Abstract
Background
We sought to assess the influences of sleep duration, sleep adequacy, and daytime sleepiness on survival outcomes among Stage III colon cancer patients.
Methods
We conducted a prospective observational study of 1175 Stage III colon cancer patients enrolled in the CALGB/SWOG 80702 randomised adjuvant chemotherapy trial who completed a self-reported questionnaire on dietary and lifestyle habits 14–16 months post-randomisation. The primary endpoint was disease-free survival (DFS), and secondary was overall survival (OS). Multivariate analyses were adjusted for baseline sociodemographic, clinical, dietary and lifestyle factors.
Results
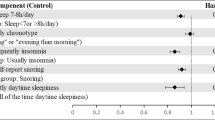
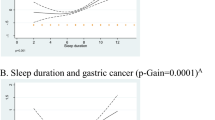
Patients sleeping ≥9 h—relative to 7 h—experienced a worse hazard ratio (HR) of 1.62 (95% confidence interval (CI), 1.01–2.58) for DFS. In addition, those sleeping the least (≤5 h) or the most (≥ 9 h) experienced worse HRs for OS of 2.14 (95% CI, 1.14–4.03) and 2.34 (95% CI, 1.26–4.33), respectively. Self-reported sleep adequacy and daytime sleepiness showed no significant correlations with outcomes.
Conclusions
Among resected Stage III colon cancer patients who received uniform treatment and follow-up within a nationwide randomised clinical trial, very long and very short sleep durations were significantly associated with increased mortality. Interventions targeting optimising sleep health among indicated colon cancer patients may be an important method by which more comprehensive care can be delivered.
Trial registration
ClinicalTrials.gov Identifier: NCT01150045.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data are from the Alliance for Clinical Trials in Oncology. Investigators may request access to this data per Alliance protocol as outlined below and as detailed at https://www.allianceforclinicaltrialsinoncology.org/main/public/standard.xhtml?path=%2FPublic%2FDatasharing. Per NCI National Clinical Trials Network (NCTN) guidelines, any investigator may submit a request for data from published Alliance or legacy ACOSOG, CALGB, or NCCTG trials. To submit a data request, the investigator should complete an Alliance Data Sharing Request Form and send it by e-mail to gro. NTCNecnailla@stpecnoc. Once received, the request will be forwarded to the Alliance Statistics and Data Center (SDC). The SDC will confirm the availability of the data. Once the SDC confirms availability, the investigator will be asked to provide documentation of Institutional Review Board (IRB) approval or exemption from their institution, as well as to submit an Alliance data release agreement. Once the IRB documentation and the data release agreement are received from the requesting investigator, the SDC will be notified that the requested data may be released. Questions about the process may be directed to gro. NTCNecnailla@stpecnoc.
References
Jiao L, Duan Z, Sangi-Haghpeykar H, Hale L, White DL, El-Serag HB. Sleep duration and incidence of colorectal cancer in postmenopausal women. Br J Cancer. 2013;108:213–21.
Luojus MK, Lehto SM, Tolmunen T, Erkkilä AT, Kauhanen J. Sleep duration and incidence of lung cancer in ageing men. BMC Public Health. 2014;14:295.
Xiao Q, Signorello LB, Brinton LA, Cohen SS, Blot WJ, Matthews CE. Sleep duration and breast cancer risk among black and white women. Sleep Med. 2016;20:25–9.
Trudel-Fitzgerald C, Zhou ES, Poole EM, Zhang X, Michels KB, Eliassen AH, et al. Sleep and survival among women with breast cancer: 30 years of follow-up within the Nurses’ Health Study. Br J Cancer. 2017;116:1239–46.
Palesh O, Aldridge-Gerry A, Zeitzer JM, Koopman C, Neri E, Giese-Davis J, et al. Actigraphy-measured sleep disruption as a predictor of survival among women with advanced breast cancer. Sleep. 2014;37:837–42.
Sturgeon SR, Luisi N, Balasubramanian R, Reeves KW. Sleep duration and endometrial cancer risk. Cancer Causes Control: Ccc 2012;23:547–53.
Girschik J, Heyworth J, Fritschi L. Self-reported sleep duration, sleep quality, and breast cancer risk in a population-based case-control study. Am J Epidemiol. 2013;177:316–27.
Vogtmann E, Levitan EB, Hale L, Shikany JM, Shah NA, Endeshaw Y, et al. Association between sleep and breast cancer incidence among postmenopausal women in the Women’s Health Initiative. Sleep. 2013;36:1437–44.
Pinheiro SP, Schernhammer ES, Tworoger SS, Michels KB. A prospective study on habitual duration of sleep and incidence of breast cancer in a large cohort of women. Cancer Res. 2006;66:5521–5.
Wong ATY, Heath AK, Tong TYN, Reeves GK, Floud S, Beral V, et al. Sleep duration and breast cancer incidence: results from the Million Women Study and meta-analysis of published prospective studies. Sleep. 2020;44:zsaa166.
Collins KP, Geller DA, Antoni M, Donnell DM, Tsung A, Marsh JW, et al. Sleep duration is associated with survival in advanced cancer patients. Sleep Med. 2017;32:208–12.
Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–92.
Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, et al. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27:440–4.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA: A Cancer J Clin. 2021;71:7–33.
Lin Y, Peng Y, Liang B, Zhu S, Li L, Jang F, et al. Associations of dinner-to-bed time, post-dinner walk and sleep duration with colorectal cancer: a case-control study. Medicine. 2018;97:e12038.
Papantoniou K, Castaño-Vinyals G, Espinosa A, Turner MC, Martín-Sánchez V, Casabonne D, et al. Sleep duration and napping in relation to colorectal and gastric cancer in the MCC-Spain study. Sci Rep. 2021;11:11822.
Lu Y, Tian N, Yin J, Shi Y, Huang Z. Association between sleep duration and cancer risk: a meta-analysis of prospective cohort studies. PLoS ONE. 2013;8:e74723.
Zhang X, Giovannucci EL, Wu K, Gao X, Hu F, Ogino S, et al. Associations of self-reported sleep duration and snoring with colorectal cancer risk in men and women. Sleep. 2013;36:681–8.
Lin CL, Liu TC, Wang YN, Chung CH, Chien WC. The association between sleep disorders and the risk of colorectal cancer in patients: a population-based nested case-control study. In Vivo. 2019;33:573–9.
Xiao Q, Arem H, Pfeiffer R, Matthews C. Prediagnosis sleep duration, napping, and mortality among colorectal cancer survivors in a large US cohort. Sleep. 2017;40:zsx010.
Innominato PF, Spiegel D, Ulusakarya A, Giacchetti S, Bjarnason GA, Lévi F, et al. Subjective sleep and overall survival in chemotherapy-naïve patients with metastatic colorectal cancer. Sleep Med. 2015;16:391–8.
Ratjen I, Schafmayer C, di Giuseppe R, Waniek S, Plachta-Danielzik S, Koch M, et al. Postdiagnostic physical activity, sleep duration, and TV watching and all-cause mortality among long-term colorectal cancer survivors: a prospective cohort study. BMC Cancer. 2017;17:701.
Meyerhardt JA, Shi Q, Fuchs CS, Meyer J, Niedzwiecki D, Zemla T, et al. Effect of celecoxib vs placebo added to standard adjuvant therapy on disease-free survival among patients with stage III Colon cancer: the CALGB/SWOG 80702 (alliance) randomized clinical trial. J Am Med Assoc. 2021;325:1277–86.
Grothey A, Sobrero AF, Shields AF, Yoshino T, Paul J, Taieb J, et al. Duration of adjuvant chemotherapy for stage III colon cancer. N Engl J Med. 2018;378:1177–88.
André T, Meyerhardt J, Iveson T, Sobrero A, Yoshino T, Souglakos I, et al. Effect of duration of adjuvant chemotherapy for patients with stage III colon cancer (IDEA collaboration): final results from a prospective, pooled analysis of six randomised, phase 3 trials. Lancet Oncol. 2020;21:1620–9.
Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17:1471–4.
Gangwisch JE, Feskanich D, Malaspina D, Shen S, Forman JP. Sleep duration and risk for hypertension in women: results from the nurses’ health study. Am J Hypertens. 2013;26:903–11.
Ayas NT, White DP, Manson JE, Stampfer MJ, Speizer FE, Malhotra A, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163:205–9.
Gangwisch JE, Rexrode K, Forman JP, Mukamal K, Malaspina D, Feskanich D. Daytime sleepiness and risk of coronary heart disease and stroke: results from the Nurses’ Health Study II. Sleep Med. 2014;15:782–8.
Drury A, Payne S, Brady AM. Prevalence vs impact: a mixed methods study of survivorship issues in colorectal cancer. Qual Life Res. 2022;31:1117–34.
Stone CR, Haig TR, Fiest KM, McNeil J, Brenner DR, Friedenreich CM. The association between sleep duration and cancer-specific mortality: a systematic review and meta-analysis. Cancer Causes Control: CCC. 2019;30:501–25.
Mormont M-C, Waterhouse J, Bleuzen P, Giacchetti S, Jami A, Bogdan A, et al. Marked 24-h rest/activity rhythms are associated with better quality of life, better response, and longer survival in patients with metastatic colorectal cancer and good performance status. Clin Cancer Res. 2000;6:3038.
Innominato PF, Focan C, Gorlia T, Moreau T, Garufi C, Waterhouse J, et al. Circadian rhythm in rest and activity: a biological correlate of quality of life and a predictor of survival in patients with metastatic colorectal cancer. Cancer Res. 2009;69:4700.
Innominato PF, Giacchetti S, Bjarnason GA, Focan C, Garufi C, Coudert B, et al. Prediction of overall survival through circadian rest-activity monitoring during chemotherapy for metastatic colorectal cancer. Int J Cancer. 2012;131:2684–92.
Lévi F, Dugué PA, Innominato P, Karaboué A, Dispersyn G, Parganiha A, et al. Wrist actimetry circadian rhythm as a robust predictor of colorectal cancer patients survival. Chronobiol Int. 2014;31:891–900.
Giovannucci E. Metabolic syndrome, hyperinsulinemia, and colon cancer: a review. Am J Clin Nutr. 2007;86:s836–42.
Ayas NT, White DP, Al-Delaimy WK, Manson JE, Stampfer MJ, Speizer FE, et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care. 2003;26:380–4.
Nock NL, Li L, Larkin EK, Patel SR, Redline S. Empirical evidence for “syndrome Z”: a hierarchical 5-factor model of the metabolic syndrome incorporating sleep disturbance measures. Sleep. 2009;32:615–22.
Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB. Association between reduced sleep and weight gain in women. Am J Epidemiol. 2006;164:947–54.
Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity. 2008;16:643–53.
Patel SR, Zhu X, Storfer-Isser A, Mehra R, Jenny NS, Tracy R, et al. Sleep duration and biomarkers of inflammation. Sleep. 2009;32:200–4.
Williams CJ, Hu FB, Patel SR, Mantzoros CS. Sleep duration and snoring in relation to biomarkers of cardiovascular disease risk among women with type 2 diabetes. Diabetes Care. 2007;30:1233–40.
Collis SJ, Boulton SJ. Emerging links between the biological clock and the DNA damage response. Chromosoma. 2007;116:331–9.
Irwin MR. Why sleep is important for health: a psychoneuroimmunology perspective. Annu Rev Psychol. 2015;66:143–72.
Blask DE. Melatonin, sleep disturbance and cancer risk. Sleep Med Rev. 2009;13:257–64.
Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;19:838–45.
Lee S, Meyerhardt JA. Impact of diet and exercise on colorectal cancer. Hematol Oncol Clin North Am. 2022;36:471–89.
Cho OH, Hwang KH. Association between sleep quality, anxiety and depression among Korean breast cancer survivors. Nurs Open. 2021;8:1030–7.
Fortner BV, Stepanski EJ, Wang SC, Kasprowicz S, Durrence HH. Sleep and quality of life in breast cancer patients. J Pain Symptom Manag. 2022;24:471–80.
Zhou ES, Partridge AH, Syrjala KL, Michaud AL, Recklitis CJ. Evaluation and treatment of insomnia in adult cancer survivorship programs. J Cancer Surviv. 2017;11:74–9.
Reynolds-Cowie P, Fleming L. Living with persistent insomnia after cancer: a qualitative analysis of impact and management. Br J Health Psychol. 2021;26:33–49.
Funding
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Numbers U10CA180821 and U10CA180882 (to the Alliance for Clinical Trials in Oncology.) https://acknowledgments.alliancefound.org. UG1CA233163, UG1CA233180, UG1CA233253, UG1CA233290, UG1CA233320, UG1CA233337, UG1CA233339, UG1CA189954, and U10CA180863 to the Canadian Cancer Trials Group; UG1CA233234; and U10CA180820 to the ECOG–ACRIN Cancer Research Group; U10CA180868 to NRG Oncology; and U10CA180888 to the SWOG Cancer Research Network from the National Cancer Institute of the National Institutes of Health. Dr. Meyerhardt is supported by the Douglas Gray Woodruff Chair Fund, the Guo Shu Shi Fund, Anonymous Family Fund for Innovations in Colorectal Cancer, and the George Stone Family Foundation. The National Cancer Institute was involved in the design of the study and review of the manuscript. Pfizer participated in initial protocol development and review and approval of the final manuscript. Pfizer provided celecoxib and placebo tablets. Pfizer was not involved in the collection, management, analysis, or interpretation of the data. Neither Pfizer nor the National Cancer Institute had the right to veto publication or control the decision to which journal the article was submitted. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
Conceptualisation: JAM and SL; data curation: JAM and CM; formal analysis: JAM and CM; funding acquisition: JAM; investigation: JAM and SL; methodology: JAM; validation: QS and JM; visualisation: SL and CM; writing and original draft: JAM and SL; writing, review and editing: SL, CM, QS, JM, PK, FC, PK, SK, DL, BT, EMO, AFS and JAM.
Corresponding author
Ethics declarations
Competing interests
Dr. Shi reported receiving institutional grant support from Celgene–Bristol Myers Squibb and Roche/Genentech; serving as a consultant to Yiviva Inc and Boehringer Ingelheim Pharmaceuticals; and owning stock in Johnson & Johnson, Merck, and Amgen. Dr. Kuebler reported receiving grants from the Columbus National Community Oncology Research Program and the National Institutes of Cancer. Dr. O’Reilly reported receiving institutional grants from Genentech/Roche, Celgene/Bristol Myers Squibb, BioNTech, AstraZeneca, and Arcus; receiving personal fees from CytomX Therapeutics, Rafael Therapeutics, Sobi Consulting, and Synthorx Inc; nonfinancial support from Silenseed Consulting, consulting fees from Boehringer Ingelheim, BioNTech, Ipsen, and Merck; and his spouse receives consulting fees from Bayer, Genentech/Roche, Celgene/Bristol Myers Squibb, Eisai, and Polaris; and personal fees from Molecular Templates Consulting. Dr. Shields reported receiving grants from National Cancer Institute. Dr. Meyerhardt reported receiving grants from National Cancer Institute and personal fees for serving on the advisory boards of COTA Healthcare and Merck, and institutional support from Boston Biomedical for a clinical trial outside the submitted work. The remaining authors declare no competing interests.
Ethics approval and consent to participate
All patients signed study-specific informed consent, which was approved by the NCI Cancer Treatment Evaluation Program and each participating site’s institutional review board. The study was performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, S., Ma, C., Shi, Q. et al. Sleep and cancer recurrence and survival in patients with resected Stage III colon cancer: findings from CALGB/SWOG 80702 (Alliance). Br J Cancer 129, 283–290 (2023). https://doi.org/10.1038/s41416-023-02290-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-023-02290-2