Abstract
Background
The prevalence of sleep disturbances among prostate cancer (PCa) survivors, and extent of urologist involvement in sleep care are not well-studied.
Methods
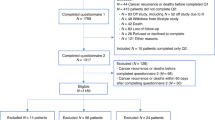
PCa survivors (n = 167) and urologists (n = 145) were surveyed about sleep disturbances and survivorship care practices.
Results
Most PCa survivors had sleep disturbances, including 50.9% with poor sleep quality, 18.0% with clinical/severe insomnia, and 36.5% at high-risk for sleep apnea. Few urologists routinely screened for sleep disturbances, as recommended in national cancer survivorship guidelines.
Conclusions
Optimal PCa survivorship care should incorporate screening for sleep disturbances, addressing comorbid factors affecting sleep and referring to sleep medicine when appropriate.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
National Comprehensive Cancer Network Guidelines: Survivorship. V1.2022. https://www.nccn.org/professionals/physician_gls/pdf/survivorship.pdf. Accessed Sep 2022.
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213.
Morin CM, Belleville G, Belanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–8.
Obstructive Sleep Apnea. The Official STOP-Bang Questionnaire Website. http://stopbang.ca/. Accessed July 2022.
Mastin DF, Bryson J, Corwyn R. Assessment of sleep hygiene using the Sleep Hygiene Index. J Behav Med. 2006;29:223–7.
Robbins R, Jean-Louis G, Chanko N, Combs P, Byrne N, Loeb S. Using data from an online health community to examine the impact of prostate cancer on sleep. BJU Int. 2020;125:634–5.
Robbins R, Cole R, Ejikeme C, Orstad SL, Porten S, Salter CA, et al. Systematic review of sleep and sleep disorders among prostate cancer patients and caregivers: a call to action for using validated sleep assessments during prostate cancer care. Sleep Med. 2022;94:38–53.
Grandner MA, Kripke DF, Yoon IY, Youngstedt SD. Criterion validity of the Pittsburgh Sleep Quality Index: Investigation in a non-clinical sample. Sleep Biol Rhythms. 2006;4:129–39.
Mondal S, Edwards S, Wibowo E, Ahmed H, Wassersug RJ, Ellis J, et al. Evaluating Patterns and Factors Related to Sleep Disturbances in Prostate Cancer Patients. Healthcare. 2022;10:832.
Beck SL, Schwartz AL, Towsley G, Dudley W, Barsevick A. Psychometric evaluation of the Pittsburgh Sleep Quality Index in cancer patients. J Pain Symptom Manag. 2004;27:140–8.
Funding
This study was supported by the NYU Perlmutter Cancer Center Developmental Project Program, which is partially supported by the Cancer Center Support Grant P30CA016087, and the Edward Blank and Sharon Cosloy-Blank Family Foundation. NG is supported by grant 5T32HS026120-04 from the Agency for Healthcare Research and Quality and the NYU Clinical and Translational Science Institute grant 5UL1TR001445. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency.
Author information
Authors and Affiliations
Contributions
Concept and design: SL, AM, SLO, SAK, AM, RR, PC, GJL, NG. Data collection: SL, KS, TSN, NB. Statistical analysis: KS, NG. Interpretation of results: All authors. Drafting of paper: FG, SL, KS, AM, NG. Critical revision of paper: All authors. Supervision: SL, NG. Funding Acquisition: SL.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
NYU IRB number #20-00078. The study was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gong, F., Loeb, S., Siu, K. et al. Sleep disturbances are underappreciated in prostate cancer survivorship. Prostate Cancer Prostatic Dis 26, 210–212 (2023). https://doi.org/10.1038/s41391-022-00630-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-022-00630-6
This article is cited by
-
Feasibility of a novel wearable thermal device for management of bothersome hot flashes in patients with prostate cancer
Prostate Cancer and Prostatic Diseases (2023)