Abstract
Regardless of treatment, the clinical progression of neurofibromatosis type 2 (NF2), particularly in terms of hearing, swallowing, and gait, tend to worsen throughout the patients’ lives. We performed a retrospective analysis of functional outcomes in Japanese NF2 patients to predict their functional prognosis. We analyzed genotype–phenotype correlation based on genetic data from a cohort of 57 patients with a mean follow-up of 14.5 ± 6.0 years. Their functional outcomes, including hearing, swallowing, and ambulation, were reviewed. Performing a targeted deep sequencing, germline NF2 mutations were identified in 28 patients (49.1%), and mosaic NF2 was identified in 20 patients (20, 35.0%). The functional preservation period and outcome differed significantly depending on clinical/genetic factors. Among these factors, “Truncating”, “Mosaic”, and “Age of symptom onset ≥ 25” had the most significant effects on functional disability. By applying a combination of an NF2 mutation type/location, and age of symptom onset, we classified different degrees of functional preservation and progression, schwannoma growth rate and total interventions per year per patient. The prediction of detailed functional outcomes in NF2 patients can plan better strategies for life-long disease management and social integration.
Similar content being viewed by others
Introduction
Neurofibromatosis type 2 (NF2) is a tumour predisposition syndrome with the autosomal-dominant transmission, complete penetrance, and variable phenotypic expression caused by germline alterations in the tumour suppressor gene NF21,2,3. Patients with NF2 develop uni- or bilateral vestibular schwannomas (UVS, BVS), intracranial and/or multiple spinal schwannomas, as well as multiple meningiomas1. The clinical diagnosis of NF2 is based on the Manchester criteria4, which are (1) BVS, or (2) family history and UVS, or (3) family history or UVS and two of: meningioma, cataract, glioma, neurofibroma, schwannoma, cerebral calcification (if UVS + ≥ 2 schwannomas only need negative LZTR1 test), or 4) multiple meningioma (2 or more) and two of: UVS, cataract, glioma, neurofibroma, schwannoma, cerebral calcification, and or (5) Constitutional pathogenic NF2 gene variant in blood or identical in two tumours (Supplementary Table 1).
Patients commonly experience hearing loss, swallowing difficulties, and gait abnormalities, with many interventions required to control the progression of numerous tumors1,2,3, significantly interfering with their daily life. Despite the availability of systematic and multimodal treatments, the symptoms associated with NF2 tend to worsen throughout the patients’ lives1,2,3.
Several retrospective studies on NF2 have reported genotype–phenotype correlations as predictors of disease progression and mortality5,6,7,8,9,10,11. The resulting clinical predictors have included age of symptom onset and the presence of intracranial meningioma5,7,12; whereas, the genetic predictions of mortality included truncating and splicing mutations at the 5'-end of the NF2 gene5,6,11. Missense mutations, somatic mosaicism, and splicing at the 3'-end of the NF2 gene appeared to have the opposite effect5,6,13. Recently, Halliday et al. proposed a genetic severity score with germline mutation types and locations to predict mortality based on the number of tumours and clinical interventions14.
However, it is not only longevity but also the quality of life (QOL) and activities of daily living (ADL) with persisting symptoms that must be considered when considering development treatment strategies. To date, a limited number of studies have reported genotype–phenotype correlations as predictors of detailed functional prognosis in NF2 patients15,16,17. Moreover, the number of articles about NF2 in the Asian population is also limited12,18,19,20,21. Thus, to improve the clinical care of NF2 patients and early predict their functional prognosis, we used retrospective genetic analysis with target deep sequencing focused on the functional outcomes of Japanese NF2 patients.
Results
Clinical characteristics
All 57 patients (24 men and 33 women) whose blood samples were obtained fulfilled the Manchester Clinical Diagnostic Criteria for NF24. Age of symptom onset ranged from 4 to 61 years (mean 25.5 ± 13.3) (Table 1). Specific lesions were as follows: vestibular schwannoma (bilateral: 84.2%, unilateral: 15.7%), intracranial meningiomas (56.1%), other cranial nerve schwannomas (47.3%), spinal schwannoma (64.9%), spinal ependymoma (22.8%), ocular lesion (22.8%), and cutaneous lesions (50.8%) (Table 1). Only four patients (7%) had a family history of NF2.
Functional/survival outcomes
Among the 57 patients, the Karnofsky Performance Scale (KPS) score of 18 (31.5%) patients were less than 40. Although 31 patients (54.3%) maintained useful hearing, the rest already had disabled hearing or deafness at presentation. Regarding swallowing function, 14 patients (24.5%) already presented “Tube feeding.” Lastly, 17 patients (29.8%) already showed “Wheelchair-bound or bedridden” in gait function. Fifty-five patients were alive at the end of 2019.
Mutation analysis
Germline NF2 mutations were identified in 28 patients (49.1%), including truncating mutations (12, 21.0%), large deletions (4, 7.0%), splice site mutations (9, 15.7%), and missense mutations (3, 5.2%). Mosaic NF2 was identified in 20 patients (35.0%) (mosaic truncating mutation (16, 28.0%), mosaic in–frame deletion (1, 1.7%), and mosaic missense mutations (3, 5.2%) (Tables 1, 2; Supplementary Table 2).
Genotype–phenotype correlation using the Kaplan–Meier method and univariate/multivariate Cox proportional hazards model
The periods of functional outcome preservation differed statistically significantly (log-rank test: p < 0.001) depending on the type of NF2 mutation (Fig. 1; supplementary Fig. 1). Univariate and multivariate Cox proportional hazards models examining the effects of all clinical/genetic factors on functional disability were performed for all patients (Supplementary table 3–6). “Truncating” (HR 3.97, 95% CI 1.28–12.25, p = 0.016) and “Mosaic” (HR 0.09, 95% CI 0.01–0.76, P = 0.027) had significant effects on KPS ≤ 40 (Supplementary table 3). For “disabled hearing or deafness”, “Truncating” (HR 11.61, 95% CI 1.77–75.85, p = 0.01), “Splice site” (HR 5.65, 95% CI 1.02–31.14, p = 0.046) and “Age of symptom onset ≥ 25” (HR 0.01, 95% CI 0.0006–0.17, p = 0.001) were significant predictors (Supplementary table 4).
Progression of functional disability and schwannoma growth rate
The line plotting the progression of functional disability throughout each patient’s life (Fig. 2) showed significant differences for each mutation type and age of symptom onset. The difference was evident by statistically comparing the line plots’ gradients (Supplementary Fig. 2). The schwannoma growth rate was also found to differ significantly depending on the type of mutation and “Age of symptom onset ≥ 25” (Supplementary Fig. 2).
Progression of the functional disability (ADL score) of NF2 patients according to each of the five NF2 mutation types (“Truncating”, “Large deletion”, “Splice site”, “Missense”, “Mosaic”) and age of symptom onset. To evaluate the progression of functional disability of each NF2 patient, we registered the total ADL score (0–7, death = 8) of each against age and created line graphs plotting the progression of functional disability throughout their life (x-axis: age, y-axis: total ADL score). Dotted line: average of gradients, denoting the speed of ADL progression using a linear functional approximate expression of the line graph.
Our classification by applying a combination of an NF2 mutation type/location, and age of symptom onset
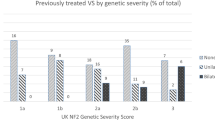
According to Halliday’s genetic severity score14 and our results, we classified our cohort into three classes (mild, moderate, or severe) based on the NF2 mutation types, NF2 mutation location, and age of symptom onset (Fig. 3). Comparing the three classes, each class (mild, moderate, severe) was significantly different, with shorter or longer periods of functional preservation for each type of functional disability. There was also a significant difference among the gradients to the progression of the ADL score, the schwannoma growth rate, and total interventions/year (Fig. 3).
NF2 functional prognostic grade at diagnosis. 3A: The NF2 functional prognostic grading scale classified patients into three grades (mild, moderate, and severe) based on the NF2 mutation types, NF2 mutation location, and age of symptom onset (statistical analysis and significance are detailed in the main text). 3B-3E: Kaplan–Meier curves of each functional prognostic grade for KPS, hearing, swallowing, and gait. 3F-3H: A boxplot depending on each functional prognostic grade shows the relationship between ADL score progression, schwannoma growth rate, and total interventions/year. This grading system indicates the different functional disabilities and the different biological tumour behaviours for each grade.
Representative cases diagnosed using Manchester’s NF2 criteria are shown in Fig. 4. Case 1 was classified as “severe” (Fig. 4, case 1). In middle childhood, she underwent left meningioma surgery, presenting dysphagia and hoarseness in another hospital. During early adolescence, the patient was referred to us. Her MRI showed bilateral vestibular schwannomas, bilateral trigeminal schwannomas (Lt. SDS: 60%, Rt. SDS: 100%). Afterwards, the annual follow-up indicated gradual hearing deterioration (Lt. SDS: 50%, Rt. SDS: 50%). In her early 20 s, she finally lost hearing function. Furthermore, the patient developed severe dysphagia and gait disturbance. Eventually, she underwent a tracheostomy and became wheelchair-bound. Since the age of disease onset, she underwent 17 interventions, including tumour resections, radiosurgery, ventriculoperitoneal shunt, tracheostomy, and abscess removal.
Representative cases of NF2 functional prognostic grading system. Case 1: NF2 functional prognostic grade “severe” (Truncating: p.Glu194Sfs*15, Exon 6, age of symptom onset = in middle childhood). Case 2: NF2 functional prognostic grade “moderate” (Large deletion, exon 15, age of symptom onset = in her mid-20 s). Case 3: NF2 functional prognostic grade “mild” (mosaic: VAF 7.2%, p.Glu392*, exon 12, age of symptom onset = in her early 30 s).
Case 2 was classified as “moderate” (Fig. 4, case 2). She had a family history of NF2. In her late 30 s, she was referred to us for right vestibular schwannoma surgery, with already impaired right hearing function (Lt. SDS: 60%, Rt. SDS: 100%). After tumour resection, the annual follow-up indicated gradual hearing deterioration. In her mid–40 s, the patient finally presented a bilateral loss of useful hearing (Lt. SDS: 10%, Rt. SDS: 20%). At present, the patient presents gait disturbance due to brain stem compression due to a growing right trigeminal schwannoma.
Case 3 was classified as “mild” (Fig. 4, case 3). She underwent resection of a right vestibular schwannoma with initial hearing impairment in her early 30 s. After tumour resection, she lost right useful hearing (Lt. SDS: 100%, Rt. SDS: 0%). In her early 40 s, she has referred again for recurrence of the operated tumour treated with radiosurgery, but she had stable left useful hearing (Lt. SDS: 80%, Rt. SDS: 0%). In her early 50 s, the patient had useful hearing with stable schwannomas on the yearly MRI (Lt. SDS: 80%, Rt. SDS: 0%).
Discussion
Given recent improvements in these patients’ prognoses due to the development of more effective treatment procedures5, the issues of ADL maintenance and the effect of persisting symptoms on patient QOL are becoming increasingly important. We analyzed the clinical and genetic predictors of the functional disability of NF2 patients. Two types of mutations were found to act as predictors, namely “Truncating” and “Mosaic”, in addition to “Age of symptom onset ≥ 25”. Consequently, we showed that patients of “Mild” had different functional prognoses compared with other NF2 patients (Figs. 3, 4).
In terms of the prediction of outcomes in NF2 patients, Halliday’s genetic severity score based on the type and location of germline mutations has been known14. Characteristically, their genetic severity score included site and degree in not only germline NF2 alteration but also mosaicism14. For clinical use, they suggested three groups: “1: Tissue mosaic,” “2: Classic,” and “3: Severe”14. In particular, their genetic severity score distinguished mosaic in the blood (subcategory: 2A(Mild), 2B(Moderate)) from tissue mosaic (subcategory: 1B)14. However, when Halliday’s genetic severity score was applied in our cases, it did not work well (Supplementary Fig. 3). In particular, the Kaplan–Meier curves for functional disabilities showed that subcategory 2A was worse than the 2B group subcategory (Supplementary Fig. 3). Furthermore, the latest report showed no significant survival difference between 2A(Mild) and 2B(Moderate) in Halliday’s genetic severity score22. We performed targeted deep sequencing for multiple tissue DNA to detect a low variant allele frequency (VAF) NF2 variant. Many mosaic NF2 in our cases, which are assumed to include subcategory 1B in previous genetic severity score, were included in subcategory 2B because most mosaic cases were detected in exon 2–13 (2A: exon 14,15 mosaic, 2B: exon 2–13 mosaic)14. Consequently, the Kaplan–Meier analysis showed that the functional outcome of group 2B was milder than that of group 2A. Considering this situation and our results, we emphasized the meaning of “Truncating” as a predictor for worsening functional outcomes and the importance of “Mosaic” as a predictor for slower functional disability.
Nine patients present without any NF2 alteration (Supplementary Table 7). Interestingly, some patients of these nine patients present with a similar phenotype to that of the patient with a pathogenic NF2 variant. Others also show the older onset age, UVS and multiple schwannomas (they have no mutation with LZTR1 by WES). We have already performed Sanger sequence, MLPA, whole exome sequence, and targeted deep sequencing for these nine patients, but we could not identify any germline or low variant frequency NF2 alteration, LZTR1, and SMARCB1 mutation. We will perform whole-genome sequences and long-read sequences in future.
This was a retrospective study with a relatively small number of enrolled NF2 patients (n = 57). And the relatively homogeneous genetic background may influence our evaluation. Our classification did not include the degree of mosaicism compared with Halliday’s genetic severity score. Hence, more patients from abroad should be recruited in the future to assess the clinical utility of our classification considering the degree of mosaicism. We thought that our main characteristics of this study were “Asian cohort”, “high rate of detected mosaic NF2 with targeted deep sequencing”, and “detailed functional outcome”.
Even if we performed mutational analysis of multiple normal tissue DNA to compensate for limited read depth, distinguishing between a true variant and error could be still problematic. Furthermore, the phenotype of mosaic cases is known as highly variable23. Identified mosaic cases are more severely affected and more likely to have presented with classical bilateral VS23. Considering the variation of the phenotype in mosaic NF2 and the accuracy of detecting mutation, diagnosing and utilising mosaic NF2 remains a limitation.
This study performed genotype–phenotype correlation analysis for the early prediction of functional prognosis in Japanese NF2 patients. By applying a combination of an NF2 mutation type/location, and age of symptom onset, we classified different degrees of functional preservation and progression, schwannoma growth rate and total interventions per year per patient. The prediction of detailed functional outcomes can be used to plan better strategies for life-long disease management and social integration.
Materials and methods
All methods were carried out in accordance with relevant guidelines and regulations.
Patient population
The data of eighty-five patients with an established diagnosis of NF2 according to Manchester’s NF2 criteria4 at The University of Tokyo Hospital and the Tokyo Metropolitan Tama Medical Center from 2000 to 2019 were used in our analysis. We retrospectively analyzed the clinical data, imaging studies, operative findings, and functional outcomes obtained from our hospital clinical database and existing medical records. We performed a patient interview directly in the outpatient clinic (37 patients) or by phone (20 patients). Twenty-eight patients were excluded because of incomplete clinical data. The remaining 57 patients attended our outpatient clinics at least once a year and performed the diagnostic and treatment procedures when required. These 57 patients included 53 de novo NF2 patients reported in our previous study21. The average follow-up period was 14.5 ± 6.0 years. All patients underwent complete neurological evaluation and hearing tests, including audiogram before and after surgery and at each follow-up visit. Imaging evaluation was performed with MRI preoperatively and postoperatively and annually thereafter.
Mutation analysis and bioinformatics analysis
DNA of NF2 patients was obtained from their peripheral blood leucocytes, buccal swabs, hair follicles, and tumour samples. As previously described, mutation analysis of NF2 (GenBank accession number, NM_000268.4) was performed, including direct Sanger sequencing, multiple ligation-dependent probe amplification (MLPA), and target deep next-generation sequencing. Sequencing reads were aligned to the human genome (hg19).
As mosaic NF2 has been previously defined (supplementary Table 1)21, proven mosaic NF2 was considered confirmed when NF2 variant with low VAF was detectable (1) in blood, (2) in both buccal and hair DNA but not in blood, and (3) detection of NF2 variant in two independent tumour DNA samples. Data analysis of the target deep sequence was performed as previously described21.
Evaluation of functional disability progression in NF2 patients
Functional disability in the NF2 patients was evaluated using KPS score and our new ADL scoring system (Fig. 2). This system was composed of three major functional scales, based on “hearing” (score 0–2), “swallowing” (score 0–2), and “gait” (score 0–3). Assessments were performed in patient interviews, establishing when and how these major functions were impaired, either directly in the outpatient clinic (37 patients) or by phone (20 patients). “Hearing” was classified as “asymptomatic” (Gardner-Robertson Hearing Scale Grade I) (score: 0), “useful hearing” (Gardner-Robertson Hearing Scale Grade II) (score: 1), “disabled hearing (Gardner-Robertson Hearing Scale Grade III, IV, V) or deafness” (score: 2). We classified “swallowing” into “asymptomatic” (score: 0), “possible oral feeding (a patient report of some difficulty with swallowing sufficient)” (score: 1), and “tube feeding” (score: 2). “Gait” was scored as “asymptomatic” (score: 0), “able to walk without assistance (a patient report of some difficulty with walking sufficient)” (score: 1), “able to walk with assistance” (score: 2), and “Wheelchair-bound or bedridden” (score: 3). To evaluate the progression of functional disability in each NF2 patient, we registered the total ADL score (0–7, death = 8) against age and created line-plotted graphs expressing the progression of functional disability throughout their life (x-axis: age, y-axis: total ADL score) (Fig. 2). Furthermore, we calculated a gradient expressing ADL progression speed using a linear functional approximate expression of the line plot graph and compared each NF2 patient gradient to genetic and clinical factors (Fig. 3).
The growth rate of schwannoma and meningioma
Tumour volumetric analysis was performed as previously described using the volumetric function of the OsiriX Lite ver. 9.0 software21. We measured the total volume of intracranial schwannoma and meningioma for each patient, respectively and compared each total volume in the initial MRI studies with those of the last study to calculate the tumour growth rate.
Total interventions per year
By reviewing the medical records and our clinical database, we calculated the number of interventions each NF2 patient underwent during the follow-up period, including surgical treatment and radiotherapy for primary or recurrent tumours. The number of interventions for each patient was then divided by the follow-up duration (in years).
Statistical analysis
Statistical analyses were performed using the survival and ggplot2 packages in R v.3.1.2 (http://www.R-project.org).
Categorical variables were expressed as the mean and standard deviation (SD). The ADL outcomes, namely the period of functional preservation, were estimated for each mutation group and each prognostic grade using the Kaplan–Meier method, followed by the log-rank test to determine the total and trends. Each curve was compared using the log-rank test after Bonferroni correction.
The hazard ratio of all clinical/genetic factors for all major functional endpoints (“Disabled hearing or deafness,” “Tube feeding,” and “Wheelchair-bound or bedridden”) was analyzed using the univariate Cox proportional hazards model. Variables associated with functional endpoints in univariate analyses (P < 0.05) were included in a backward, stepwise Akaike’s Information Criterion (AIC) multivariate analysis. We checked the proportional hazards assumption for each variable by testing Schoenfeld residuals and using the double-log plot method.
Clinical factors included age of symptom onset (“25 ≦” or “24 ≧”; based on the mean of age of symptom onset), onset symptoms (hearing impairment or not), presence of an extra-CNS lesion, presence of intracranial meningioma, and family history. Genetic factors included types of germline mutations (“Truncating”, “Large deletion”, “Splice site”, “Missense” and “Mosaic”), and the locations of the germline mutations according to the functional domains (exon 2–7, exon 8–13, and exon 1 and 14–15).
The Mann–Whitney U test was used to compare two non-parametric continuous variables, while the Kruskal–Wallis and Steel–Dwass tests were used for multiple comparisons with non-parametric continuous variables. The Jonckheere-Terpstra test was used to test the trend across the five mutation groups and the four prognostic grades.
All reported p-values are two-sided. In all comparisons, p-values of less than 0.05 were considered statistically significant. Post-hoc pairwise comparisons between the five mutation groups or the four prognostic grades were adjusted using the Bonferroni method.
Ethical approval
The Institutional Review Board approved the study protocol of the University of Tokyo Hospital (G10026), and informed consent was obtained from all patients.
Data availability
The authors confirm that the data supporting the findings of this study will be shared by request from any qualified investigator.
References
Asthagiri, A. R. et al. Neurofibromatosis type 2. Lancet. 373, 1974 (2009).
Evans, D. G. Neurofibromatosis 2: GeneReviews®. 1993–2015 (University of Washington, Seattle).
Evans, D. G. Neurofibromatosis type 2 (NF2): A clinical and molecular review. Orphanet. J. Rare Dis. 4, 16 (2009).
Smith, M. J. et al. Revisiting neurofibromatosis type 2 diagnostic criteria to exclude LZTR1-related schwannomatosis. Neurology 88, 87–92 (2018).
Hexter, A. et al. Clinical and molecular predictors of mortality in neurofibromatosis 2: A UK national analysis of 1192 patients. J. Med. Genet. 52, 699–705 (2015).
Baser, M. E. et al. The location of constitutional neurofibromatosis 2 (NF2) splice site mutations is associated with the severity of NF2. J. Med. Genet. 42(7), 540–546 (2005).
Baser, M. E. et al. Predictors of the risk of mortality in neurofibromatosis 2. Am. J. Hum. Genet. 71, 715–23 (2002).
Ruttledge, M. H. et al. Type of mutation in the neurofibromatosis type 2 gene (NF2) frequently determines severity of disease. Am. J. Hum. Genet. 59(2), 331–342 (1996).
Parry, D. M. et al. Germ-line mutations in the neurofibromatosis 2 gene: correlations with disease severity and retinal abnormalities. Am. J. Hum. Genet. 59(3), 529–539 (1996).
Selvanathan, S. K. et al. Further genotype–phenotype correlations in neurofibromatosis 2. Clin. Genet. 77(2), 163–170 (2010).
Evans, D. G., Trueman, L., Wallace, A., Collins, S. & Strachan, T. Genotype/phenotype correlations in type 2 neurofibromatosis (NF2): Evidence for more severe disease associated with truncating mutations. J. Med. Genet. 35(6), 450–455 (1998).
Otsuka, G., Saito, K., Nagatani, T., Nagatani, T. & Yoshida, J. Age at symptom onset and long-term survival in patients with neurofibromatosis Type 2. J. Neurosurg. 99(3), 480–483 (2003).
Gutmann, D. H., Geist, R. T., Xu, H.-M., Kim, J. S. & Saporito-Irwin, S. Defects in neurofibromatosis 2 protein function can arise at multiple levels. Hum. Mol. Genet. 7, 335–345 (1998).
Halliday, D. et al. Genetic Severity Score predicts clinical phenotype in NF2. J. Med. Genet. 54(10), 657–664 (2017).
Plotkin, S. R. et al. Hearing and facial function outcomes for neurofibromatosis 2 clinical trials. Neurology. 81(21 Suppl. 1), 25–32 (2013).
Plotkin, S. R., Merker, V. L., Muzikansky, A., Barker, F. G. & Slattery, W. Natural history of vestibular schwannoma growth and hearing decline in newly diagnosed neurofibromatosis type 2 patients. Otol. Neurotol. 35(1), e50-56 (2014).
Wolters, P. L. et al. Patient-reported outcomes of pain and physical functioning in neurofibromatosis clinical trials. Neurology. 87(7 Suppl. 1), 4–12 (2016).
Cui, Y. X. et al. Mutation analysis of NF2 gene and clinical investigation in a Chinese family with neurofibromatosis type II. Zhonghua Yi Xue Yi Chuan Xue Za Zhi. 27(6), 688–691 (2010).
Seong, M. W. et al. Molecular characterization of the NF2 gene in Korean patients with neurofibromatosis type 2: A report of four novel mutations. Korean J. Lab. Med. 30(2), 190–194 (2010).
Kuo, H. C. et al. Neurofibromatosis 2 with peripheral neuropathies: Electrophysiological, pathological and genetic studies of a Taiwanese family. Neuropathology. 30(5), 515–523 (2010).
Teranishi, Y. et al. Targeted deep sequencing of DNA from multiple tissue types improves the diagnostic rate and reveals a highly diverse phenotype of mosaic neurofibromatosis type 2. J. Med. Genet. 58, 701 (2020).
Forde, C. et al. Disease course of neurofibromatosis type 2: A 30-year follow-up study of 353 patients seen as a single institution. Neuro. Oncol. 23, 1113 (2020).
Evans, D. G. et al. Incidence of mosaicism in 1055 de novo NF2 cases: Much higher than previous estimates with high utility of next–generation sequencing. Genet. Med. 22(1), 53–59 (2020).
Acknowledgements
We are grateful to Dr Kostadin Karagiozov for his helpful discussions and the editing of the manuscript.
Funding
This project was supported by a Grant-in-Aid for Scientific Research (B) (No. 21H03041) from the Japan Society for the Promotion of Science to Dr Saito, a Grant-in-Aid for Scientific Research (C) (No. 19K09473) from the Japan Society for the Promotion of Science to Dr Miyawaki, a Grant-in-Aid for Research Activity Start-up (No. 19K24023) from the Japan Society for the Promotion of Science to Dr Teranishi, a Grant-in-Aid for Young Scientists (20K17954) from the Japan Society for the Promotion of Science to Dr Teranishi, a research grant from the Takeda Science Foundation to Dr Miyawaki, a research grant from Japan Intractable Diseases (Nanbyo) Research Foundation to Dr Miyawaki, and a JSPS KAKENHI (221S0002 PAGS).
Author information
Authors and Affiliations
Contributions
Y.T. analyzed and interpreted all clinical data. S.M., J.M., H.N., S.M., S.T., and N.S. designed the experiments. Y.T., H.H., S.D., A.O., S.T., T.O., and S.M. performed the experiments. J.Y., W.Q., and S.M. performed the bioinformatics analysis. Y.T. and S.M. interpreted the results and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Teranishi, Y., Miyawaki, S., Nakatomi, H. et al. Early prediction of functional prognosis in neurofibromatosis type 2 patients based on genotype–phenotype correlation with targeted deep sequencing. Sci Rep 12, 9543 (2022). https://doi.org/10.1038/s41598-022-13580-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-13580-9
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.