Abstract
We evaluated the pre- and postoperative sleep quality of patients with newly diagnosed papillary thyroid carcinoma (PTC) who underwent thyroid surgery, and investigated the factors associated with persistent poor sleep quality. The Pittsburgh sleep quality index (PSQI), Epworth sleepiness scale, and Stanford sleepiness scale were used to estimate sleep quality and daytime sleepiness. Face-to-face surveys were conducted preoperatively, and 1, 4, and 10 months after thyroid surgery. The PSQI was administered during a telephone interview about after 5 years after surgery. Forty-six patients (mean age 47.3 ± 10.1 years) with PTC (11 males, 35 females) were included in this study. Twenty-one participants underwent lobectomy and 25 underwent total thyroidectomy. Preoperatively, 35 (76.1%) patients showed poor sleep quality. PSQI scores at postoperative 1, 4, and 10 months were significantly lower than preoperative scores (p < 0.001). Postoperative 5-year PSQI scores decreased significantly compared to the preoperative scores (p < 0.001). Patients newly diagnosed with PTC suffered from sleep disturbance before and after surgery for at least 10 months, recovering to a comparable rate of sleep disturbance with the general population by 5 years after surgery. Higher preoperative PSQI score was at risk for prolonged poor sleep quality in patients with PTC.
Similar content being viewed by others
Introduction
Thyroid cancer is the most common malignancy of the endocrine system. Due to improvements in diagnostic techniques, the worldwide incidence of thyroid cancer diagnosis has been increasing rapidly since the mid-1990s1. Treatment typically involves surgical intervention and radioactive iodine therapy to minimize the risk of recurrence and metastatic spread2.
The quality of life of patients with cancer links to their sleep quality3. Impaired sleep quantity or quality have been linked to numerous negative health outcomes, including insulin resistance, type 2 diabetes mellitus, cardiovascular disease, and mortality4. The prevalence of sleep disturbance in patients with cancer is 33–40%, which is about twice as high as the rate reported among the general population5. Physiological and psychological burdens related to a patient’s condition and treatment may increase their risk of poor sleep quality6,7. There are reports that sleep disturbance is associated with increased risk of thyroid cancer8,9. Likewise, good quality of sleep is reported to be a protective factor against thyroid cancer10.
While patients often complain of fatigue or sleep disturbance after thyroid surgery, there is a lack of research investigating sleep quality before and after surgery among patients with newly diagnosed thyroid cancer. In this study, we evaluated the preoperative and postoperative (PO) sleep quality of patients with newly diagnosed papillary thyroid cancer (PTC) and investigated the factors associated persistent poor sleep quality.
Methods
Study participants
We prospectively recruited subjects with newly diagnosed PTC at Seoul Metropolitan Government Seoul National University Boramae Medical Center between June 2016 and February 2017. Past medical history and clinicopathological features of thyroid cancer were obtained from the patient’s medical records. Written informed consent was obtained from all participants, and the Institutional Review Board at Seoul Metropolitan Government Seoul National University Boramae Medical Center approved this study (IRB No. 16-2016-61). The work described here was carried out in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans.
Surgical procedures and postoperative follow-up
All participants underwent conventional open lobectomy (n = 21) or total thyroidectomy (n = 25). Thyroid surgeries were performed in a standardized method. Surgical extent and use of radioactive iodine treatment were determined in accordance with the 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer11. Thyroid hormone replacement therapy was initiated to maintain target thyroid stimulating hormone level below 0.1 mU/L for high-risk of recurrence patients and below 2.0 mU/L for low-risk patients11.
Assessment of sleep
Following confirmation of thyroid carcinoma by fine needle aspiration or gun biopsy, three questionnaires about sleep quality were administered preoperatively, and at PO 1, 4, and 10-month timepoints. To assess the long-term sleep quality outcomes after thyroidectomy, the PSQI was administered via a telephone interview by an independent surveyor in April 2022, approximately 5 years after surgery.
The Pittsburgh Sleep Quality Index (PSQI) was used with permission from the authors to measure sleep quality and sleep patterns during the month before surgery (Supplementary Table S1)12. The PSQI contains self-rated questions addressing seven domains of sleep, which are evaluated on a 3-point scale (0–3 points). Total PSQI scores ranges from 0 to 21 with higher scores indicating worse sleep quality. The original authors proposed a cutoff value of 5 in the global score to distinguish poor sleepers (> 5) from good sleepers (≤ 5)12. In clinical practice, a cutoff score greater than 7 point has been reported to be more appropriate to determine poor sleep13,14,15,16. Therefore, we defined a ‘poor sleeper’ as a patient with a PSQI score greater than 7 points and a ‘persistent poor sleeper’ as a patient whose PSQI score at postoperative 10 months was greater than 717,18,19. Daytime sleepiness was evaluated using the Epworth sleepiness scale (ESS; Supplementary Table S2) and the Stanford sleepiness scale (SSS; Supplementary Table S3)20,21. ESS scores range from 0 to 24, with a score greater than 10 indicating pathological sleepiness22. The SSS consists of a seven-point scale ranging from 1 (very alert) to 7 (very sleepy)21.
Statistical analysis
The normality assumption of continuous variables was checked using the Kolmogorov–Smirnov test. The normality of the residuals was checked by linear regression analysis, to meet the assumptions of the model. An analysis of covariance (ANCOVA) model for continuous variables was used to compare sleep quality before surgery and at PO 1, 4, and 10 months. Cohen suggests that an effect size of 0.2–0.3 indicates a small effect, an effect size of around 0.5 indicates a medium effect, and an effect size of 0.8 or higher indicates a large effect. Binary outcomes were compared using χ2 tests or Fisher’s exact tests, depending on the distribution of variables according to the Kolmogorov–Smirnov test. Comparisons between groups were performed with the Mann–Whitney U test. Variables with a p-value < 0.1 on univariate regression were considered to be candidates for multivariate analysis. Odds ratios (ORs) and 95% CI were reported for significant differences. Statistical analyses were performed using SPSS statistical software version 21 (IBM Corp: IBM SPSS Statistics for Windows, Armonk, NY). Two-sided p values < 0.05 were considered statistically significant.
Results
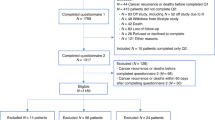
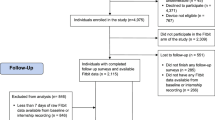
A total of 46 patients were included in the analysis. The mean age was 47.3 ± 10.1 and 11 male and 35 female patients were enrolled. No patient was on medication for mood disorder such as depression or anxiety disorder. The mean preoperative PSQI score was 9.5 ± 3.0, with 11 (23.9%) good sleepers, and 35 (76.1%) poor sleepers. The mean ESS and SSS scores were 6.7 ± 4.6 and 2.2 ± 0.8, respectively. Preoperatively, 46 patients completed all three questionnaires; at PO 1 month, only 29 patients completed all three questionnaires; at PO 4 and 10 months, 33 patients completed all three questionnaires; and 5.5 ± 0.2 years after preoperative evaluation, 33 patients completed long-term telephone PSQI questionnaires.
After adjusting for age, sex, BMI, and surgical extent, PO 1, 4, and 10-month PSQI scores decreased significantly compared with preoperative scores (8.2 ± 2.9, 7.5 ± 3.1, and 7.5 ± 3.1, respectively; Fig. 1). Compared to the preoperative PSQI scores, PO 5-year PSQI scores indicated a significant improvement in sleep quality (9.5 ± 3.0 to 5.4 ± 1.8, p < 0.001). Neither ESS or SSS scores changed significantly before and after surgery. Table 1 shows the clinicopathological characteristics of good and poor sleepers. There were no differences in any parameters between the two groups including age, gender, body mass index, preoperative thyroid stimulating hormone level, tumor size, nodal stage, postoperative risk, or the presence of radioactive iodine treatment.
Table 2 demonstrates the sleep quality scores of the lobectomy verses the total thyroidectomy groups. There were no differences between groups in the PSQI, ESS, or SSS scores at preoperative, and PO 1, 4, and 10 months. However, the mean PSQI score of the lobectomy group was lower than that of total thyroidectomy group (4.6 ± 1.4 vs 6.0 ± 1.8, p = 0.030) at the 5-year follow-up interview.
Figure 2 demonstrates the trend of the PSQI scores of the lobectomy and total thyroidectomy groups over time. In the lobectomy group, PSQI scores at preoperative and PO 1, 4, and 10 months were 8.6 ± 2.4, 8.0 ± 2.6, 7.2 ± 2.2, and 7.4 ± 2.4, respectively. No significant difference was observed between preoperative and 1, 4 and 10 months time points. Overall, the mean PO 5-year PSQI scores were significantly improved compared to the mean preoperative value (8.6 ± 2.4 vs 4.6 ± 1.4, p = 0.002). In the total thyroidectomy group, the preoperative PSQI scores before surgery and at PO 1, 4, and 10 months were 10.2 ± 3.4, 8.4 ± 3.1, 7.7 ± 3.6, and 7.7 ± 3.6, respectively. The PO 1, 4, and 10-month PSQI scores were lower than the preoperative PSQI scores (p < 0.001, p < 0.001, and p < 0.001). Mean PO 5-year PSQI scores were significantly improved compared to the preoperative scores (10.2 ± 3.4 to 6.0 ± 1.8, p < 0.001). The PSQI, ESS, and SSS scores of the six patients who underwent total thyroidectomy followed by radioactive iodine treatment are shown in Table 3.
The clinicopathological features of non-persistent and persistent poor sleepers are compared in Table 4. Persistent poor sleepers showed higher PSQI scores at preoperative, and PO 1, 4, and 10 months compared to non-persistent poor sleepers (p = 0.022, p < 0.001, p = 0.002, and p < 0.001, respectively).
Table 5 summarizes the results of univariate and multivariate logistic regressions of the factors associated with persistent poor sleep quality after surgery. Multivariate analysis revealed that older age (adjusted OR, 1.13; 95% CI 1.13–1.26; p = 0.032) and higher preoperative PSQI scores (adjusted OR, 1.46; 95% CI 1.06–2.01; p = 0.021) were risk factors for persistent poor sleep quality.
Discussion
This prospective longitudinal study investigated sleep quality before and after thyroid surgery among patients diagnosed with PTC, and explored the factors associated with persistent poor sleep quality in the target population. To the best of our knowledge, this is the first report to demonstrate the immediate and long-term impact of PTC and thyroid surgery on sleep quality among patients with PTC. Our results indicate that a considerable number of patients with PTC suffer from sleep disturbance before and after thyroid surgery, and that older age and higher preoperative PSQI scores are associated with persistent poor sleep quality.
Patients with thyroid cancer often complain of sleep disturbance after surgery. In fact, a cross-sectional study reported that poor sleep quality was more common among patients with thyroid cancer than in patients with benign thyroid disease, even after thyroid surgery9. However, because of its cross-sectional design, the previous study could not evaluate the impact of surgery on sleep quality. A large-scale longitudinal study which investigated the natural course of insomnia among patients with various types of cancer over an 18-month period reported that the incidence of insomnia peaked before surgery and dwindled after surgery over the subsequent 18 months23. Insomnia was more commonly observed among patients with many types of cancer including breast, prostate, gynecological, head and neck, and upper gastrointestinal tract cancers. The study showed that while the incidence of insomnia decreased over time after surgery, the incidence was still higher than that of the ‘non-cancer’ population. Likewise, in the current study, the mean PSQI score was highest before surgery and remained above 7 in the 10 months following surgery, although it tended to decrease after surgery.
In the current study, we found that sleep quality was significantly worse before thyroid surgery compared to after surgery. There are several factors which may be involved in the association between sleep disturbance and thyroid cancer. First, sleep disturbance itself may increase the risk of cancer. The prevalence of sleep disturbance is at least two times higher in patients with cancer than in the general population5. Our results revealed the prevalence of poor sleep quality was much higher among patients with PTC (PSQI > 5, 89.1%; PSQI > 7, 76.1%) than the general population (15.9–41.0%)24,25. Another explanation for the high prevalence of sleep disturbance among patients with thyroid cancer is that sleep deprivation may cause thyroid stimulating hormone elevation26 which may be associated with a greater likelihood of thyroid cancer26,27,28,29,30. However, in the current study, preoperative serum thyroid stimulating hormone (TSH) levels were not different between good and poor sleepers. Impaired immune function caused by sleep disturbance has been proposed as another possible risk factor for thyroid cancer31. Disrupted endocrine and physiologic circadian rhythms may lead to impaired circadian rhythm at the level of immune cells32. A recent study demonstrated that patients with well-differentiated thyroid cancer exhibit altered expression of clock genes in comparison with healthy controls or subjects with benign thyroid nodules33. Another study demonstrated alterations of clock genes, overexpression of BMAL1, and downregulation of CRY2, in patients with follicular thyroid carcinoma and PTC34.
Fear is another important potential cause of sleep disturbance in patients with thyroid cancer. There are various relevant types of fear such as fear of cancer diagnosis and fear of general anesthesia or surgery, as well as fear of postsurgical treatment including life-long medication, surgical complications, or recurrence. A recent study reported that anxiety in patients with thyroid cancer significantly improved after surgery35. PSQI scores decreased after surgery in that study. The authors believed that relief from fear of surgery or surgical complications was the key factor in the improvement in sleep quality after surgery. They suggested that because TSH levels are controlled after surgery with medication if needed, sleep disturbance may be caused by anxiety or fear, rather than the hormonal effects of the condition.
We hypothesized that when stratified by surgical type, sleep quality before and after surgery would be worse in the total thyroidectomy group compared to the lobectomy group. There are several reasons that patients undergoing total thyroidectomy may have more anxiety than those undergoing lobectomy prior to surgery. Total thyroidectomy is indicated for tumors larger than 4 cm, tumors with extensive lymph node involvement or distant metastasis, or for bilateral tumors, all of which are associated with unfavorable prognosis. In addition, there are complications which occur only after total thyroidectomy such as bilateral recurrent laryngeal nerve palsy, hypoparathyroidism, and life-long thyroid hormone replacement. During the preoperative period, concerns about poor prognosis and postoperative complications may aggravate the psychological fear of surgery among patients scheduled for total thyroidectomy. Contrary to our expectation, PSQI scores of total thyroidectomy group and lobectomy group were comparable during the pre- and postoperative period during the 10 months follow-up. This can be explained by the assumption that the number of the patients in the both groups were too small to show the difference and the concerns for thyroid surgery were alleviated after surgery.
The PSQI scores of the PTC patients 10 months after surgery remained higher than that of the normal population, which was reported to be 5.6 by a Korea Community Health Survey25. This suggests that anxiety among patients with PTC may continue after surgery. On the other hand, the PSQI scores decreased to 5.4, which is comparable to that of the general population, by the PO 5-year timepoint25. Furthermore, the PO 5-year PSQI scores indicate that the long-term sleep quality of the lobectomy group was significantly improved compared to the total thyroidectomy group. This suggests that sleep quality may improve as concern and anxiety is gradually alleviated over time, and the effect size may depend on the surgical extent.
Reports show that sleep disturbance may be associated with the initiation of radiotherapy or chemotherapy, and a high degree of sleep disturbance can be maintained over the treatment period with adjuvant therapies9,36,37,38. Radioactive iodine treatment is the most common β radiation nuclear medicine therapy. A study reported that mean PSQI scores increased from 7.6 to 8.8 after radioactive iodine treatment9. In the current study, among the six patients treated with total thyroidectomy followed by radioactive iodine therapy, the mean preoperative PSQI score was 9.8. At PO 1 month, the mean PSQI score reduced to 8.9, and further decreased to 7.8 at PO 4 months, before increasing again to 8.9 at PO 10 months. Our repeated measures of PSQI score data indicated that radioactive iodine treatment showed no harmful effect on sleep quality, although diet restriction and conditioning with severe hypothyroidism may have an unfavorable impact on sleep39,40.
Excessive daytime sleepiness, which is a cardinal feature of altered sleep status, is commonly reported in patients with cancer41. Hypersomnia has been associated with multiple factors including cancer types, advanced cancers, active chemotherapy, and side effects from antineoplastic therapy5,42. A previous study of patients with advanced cancers (head and neck, lung, breast, gynecological, genitourinary, gastrointestinal, etc.) demonstrated that 50% of patients showed cancer-related somnolence and mean ESS score was 11.243. In this study, the reason why there was no significant change in the ESS and SSS scores was that preoperative scores (ESS 7.2, SSS 2.2) were already low. It shows patients were not in sleepy status before surgery, therefore, no improvement could be observed. Our data suggests that thyroid cancer might have a lower risk for daytime sleepiness, although hypersomnia in cancer patients has been associated with active chemotherapy, brain tumors, and advanced cancers5,42,44.
This study has several limitations. First, we did not apply scales to evaluate mood disorders such as anxiety or depression, which are important factors associated with sleep disturbance among cancer patients9. Although no patients were on medication for mood disorders during the study period, in-depth interview evaluations of mild mood disorders which do not require medication were not conducted. Second, we did not evaluate the sleep quality of study participants at regular intervals between PO 10 months and 5 years. Therefore, although we showed long-term sleep quality outcomes around 5 years after surgery, we were unable to ascertain the specific point at which the sleep quality of patients with PTC became comparable to that of the general population. Another limitation of this study was the relatively scarce number of patients and the lack of a control group. Comparing sleep quality of patients with PTC with that of patients with different cancers or patients without cancer may have further elucidated the impact of PTC on sleep disturbance in the target population. Further studies with a broader case series should be followed. Next, sleep characteristics, including sleep architecture and sleep apnea, were not assessed objectively using polysomnography in this study. As a recent study reported that moderate to severe obstructive sleep apnea may have a negative impact on cancer progression in patients with PTC45, further studies to elucidate the association between sleep apnea and the aggressiveness of thyroid cancer are required. Last, we could not determine whether PTC had a causative role in sleep disturbance or sleep disturbance had a causative role in PTC occurrence. In this study, preoperative questionnaires were administered when cytologic tests result confirmed PTC and surgery was planned. Therefore, the results reflect only the patient’s sleep quality during a period when they were experiencing fear while waiting for surgery. The use of a measurement tool that reflects sleep quality before recognition of the thyroid nodule or diagnosis of thyroid cancer may be required to determine the causative role of sleep disturbance on thyroid cancer, or vice-versa.
Conclusions
Newly diagnosed patients with PTC suffered from sleep disturbance before and after surgery. High preoperative PSQI scores were associated with persistent poor sleep quality 10 months after surgery. The sleep quality of patients with PTC 5 years after surgery was comparable with that of the general population. Although the cause of sleep disturbance among patients with PTC remains unknown, physicians should be aware of the high incidence of sleep disturbance among this population and take measures to assess and manage sleep quality in patients with PTC.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 70, 7–30. https://doi.org/10.3322/caac.21590 (2020).
American Thyroid Association Guidelines Taskforce on Thyroid Network. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19, 1167–1214. https://doi.org/10.1089/thy.2009.0110 (2009).
Mercadante, S., Girelli, D. & Casuccio, A. Sleep disorders in advanced cancer patients: Prevalence and factors associated. Support Care Cancer 12, 355–359. https://doi.org/10.1007/s00520-004-0623-4 (2004).
Koo, D. L., Nam, H., Thomas, R. J. & Yun, C. H. Sleep disturbances as a risk factor for stroke. J. Stroke 20, 12–32. https://doi.org/10.5853/jos.2017.02887 (2018).
Berger, A. M. Update on the state of the science: Sleep-wake disturbances in adult patients with cancer. Oncol. Nurs. Forum 36, E165–E177. https://doi.org/10.1188/09.ONF.E165-E177 (2009).
Dahiya, S., Ahluwalia, M. S. & Walia, H. K. Sleep disturbances in cancer patients: Underrecognized and undertreated. Cleve Clin. J. Med. 80, 722–732. https://doi.org/10.3949/ccjm.80a.12170 (2013).
Liu, L. & Ancoli-Israel, S. Sleep disturbances in cancer. Psychiatr. Ann. 38, 627–634. https://doi.org/10.3928/00485713-20080901-01 (2008).
Luo, J., Sands, M., Wactawski-Wende, J., Song, Y. & Margolis, K. L. Sleep disturbance and incidence of thyroid cancer in postmenopausal women the Women’s Health Initiative. Am. J. Epidemiol. 177, 42–49. https://doi.org/10.1093/aje/kws193 (2013).
He, Y. et al. Sleep quality of patients with differentiated thyroid cancer. PLoS ONE 10, e0130634. https://doi.org/10.1371/journal.pone.0130634 (2015).
Afrashteh, S., Fararouei, M.A.-O.X., Parad, M. T. & Mirahmadizadeh, A. Sleep quality, stress and thyroid cancer: A case-control study. J. Endocrinol. Investig. 45, 1219. https://doi.org/10.1007/s40618-022-01751-4 (2022).
Haugen, B. R. et al. 2015 American Thyroid Association Management Guidelines for adult patients with thyroid nodules and differentiated thyroid cancer. Thyroid 26, 1–133. https://doi.org/10.1089/thy.2015.0020 (2016).
Buysse, D. J., Reynolds, C. F. 3rd., Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213. https://doi.org/10.1016/0165-1781(89)90047-4 (1989).
Del Rio Joao, K. A., Becker, N. B., de Neves Jesus, S. & Isabel Santos Martins, R. Validation of the Portuguese version of the Pittsburgh sleep quality index (PSQI-PT). Psychiatry Res. 247, 225–229. https://doi.org/10.1016/j.psychres.2016.11.042 (2017).
Kotronoulas, G. C., Papadopoulou, C. N., Papapetrou, A. & Patiraki, E. Psychometric evaluation and feasibility of the Greek Pittsburgh sleep quality index (GR-PSQI) in patients with cancer receiving chemotherapy. Support Care Cancer 19, 1831–1840. https://doi.org/10.1007/s00520-010-1025-4 (2011).
Sohn, S. I., Kim, D. H., Lee, M. Y. & Cho, Y. W. The reliability and validity of the Korean version of the Pittsburgh sleep quality index. Sleep Breath 16, 803–812. https://doi.org/10.1007/s11325-011-0579-9 (2012).
Zhang, C. et al. Reliability, validity, and factor structure of Pittsburgh sleep quality index in community-based Centenarians. Front. Psychiatry 11, 573530. https://doi.org/10.3389/fpsyt.2020.573530 (2020).
Beck, S. L., Schwartz, A. L., Towsley, G., Dudley, W. & Barsevick, A. Psychometric evaluation of the Pittsburgh sleep quality index in cancer patients. J. Pain Symptom Manag. 27, 140–148. https://doi.org/10.1016/j.jpainsymman.2003.12.002 (2004).
Carpenter, J. S. & Andrykowski, M. A. Psychometric evaluation of the Pittsburgh sleep quality index. J. Psychosom. Res. 45, 5–13. https://doi.org/10.1016/s0022-3999(97)00298-5 (1998).
Fichtenberg, N. L., Zafonte, R. D., Putnam, S., Mann, N. R. & Millard, A. E. Insomnia in a post-acute brain injury sample. Brain Inj. 16, 197–206. https://doi.org/10.1080/02699050110103940 (2002).
Cho, Y. W. et al. The reliability and validity of the Korean version of the Epworth sleepiness scale. Sleep Breath 15, 377–384. https://doi.org/10.1007/s11325-010-0343-6 (2011).
Hoddes, E., Zarcone, V., Smythe, H., Phillips, R. & Dement, W. C. Quantification of sleepiness: A new approach. Psychophysiology 10, 431–436. https://doi.org/10.1111/j.1469-8986.1973.tb00801.x (1973).
Johns, M. W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 14, 540–545. https://doi.org/10.1093/sleep/14.6.540 (1991).
Savard, J., Ivers, H., Villa, J., Caplette-Gingras, A. & Morin, C. M. Natural course of insomnia comorbid with cancer: An 18-month longitudinal study. J. Clin. Oncol. 29, 3580 (2011).
Zhang, Y. S. et al. Prevalence and socio-demographic correlates of poor sleep quality among older adults in Hebei Province, China. Sci. Rep. 10, 12266. https://doi.org/10.1038/s41598-020-68997-x (2020).
Lee, S. Y. et al. Factors associated with poor sleep quality in the Korean general population: Providing information from the Korean version of the Pittsburgh sleep quality index. J. Affect. Disord. 271, 49–58. https://doi.org/10.1016/j.jad.2020.03.069 (2020).
Gary, K. A. et al. Total sleep deprivation and the thyroid axis: Effects of sleep and waking activity. Aviat. Space Environ. Med. 67, 513–519 (1996).
Boelaert, K. et al. Serum thyrotropin concentration as a novel predictor of malignancy in thyroid nodules investigated by fine-needle aspiration. J. Clin. Endocrinol. Metab. 91, 4295–4301. https://doi.org/10.1210/jc.2006-0527 (2006).
Haymart, M. R. et al. Higher serum thyroid stimulating hormone level in thyroid nodule patients is associated with greater risks of differentiated thyroid cancer and advanced tumor stage. J. Clin. Endocrinol. Metab. 93, 809–814. https://doi.org/10.1210/jc.2007-2215 (2008).
Meinhold, C. L. et al. Nonradiation risk factors for thyroid cancer in the US Radiologic Technologists Study. Am. J. Epidemiol. 171, 242–252. https://doi.org/10.1093/aje/kwp354 (2010).
Polyzos, S. A. et al. Serum thyrotropin concentration as a biochemical predictor of thyroid malignancy in patients presenting with thyroid nodules. J. Cancer Res. Clin. Oncol. 134, 953–960. https://doi.org/10.1007/s00432-008-0373-7 (2008).
Bovbjerg, D. H. Circadian disruption and cancer: Sleep and immune regulation. Brain Behav. Immun. 17(Suppl 1), S48-50. https://doi.org/10.1016/s0889-1591(02)00066-1 (2003).
Bollinger, T., Bollinger, A., Oster, H. & Solbach, W. Sleep, immunity, and circadian clocks: A mechanistic model. Gerontology 56, 574–580. https://doi.org/10.1159/000281827 (2010).
Ikegami, K., Refetoff, S., Van Cauter, E. & Yoshimura, T. Interconnection between circadian clocks and thyroid function. Nat. Rev. Endocrinol. 15, 590–600. https://doi.org/10.1038/s41574-019-0237-z (2019).
Mannic, T. et al. Circadian clock characteristics are altered in human thyroid malignant nodules. J. Clin. Endocrinol. Metab. 98, 4446–4456. https://doi.org/10.1210/jc.2013-2568 (2013).
Song, C. M., Bang, H. S., Kim, H. G., Park, H. J. & Tae, K. Health-Related Quality of Life After Transoral Robotic Thyroidectomy in Papillary Thyroid Carcinoma.
Garrett, K. et al. Differences in sleep disturbance and fatigue between patients with breast and prostate cancer at the initiation of radiation therapy. J. Pain Symptom Manag. 42, 239–250. https://doi.org/10.1016/j.jpainsymman.2010.11.010 (2011).
Thomas, K. S., Bower, J., Hoyt, M. A. & Sepah, S. Disrupted sleep in breast and prostate cancer patients undergoing radiation therapy: The role of coping processes. Psychooncology 19, 767–776. https://doi.org/10.1002/pon.1639 (2010).
Tian, J., Chen, G. L. & Zhang, H. R. Sleep status of cervical cancer patients and predictors of poor sleep quality during adjuvant therapy. Support Care Cancer 23, 1401–1408. https://doi.org/10.1007/s00520-014-2493-8 (2015).
Green, M. E., Bernet, V. & Cheung, J. Thyroid dysfunction and sleep disorders. Front. Endocrinol. (Lausanne) 12, 725829. https://doi.org/10.3389/fendo.2021.725829 (2021).
Theorell-Haglow, J. et al. Sleep duration is associated with healthy diet scores and meal patterns: Results from the population-based EpiHealth study. J. Clin. Sleep Med. 16, 9–18. https://doi.org/10.5664/jcsm.8112 (2020).
Jaumally, B. A. et al. Excessive daytime sleepiness in cancer patients. Sleep Breath 25, 1063–1067. https://doi.org/10.1007/s11325-020-02151-9 (2021).
Lopez, E., de la Torre-Luque, A., Lazo, A., Alvarez, J. & Buela-Casal, G. Assessment of sleep disturbances in patients with cancer: Cross-sectional study in a radiotherapy department. Eur. J. Oncol. Nurs. 20, 71–76. https://doi.org/10.1016/j.ejon.2014.12.008 (2016).
Yennurajalingam, S., Barla, S. R., Arthur, J., Chisholm, G. B. & Bruera, E. Frequency and characteristics of drowsiness, somnolence, or daytime sleepiness in patients with advanced cancer. Palliat. Support Care 17, 459–463. https://doi.org/10.1017/S1478951518000779 (2019).
Dauvilliers, Y. Differential diagnosis in hypersomnia. Curr. Neurol. Neurosci. Rep. 6, 156–162. https://doi.org/10.1007/s11910-996-0039-2 (2006).
Chen, R. et al. Impact of moderate-to-severe obstructive sleep apnea on aggressive clinicopathological features of papillary thyroid carcinoma. Sleep Med. 96, 99–104. https://doi.org/10.1016/j.sleep.2022.04.015 (2022).
Acknowledgements
Authors would like to thank Hana Lee for the telephone interview. This research was supported by the Clinical Research Grant of Seoul National University Boramae Medical Center (04-2021-0019), and a Grant of Patient-Centered Clinical Research Coordinating Center funded by the Ministry of Health & Welfare, Republic of Korea (Grant Number: HI19C0481, HC19C0103).
Author information
Authors and Affiliations
Contributions
Y.J.C. and D.L.K. designed research. Y.J.C. and D.L.K. collected patients’ data. D.L.K., Y.P., H.N., and Y.J.C. carried out data analysis; D.L.K. and Y.J.C. wrote the article. D.L.K., Y.P., H.N., and Y.J.C. contributed to the discussion and interpretation of the results, and to the refinement of the article. All authors reviewed and approved the final article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Koo, D.L., Park, Y., Nam, H. et al. Sleep quality of patients with papillary thyroid carcinoma: a prospective longitudinal study with 5-year follow-up. Sci Rep 12, 18823 (2022). https://doi.org/10.1038/s41598-022-23549-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-23549-3
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.