Abstract
Although patients with advanced cancer often experience multiple symptoms simultaneously, clinicians usually focus on symptoms that are volunteered by patients during regular history-taking. We aimed to evaluate the feasibility of a Bayesian network (BN) model to predict the presence of simultaneous symptoms, based on the presence of other symptoms. Our goal is to help clinicians prioritize which symptoms to assess. Patient-reported severity of 11 symptoms (scale 0–10) was measured using an adapted Edmonton Symptom Assessment Scale (ESAS) in a national cross-sectional survey among advanced cancer patients. Scores were dichotomized (< 4 and ≥ 4). Using fourfold cross validation, the prediction error of 9 BN algorithms was estimated (Akaike information criterion (AIC). The model with the highest AIC was evaluated. Model predictive performance was assessed per symptom; an area under curve (AUC) of ≥ 0.65 was considered satisfactory. Model calibration compared predicted and observed probabilities; > 10% difference was considered inaccurate. Symptom scores of 532 patients were collected. A symptom score ≥ 4 was most prevalent for fatigue (64.7%). AUCs varied between 0.60 and 0.78, with satisfactory AUCs for 8/11 symptoms. Calibration was accurate for 101/110 predicted conditional probabilities. Whether a patient experienced fatigue was directly associated with experiencing 7 other symptoms. For example, in the absence or presence of fatigue, the model predicted a 8.6% and 33.1% probability of experiencing anxiety, respectively. It is feasible to use BN development for prioritizing symptom assessment. Fatigue seems most eligble to serve as a starting symptom for predicting the probability of experiencing simultaneous symptoms.
Similar content being viewed by others
Introduction
Most patients with advanced cancer experience multiple symptoms simultaneously1. However, in daily practice the focus of symptom management is often on one or few main symptoms, that is, the symptoms that are spontaneously volunteered by the patient during regular history-taking2,3. This causes other simultaneous symptoms to remain unrelieved, which negatively impacts a patient’s functioning and quality of life4. Several solutions have been suggested for assessing symptom burden more comprehensively. Most notably, symptom assessment scales have shown to improve the assessment of total symptom burden5,6 but it is difficult to widely implement such scales in both specialist and non-specialist palliative care settings7. In addition, efforts were made to identify which symptoms frequently occur simultaneously in patients with advanced cancer, so called symptom clusters8. Symptom cluster research has advanced the way simultaneous symptoms are approached theoretically, for example by fostering research about common etiologies of clusters9. However, symptom clusters are inconsistent across studies8 and, perhaps as a result, cluster research has not yet convincingly impacted symptom assessment in daily practice9.
It could help clinicians prioritize which symptoms to assess if they are provided with the probability that their patient experiences specific simultaneous symptoms, based on volunteered main symptoms. For this purpose, a Bayesian network (BN) may be developed. A BN is a probabilistic graphical model used to visualize associations between large numbers of variables. In addition, in case of dichotomized variables, a BN can provide the conditional probability that a variable is present or absent, based on the presence or absence of other variables in the network. BNs have been widely used in medicine to predict outcomes such as diagnosis, functional outcome, quality of life and survival, based on patient and disease characteristics10,11,12,13,14,15. The advantage compared to other probabilistic modelling methods is that they do not need dedicated input and output variables and that they can be constructed in case of insufficient available evidence on associations between variables15. BNs are also easy to understand: The graphical structure makes associations between variables directly interpretable and the provided conditional probabilities align with clinical reasoning15,16. The aim of this study is to evaluate the statistical feasibility of a BN model for predicting the probability of a simultaneously occurring symptom, based on a patient’s other symptoms.
Methods
Context
This study is part of the Multidimensional Strategy for Palliative Care (MuSt-PC) project (2017–2021; NCT03665168). The project aims to improve multidimensional symptom management in palliative care by studying the prevalence of multidimensional symptoms in a national cross-sectional study17, evaluating the acceptability of a clinical decision support system (CDSS) according to various stakeholders18, assessing barriers and facilitators for multidimensional symptom management19, developing symptom management recommendations for simultaneously occurring symptoms and constructing a CDSS to support generalist clinicians.
Participants and study design
Data on symptom presence and severity were collected during four weeks in September and November 2018 in a nation-wide cross-sectional survey among patients with palliative care needs, regardless of their underlying illness. Physicians and nurses working in different care settings were asked to participate in data collection (general practices, nursing homes, hospices and outpatient departments and clinical wards of academic and community hospitals). Clinicians were asked to identify patients with palliative care needs, using a negative answer to the one-year surprise question as the sole inclusion criterion (answer “No” to the question “Would I be surprised if this patient died within the next twelve months?”)20. Patients unable or unwilling to self-assess their symptoms were excluded. In this study we performed a secondary analysis of collected data of patients with advanced cancer.
Measurements
In case of eligibility, the attending clinician asked their patient to complete a questionnaire to report their symptoms at the time of consultation. The questionnaire included the Utrecht Symptom Diary (USD), a validated Dutch translation and adaptation of the Edmonton Symptom Assessment System (ESAS)21. The USD measures presence and severity of 11 symptoms on a 0-to-10-numeric rating scale (NRS) (0 = ‘no complaint’; 10 = ‘worst complaint possible’): Pain, sleeping problems, dry mouth, dysphagia, lack of appetite, constipation, nausea, shortness of breath, fatigue, anxiety and depressed mood. Additionally, the questionnaire contained questions on demographic, treatment and disease characteristics, including a Patient Reported Performance Status (PRFS; scale 1–4). A PRFS 1 indicated ‘not my normal self, but able to be up and about with fairly normal activities’ and a PRFS 4 indicated ‘pretty much bedridden, rarely out of bed’ (see Table 1)22. Questionnaires were available via a secured website or on paper.
Statistical analysis
Frequencies of demographic, disease and treatment characteristic were analyzed using descriptive statistics. In case of missing values, symptom scores (NRS 0–10) were estimated using k-nearest neighbor imputation (k = 5)23. Scores were dichotomized into clinically relevant (≥ 4) and not clinically relevant (< 4), since an ESAS score of ≥ 4 is generally considered as the cut-off point for symptoms that require additional assessment21,24. For each of the USD-listed symptoms, the frequency of clinically relevant symptom scores was calculated.
Bayesian network development
A Bayesian network (BN) was developed to assess whether the presence or absence of a clinically relevant USD-listed symptom could be predicted based on the presence or absence of the other 10 USD-listed symptoms. The dichotomized symptom scores of the 11 USD-listed symptoms served as the network’s variables.
BN development consists of two stages: Structure learning and parameter learning. During structure learning, a graphical structure is constructed: The directed acyclic graph (DAG) (Fig. 1). In the DAG, edges point from parent nodes towards child nodes, indicating that the model found a direct association, or conditional dependency, between those variables. The DAG presented in this study is based on the total dataset as a way of presenting the mean DAG for our data. All other analyses were conducted per fold within a fourfold cross validation set-up.
Structure learning was done using 9 automated BN algorithms (constraint-based, score-based and hybrid learning). For each of the four resulting DAGs, the Akaike information criterion (AIC) score was calculated. The AIC indicates how accurate a model will be able to predict future data, but only in comparison to other algorithms. The highest AIC score denoted the lowest prediction error estimate25.
The algorithm with the highest mean AIC across the four folds was then used for parameter learning. During parameter learning, a conditional probability table (CPT) is calculated for each dichotomized symptom in the model. In theory, conditional probabilities of the presence or absence of each symptom can be calculated, based on the presence or absence of all other variables that the symptom is directly or indirectly connected with in the DAG. In this study, we labelled symptoms that the model identified as parent nodes as ‘main symptoms’ and labelled child nodes as ‘simultaneous symptoms’. We only present the predicted probabilities of the presence of child nodes based on the presence or absence of parent nodes. That way, we limited the number of analyses to illustrate the use of a BN model in a simplified manner.
Predictive performance and calibration of the Bayesian network
For the algorithm with the highest AIC score, a mean AUC score over the four folds was calculated per simultaneous symptom and accepted as the model’s overall AUC-ROC. The AUC-ROC indicates how well the BN model can determine the outcome for an individual patient (simultaneous symptom present or absent), based on the presence or absence of the other 10 USD-listed symptoms. In general, an AUC-ROC of 0.5 implies a lack of predictive performance and an AUC-ROC of > 0.9 implies outstanding predictive performance26. An AUC-ROC of ≥ 0.65 was considered satisfactory. We also aimed to determine how accurate the BN was in predicting the conditional probabilites of a patient experiencing each simultaneous symptom, based on the presence or absence of the other 10 USD-listed symptoms. For this purpose, a calibration plot was constructed for each symptom using the model's predictions for all four test sets of the cross validation. Patients in the dataset were grouped into deciles, based on their similar predicted conditional probabilities of experiencing the symptom by the BN model. The mean conditional probability predicted by the model was plotted against the mean observed frequency in the dataset per decile. A > 10% difference between predicted and observed conditional probabilities was considered an inaccurate calibration. R 4.1.0 and bn learn R package 4.7 were used to conduct analyses.
Development of a symptom prediction system
We aimed to indicate the potential of using a BN model for the development of a symptom prediction system. Based on the BN, we propose a preliminary symptom prediction flow-chart that uses main symptoms that can directly predict the presence or absence of simultaneous symptoms as system input. In addition, the system’s input should preferably consist of those symptoms that are most frequently volunteered by patients with advanced cancer after open-ended questioning during regular history-taking. The only available study on this subject by Homsi et al. identified that pain and fatigue are the most frequently volunteered symptoms, by 50.5% and 25.5% of patients with advanced cancer, respectively. Pain and fatigue were followed by anorexia (13.5%) and constipation (5.5%)5.
Ethical considerations
The Medical Ethics Review Board of the University Medical Center Groningen approved the research protocol (NCT number 03665168) and waived informed consent (12 June 2018). Data in this study were anonymously obtained and recorded. The opt-in method was used with an anonymous consent statement for study participation and publication of data, to ensure no personal information was reported. The study was conducted in full compliance with the codes of ethical conduct from the 1964 Declaration of Helsinki.
Results
Baseline characteristics
The survey was returned by 532 patients with advanced cancer. Twenty-six questionnaires had 1 to 3 missing scores, resulting in 36 missing symptom scores and 5816 complete symptom scores. An overview of baseline characteristics is shown in Table 1. The most frequently reported primary cancer site was lung (19.0%), colon (15.2%), and breast (13.0%), and 70% had metastatic cancer. In the 3 months prior to data collection, 49.4% received systemic therapy and 24.8% radiotherapy. A patient-reported functional status (PRFS)22 of 1 was reported by 33.5%; a PRFS of 3 or 4 was reported by 35.8%. At the time of the survey, 51% of patients resided at home.
Symptom burden
Fatigue was experienced by 64.7% and 51.5% experienced lack of appetite as a clinically relevant symptom (NRS ≥ 4; see Table 1). Clinically relevant constipation was reported by 49.8% of patients, dry mouth by 45.3%, sleeping problems by 39.3% and pain by 36.6%. Clinically relevant depressed mood was reported by 30.3% of patients, anxiety by 24.6%, dysphagia by 20.9%, shortness of breath by 18.6% and nausea by 12.0%.
Bayesian network model
Of the 9 tested automated BN algorithms, Tabu search algorithm27 had the highest AIC score. An overview of AIC scores for all tested algorithms is provided in Supplementary Fig. 1. When trained on the full data set, the Tabu search algorithm constructed the BN structure shown in Fig. 1. Each node represents 1 of the 11 USD-listed symptoms. In the identified BN structure, fatigue was most frequently directly associated with other USD-listed symptoms. Experiencing shortness of breath, dry mouth, anxiety, nausea, pain, sleeping problems and lack of appetite was conditionally dependent on whether a patient experienced fatigue.
Directed acyclic graph of the Baysian network; as constructed during structure learning by the algorithm with the lowest prediction error estimate (Tabu search algorithm). Edges (arrows) between nodes indicate that the model found a direct association between those variables. An edge points from a parent node towards a child node, indicating that the BN structure found that the child node is conditionally dependent on the parent node.
The model predicted a conditional probability of > 75% of experiencing a specific simultaneous symptom based on the absence or presence of other USD-listed symptoms for the following combinations (Table 2): Patients who experienced fatigue and dysphagia had a 80.0% probability of experiencing a lack of appetite and also experiencing dysphagia and no fatigue also gave a probability of 81.0% of a lack of appetite. Experiencing dysphagia and a lack of appetite gave a 78.7% probability of experiencing constipation. Experiencing anxiety and a dry mouth gave a probability of 79.8% of a depressed mood, and also experiencing anxiety and not having a dry mouth gave a probability of 76.4% of a depressed mood.
Predictive performance and calibration of the Bayesian network
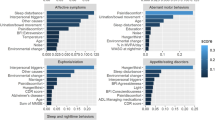
The mean AUC-ROC per predicted symptom (see Supplementary Table 1 for AUC-ROCs per cross-validation fold) varied between 0.60 for pain and sleeping problems and 0.78 for depressed mood (Table 3). AUCs were satisfactory (≥ 0.65) for 8 out of 11 symptoms. The calibration plots show the mean predicted probabilites plotted against the mean observed frequentcies per decile (Fig. 2). The model accurately predicted 101 of a total of 110 conditional probabilities. For 7/11 symptoms, all predicted conditional probabilities were accurate at calibration. A difference of > 10% between predicted probabilities and observed frequencies was observed for sleeping problems (2 deciles), dry mouth (3 deciles), constipation (2 deciles) fatigue (1 decile) and anxiety (1 decile).
Calibration plots per predicted simultaneous symptom. The mean observed frequencies are plotted against the mean predicted probabilites per decile. Each decile represents a group of patients with a similar conditional probabilty predicted by the model. The black line corresponds to a model with ideal calibration, that is, a model that perfectly predicts the conditional probabilities.
Symptom prediction flow-chart
We propose a flow-chart (Fig. 3) based on the BN structure (Fig. 1) and conditional probabilities predicted by the BN (Table 2) to illustrate the potential of BN development for a clinical symptom prediction system. Fatigue serves as the system’s starting point because it was the symptoms that was most frequently directly associated with other symptoms and moreover, is the second most frequently volunteered symptom by patients with advanced cancer in available research5.
Preliminary symptom prediction system that uses the presence of fatigue as system input. Fatigue is the second most frequently volunteered symptom by patients with advanced cancer5, and in our Bayesian network this symptom was identified as the symptom that most frequently was directly associated with other USD-listed symptoms (7 other symptoms). When using fatigue as system input, the conditional probabilities (%) of the patient also experiencing pain, dry mouth, sleeping problems, lack of appetite, nausea, shortness of breath and anxiety can be presented. This may help clinicians to prioritize which symptoms to assess.
Discussion
Main findings
We evaluated the statistical feasibility of developing a Bayesian network (BN) for predicting the presence of simultaneous symptoms, based on the presence or absence of a patient’s other symptoms. By presenting the probability of experiencing specific simultaneous symptoms, we aim to help clinicians prioritize which symptoms to assess during consultations. The developed BN model had satisfactory performance in predicting the presence or absence of 8 out of 11 USD-listed symptoms, indicated by an AUC-ROC of ≥ 0.65. Model calibration showed that 101 out of a total of 110 conditional probabilities predicted by the BN model were accurate. Fatigue was most frequently directly associated with other USD-listed symptoms and seems most eligble to serve as the starting symptom in a future symptom prediction system.
Identified direct associations between symptoms
All direct associations between symptoms, represented by the edges (arrows) in the BN structure, were also identified in at least one previous symptom cluster study among patients with advanced cancer. Previously identified were associations between fatigue and pain28,29, sleeping problems and pain30, fatigue and sleeping problems30,31, anxiety and sleeping problems32, dysphagia and dry mouth33, fatigue and anxiety34, fatigue and a lack of appetite32,35,36, dysphagia and lack of appetite33, dysphagia and constipation33, a lack of appetite and constipation33, fatigue and nausea35 dry mouth and shortness of breath37, fatigue and shortness of breath31,38,39, fatigue and anxiety36,40,sleeping problems and anxiety32,37, sleeping problems and dry mouth41, fatigue and dry mouth37, depressed mood and nausea42, dry mouth and depressed mood30, nausea and dysphagia33 and anxiety and depressed mood32,35,36,37,39,43.
In line with previous studies, fatigue was most frequently directly associated with other ESAS symptoms, seven in total. Fatigue is the most prevalent symptom in patients with advanced cancer, both in our study and in others44. Also similar to our findings, others have found that contributory factors of cancer-related fatigue include pain, sleep disturbances, emotional disturbances, depression, anxiety and weight loss45. Vice versa, fatigue may be a contributing factor in how severe patients experience the associated seven other ESAS symptoms. Fatigue has been found to be one of the most distressing symptoms in patients with cancer and often is accompanied by mental fatigue, including emotional liability45,46. These psychological factors may affect how well patients are able to cope with their other symptoms. Our ultimate aim is to use the results of a BN model for developing a clinical symptom prediction system that present clinicians with the probability that their patient experiences specific simultaneous symptoms, based on the main symptom(s) a patient volunteers during regular history taking. For this purpose, the BN model should be validated on an external dataset. External validation is a crucial step in verifying a model’s generalizibility15. In the external dataset, data should preferably be available on the actual volunteered main symptom(s) by patients during regular history taking. This information was absent in the current study, which likely influenced the identified assocations between symptoms. In addition to external validation, future research should aim to gain more certainty about the directions of the edges in the BN structure. This is important because the direction of the edges in the identified BN structure remains uncertain, due to the fact that automated learning was used to develop the BN. This was the only option because there was no consistent available evidence about associations between symptoms to facilitate hybrid causal learning, which means a BN model is developed based on a combination of initial expert knowledge and automated learning47. Automated learning may result in edges that point in a certain direction for other reasons than that it best fits the data, for example, to simplify the constructed network. When developing a final BN model to support a symptom prediction system, the probability of the edges’ directions between symptoms could be further assessed by the methods used by McNally et al., who used BN development for gaining insight in associations between the symptoms of Post Traumatic Stress Disorder48. They determined the direction of each edge between symptoms in 10.000 bootstrapped networks. If a direction of an edge was present in at least 51% of networks, this was considered the edge’s direction.
Predictive preformance and model calibration
The developed BN model had an AUC-ROC of ≥ 0.65 for 8 out of 11 USD-listed symptoms. For the purpose of advising clinicians which symptoms to assess, we considered an AUC-ROC of ≥ 0.65 a satisfactory predictive performance because it is considerably better than chance (AUC-ROC = 0.5)26. Moreover, the consequences of symptom prediction being wrong are small, in comparison to, for example, diagnostic tests in which one generally strives for AUC scores > 0.95 because the consequences of being wrong are severe. For the same reason, we considered a difference of ≤ 10% between predicted an observed probability in model calibration acceptable.
Potential of using Bayesian networks for symptom prediction
Using BNs to develop a symptom prediction system is a promising approach because additional variables can easily be added as the model’s variables in future research15, for example the patient’s age, gender, primary cancer site, functional status and disease-modifing treatment during the previous 3 months. It is likely that conditional dependency between these variables and symptoms will be identified, as others have previously identified variables such as cancer site, age and gender as predictors for differences in symptom cluster composition8. Inclusion of these variables may enable symptom prediction to be further individualized. In addition, problems in other than the physical and psychological dimension of palliative care could be used as variables in the BN. The Utrecht Symptom Diary (USD), a Dutch adaptation of the ESAS, was used for data analysis, which measures 11 symptoms, whereas advanced cancer patients usually experience a wider array of physical symptoms and psychological, social and existential problems49. Multidimensional symptoms and problems could serve as variables for future BN development to gain further insight into the complex associations between physical symptoms and non-physical problems.
The purpose of the proposed symptom prediction system is to help clinician prioritize which symptoms to assess. Since the need for prioritization will largely depend on the amount of time a clinician has available for symptom assessment, we propose that in the future system a clinician can indicate whether they have sufficient or limited time. In case of limited time, the clinician will likely only want to asses those simultaneous symptoms that are highly likely present. This could be achieved by establishing two different probability thresholds within the system, above which clinicians are advised to assess a specific simultaneous symptom. Probability thresholds can be extracted from the model’s AUC-ROC, with a specific sensitivity and specificity per threshold. If time is limited, we suggest to adhere to a threshold with relatively high specificity (low probability of false positives) and in case of sufficient time, to adhere to a threshold with high sensitivity (low probability of false negatives). When evaluating the effect of using the proposed symptom prediction system in the future, it should be noted that the ultimate problem of missing out on important symptoms is the fact that the single missed symptoms are not targeted in regular history taking and that the complex interaction of multiple symptoms is not taken into account when choosing a treatment strategy to try to relieve the patient’s total symptom burden. We therefore suggest the following positive clinical outcome of using a symptom prediction system: a significant clinically relevant relief of overall symptom burden in patients of clinicians that used the symptom prediction system compared to patients of clinicians who identified symptoms through regular history taking.
Limitations and strenghts
In this study, a symptom assessment scale was used for data collection. To illustrate the potential of BN development we labelled symptoms as ‘main symptoms’ and ‘simultaneous symptoms’. However, we want to underline that no data were available on the actual volunteered main symptom(s) of patients. This has likely affected the identified associations between symptoms. Therefore, the current results cannot be used to present clinicians with the probability that a patient experiences specific simultaneous symptoms, based on the main volunteered symptom(s) during regular history taking.
USD scores were dichotomized into clinically relevant (≥ 4) and not relevant (< 4) since an ESAS score of ≥ 4 is generally considered as the cut off point for symptoms that require additional assessment21,24. Moreover, BN development is easier to illustrate using dichotomized variables, as dichotomization minimizes the number of combinations and opportunities. This dichotomization determined whether a symptom was considered present (score ≥ 4) or absent (score < 4). In future research, instead of dichotomizing the symptoms, the ESAS scores could also be categorized into severity categories (mild, moderate, severe)50. This way, it can be evaluated to what extent BN structure and conditional probabilites differ when ESAS scores are dichotomized or categorized. It may be argued that imputation of missing symptom scores influenced the BN structure and conditional probabilities. However, we consider this effect neglectable because only 26 symptom scores of overall 5852 symptom scores were missing in the data set. A strength of this study is that, to our knowledge, we are first to present the idea of a symptom prediction system that quantifies the probability of a patient experiencing a simultaneous symptom based on their volunteered symptoms, which we believe could be a valuable addition to the solutions already offered for improving symptom assessment in patients with advanced cancer.
Conclusion
It is feasible to use BN development to support clinicians in prioritizing symptom assessment. The developed model was able to predict the probability that patients experience specific simultaneous symptoms based on the presence or absence of their other symptoms, given the model’s satisfactory predictive performance for 8 out of 11 symptoms. Moreover, the conditional probabilities that the BN model predicted were generally accurate. BN development could support the implementation of a symptom prediction system to help clinicians prioritize the asssesment of simultaneous symptoms in patients with advanced cancer. Fatigue seems most eligible to serves as a starting symptom of such a system. To develop a symptom prediction system, future research is needed to validate the identified model using an external dataset.
Data availability
The dataset and code used in this study is available from the corresponding author on reasonable request.
References
Gilbertson-White, S., Aouizerat, B. E., Jahan, T. & Miaskowski, C. A review of the literature on multiple symptoms, their predictors, and associated outcomes in patients with advanced cancer. Palliat. Support Care 9, 81–102 (2011).
Okuyama, T. et al. Oncologists’ recognition of supportive care needs and symptoms of their patients in a breast cancer outpatient consultation. Jpn. J. Clin. Oncol. 41, 1251–1258 (2011).
Laugsand, E. A. et al. Health care providers underestimate symptom intensities of cancer patients: A multicenter European study. Health Qual. Life Outcomes 8, 104 (2010).
Miaskowski, C., Dodd, M. & Lee, K. Symptom clusters: the new frontier in symptom management research. J. Natl. Cancer Inst. Monogr. 32, 17–21 (2004).
Homsi, J. et al. Symptom evaluation in palliative medicine: Patient report vs systematic assessment. Support Care Cancer 14, 444–453 (2006).
Hui, D. & Bruera, E. The Edmonton symptom assessment system 25 years later: Past, present, and future developments. J. Pain Symptom Manage. 53, 630–643 (2017).
Schick-Makaroff, K., Sawatzky, R., QR Team. Divergent perspectives on the use of the edmonton symptom assessment system (Revised) in palliative care. J. Hospice Palliat. Nurs. 22(1), 75–81 (2020).
Dong, S. T., Butow, P. N., Costa, D. S., Lovell, M. R. & Agar, M. Symptom clusters in patients with advanced cancer: A systematic review of observational studies. J. Pain Symptom Manage. 48, 411–450 (2014).
Miaskowski, C. et al. Advancing symptom science through symptom cluster research: Expert panel proceedings and recommendations. J. Natl. Cancer Inst. 109, 4 (2017).
Sieswerda, M. S. et al. Predicting lung cancer survival using probabilistic reclassification of TNM editions with a Bayesian network. JCO Clin. Cancer Inform. 4, 436–443 (2020).
Karaboga, H. A., Gunel, A., Korkut, S. V., Demir, I. & Celik, R. Bayesian network as a decision tool for predicting ALS disease. Brain Sci. 11, 2 (2021).
Kaewprag, P. et al. Predictive models for pressure ulcers from intensive care unit electronic health records using Bayesian networks. BMC Med. Inform. Decis. Making 2, 65 (2017).
Crump, C. et al. Using Bayesian networks and rule-based trending to predict patient status in the intensive care unit. AMIA Annu. Symp. Proc. 9, 124–128 (2009).
Xu, S. et al. Cognition, quality-of-life, and symptom clusters in breast cancer: Using Bayesian networks to elucidate complex relationships. Psychooncology 27, 802–809 (2018).
Kyrimi, E. et al. Bayesian networks in healthcare: What is preventing their adoption?. Artif. Intell. Med. 116, 102079 (2021).
Park, E., Chang, H. J. & Nam, H. S. A Bayesian network model for predicting post-stroke outcomes with available risk factors. Front. Neurol. 9, 699 (2018).
De Heij, A. H. et al. Abstracts from the 11th EAPC World Research Congress Online, Abstract number FC74 Identification of symptom clusters in a palliative care trajectory; the multidimensional strategies for palliative care study (MuSt-PC). Palliat. Med. 34, 38 (2020).
van der Stap, L., De Heij, A. H., van der Heide, A,, Reyners, A. K. L., van der Linden, Y. M. A Clinical decision support system to optimize symptom management in palliative medicine: Focus group study. BMJ Support Palliat Care 002940 (2021).
van der Stap, L., de Heij, A. H., van der Heide, A., Reyners, A. K. L. & van der Linden, Y. M. Barriers and facilitators to multidimensional symptom management in palliative care: A focus group study among patient representatives and clinicians. Palliat. Support Care 30, 1–12. https://doi.org/10.1017/S147895152200133X (2022).
Downar, J., Goldman, R., Pinto, R., Englesakis, M. & Adhikari, N. K. The “surprise question” for predicting death in seriously ill patients: A systematic review and meta-analysis. CMAJ 189, E484–E493 (2017).
van der Baan, F. H. et al. Validation of the Dutch version of the Edmonton symptom assessment system. Cancer Med. 9, 6111–21 (2020).
Popovic, G. et al. Patient-reported functional status in outpatients with advanced cancer: Correlation with physician-reported scores and survival. J. Pain Symptom Manag. 55, 1500–1508 (2018).
Massidda, D. (2019). Missing data replacement by k-Nearest neighbor. https://rdrr.io/github/DavideMassidda/testing/man/knn.impute.html. Accessed 28 June 2019.
Oldenmenger, W. H., de Raaf, P. J., de Klerk, C. & van der Rijt, C. C. Cut points on 0–10 numeric rating scales for symptoms included in the Edmonton symptom assessment scale in cancer patients: A systematic review. J. Pain Symptom Manag. 45, 1083–1093 (2013).
Shmueli, G. To explain or to predict?. Stat. Sci. 25, 289–310 (2010).
Hosmer, D. W. Assessing the fit of the model. In Applied Logistic Regression 2nd edn 178 (John Wiley & Sons, 2000).
Russel, S. & Norvig, P. Beyond classical search. In Artifical Intelligence: A Modern Approach 3rd edn 155 (Pearson Education Inc, 2010).
Yennurajalingam, S. et al. Consistency of symptom clusters among advanced cancer patients seen at an outpatient supportive care clinic in a tertiary cancer center. Palliat. Support Care 11, 473–480 (2013).
Chow, E., Fan, G., Hadi, S. & Filipczak, L. Symptom clusters in cancer patients with bone metastases. Support Care Cancer 15, 1035–1043 (2007).
Chaiviboontham, S., Viwatwongkasem, C., Hanucharurnkul, S. & McCorkle, R. Symptom clusters in Thais with advanced cancer. Pacific Rim. Int. J. Nurs. Res. 15, 265–277 (2011).
Francoeur, R. B. The relationship of cancer symptom clusters to depressive affect in the initial phase of palliative radiation. J. Pain Symptom Manag. 29, 130–155 (2005).
Jiménez, A. et al. Symptom clusters in advanced cancer. J. Pain Symptom Manag. 42, 24–31 (2011).
Tsai, J. S., Wu, C. H., Chiu, T. Y. & Chen, C. Y. Significance of symptom clustering in palliative care of advanced cancer patients. J. Pain Symptom Manag. 39, 655–662 (2010).
Chan, C. W., Richardson, A. & Richardson, J. A study to assess the existence of the symptom cluster of breathlessness, fatigue and anxiety in patients with advanced lung cancer. Eur. J. Oncol. Nurs. 9, 325–333 (2005).
Cheung, W. Y., Le, L. W. & Zimmermann, C. Symptom clusters in patients with advanced cancers. Support. Care Cancer 17, 1223–1230 (2009).
Husain, A., Myers, J., Selby, D., Thomson, B. & Chow, E. Subgroups of advanced cancer patients clustered by their symptom profiles: Quality-of-life outcomes. J. Palliat. Med. 14, 1246–1253 (2011).
Walsh, D. & Rybicki, L. Symptom clustering in advanced cancer. Support Care Cancer 14, 831–836 (2006).
Cheung, W. Y. et al. The association of physical and psychological symptom burden with time to death among palliative cancer outpatients. J. Pain Symptom Manag. 37, 297–304 (2009).
Fan, G., Hadi, S. & Chow, E. Symptom clusters in patients with advanced-stage cancer referred for palliative radiation therapy in an outpatient setting. Support Cancer Ther. 4, 157–162 (2007).
Bender, C. M., Ergÿn, F. S., Rosenzweig, M. Q., Cohen, S. M. & Sereika, S. M. Symptom clusters in breast cancer across 3 phases of the disease. Cancer Nurs. 28, 219–225 (2005).
Wang, X. S. et al. Longitudinal study of the relationship between chemoradiation therapy for non-small-cell lung cancer and patient symptoms. J. Clin. Oncol. 24, 4485–4491 (2006).
Chen, E. et al. Symptom clusters in patients with advanced cancer: Sub-analysis of patients reporting exclusively non-zero ESAS scores. Palliat. Med 26, 826–833 (2012).
Kirkova, J., Aktas, A., Walsh, D., Rybicki, L. & Davis, M. P. Consistency of symptom clusters in advanced cancer. Am. J. Hosp. Palliat. Care 27, 342–346 (2010).
Barnes, E. A. & Bruera, E. Fatigue in patients with advanced cancer: A review. Int. J. Gynecol. Cancer 12, 424–428 (2002).
Hawthorn, M. Fatigue in patients with advanced cancer. Int. J. Palliat. Nurs 16, 536–541 (2010).
Bower, J. E. Cancer-related fatigue—Mechanisms, risk factors, and treatments. Nat. Rev. Clin. Oncol. 11, 597–609 (2014).
Julia Flores, M., Nicholson, A. E., Brunskill, A., Korb, K. B. & Mascaro, S. Incorporating expert knowledge when learning Bayesian network structure: A medical case study. Artif. Intell. Med. 53, 181–204 (2011).
McNally, R. J., Heeren, A. & Robinaugh, D. J. A Bayesian network analysis of posttraumatic stress disorder symptoms in adults reporting childhood sexual abuse. Eur. J. Psychotraumatol. 8, 1341276 (2017).
Krikorian, A., Limonero, J. T., Román, J. P., Vargas, J. J. & Palacio, C. Predictors of suffering in advanced cancer. Am. J. Hosp. Palliat. Care 31, 534–542 (2014).
Selby, D. et al. A single set of numerical cutpoints to define moderate and severe symptoms for the Edmonton Symptom Assessment System. J. Pain Symptom Manag. 39, 241–249 (2010).
Acknowledgements
The authors would like to thank all participating centres, the healthcare professionals who helped with patient recruitement and the patients who provided the survey data.
Funding
This study was funded by a grant from ZonMw, The Netherlands Organisation for Health Research and Development (grant number 844001402).
Author information
Authors and Affiliations
Contributions
Study design: L.S., A.H., A.R., Y.L. Conceptualization: L.S., Y.L. Data collection: L.S., A.H., A.R., Y.L. Methodology: M.H., E.M., P.J., J.B., M.S., R.L. Formal analysis: M.H., E.M., R.L. Writing and drafting manuscript: L.S., M.H., E.M. Revision and editing of manuscript: M.H., E.M., A.H., P.J., J.B., M.S., R.L., A.R., Y.L. Funding acquisition: A.R., Y.L. Supervision: R.L., A.R., Y.L.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van der Stap, L., van Haaften, M.F., van Marrewijk, E.F. et al. The feasibility of a Bayesian network model to assess the probability of simultaneous symptoms in patients with advanced cancer. Sci Rep 12, 22295 (2022). https://doi.org/10.1038/s41598-022-26342-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-26342-4
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.