Abstract
Hypokalemia in dairy cows, which is characterized by too low serum potassium levels, is a severe mineral disorder that can be life threatening. In this paper, we explore different originating conditions of hypokalemia—reduced potassium intake, increased excretion, acid-base disturbances, and increased insulin—by using a dynamic mathematical model for potassium balance in non-lactating and lactating cows. The simulations confirm observations described in literature. They illustrate, for example, that changes in dietary intake or excretion highly effect intracellular potassium levels, whereas extracellular levels vary only slightly. Simulations also show that the higher the potassium content in the diet, the more potassium is excreted with urine. Application of the mathematical model assists in experimental planning and therefore contributes to the 3R strategy: reduction, refinement and replacement of animal experiments.
Similar content being viewed by others
Introduction
Potassium is a monovalent cation that is fundamental for cell functioning. It is involved in cell homeostasis and osmotic volume regulation1,2, in acid-base regulation3, formation of resting membrane potential, nerve impulse transmission, and muscle contraction. Its metabolism is a complex dynamical network. Potassium is taken up with feed, distributed between intra- and extracellular space, and excreted mainly with urine4. Milk contains about 1.4 g potassium per liter5,6 and is therefore an important contributor to excretion and loss from the organism, especially in high yielding dairy cows.
Potassium balance disorders can be life-threatening. Hypo- and hyperkalemia describe extracellular potassium below or above its physiological range of 3.9–5.2 mmol/L7, respectively. Hypokalemia is described frequently in cows presented to a veterinary clinic6,8. Clinical records include displaced abomasum with or without volvulus, mastitis, retained placenta, metritis and hepatic lipidosis. A serum potassium concentration below 2.5 mmol/L reflects severe hypokalemia, and most animals will be weak or recumbent. A serum potassium concentration of 2.5–3.5 mmol/L reflects moderate hypokalemia, and some cattle will be recumbent or appear weak with depressed gastrointestinal motility3.
Hypokalemia can result from increased loss, trans-cellular shift, or decreased intake of potassium. Increased loss may occur through the kidney, gastrointestinal tract, or milk. Hypokalaemia can also occur as a result of a redistributing shift of potassium from the extracellular space into cells9. Risk factors described for hypokalemia include high milk yield, reduced feed intake (e.g. due to illness), sweating in the hot season10, systemic or intramammary glucocorticoid treatment (e.g. isoflupredone acetate, dexamethasone3), treatment with multiple doses of dextrose and insulin8,11, and gastrointestinal absorption problems (e.g. due to enteritis or diarrhea).
The aim of our work is to showcase how a systems biology approach based on a kinetic model can be used to advance our understanding of the physiological mechanisms underlying hypokalemia. Kinetic models have already been useful in areas like dairy cattle nutrition12, metabolism13, and reproduction14. However, even though systems biology approaches have already been advocated for many years15, and despite the progress that has been made on the genomic level16, kinetic models in animal sciences are still scarce. One reason is that many animal scientists are simply not acquainted with this approach, so we want to raise awareness with our work. Another reason is that the data needed to parameterize these models are often limited in quality and quantity. Therefore, kinetic models are usually developed iteratively and incrementally, meaning that the model needs to be validated and maybe refined every time new data is gathered. This process becomes easier if a model is extensible and reusable, that is, if it has been designed to evolve and be used beyond its original purpose17. We hypothesize that our previously developed model for potassium balance in dairy cows18 satisfies this criterion by challenging it with a variety of experiments on potassium metabolism from the literature. These experiments include decreased potassium intake, increased excretion with urin or milk, changes in blood pH, a hyperglycaemic clamp for the illustration of elevated insulin, and dexamethasone administration. This model-based approach allows us to study perturbations of potassium homeostasis in silico and to identify knowledge gaps on which future research can be focused.
Methods
Model development and validation
Schematic representation of the components and their relationships in the mechanistic model of potassium balance in cows. Each box represents a model component. The pink color represents potassium, green boxes correspond to metabolic components, and gray arrows and boxes indicate stimulatory or inhibitory effects. All components are fully explained in Table 1.
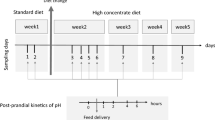
The simulations were performed with an ordinary differential equation (ODE) model published by Berg et al.18, which can be used to simulate the potassium balance in non-lactating and lactating cows. The model had been designed on a whole organism level and includes mechanisms for dry matter intake, the glucose-insulin metabolism, potassium distribution between intra- and extracellular fluid, as well as potassium excretion, see Fig. 1. The model consists of two compartments (intra- and extracellular blood fluid), 12 ODEs, 4 algebraic equations, 63 model parameters, and experimental parameters. All model components and their units are listed in Table 1. The rates are explained in Table 2. The full equations and model parameters are listed in the Supplementary Information.
The model had been validated with data from literature and data from a clinical trial at Freie Universität Berlin. In this trial, potassium concentrations in blood were measured at several time points throughout a day in non-lactating cows without any treatment interventions19. The model can be downloaded as SBML file (Systems Biology Markup Language) from the BioModels database20 and can be run in, e.g., the CellDesigner software.
The starting point for all experiments is the default model setting18,19. It describes a non-lactating cow weighing 600 kg, fed 11.7 kg DMI per day with 1.137% potassium content. If changes are made in this setting, it will be stated in the description of the respective numerical experiment.
The dry matter intake (DMI) is modelled as a periodic function with period length of 24 h according to the day-night rhythm, whereby we assume that feed intake is higher at day time and lower during night. Therefore, all simulated components also show this periodic pattern.
Model improvement
In the following, we describe the changes that were made in the model equations compared to the original model by Berg et al.18. We changed the parameter \(p_{46}\), representing the fraction of glucose and glucogenic substances in the diet, from 0.08 to 0.3, since the latter value more accurately represents the carbohydrate fraction21. Furthermore, when performing simulations with very low to zero feed intake with the original model, we found that the renal potassium excretion was reduced to almost zero. However, literature describes an obligatory potassium excretion in vivo, which is a prerequisite for hypokalemia9. In cows, this potassium excretion is estimated to be 6 g in 24 h21,22. Hence, the parameter \(p_{53}\), which represents the basic potassium excretion with urine in the rate KeKu, was changed from 0.01 to 0.25 g/h to meet the criterion of a basic potassium excretion of 6 g/day during fasting. Moreover, the linear dependency of the rate KeKu on \(K_{ECF}\) was replaced by a threshold-dependent stimulation. This prevents KeKu from becoming too large, which would result in negative concentrations for \(K_{ECF}\).
Numerical experiments on hypokalemia
The numerical experiments were designed to simulate possible scenarios of hypokalemia. Hypokalemia in the model is characterized by a value of extracellular potassium, \(K_{ECF}\), being less than 3.9 mmol/L6. Hypokalemia can result from whole body depletion, where the organism runs out of potassium, or from redistribution, where potassium is moved from extracellular into intracellular space. Glucose blood concentrations, represented by the model component \(Gluc_B\), may also fall below their physiological range of 2.22–3.30 mmol/L (0.40–0.59 g/L)7. This state is referred to as hypoglycemia. Hypokalemia and hypoglycemia may lead to life-threatening conditions within the organism. If one of the two components, i.e., \(K_{ECF}\) or \(Gluc_B\), drops to zero, this marks the end of the numerical experiment.
Whole body depletion
Whole body depletion is characterized by too few potassium being available within the organism. Two scenarios are possible to arrive at this state: reduced potassium intake or increased potassium excretion. Decreased potassium intake over a long time period leads to hypokalemia because of the obligatory potassium loss by the kidney9. In the model, the potassium intake can be reduced by reducing total DMI or by reducing the potassium content in DMI, \(K_{FEED}\).
In the adult cow, an increased potassium excretion happens via the kidney, with milk or with feces. We simulate these different scenarios of whole body depletion in experiments 1–4.
Experiment 1: reduced dry mater intake
In experiment 1, we simulate a reduced potassium intake by reducing DMI, within the default model setting and without milk production. DMI is reduced to zero after 100 h by multiplying the original DMI equation (see Supplementary Information) with a negative Hill function, which switches off DMI at time \(t=p_{100}\). The equation reads
with \(p_{100}=100\) h.
Experiment 2: reduced potassium content in feed
In experiment 2, the potassium content in DMI, \(K_{FEED}\), is varied. To achieve values for \(K_{FEED}\) of 13 g, 40 g, 80 g and 133 g, the model is simulated with the parameter \(p_{56}\) set to 0.001137, 0.003411, 0.006822, and 0.01137, respectively. One should note that low values of \(K_{Feed}\) can easily be simulated in silico, but are difficult to prepare in vivo since ruminants‘ diet is generally rich in potassium23.
Experiment 3: increased potassium excretion with urine
For this experiment, the rate for potassium excretion via urin, KeKu, is multiplied with the experimental parameter \(p_{80}\), which is set to values between 1 and 4, leading to an up to fourfold increased rate KeKu:
All other components are as in the default model setting.
Experiment 4: increased potassium excretion with milk
In vivo, the potassium content in milk varies between individuals and depends on the lactational state24. Potassium content in milk is fixed in the model to be 1.4 mmol/L6. Since the model does not account for varying potassium content in milk, we can only increase overall milk yield. This is achieved by varying parameter \(p_{55}\) [liter milk/h] between 0.0 and 2.0, which corresponds to a milk production of 0–48 L/day. All other components are in the default model setting.
Redistribution
In some conditions, the potassium shift from extracellular to intracellular space increases and may result in hypokalemia. This can be caused by medications, hormonal dysregulation, or raised blood pH9. In experiments 5, 6, and 7, we explore different scenarios of redistribution.
Experiment 5: acidosis, alkalosis
Changes in blood pH affect the potassium distribution between extra- and intracellular space. In alkalosis, i.e. blood pH over 7.45, potassium shifts into the cells, whereas in acidosis, i.e. blood pH below 7.3525, potassium is shifted out of the cells. To change blood pH in the model, we introduce the experimental parameter \(p_{85}\) into the equation for pH,
The model parameter is set to \(p_{85}=\{7.2,\,7.35,\,7.5,\,7.65,\,7.8\}\), respectively, whereby \(p_{85} = 7.5\) corresponds to the default model setting.
Experiment 6: increased insulin
Insulin causes a dose related decline in extracellular potassium26, while potassium shifts into the intracellular space. We simulate the hyperglycaemic clamp as described in26 , where men are infused with glucose solution until reaching a steady state in blood glucose. Responsively, the adrenal glands increase excretion of insulin in order to decrease the blood glucose. During the experiment, the steady state of blood glucose is maintained by further infusions of the same. In the model, we manually set the component \(Gluc_B\) to 1.2 g/L at \(t = 150\) h for the next 50 h.
Experiment 7: dexamethasone administration
Dexamethasone treatment is frequently applied in cows with ketosis to increase available glucose in the blood serum27,28. Furthermore, dexamethasone treatment is described together with decreasing serum potassium concentrations in dairy cows11,29 and in goats30. Complications of dexamethasone treatment can be wide spread. Kojouri et al.31, for example, report a case of atrial fibrillation after ketosis treatment in conjunction with hypokalemia.
We implemented dexamethasone administration in the model to explore its interaction with the glucose-insulin and potassium dynamics, thereby following the dosing scheme from an in vivo experiment at the clinic for Ruminants, Freie Universität Berlin19. Non-lactating cows were treated with Voren Suspension (Dexamethason-21-isonicotinat), using a dose of 0.02 mg/kg body weight as recommended by the producing company Boehringer Ingelheim, which results in a dose of 12 mg for a 600 kg cow, the default body weight in the model.
The pharmakokinetics of Dexamethason-21-isonicotinat was described by Toutin et al.32. In their study, the dose was 0.1 mg/kg body weight, as recommended by the producer at that time, and the pharmacokinetic parameters were determined to be \(t_{max} = 3.6\) h, \(c_{max}= 44.1\) ng/ml and \(AUC = 646.2\). Based on the approach described in Stötzel et al.33, the change of dexamethasone concentration in the blood (in ng/ml) is calculated in our model as
The parameter D represents the amount of administered drug, \(\beta\) is an inverse scale parameter that determines the shape of the area under the curve, and \(c_{Dexa}\) denotes the clearance rate of \(y_{Dexa}\). The values of these three parameters were computed from the pharmacokinetic parameters in32 such that the simulated concentration profile of dexamethason agrees with the dynamics described therein:
Today, a fivefold smaller dose of 0.02 mg per kg bodyweight is recommended by the producer compared with the dose applied in32. To account for this fact, we scaled the parameter D accordingly to \(D=2.36\) ng/mL.
Dexamethasone administration in the model stimulates the rate GpGb, i.e., the release of glucose produced by the liver via gluconeogenesis to the circulating blood. The rate is therefore modified as follows:
This represents the stimulating effect of dexamethasone on gluconeogenesis observed in vivo27,34.
Results and discussion
Whole body depletion
In the model, reduced potassium intake with DMI or \(K_{FEED}\) leads to reduced extracellular potassium concentrations, \(K_{ECF}\). As a consequence, the amount of potassium excreted with urine, \(K_{URIN}\), is also reduced because the rate of urinary potassium excretion, KeKu, depends on \(K_{GIT}\) and \(K_{ECF}\) (compare the full notation of equations and rates in the Supplementary Information). The obligatory urinary potassium loss finally leads to hypokalemia and depletion of extracellular and intracellular potassium, as well as depletion of the store, \(K_{TISS}\).
In vivo, magnesium depletion is described to aggravate severe hypokalemia by increasing renal potassium loss35. Increased excretion via the kidney may be caused by diuretic treatment or aldosterone increase. Aldosterone may increase via the renin-angiotensin-aldosterone-system, e.g., if the blood volume decreases. Increased aldosterone may cause metabolic alkalosis9, which can worsen the diuretic-induced hypokalemia by increasing the potassium shift into cells. Diarrhea can also cause increased potassium loss. It is frequently observed in calves, but also adult cows can suffer from diarrhea, following indigestion with energetic and metabolic imbalances.
Experiment 1: reduced dry matter intake
The results of reducing DMI to 0 g/h after 100 h are presented in Fig. 2. Figure 2a shows the components \(K_{ECF}\) and \(Gluc_B\). Hypokalemia occurs at time \(t = 155\) h, hypoglycemia at time \(t = 523\) h. Figure 2b shows that \(K_{TISS}\) decreases towards its lower bound of about 1444 g, and that the urinary excretion with \(K_{URIN}\) is reduced but ongoing. In Fig. 2c, experimental data from Clabough and Swanson36 are presented together with the simulation results of \(K_{ECF}\). Clabough et al.36 studied six non-pregnant, non-lactating Holstein cows, fasted for 48 h. They measured mean serum potassium values before and after 48 h of fasting being 4.9 and 4.3 mmol/L. The simulated dynamics in experiment 1 and the experimental data from Clabough and Swanson36 match very well. In another study, plasma potassium in beef steers fasted for up to four days fell from 4.1 to 3.7 mmol/L37. Compared to the simulation results, the relatively smaller decline in steers over a longer fasting period may be due to the fact that steers have more muscle mass and hence more potassium storage capacity.
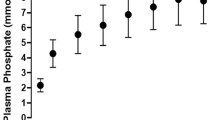
Experiment 2: reduced potassium content in feed
Experiment 2: We observe reduced potassium intake by decreasing \(K_{FEED}\) from its default value of 133 g/day to 13 g/day. With decreasing \(K_{FEED}\), \(K_{ECF}\) (pink, in mmol/L) and \(K_{ICF}\) (green, in mmol/L) decrease as well. For the lowest experimental value \(K_{FEED}=13\) g/day, hypokalemia occurs after 35 h.
In Fig. 3a, \(K_{FEED}\) is lowered from its default value of 133 g/d to 13 g/day. With decreasing potassium intake, \(K_{ECF}\) and \(K_{ICF}\) are decreasing as well. However, as it is visible from the simulations, extracellular potassium levels decrease only slightly, whereas the decrease in intracellular potassium is much more pronounced, which nicely illustrates the buffering function. For \(K_{FEED}=13\) g/day, hypokalemia occurs after 35 h.
Since ruminants’ diet is generally rich in potassium, a deficient diet in vivo is challenging to prepare23. Nevertheless, Pradhan and Hemken23 managed to perform experiments with potassium deficient diets in lactating dairy cows. In their study, diets with a potassium content of 0.06% and 0.15% were fed to lactating cows. Clinical symptoms such as floor licking, changes in skin and hair appeared after 3–4 weeks of deficient diet. Unfortunately, the authors only state one mean experimental measurement of serum potassium per cow for the studied period. The mean serum potassium values range from 3.5 mmol/L to 5.1 mmol/L in the 0.06% diet group, and from 4.5 mmol/L to 6.9 mmol/L in the 0.15% diet group. For comparison with experiment 2, we calculated the potassium content in DMI on the basis of the default DMI (11.7 g) to be 7 g and 17 g for the 0.06% and 0.15% diet group, respectively. In the simulations with \(K_{FEED}=13\) g/day and 40 g/day, the mean values of \(K_{ECF}\) over 300 hours were calculated to be 3.24 mmol/L and 4.13 mmol/L, respectively, the minimum values are 1.79 mmol/L and 3.01 mmol/L. The results, however, are difficult to compare since most of the stated serum potassium values in Pradhan and Hemken23 are above the hypokalemic threshold even though clinical symptoms are reported. This can possibly be attributed to an imprecise potassium assay technique back then and the fact that only one mean value for the whole study period is reported.
Experiment 3: increased potassium excretion with urine
Figure 4a shows the model dynamics resulting from a twofold increase of the rate for urinary potassium excretion, KeKu. We observe that \(K_{ICF}\) and \(K_{ECF}\) are initially decreasing rapidly and then stabilize at lower values. Hypokalemic values for \(K_{ECF}\) are reached within 17 h after the start of the experiment. Glucose in the blood and insulin stay within their physiological ranges. Figures 4,b,c show the dynamics of \(K_{ICF}\) and \(K_{ECF}\) when the rate KeKu is increased up to the fourfold of its default value. With an increasing rate KeKu, \(K_{ECF}\) and \(K_{ICF}\) decrease faster at the beginning and then remain stable at lower values throughout the simulation period. Figure 4d shows the difference between \(K_{URIN}\) in the default condition and \(K_{URIN}\) at the fourfold increased rate KeKu. This difference rapidly increases within the first 24 h and then starts oscillating between 27 and 33 g. The trend in the predicted urinary excretion with potassium agrees with the observation in St. Omer and Roberts22: the higher the potassium content in the diet, the more potassium is excreted with urine. The renal excretion of potassium with \(K_{URIN}\) in the model is not related to other minerals or acid base components, as it is crucial in vivo. Hence, the numerical experiments explore the quantitative dynamics solely inside the potassium network. Simulations mainly predict that increased urinary potassium excretion with \(K_{URIN}\) finally leads to depletion of \(K_{ECF}, K_{ICF}\), and \(K_{TISS}\).
Experiment 4: increased potassium excretion with milk
With increasing milk production, the values for intra- and extracellular potassium content, \(K_{ECF}\) and \(K_{ICF}\), decrease and stabilize at lower values (Fig. 5a). The blood glucose, \(Gluc_B\), is maintained within its physiological limits until stores are empty (Fig. 5b). For 48 L milk production per day, hypokalemic values of \(K_{ECF}\) can be observed after 9 h. Values of \(Gluc_B\) are hypoglycemic right from the beginning but recover until the stores are empty after 102 h. Since the model does not allow for varying potassium content in milk, milk increase leads to early hypokalemia.
Redistribution
Changes in blood pH or medications can increase the shift of potassium from extracellular to intracellular space. The results of the corresponding numerical experiments are discussed in the following.
Experiment 5: acidosis, alkalosis
Figure 6 shows the dynamics of the model components \(K_{ECF}\), \(K_{ICF}\), and pH during the experiments. When the model parameter \(p_{85}\) is set to \(p_{85}=\{7.2,\,7.35,\,7.5,\,7.65,\,7.8\}\), this leads to mean pH values of 7.05, 7.2, 7.35, 7.5, and 7.65, respectively. With increasing pH, also \(K_{ICF}\) increases, whereas the acid-base variations in the numerical experiments do not have any effect on extracellular potassium levels \(K_{ECF}\) (Fig. 6a). The latter is in contradiction to experimental findings in humans9, and hence probably also in contradiction to what is happening in cows. Rastergar and Soleimani9 describe the behaviour of potassium under changing pH conditions in humans. They observed that for each 0.1 unit change in pH, there is a change of approximately 0.6 mmol/L serum potassium, varying greatly by the nature of the acid-base disorder. In a recent study of cows with left displaced abomasum, Ismael et al.38 observed alkalic blood pH values and hypokalemic potassium values (mean values in affected cows). It seems that the mechanisms describing the acid-base metabolism in the model are not sophisticated enough to have an effect on \(K_{ECF}\). More precisely, pH influences the rate KeKi more than the rate KiKe. In addition, the effect parameter \(p_{21}\) is too small to have an appropriate effect on the rate KiKe.
Experiment 6: increased insulin
In the simulated hyperglycemic clamp the model component \(Gluc_B\) is manually set to 1.2 at time \(t=150\) h for a duration of 50 h. As a consequenc, insulin increases and also the rate of potassium shift from extra- to intracellular space, KeKi. Hence, we observe an increase in the component \(K_{ICF}\) (Fig. 7a) and a decrease in \(K_{ECF}\) (Fig. 7b). All components return to their previous levels after the end of the experiment without further intervention.
We compare the simulation results with measurements from Grossen-Rösti et al.39, who studied hyperglycemic clamp dynamics in 11 dairy cows at different times around parturition. The authors report a steady state glucose concentration between 1.07 and 1.12 g/L, which is comparable with the simulated steady state of \(Gluc_B = 1.2\) g/L in our model. In the study, insulin was measured before the beginning of manipulation as less than 20 \(\upmu\)U/mL. Insulin rose up to 140 \(\upmu\)U/mL and 78 \(\upmu\)U/mL in non-lactating pregnant cows and in postpartum lactating cows, respectively, while glucose was in the steady state clamp condition. In the simulation, insulin increases to a maximum of 48 \(\upmu\)U/mL. This means that the insulin increase due to blood glucose increase is less pronounced in the model compared to the experimental measurements from Grossen-Rösti et al.39.
The authors in DeFronzo et al.26 studied potassium shift due to a HGC in 29 humans. In the HGC condition the mean serum potassium decreased by \(0.54\pm 0.04\) mmol/L. In the model simulation, the 24 h mean value of \(K_{ECF}\) before the start of the experiment was 4.36 mmol/L, and it decreased to a 24 h mean of 4.31 mmol/L during HGC, with a minimal value of 3.59 mmol/L. This average decrease of 0.05 mmol/L during HGC is very small compared to the study26. This can be attributed to the oscillatory dynamic behavior of potassium in the model. The difference in serum potassium between feed intake and fasting is increased during HGC, while maximum peak concentrations decrease only slightly.
Experiment 7: dexamethasone administration
Upon dexamethasone administration, the glucose level in blood, \(Gluc_{B}\), rises, followed by a rise in insulin (Fig. 8a). Insulin enhances the rate for potassium transport from extra- to intracellular space, KeKi. This potassium shift to the intracellular space is visible in the simulation result as an increase in \(K_{ICF}\) (Fig. 8a). Coffer et al.29 studied the effect of a single dose of 20 mg dexamethasone in seven cows between days 20–25 of lactation. They report the mean values of blood glucose and serum potassium in their Figs. 1 and 3, from where we extracted the following values for comparison with our simulation results. Glucose blood concentrations increased from an average of 0.48 g/L (mean of the seven studied cows) before dexamethasone administration by 0.44 g/L up to a maximum value of 0.92 g/L at 24 h after drug administration. Note, however, that the authors measured only every 24 h such that the peak concentration could have occurred at any time between \(t=0\) and \(t=48\) h. In the model simulations, the maximum value \(Gluc_B=0.91\) g/L is reached seven hours after drug administration (Fig. 8a). Compared to the value \(Gluc_B=0.59\) g/L attained 24 h before administration, this corresponds to an increase of 0.32 g/L in the model. In the study by Coffer et al.29, serum potassium levels increased very little after dexamethasone administration and decreased towards the pre-treatment value within 24 h after treatment. In the simulation, we observe a very small decrease in extracellular potassium down to a minimum of \(K_{ECF}=3.8\) mmol/L four hours after drug administration (Fig. 8b). This decrease is caused by the increase in blood glucose, \(Gluc_B\), which causes an increase in insulin and hence an increase in the rate of potassium shift from extra- to intracellular space, KeKi. This difference in qualitative behavior could hint to the fact that the effect parameter \(p_{74}\) needs to be adapted in a more sophisticated manner. For this purpose, however, time series data would be needed.
On the other hand, there is good quantitative agreement with a measurement value reported in Kojouri et al.31. In this case study about atrial fibrillation and hypokalemia, the authors report a serum potassium value of 3.5 mmol/L after dexamethasone administration in a postpartum cow.
Conclusion and outlook
We have illustrated that the model for potassium balance in dairy cows can be used to simulate the dynamics of hypokalemia for a number of scenarios described in literature. In most cases, model simulations agree qualitatively, in some cases even quantitatively, with clinical studies. To obtain these results, only minor modifications needed to be made on the original model. This demonstrates the capability of our model to evolve and be used beyond its original purpose, i.e., its extensibility and reusability.
We have also identified some mismatches between model simulations and results from literature. Some of these mismatches can be attributed to imprecise data reported in literature, e.g. imprecise potassium assay techniques or lack of information about measurement time w.r.t. last feed intake. The latter is important because there are fluctuations in potassium levels depending on the time of feed intake, which is also visible in our model simulations. In addition, the definition of hypokalemia is inconsistent. The feasibility of the threshold \(K_{ECF}=3.9\) mmol/L cannot be evaluated with our simulations because the numerical experiments neither included treatment nor correlated symptoms with plasma values of potassium. Other mismatches between model simulations and data are due to insufficiencies in the potassium balance model, for example in the mechanisms describing the acid-base metabolism. Further adjustments of model equations and parameters based on experimental time-series data are needed to make the model even more reliable in future.
A previous review on hypokalemia in cattle3 points out the importance of considering extra- and intracellular potassium dynamically to evaluate more precisely the whole body situation with respect to clinical assessment and prognosis of the patient. Hence, we believe that further research on this topic can benefit from a model-based approach. For example, experiments on hyperkalemia and the treatments of hypo- and hyperkalemia could be simulated in silico. Furthermore, one could include sodium in order to study more precisely the intra- and extracellular shifts and renal excretion mechanisms.
Finally,the model may be used in teaching and research situations in which knowledge of potassium (or other nutrient) metabolism is important, but in which there is truly no need to go to the expense of repetitive animal experimentation. We hope that this type of modeling will make it possible to test new therapeutic approaches in silico first, thus filtering out the most promising approaches before carrying out experiments on animals. In that way, modeling and simulation are useful tools for the reduction, refinement and replacement of animal experiments40,41.
Data availibility
All data generated or analysed during this study are included in this published article and its supplementary information files.
Code availibility
Accession codes: The code for the updated model is available from the BioModels database: https://www.ebi.ac.uk/biomodels/MODEL2201250001. The software to run the model can be downloaded from http://www.celldesigner.org
References
Andronic, J. et al. Identification of two-pore domain potassium channels as potent modulators of osmotic volume regulation in human T lymphocytes. Biochimica Biophysica Acta BBA Biomembranes 1828, 699–707 (2013).
Bobak, N. et al. Volume regulation of murine T lymphocytes relies on voltage-dependent and two-pore domain potassium channels. Biochimica Biophysica Acta BBA Biomembranes 1808, 2036–2044 (2011).
Sattler, N. & Fecteau, G. Hypokalemia syndrome in cattle. Vet. Clin. N. Am. Food Anim. Pract. 30, 351–7 (2014).
Sweeney, R. Treatment of potassium balance disorders. Vet. Clin. N. Am. Food Anim. Pract. 15, 609–617 (1999).
Goff, J. P. Macromineral physiology and application to the feeding of the dairy cow for prevention of milk fever and other periparturient mineral disorders. Anim. Feed Sci. Technol. 126, 237–257 (2006).
Constable, P., Grünberg, W., Staufenbiel, R. & Stämpfli, H. R. Clinicopathologic variables associated with hypokalemia in lactating dairy cows with abomasal displacement or volvulus. J. Am. Vet. Med. Assoc. 242, 826–835 (2013).
Medical Clinic, University of Leipzig. Laboratoy Reference Values. http://www.vetmed.uni-leipzig.de/ik/wmedizin/labor/diagnostik/referenzwerte/rind.htm (2018).
Peek, S. F., Divers, T. J., Guard, C., Rathe, A. & Rebhun, W. C. Hypokalemia, muscle weakness, and recumbency in dairy cows. Vet. Ther. 1, 235–244 (2000).
Rastergar, A. & Soleimani, M. Hypokalaemia and hyperkalaemia. Postgrad. Med. J. 77, 759–764 (2001).
West, J. W. Nutritional strategies for managing the heat-stressed dairy cow. J. Anim. Sci. 77, 21–35 (1999).
Sattler, N., Fecteau, G., Girard, C. & Couture, Y. Description of 14 cases of bovine hypokalaemia syndrome. Vet. Record 143, 503–507 (1998).
Bannink, A., Spek, W. J., Dijkstra, J. & Šebek, L. B. J. A Tier 3 method for enteric methane in dairy cows applied for fecal N digestibility in the ammonia inventory. Front. Sustain. Food Syst. 2, 66 (2018).
McNamara, J., Huber, K. & Kenéz, A. A dynamic, mechanistic model of metabolism in adipose tissue of lactating dairy cattle. J. Dairy Sci. 99, 5649–5661 (2016).
Boer, H. et al. A simple mathematical model of the bovine estrous cycle: Follicle development and endocrine interactions. J. Theor. Biol. 278, 20–31 (2011).
Woelders, H., te Pas, M. F. W., Bannink, A., Veerkamp, R. F. & Smits, M. A. Systems biology in animal sciences. Animal 5, 1036–1047 (2011).
Suravajhala, P., Kogelman, L. & Kadarmideen, H. Multi-omic data integration and analysis using systems genomics approaches: Methods and applications in animal production, health and welfare. Genet. Sel. Evol. 48, 1–14 (2016).
Mader, A. H., Wupper, H. & Boon, M. The construction of verification models for embedded systems. Technical Report No. TR-CTIT-07-02 (Institution University of Twente, Netherlands, 2007).
Berg, M., Plöntzke, J., Leonhard-Marek, S., Müller, K. E. & Röblitz, S. A dynamic model to simulate potassium balance in dairy cows. J. Dairy Sci. 100, 9799–9814 (2017).
Plöntzke, J. et al. Modeling potassium balance in dairy cows. Technical Report No. 13-09 (ZIB, Takustr, Berlin, 2013).
Berg, M., Plöntzke, J., Leonhard-Marek, S., Müller, K. E. & Röblitz, S. SBML code of the potassium balance model. BioModels database. https://www.ebi.ac.uk/biomodels/MODEL1710230000 (2017).
National Research Council. Nutrient Requirements of Dairy Cattle: Seventh Revised Edition (The National Academies Press, Washington, DC, 2001).
Omer, V. & Roberts, W. Some effects of dietary potassium upon digestibility, serum electrolytes and utilization of potassium, sodium, nitrogen and water in heifers. Can. J. Anim. Sci. 47, 39–46 (1967).
Pradhan, K. & Hemken, R. Potassium depletion in lactating dairy cows. J. Dairy Sci. 51, 1377–1381 (1968).
Sattler, N., Fecteau, G., Couture, Y. & Tremblay, A. Determination of the potassium balances in diary cows and the examination of daily and lactation period-associated variations. Can. Vet. J. 42, 107–115 (2001).
Owens, F., Secrist, D., Hill, W. & Gill, D. Acidosis in cattle: A review. J. Anim. Sci. 76, 275–286 (1998).
DeFronzo, R. A., Felig, P., Ferrannini, E. & Wahren, J. Effect of graded doses of insulin on splanchnic and peripheral potassium metabolism in man. Am. J. Physiol. Endocrinol. Metab. 238, E421–E427 (1980).
CliniPharm. Dexamethasone. http://www.vetpharm.uzh.ch/wir/00000005/0022__F.htm (2018).
Shpigel, N., Chen, R., Avidar, Y. & Bogin, E. Use of corticosteroids alone or combined with glucose to treat ketosis in dairy cows. J. Am. Vet. Med. Assoc. 208, 1702–1704 (1996).
Coffer, N. J., Frank, N., Elliott, S. B., Young, C. D. & van Amstel, S. R. Effects of dexamethasone and isoflupredone acetate on plasma potassium concentrations and other biochemical measurements in dairy cows in early lactation. Am. J. Vet. Res. 67, 1244–1251 (2006).
Bughio, S., Qureshi, T., Daraghmah, E., Malhi, M. & Tunio, A. Evaluation of clinical and blood biochemical effects of dexamethasone in goat species. Pak. J. Agric. Agric. Eng. Vet. Sci. 31, 298–307 (2015).
Kojouri, G. A., Samani, R. E. & Yousefi, A. Atrial fibrillation associated with dexamethasone in dairy cattle. Comp. Clin. Pathol. 26, 1413–1416 (2017).
Toutain, P., Brandon, R., Alvinerie, M., Garcia-Villar, R. & Ruckebusch, Y. Dexamethasone in cattle: Pharmacokinetics and action on the adrenal gland. J. Vet. Pharmacol. Ther. 5, 33–43 (1982).
Stötzel, C., Plöntzke, J., Heuwieser, W. & Röblitz, S. Advances in modeling of the bovine estrous cycle: Synchronization with pgf2\(\alpha\). Theriogenology 78, 1415–1428 (2012).
Ungemach, F. Pharmaka zur Beeinflussung von Entzündungen, vol. 6 (Parey Buchverlag, IM Blackwell Verlag GmBH, Berlin, 2003). ISBN: 3-8263-3450-7.
Huang, C.-L. & Kuo, E. Mechanism of hypokalemia in magnesium deficiency. J. Am. Soc. Nephrol. 18, 2649–2652 (2007).
Clabough, D. L. & Swanson, C. R. Heart rate spectral analysis of fasting-induced bradycardia of cattle. Am. J. Physiol. Regul. Integr. Comp. Physiol. 257, R1303–R1306 (1989).
Smith, S. & Prior, R. Metabolic responses to fasting and alloxan-induced diabetes mellitus in steers. Am. J. Vet. Res. 45, 1829–1834 (1984).
Ismael, M. M., Elshahawy, I. I. & Abdullaziz, I. A. New insights on left displaced abomasum in dairy cows. Alex. J. Vet. Sci. 56, 127 (2018).
Grossen-Rösti, L., Kessler, E. C., Tröscher, A., Bruckmaier, R. & Gross, J. J. Hyperglycaemia in transition dairy cows: Effects of lactational stage and conjugated linoleic acid supplementation on glucose metabolism and turnover. J. Anim. Physiol. Anim. Nutr. 102, 483–494 (2018).
Lang, A. et al. In silico methods—Computational alternatives to animal testing. Altex 35, 124–126 (2018).
Madden, J. C., Enoch, S. J., Paini, A. & Cronin, M. T. A review of in silico tools as alternatives to animal testing: Principles, resources and applications. Altern. Lab. Anim. 48, 146–172 (2020).
Acknowledgements
This work was partially supported by the German Federal Ministry of Education and Research (BMBF). JP and MB obtained funding from the BMBF project BovSys (Grant FKZ031A311). SR obtained funding from Trond Mohn Foundation (Grant BFS2017TMT01).
Author information
Authors and Affiliations
Contributions
J.P. designed the model and the experiments, performed experiments, wrote the manuscript. M.B. implemented the model and the experiments, performed experiments, wrote the manuscript. R.E. implemented and executed the dexamethasone experiment. S.L.M. supported the design of the model mechanisms and the experiments. K.E.M provided the clinical data for the model development. S.R. provided funding, supported the design and implementation of the model, and wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Plöntzke, J., Berg, M., Ehrig, R. et al. Model-based exploration of hypokalemia in dairy cows. Sci Rep 12, 19781 (2022). https://doi.org/10.1038/s41598-022-22596-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-22596-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.