Abstract
Traumatic cervical spine injuries (TCSI) are rare injuries. With increasing age the incidence of TCSI is on the rise. TCSI and traumatic brain injury (TBI) are often associated. Both TCSI and TBI are allocated to the Abbreviated Injury Scale (AIS) head region. However, the nature and outcome of these injuries are potentially different. Therefore, the aim of this study was to investigate the epidemiology, demographics and outcome of severely injured patients with severe TCSI, and compare them with polytrauma patients with severe TBI in the strict sense. Consecutive polytrauma patients aged ≥ 15 years with AIShead ≥ 3 who were admitted to a level-1 trauma center Intensive Care Unit (ICU) from 2013 to 2021 were included. Demographics, treatment, and outcome parameters were analyzed for patients who had AIShead ≥ 3 based on TCSI and compared to patients with AIShead ≥ 3 based on proper TBI. Data on follow-up were collected for TCSI patients. Two hundred eighty-four polytrauma patients (68% male, Injury Severity Score (ISS) 33) with AIShead ≥ 3 were included; Thirty-one patients (11%) had AIShead ≥ 3 based on TCSI whereas 253 (89%) had AIShead ≥ 3 based on TBI. TCSI patients had lower systolic blood pressure in the Emergency Department (ED) and stayed longer in ICU than TBI patients. There was no difference in morbidity and mortality rates. TCSI patients died due to high cervical spine injuries or respiratory insufficiency, whereas TBI patients died primarily due to TBI. TCSI was mainly located at C2, and 58% had associated spinal cord injury. Median follow-up time was 22 months. Twenty-two percent had improvement of the spinal cord injury, and 10% died during follow-up. In this study the incidence of severe TCSI in polytrauma was much lower than TBI. Cause of death in TCSI was different compared to TBI demonstrating that AIShead based on TCSI is a different entity than based on TBI. In order to avoid data misinterpretation injuries to the cervical spine should be distinguished from TBI in morbidity and mortality analysis.
Similar content being viewed by others
Introduction
Traumatic cervical spinal injuries (TCSI) are a rare entity in the general trauma population with a historically bimodal distribution with peaks in younger people around their 20s and elderly in their 60–70s. With increasing age of the general trauma population, the incidence of TCSI has increased (with conservation of the bimodal distribution), and an incidence up to 6.7% has been reported in trauma patients1,2,3,4. Additionally, the incidence of moderate to severe traumatic brain injury (TBI) is on the rise5. In a previous study it was demonstrated that the proportion of TBI has become the most common cause of death in blunt trauma6. In literature, the incidence of cervical spine injury in patients with TBI has been reported up to 13%7,8,9,10. Conversely, TBI is frequently associated with cervical spinal injury; the incidence of moderate to severe TBI in patients with cervical spine injury is reported between 18 and 40%4,7. Additionally, recent studies estimated that concurrent TBI in patients with primary traumatic spinal cord injury ranged from 12.5 to 74.2%, based on the diagnostic criteria utilized11,12.
Injury severity score (ISS) is an anatomical scoring system that provides an overall score for patients with multiple injuries. Each injury is assigned an abbreviated injury scale (AIS) score and is allocated to one of six body regions. ISS is calculated by taking the highest AIS severity code in each of the three most severely injured ISS body regions, square each AIS code and add the three squared numbers for an ISS. When calculating data on ISS in trauma patients, TBI and injury to the cervical spine are both part of AIShead, since AIS scores are created to assess the injury severity including the threat to life associated with the injury based on anatomical location13. However, the nature and outcome of these injuries are potentially different. Therefore, the aim of this study was to investigate the epidemiology, demographics and outcome of severely injured patients with severe TCSI (AIShead ≥ 3), and compare them with polytrauma patients with severe TBI in the strict sense. It was hypothesized that there was no difference in morbidity and (cause of) mortality between polytrauma patients with associated severe TCSI and severe TBI.
Methods
Study setting
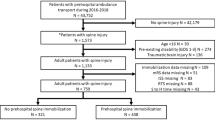
From November 2013–November 2021 a prospective population-based cohort study was undertaken including all consecutive polytrauma patients with AIShead ≥ 3 who were admitted to the Intensive Care Unit (ICU) of the University Medical Center Utrecht. This is a level-1 trauma center in the province of Utrecht and covers the central region of the Netherlands with a service area of 1500 square kilometers and approximately 1.3 million residents. The service area for neurosurgery facilitates 2.1 million residents. Around 1300 trauma patients with full activation of a trauma team are annually admitted. Approximately 375 of them are polytrauma patients14. Polytrauma (severely injured) patients included in the study were all admitted to ICU either directly from the emergency department (ED) or postoperatively after urgent surgery was performed. Patients < 16 years of age, and/or with isolated injury to the brain (AIShead 3 or more and AIS 2 or less in other regions), asphyxiation, hanging, drowning and burns were excluded, because of possible different physiologic response to severe trauma and a significantly different mortality and morbidity profile15,16. Patients who had both severe TCSI and severe TBI (AIShead ≥ 3) were also excluded from further analysis.
A polytrauma patient was defined as a patient with AIS score of greater than 2 in at least two ISS body regions combined with the presence of one or more physiological risk factors such as hypotension (systolic blood pressure ≤ 90 mmHg), level of consciousness (Glasgow Coma Scale score ≤ 8), acidosis (base excess ≤ − 6.0 mEq/L), coagulopathy (international normalized ratio ≥ 1.4/partial thromboplastin time ≥ 40 s) and age (≥ 70 years)17.
Data collection
All in-hospital data were prospectively collected on arrival in ED and on a daily basis in ICU by authors KW and LL, and included patient demographics, ISS, shock and resuscitation parameters. Both crystalloid and blood product (Packed Red Blood Cells (PRBC), Fresh Frozen Plasma (FFP), Platelets (PLT)), and tranexamic acid (TXA) administration was recorded in the first 24 h following admission. Denver Multiple Organ Failure (MOF) scores and Adult Respiratory Distress Syndrome (ARDS) Berlin criteria were registered daily up until 28 days or discharge from ICU18,19. All severely injured patients had a total body CT scan on arrival in ED. Cervical spinal injuries were classified based on the level of the bony injury. In case of suspicion of ligamentous spinal injury and/or spinal cord injury, an additional magnetic resonance imaging (MRI) was performed to evaluate the spinous ligaments and spinal cord. Spinal cord injury was quantified by the American Spinal Injury Association (ASIA) impairment scale20.
There were two causes of death in which patients developed failure of the respiratory system; Patients with high cervical spinal cord injuries (above C5) and the inability to breath spontaneously who subsequently died of respiratory failure were classified as death by high cervical spinal injury. In contrast, to avoid confusion between the two causes of death, patients who died because of respiratory failure caused by injuries to the chest and/or pulmonary complications such as pneumonia were classified as death by respiratory failure.
Follow-up data in polytrauma patients with associated cervical spine injury were retrospectively collected and follow-up time was calculated up until 31st January 2022.
Primary outcome was the comparison of polytrauma patients with associated AIShead ≥ 3 based on TCSI and TBI. Additionally, detailed data on the epidemiology and outcome of TCSI patients was collected.
Ethical approval
The Medical Ethical Review Board of the University Medical Center Utrecht approved this study and granted a waiver of informed consent (reference number WAG/mb/16/026664). All methods were performed in accordance with the relevant guidelines and regulations.
Statistical analysis
Data were analyzed using IBM SPSS Statistics, version 25.0 (Armonk, NY, USA). Results are presented as median and interquartile range (IQR). Comparison of continuous variables was done using Kruskal–Wallis. Significant differences for categorical variables were calculated through Chi-Square test or Fisher’s exact test depending on the size of the groups. Statistical significance was defined as P < 0.05.
Results
Two hundred eighty-seven severely injured patients (68% male, ISS 33) with AIShead ≥ 3 who were admitted to ICU were included. A flowchart of included patients is shown in Fig. 1. Two hundred fifty-three patients had AIShead ≥ 3 based on TBI in the strict sense, whereas 31 patients had AIShead ≥ 3 based on TCSI. Three patients who had both severe TCSI and severe TBI (AIShead ≥ 3) were excluded, so two hundred eighty-four patients were included for further analysis. Physiology, resuscitation, and outcome data of both patient groups are presented in Table 1. Patients who had AIShead ≥ 3 based on TCSI had a lower AIShead (3 (3–5) vs. 4 (3–4), P < 0.001), and lower AISpelvis/extremities (0 (0–3) vs. 2 (1–3), P = 0.008). Both groups had associated severe chest injuries; Seventy-one % (22/31) of TCSI patients and 72% (183/253) had a serious associated thoracic injuries (AISchest ≥ 3).
Further, TCSI patients had a lower systolic blood pressure (SBP) on arrival in ED (SBP_ED 100 (80–124) vs. 124 (101–142) mmHg, P < 0.0001). There were no differences in other physiological parameters. There was also no difference in the administration of crystalloids nor in blood products in the first 24 h between both groups. Patients with associated severe TCSI stayed longer in ICU, but had similar days on the ventilator and length of hospital stay. There was no difference in complication rate and mortality (Table 1). Median time of death in TBI was 6 (2–11) days after admission compared to 11 (2–47) days in TCSI patients (P = 0.18). There was however a difference in cause of death between both groups; patients with associated TCSI died mainly of inability to breath spontaneously caused by the spinal cord injury on the level on C2–C3, followed by respiratory insufficiency (due to injuries to the chest or pulmonary complications, but not primarily caused by spinal cord injury), whereas the vast majority of patients with associated TBI died of the brain injury, followed by respiratory insufficiency (Fig. 2).
Traumatic cervical spine injury location
The most common cervical spine injury was located in C2 (n = 16, 29%), followed by C6 and C7 (n = 11, (18%) and n = 12, (22%), respectively). Three patients (5%) had injuries located in C1, four patients (7%) in C3, six patients (11%) in C4, and five patients (9%) in C5. Nineteen (61%) patients with severe TCSI had injuries on multiple levels in the cervical spine. Twenty patients (65%) who had cervical spine injuries also had injuries in thoracic (16 patients) and/or lumbar spine (5 patients, one of them had injuries in both thoracic and lumbar spine, Table 2). Two TCSI patients (6%) had associated minor TBI (AIShead ≤ 2).
Five patients suffered from associated blunt cerebrovascular injuries to either internal carotid arteries or vertebral arteries. They were treated with antiplatelet therapy without further complications.
Twenty-one (68%) patients underwent urgent surgery (≤ 24 h), thirteen of them had spinal fixation within 24 h. Another two patients had spinal fixation on respectively day 1 and day 3 after admission. Eight patients had urgent surgery for other injuries (abdominal injuries, extremity fractures, Table 3).
Traumatic spinal cord injury (TSCI)
Eighteen patients (65%) had associated traumatic spinal cord injury (TSCI), and more than half of patients sustained a complete spinal cord injury (ASIA A, Table 2). C3–C4 was the most frequent location of TSCI (Table 4). All patients with C1 and C2 fractures with associated TSCI died in hospital because of high cervical spinal cord injury and the inability to breath spontaneously. Twelve TSCI patients (67%) had fixation of their spinal fractures, all within 24 h after arrival in ED. Six patients had no spinal fixation; three of them died early after admission due to high cervical spinal cord injury, one other patient had a penetrating injury to C5, and two others had minimal osseous injuries that needed no surgical stabilization. There was no difference in physiological and resuscitation parameters nor any difference in morbidity and in-hospital mortality compared to patients without TSCI.
Follow-up of TCSI patients
Five (16%) TCSI patients died in hospital (3 patients with ASIA A, and 2 patients with ASIA E). Median follow-up time of TCSI patients was 22 (11–29) months. One patient with ASIA E was lost to follow-up. Three patients remained ventilator-dependent at discharge. Figure 3 demonstrates the relation between ASIA on arrival in hospital and ASIA during last follow-up. None of the patients developed deterioration of their spinal cord injury. Four TSCI patients (22%) had amelioration of their spinal cord injury during follow-up; Two patients with TSCI on thoracic spine level improved from ASIA D to normal motor and sensory function (ASIA E), one patient with TSCI on C3 progressed from ASIA A to B, and one patients with TSCI on C3 improved from ASIA C to D. During follow-up period three TCSI patients (10%) died, all with associated spinal cord injury on the level of C3 or C4. One patient died due to sepsis caused by a pressure ulcer, one due to arrhythmias caused by autonomic dysfunction associated with high spinal cord injury, and one died of respiratory insufficiency due to pulmonary complications.
Discussion
In this study the incidence of severe TCSI in polytrauma was much lower than severe TBI. Cause of death in TCSI was different compared to TBI demonstrating that AIShead based on cervical spine injury is a different entity than AIShead based on TBI.
The incidence of severe TCSI was 6% (31/486) in all polytrauma patients admitted to ICU, and 11% (31/284) in patients with AIShead ≥ 3. Additionally, 9% of patients with severe TCSI had associated severe TBI. The incidence of TCSI and its association with TBI is in accordance with several other reports from literature1,2,3,4,7,8,9,10.
TCSI patients had a lower SBP on arrival in ED. It is likely that the majority of TCSI patients with associated serious spinal cord injury had developed neurogenic shock. However, there was no significant difference in SBP in ED in TCSI patients with and without spinal cord injury. Further, TCSI patients stayed almost twice as long in ICU than TBI patients even though ventilator days and length of hospital stay were comparable. Again, this could not be explained by the presence of spinal cord injury since there was no difference in ventilator days, days in ICU, and days in hospital in TCSI patients with and without spinal cord injury. Possibly, TCSI patients had a higher risk of respiratory problems, needed a tracheostomy more often, and therefore stayed longer in ICU even though they were technically not mechanically ventilated anymore.
In this study detailed data on traumatic cervical spine injuries showed that C2 was the most common location of cervical spine fracture, followed by C6–C7. This is in line with other studies1,4,21. More than half the patients suffered from complete spinal cord injury with C3–C4 being the most common location for the spinal cord injury. This complete spinal cord injury rate is higher than reported in previous studies4,22,23. This is likely caused by the inclusion criteria of polytrauma patients with associated AIShead ≥ 3. Another explanation could be that there were several TCSI patients with associated high spinal cord injury. In the past these patients would have died prior to arrival to the hospital because of the inability to breath spontaneously. With short transport times and quick access to medical treatment these patients nowadays frequently arrive alive in ED. Consequently, this high cervical spinal cord injury with subsequent inability to breath spontaneously has become one of the most common causes of death in TCSI patients. The high incidence of respiratory insufficiency which was the other major cause of death could be explained by the fact that injuries to the chest were the most frequently and most severely associated injuries in both TCSI and TBI. This association of chest injuries and injuries to the cervical spine and TBI in severely injured have been reported previously as well22,24. The differences in cause of death between TCSI and TBI patients were also reflected by the time of death; median time to death was almost twice as long in TCSI patients compared to TBI patients. This was however not statistically significant which was likely caused by the relative low numbers of deceased in TSCI group.These differences in cause and time of death also indicate that AIShead based on TCSI should be treated as a different entity than AIShead based on TBI.
Twenty-two percent of TCSI patients with traumatic spinal cord injury had any improvement in motor and/or sensory function during median follow-up of almost two years; 66% of ASIA D, 9% of ASIA A and 33% of ASIA C patients improved by one grade. This seems lower than reported in the meta-analysis by Khorasanizadeh et al.25. This is likely caused by both the inclusion criteria (polytrauma, AIShead ≥ 3, admission to ICU) and the low numbers in this study.
TCSI patients with associated spinal cord injury had similar in-hospital mortality rates than TCSI without spinal cord injury, suggesting that in-hospital care for patients with associated traumatic spinal cord injury was adequate. However, when overall mortality including death during follow-up was calculated, 26% (8/31) of TCSI patients died. Thirty-three percent (6/18) of patients with spinal cord injury died compared to 15% (2/13) without spinal cord injury. This seems to be higher than in polytrauma patients with associated TBI. In a previous study in isolated moderate to severe TBI it was demonstrated that few patients died post hospital discharge26.
This high overall death rate shows that patients with associated spinal cord injury have residual problems after discharge from hospital with significant risk at dying from complications related to the immobility caused by the spinal cord injury. This was demonstrated by others as well27.
The strength of this study was detailed data of both demographics, physiology, resuscitation and in-hospital outcome in polytrauma patients with AIShead ≥ 3, and an almost 2-year follow-up in severely injured patients with associated traumatic cervical spine injury.
A few limitations need to be acknowledged: Firstly, this was a retrospective analysis of a single center prospective cohort study with relatively low numbers and its accompanying limits. Further, treating clinicians were also the researchers. Additionally, no details on comorbidities were collected nor any post discharge data on polytrauma patients with associated TBI.
To our knowledge, this is the first study in which polytrauma patients with AIShead ≥ 3 based on either TCSI or TBI were compared. Data demonstrated that TCSI patients are a different entity than TBI patients which is clearly shown by differences in cause of death. For future studies it is important to keep in mind that traumatic cervical spinal (cord) injuries have a potentially different threat of life associated with the injury than TBI. To acknowledge these differences and to avoid data misinterpretation injuries to the cervical spine should be distinguished from TBI in morbidity and mortality analysis even though they have similar injury severity according to Abbreviated Injury Scale.
Data availability
The dataset supporting the conclusions of this article are available upon reasonable request from the corresponding author.
References
Passias, P. G. et al. Traumatic fractures of the cervical spine: Analysis of changes in incidence, cause, concurrent injuries, and complications among 488,262 patients from 2005 to 2013. World Neurosurg. 110, e427–e437. https://doi.org/10.1016/j.wneu.2017.11.011 (2018).
Clayton, J. L. et al. Risk factors for cervical spine injury. Injury 43(4), 431–435 (2012).
Milby, A. H., Halpern, C. H., Guo, W. & Stein, S. C. Prevalence of cervical spinal injury in trauma. Neurosurg. Focus 25(5), E10. https://doi.org/10.3171/FOC.2008.25.11.E10 (2008).
Jochems, D. et al. Incidence, causes and consequences of moderate and severe traumatic brain injury as determined by abbreviated injury score in the Netherlands. Sci. Rep. 11(1), 19985. https://doi.org/10.1038/s41598-021-99484-6 (2021).
Jochems, D., Leenen, L. P. H., Hietbrink, F., Houwert, R. M. & van Wessem, K. J. P. Increased reduction in exsanguination rates leaves brain injury as the only major cause of death in blunt trauma. Injury 49(9), 1661–1667 (2018).
Utheim, N. C. et al. Epidemiology of traumatic cervical spinal fractures in a general Norwegian population. Inj. Epidemiol. 9(1), 10. https://doi.org/10.1186/s40621-022-00374-w (2022).
Pandrich, M. J. & Demetriades, A. K. Prevalence of concomitant traumatic cranio-spinal injury: A systematic review and meta-analysis. Neurosurg. Rev. 43(1), 69–77 (2020).
Hlwatika, P. & Hardcastle, T. C. Concurrent cranial and cervical spine injuries by associated injury mechanisms in traumatic brain injury patients. S. Afr. J. Radiol. 26(1), 2321. https://doi.org/10.4102/sajr.v26i1.2321 (2022).
Thesleff, T., Kataja, A., Öhman, J. & Luoto, T. M. Head injuries and the risk of concurrent cervical spine fractures. Acta Neurochir. (Wien) 159(5), 907–914. https://doi.org/10.1007/s00701-017-3133-0 (2017). Erratum in: Acta Neurochir. (Wien) 159(5), 915–916 (2017).
Fujii, T., Faul, M. & Sasser, S. Risk factors for cervical spine injury among patients with traumatic brain injury. J. Emerg. Trauma Shock 6(4), 252–258 (2013).
Sikka, S. et al. Inconsistencies with screening for traumatic brain injury in spinal cord injury across the continuum of care. J. Spinal Cord. Med. 42(1), 51–56 (2019).
Valbuena Valecillos, A. D., Gater, D. R. & Alvarez, G. Concomitant brain injury and spinal cord injury management strategies: A narrative review. J. Pers. Med. 12(7), 1108. https://doi.org/10.3390/jpm12071108 (2022).
AAAM. The Abbreviated Injury Scale-2005 Revision, Update 2008 (AAAM, 2008).
Gunning, A. C. et al. Demographic patterns and outcomes of patients in level-1 trauma centers in three international trauma systems. World J. Surg. 39(11), 2677–2684 (2015).
Dewar, D. C., Tarrant, S. M., King, K. L. & Balogh, Z. J. Changes in the epidemiology and prediction of multiple-organ failure after injury. J. Trauma Acute Care Surg. 74(3), 774–779 (2013).
Dewar, D. C. et al. Comparison of postinjury multiple-organ failure scoring systems: Denver versus sequential organ failure assessment. J. Trauma Acute Care Surg. 77, 624–629 (2014).
Pape, H. C. et al. The definition of polytrauma revisited: An international consensus process and proposal of the new “Berlin definition”. J. Trauma Acute Care Surg. 77(5), 780–786 (2014).
Sauaia, A., Moore, F. A. & Moore, E. E. Early predictors of postinjury multiple organ failure. Arch. Surg. 129, 39–45 (1994).
Ranieri, V. M. et al. Acute respiratory distress syndrome: The Berlin definition. JAMA 307(23), 2526–2533 (2012).
American Spinal Injury Association/International Medical Society of Paraplegia. International Standards for Neurological and Functional Classification of Spinal Cord Injury-Revised 2000 (ASIA, 2002).
Prasad, V. S., Schwartz, A., Bhutani, R., Sharkey, P. W. & Schwartz, M. L. Characteristics of injuries to the cervical spine and spinal cord in polytrauma patient population: Experience from a regional trauma unit. Spinal Cord. 37(8), 560–568 (1999).
Laurer, H. et al. Distribution of spinal and associated injuries in multiple trauma patients. Eur. J. Trauma Emerg. Surg. 33(5), 476–481 (2007).
Hackenberg, R. K. et al. Cervical spine injuries requiring surgery in a Level I trauma centre in a major German city. Acta Neurochir. (Wien) 164(1), 35–41 (2022).
Niemeyer, M. et al. Mortality in polytrauma patients with moderate to severe TBI on par with isolated TBI patients: TBI as last frontier in polytrauma patients. Injury 53(4), 1443–1448 (2022).
Khorasanizadeh, M. et al. Neurological recovery following traumatic spinal cord injury: A systematic review and meta-analysis. J. Neurosurg. Spine. https://doi.org/10.3171/2018.10.SPINE1880 (2019).
Jochems, D. et al. Outcome in patients with isolated moderate to severe traumatic brain injury. Crit. Care Res. Pract. https://doi.org/10.1155/2018/3769418 (2018).
Adegeest, C. Y. et al. Influence of severity and level of injury on the occurrence of complications during the subacute and chronic stage of traumatic spinal cord injury: A systematic review. J. Neurosurg. Spine 36(4), 632–652 (2021).
Author information
Authors and Affiliations
Contributions
K.W. and L.L. have contributed to the conception and design of the study. K.W. and L.L. have performed acquisition of data. K.W. has done the analysis and interpretation of data. K.W. and M.N. have drafted the article. M.N. and L.L. have revised it critically for important intellectual content. K.W., L.L., and M.N. have given final approval of the version to be submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van Wessem, K.J.P., Niemeyer, M.J.S. & Leenen, L.P.H. Polytrauma patients with severe cervical spine injuries are different than with severe TBI despite similar AIS scores. Sci Rep 12, 21538 (2022). https://doi.org/10.1038/s41598-022-25809-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-25809-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.