20, 1083–1086, https://doi.org/10.1007/s00167-011-1696-5 (2012).
Morgan, H., Battista, V. & Leopold, S. S. Constraint in primary total knee arthroplasty. The Journal of the American Academy of Orthopaedic Surgeons 13, 515–524 (2005).
Babazadeh, S., Stoney, J. D., Lim, K. & Choong, P. F. The relevance of ligament balancing in total knee arthroplasty: how important is it? A systematic review of the literature. Orthopedic reviews 1, e26, https://doi.org/10.4081/or.2009.e26 (2009).
Heesterbeek, P. J. C., Haffner, N., Wymenga, A. B., Stifter, J. & Ritschl, P. Patient-related factors influence stiffness of the soft tissue complex during intraoperative gap balancing in cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25, 2760–2768, https://doi.org/10.1007/s00167-015-3694-5 (2017).
Abdel, M. P. & Haas, S. B. The unstable knee: wobble and buckle. The bone & joint journal 96-B, 112–114, https://doi.org/10.1302/0301-620X.96B11.34325 (2014).
Chang, M. J., Lim, H., Lee, N. R. & Moon, Y. W. Diagnosis, causes and treatments of instability following total knee arthroplasty. Knee surgery & related research 26, 61–67, https://doi.org/10.5792/ksrr.2014.26.2.61 (2014).
Sharkey, P. F., Hozack, W. J., Rothman, R. H., Shastri, S. & Jacoby, S. M. Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res, 7–13 (2002).
Pinskerova, V. et al. The knee in full flexion: an anatomical study. The Journal of bone and joint surgery. British volume 91, 830–834, https://doi.org/10.1302/0301-620X.91B6.22319 (2009).
Hoshino, Y. & Tashman, S. Internal tibial rotation during in vivo, dynamic activity induces greater sliding of tibio-femoral joint contact on the medial compartment. Knee Surg Sports Traumatol Arthrosc 20, 1268–1275, https://doi.org/10.1007/s00167-011-1731-6 (2012).
Koo, S. & Andriacchi, T. P. The knee joint center of rotation is predominantly on the lateral side during normal walking. J Biomech 41, 1269–1273, https://doi.org/10.1016/j.jbiomech.2008.01.013 (2008).
Kozanek, M. et al. Tibiofemoral kinematics and condylar motion during the stance phase of gait. J Biomech 42, 1877–1884, https://doi.org/10.1016/j.jbiomech.2009.05.003 (2009).
Isberg, J. et al. Will early reconstruction prevent abnormal kinematics after ACL injury? Two-year follow-up using dynamic radiostereometry in 14 patients operated with hamstring autografts. Knee Surg Sports Traumatol Arthrosc 19, 1634–1642, https://doi.org/10.1007/s00167-011-1399-y (2011).
Yamaguchi, S. et al. In vivo kinematics of anterior cruciate ligament deficient knees during pivot and squat activities. Clinical biomechanics 24, 71–76, https://doi.org/10.1016/j.clinbiomech.2008.08.007 (2009).
Dennis, D. A., Mahfouz, M. R., Komistek, R. D. & Hoff, W. In vivo determination of normal and anterior cruciate ligament-deficient knee kinematics. J Biomech 38, 241–253, https://doi.org/10.1016/j.jbiomech.2004.02.042 (2005).
Barink, M. et al. A mechanical comparison of high-flexion and conventional total knee arthroplasty. Proceedings of the Institution of Mechanical Engineers. Part H, Journal of engineering in medicine 222, 297–307, https://doi.org/10.1243/09544119JEIM353 (2008).
Engel, K., Fischer, K. M., Brüggermann, G. P. & Liebau, C. Total knee arthroplasty with a lateral centre of rotation design retained native knee joint kinematics: a cadaveric study under simulated mscle loads. J Orthopedics Rheumatol. 3, 6 (2016).
Mikashima, Y. et al. In vivo deep-flexion kinematics in patients with posterior-cruciate retaining and anterior-cruciate substituting total knee arthroplasty. Clinical biomechanics 25, 83–87, https://doi.org/10.1016/j.clinbiomech.2009.09.009 (2010).
Watanabe, T., Ishizuki, M., Muneta, T. & Banks, S. A. Knee kinematics in anterior cruciate ligament-substituting arthroplasty with or without the posterior cruciate ligament. J Arthroplasty 28, 548–552, https://doi.org/10.1016/j.arth.2012.06.030 (2013).
Ginsel, B. L., Banks, S., Verdonschot, N. & Hodge, W. A. Improving maximum flexion with a posterior cruciate retaining total knee arthroplasty: a fluoroscopic study. Acta orthopaedica Belgica 75, 801–807 (2009).
Garling, E. H., Kaptein, B. L., Geleijns, K., Nelissen, R. G. & Valstar, E. R. Marker Configuration Model-Based Roentgen Fluoroscopic Analysis. J Biomech 38, 893–901 (2005).
Ewald, F. C. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res, 9–12 (1989).
Behrend, H., Giesinger, K., Giesinger, J. M. & Kuster, M. S. The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty 27, 430–436 e431, https://doi.org/10.1016/j.arth.2011.06.035 (2012).
Na, S. E., Ha, C. W. & Lee, C. H. A new high-flexion knee scoring system to eliminate the ceiling effect. Clin Orthop Relat Res 470, 584–593, https://doi.org/10.1007/s11999-011-2203-5 (2012).
Moewis, P. et al. The quality of bone surfaces may govern the use of model based fluoroscopy in the determination of joint laxity. Medical engineering & physics 34, 1427–1432, https://doi.org/10.1016/j.medengphy.2012.01.007 (2012).
Kaptein, B. L., Valstar, E. R., Stoel, B. C., Rozing, P. M. & Reiber, J. H. A new model-based RSA method validated using CAD models and models from reversed engineering. J Biomech 36, 873–882 (2003).
Pfitzner, T. et al. Modifications of femoral component design in multi-radius total knee arthroplasty lead to higher lateral posterior femoro-tibial translation. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-017-4622-7 (2017).
Fuss, F. K. An analysis of the popliteus muscle in man, dog, and pig with a reconsideration of the general problems of muscle function. The Anatomical record 225, 251–256, https://doi.org/10.1002/ar.1092250311 (1989).
Petersen, W. et al. Anterior knee pain after total knee arthroplasty: a narrative review. Int Orthop 38, 319–328, https://doi.org/10.1007/s00264-013-2081-4 (2014).
Stiehl, J. B., Dennis, D. A., Komistek, R. D. & Keblish, P. A. In vivo kinematic comparison of posterior cruciate ligament retention or sacrifice with a mobile bearing total knee arthroplasty. The American journal of knee surgery 13, 13–18 (2000).
Hommel, H., Abdel, M. P. & Perka, C. Kinematic femoral alignment with gap balancing and patient-specific instrumentation in total knee arthroplasty: a randomized clinical trial. European journal of orthopaedic surgery & traumatology: orthopedie traumatologie 27, 683–688, https://doi.org/10.1007/s00590-016-1865-9 (2017).
Hommel, H., Perka, C. & Pfitzner, T. Preliminary results of a new surgical technique in total knee arthroplasty (TKA) using the native ligament tension for femoral implant positioning in varus osteoarthritis. Arch Orthop Trauma Surg 136, 991–997, https://doi.org/10.1007/s00402-016-2480-2 (2016).
Acknowledgements
This work was supported by Implantcast GmbH, the European Regional Development Fund (EFRE, 16409608, OrthoLoadLab), the Federal Ministry of Education and Research (BMBF, OVERLOAD-PrevOP, 01EC1408A), the German Research Foundation (DFG, TR 1657/1-1) and the OrthoLoad Club. We also acknowledge support from the German Research Foundation (DFG) and the Open Access Publication Funds of Charité – Universitätsmedizin Berlin.
Author information
Authors and Affiliations
Contributions
P.M.: conceptualization, data collection, formal analysis, funding acquisition, investigation, methodology, project administration, supervision, writing – original draft, review and editing. H.H.: conceptualization, data collection, formal analysis, funding acquisition, supervision, writing – review and editing. A.T.: formal analysis, methodology, writing – review and editing. L.K.: data curation, writing – review and editing. P.v.R.: writing – review and editing. G.N.D.: conceptualization, formal analysis, funding acquisition, supervision, writing – review and editing.
Corresponding author
Ethics declarations
Competing Interests
P. M. is an unpaid consultant for Implantcast GmbH.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Moewis, P., Hommel, H., Trepczynski, A. et al. Weight Bearing Activities change the Pivot Position after Total Knee Arthroplasty. Sci Rep 9, 9148 (2019). https://doi.org/10.1038/s41598-019-45694-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-45694-y
This article is cited by
-
Comparison of joint awareness after total knee arthroplasty, medial unicompartmental knee arthroplasty, and high tibial osteotomy: a retrospective study
BMC Musculoskeletal Disorders (2023)
-
Changes in femoral rollback and rotation with increasing coupling in knee arthroplasty—a biomechanical in-vitro study
BMC Musculoskeletal Disorders (2023)
-
Patient-specific resurfacing implant knee surgery in subjects with early osteoarthritis results in medial pivot and lateral femoral rollback during flexion: a retrospective pilot study
Knee Surgery, Sports Traumatology, Arthroscopy (2023)
-
Kinematics and kinetics comparison of ultra-congruent versus medial-pivot designs for total knee arthroplasty by multibody analysis
Scientific Reports (2022)
-
A New La(III)-MOF for Efficient Dye Photodegradation and Protective Effect on Exercise Pain After Total Knee Arthroplasty by Reducing Nicotinic Acetylcholine Receptors Expression
Journal of Inorganic and Organometallic Polymers and Materials (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.