Abstract
This study explores the natural history of vestibular, trigeminal and lower cranial nerve schwannomas (VS, TS, LCNS) in patients with Neurofibromatosis type 2 (NF2), to understand how pathogenic variants (PVs) of the NF2 gene affect tumour burden and growth rate, via a retrospective analysis of a UK NF2 centre database and imaging. VS, TS and LCNS location and size were measured in accordance with a standardised protocol. PVs were categorised in accordance with the UK NF2 Genetic Severity Score (GSS). 153 patients (age 5–82) had 458 schwannomas, of which 362 were previously untreated comprising: 204 VS, 93 TS, and 65 LCNS (IX, X, XI). 322 schwannomas had sequential imaging allowing growth rate analysis with a mean follow-up of 45 months. VS were universally present, and bilateral in 146/153 cases. 65% of tumours grew >2 mm during the study period at mean rate 2.0 mm/year. Significant association was found between increasing GSS and growth rate. TS occurred in 66/153 patients (bilateral in 27/153); 31% of tumours showed growth (mean 1.8 mm/yr). Significant increase in tumour prevalence was noted with increasing GSS. LCNS were found in 47/153 patients (bilateral in 19/153); 27% of tumours showed growth (mean 1.9 mm/yr). The trend for increased prevalence with increasing GSS did not reach significance. VS growth rate was significantly influenced by GSS and they were much more likely to grow than TS and LCNS. TS prevalence also correlated with increasing GSS.
Similar content being viewed by others
Introduction
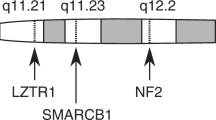
Neurofibromatosis type 2 (NF2) is an autosomal dominant heritable syndrome resulting in a predisposition for tumours of the nervous system [1]. The reported birth incidence is ~1 in 28,000, with a population prevalence of 1 in 50,500. The latter is likely to be increasing due to improved disease recognition and management [2, 3]. The pathophysiology of NF2 arises from defects in the NF2 gene located on chromosome 22q12 which produces merlin protein which regulates cell proliferation and ordinarily functions as a tumour suppressor [4]. Many pathogenic variants (PVs) of the NF2 gene have been described including insertions, deletions, splice-site, missense and truncating variants (nonsense/frameshift) [5]. PVs may be either constitutional, involving all cells in the body, or mosaic when somatic mutations occur during early embryogenesis resulting in a subpopulation of affected cells.
The hallmark of NF2 is bilateral vestibular schwannomas (VS) which are found in over 90% of patients [6, 7], although other tumours including meningiomas, ependymomas and non-VS may feature and can contribute to the diagnosis. VS frequently result in tinnitus and hearing loss which are the most common presenting symptoms of NF2 [6, 8]; tumours may become life threatening if progressive growth results in significant brainstem compression. Non-VS have been reported on all cranial nerves (CN) except olfactory and optic nerves [9]. The prevalence varies by nerve of origin and between studies. Trigeminal schwannomas (TS) are found in 27–72% of patients, while lower cranial nerve schwannomas (LCNS) have been reported in 9–36% [7, 9, 10].
The overall management strategy for patients with NF2 is centred on avoiding/treating complications of the disease while preserving function and quality of life for as long as possible. The bilateral nature of VS presents challenging clinical dilemmas due to the potential morbidity associated with treatment which is often in the form of surgical resection [8]. For this reason, it is important to understand the natural history of VS in NF2 so that the likely clinical course both with and without treatment can be evaluated when considering the timing of interventions. There are large published series describing the growth behaviour of hundreds of sporadic VS [11, 12], however a relative paucity of evidence for patients with NF2, no doubt due to the rarity of the condition [13,14,15,16]. The evidence base for the behaviour of non-vestibular cranial nerve schwannomas in NF2 is even more limited [7, 9]. Our experience has been that many non-VS are indolent and remain largely static. Although, we have seen TS and LCNS growing to a significant size, we have found treating them due to brainstem compression, largely unnecessary.
Disease severity in NF2 is strongly correlated with the type of genetic PV [17]. Truncating PVs are associated with particularly aggressive disease [18]. The UK NF2 genetic severity score (GSS) is a validated categorisation of the many different types of PVs into five ranked severity groups which were shown to be associated with many aspects of NF2 disease, although it was not tested against intracranial schwannomas [19]. Indeed, only one study to date has demonstrated an association of VS growth and specific PVs [20].
The aim of this study was to characterise the natural history of the most common intracranial schwannomas in NF2 and to understand how PVs might affect tumour burden and growth rate between these different tumour types.
Method
A retrospective analysis was conducted using data from the Manchester (UK) NF2 centre database. Such service evaluations are not required to seek ethical review and are given automatic approval. All patients meeting the latest diagnostic criteria for NF2 [3] and managed by the multi-disciplinary team (MDT) between 2010 and 2015 were included.
Data collection included patient demographics (gender, date of birth), type and location of PV, PV pattern (mosaic/constitutional), age-at-diagnosis, cranial nerve schwannoma location and previous treatment details. Age-at-study-enrollment was determined as the patient age when the first scan that was included in this study was performed.
PVs were categorised in accordance with the UK NF2 GSS [19]. This score assigns patients to one of five categories (1a, 1b, 2a, 2b, 3) based on PV pattern, with 1a representing the mildest clinical phenotype, and 3 the most severe. Molecular analysis was undertaken on DNA extracted from blood lymphocytes and, where available, tumour as previously described using next generation sequencing and Multiplex Ligation-dependant Probe Amplification [19, 21]. It is our intention to submit pathological variants to DECIPHER.
Tumour size was assessed by Magnetic Resonance Imaging (MRI) in the large majority of cases, with Computed Tomography (CT) studies only used for a small number of clearly visible tumours. MRI was used to assess final cranial nerve schwannoma size in all cases. Imaging was considered adequate if (i) the schwannomas of interest were visible and delineable on axial sequences with no evidence of significant distortion from auditory brainstem or cochlear implants (where present) and (ii) the z-axis slice interval was ≤3 mm. Where available T1-weighted post-contrast imaging was assessed; otherwise, high-resolution axial FIESTA/CISS imaging was assessed.
Tumours were excluded from the growth data set if there had been prior local (surgery/radiotherapy) treatment. No patient was included in the growth data set who had previously been treated with systemic therapy (bevacizumab/‘avastin’). During the study, growth was censored at the time of treatment with radiotherapy or surgery for individual tumours. If a patient received systemic therapy with bevacizumab, growth was censored for all tumours in that patient at the time of treatment.
Cranial nerve schwannomas were characterised by anatomical location. VS and TS were analysed separately, whereas LCNS (CN 9-11) were grouped together due to the radiological difficulty in determining the individual nerve of origin in these cases. Tumours in the internal auditory meatus (IAM) projecting into the cerebellopontine angle (CPA) were presumed to be VS. Extra-cranial components of TS and LCNS were not measured, in particular extension into the skull base or the jugular foramen respectively. Tumours that were clearly meningiomas based on shape and dural attachment were excluded. Collision tumours presented a measurement challenge. In these cases a best estimate was made with reference to previous imaging.
Tumour measurements were made by specialist neuro-radiologists (OT/RS/CC) or neuro-otologists (SF/DM) working within the NF2 MDT. Tumour size was measured in accordance with a standardised protocol, with all measurements taken in the axial plane using the image with the greatest tumour diameter with measurements from follow up scans matched to the same anatomical position. For TS and LCNS the maximum overall diameter in the axial plane was measured; for TS this included both the middle fossa and CPA components combined into a single measurement for “dumbbell” tumours that crossed these compartments. For VS two measurements were obtained: (i) maximum diameter of the cerebello-pontine angle (CPA) component and (ii) maximum mediolateral overall length (OL) including the intracanalicular component. For each tumour, growth was assessed by comparing the first and last available imaging and calculating an annualised rate. ‘Tumour growth’ was defined as occurring if there was a ≥ 2 mm in size of the schwannoma between two time points [22, 23].
Statistical analysis for the prevalence of TS and LCNS was conducted using Fisher’s exact test to determine if there were significant differences between GSS categories. Tumour status (none/unilateral/bilateral) was treated as nominal and each GSS category was compared against the others using the Freeman–Halton extension to Fisher’s exact test [24, 25] with a p = 0.05 significance level. Due to the number of comparisons required an initial 5 × 5 Fisher’s exact test was conducted at the p = 0.005 significance level (a Bonferroni correction for 10 comparisons).
For VS growth rate data, we used ordinal logistic regression with the OL growth rate as the outcome, and GSS as the categorical independent variable to examine how these two variables were associated. Ordinal logistic regression was chosen as growth rate did not meet the assumptions of linear regression, but this did necessitate that we categorise this variable. We divided growth rate into three categories: no growth/reduction in size (though very few reduced), growth up to 2 mm per year and growth greater than 2 mm per year. Whether adjusting for age-at-study-enrollment in the model is appropriate or bias-inducing depends on whether it is a confounder or a mediator of the relationship between tumour growth and genetic severity. As a sensitivity analysis we repeated the model, this time including age-at-study-enrolment in the model as an adjustment factor.
Within subject variation was assessed in patients with growth rate data for bilateral VS by calculating Pearson’s correlation coefficient.
Results
153 patients aged 5–82 years (mean: 32.9, median: 29) were included in this study and had 458 intracranial schwannomas (VS/TS/LCNS). Table 1 shows mean age-at-diagnosis, mean age-at-study-enrollment and mean tumour baseline sizes. Adequate MR imaging was available for all included patients. Two patients were excluded as it was not possible to reliably determine tumour margins due to meningioma/schwannoma collision tumours in the CPA.
Prevalence data included 96 tumours (95 VS, 1 LCNS) that had received treatment prior to the start of this study. These were excluded from size and growth analysis (Fig. 1). There were 362 untreated intracranial schwannomas (204 VS, 93 TS and 65 LCNS) that were assessed for baseline size and 322 schwannomas with sequential imaging allowing growth rate analysis with mean follow-up 45 months (range: 4–171, median: 38). Initially included tumours were censored from ongoing growth analysis due to starting bevacizumab treatment (31 patients, 95 tumours), surgery (16 patients, 17 tumours) or radiotherapy (3 patients, 3 tumours). Patients in higher GSS categories were more likely to undergo treatment during the study period (Table 2).
There was no association between baseline size of schwannoma with other variables including age or GSS. Table 3 summarises the growth rates for each schwannoma type stratified by GSS.
Vestibular schwannomas
There were 299 VS, with 146/153 patients(95%) having bilateral tumours, and 7/153 patients(5%) unilateral. Baseline OL ranged from 2 to 49 mm (mean: 13.7 mm) with 86/204(42%) of tumours being entirely intra-canalicular. Tumours extending beyond the IAM had CPA components with maximal diameters from 3 to 59 mm (mean: 14.6 mm).
Growth data was available for 177 VS; this was assessed using OL as it allowed inclusion of both intra-canalicular tumours and those with CPA component. 115/177(65%) tumours showed ≥2 mm growth over a mean period of 45 months, with a mean growth rate (for all growing tumours) of 2.0 mm/year (range: 0.2–6.5 mm/year). The remaining tumours were stable except for 3/177(2%) that decreased in size.
For GSS 1a only 12/33(36%) of VS showed growth and the growth rate for those growing tumours was mean 0.9 mm/year. For patients with GSS 3, all tumours (10/10) showed growth at a mean rate of 2.5 mm/year. There was a progressive increase in both likelihood of tumour growth, and growth rate, with each step in increasing GSS (Table 3).
The results of the ordinal logistic regression for growth rate are shown in Table 4a. The confidence intervals for all coefficients are wide and this should be considered when interpreting the results. There was no significant difference between the odds of growth for genetic severity categories 1a and 1b. For those of GSS 2a the odds of being in a higher growth category are 2.62 (95% CI 1.08–6.34) greater than those of genetic severity 1a, a significant result (p = 0.032). As the GSS increased so too did the magnitude of the effect although the precision of our estimate decreases. For those of GSS 2b the odds of being in a higher growth category, compared to those of GSS 1a, are 5.78 (95% CI 2.52–13.24), p < 0.001. For those of GSS 3 the odds of being in a higher growth category, compared to those of GSS 1a, are 24.23 (95% CI 5.25–111.83), p < 0.001. This last result should be taken with extra caution, the confidence interval is wide enough to suggest that the sample size for GSS 3 was too small to be usefully included in the model.
The sensitivity analysis included age-at-study-enrollment as a covariate in the aforementioned model, reducing the magnitude of all coefficients and reducing all but the comparison of genetic severity 3 and 1a to non-significance. Results are presented in Table 4b. Which of the two models is more appropriate is debatable.
Within subject analysis of 62 patients with growth rate data for bilateral VS yields a correlation coefficient of 0.46 (p < 0.001) when comparing growth rates of left against right sided tumours.
Trigeminal schwannomas
93 TS were found, with 87/153 patients (57%) having none, 39/153 patients (25%) having unilateral and 27/153 patients (18%) having bilateral TS. Baseline size ranged from 2 to 40 mm (mean: 11.6 mm). Patients with GSS 1a did not have TS in 17/23(74%) cases and only 1/23 patients(4%) had bilateral tumours. This contrasts to patients with GSS 3 in whom only 3/15(20%) had no tumours and 7/15(47%) had bilateral tumours (p = 0.002) (Fig. 2). There was a progressive step-wise decrease in the proportion of patients without TS with increasing GSS, and a corresponding increase in the proportion of bilateral tumours. Statistically significant differences were found between GSS 3 and all other groups except 2b (p = 0.0008, 0.006, 0.001, 0.134, for 1a, 1b, 2a, and 2b respectively). There was also a significant difference between category 2b and 1a (p = 0.042). TS showed ≥2 mm growth in 27/86(31%) tumours over a 43 month mean follow-up. Growing tumours increased in size at mean rate of 1.8 mm/year (range 0.5–5.0 mm/year). All remaining TS were stable. The relationship between GSS and growth rates of TS and LCNS was more variable than for VS. The small numbers of growing tumours at these locations meant that individual outlying results had a disproportionately large effect on the overall results for each sub-category in some cases (Table 3).
Lower cranial nerve schwannomas
66 LCNS were found with 106/153 patients(69%) having none, 28/153 patients(18%) having unilateral, and 19/153 patients(12%) having bilateral LCNS. Baseline size was between 2 and 28 mm (mean: 8.8 mm). The relationship between prevalence and GSS for LCNS was similar to TS with patients in category 1a having no tumour in 20/23(87%) of cases and no bilateral tumours, compared to patients in category 3 having no tumour in 9/15(60%) of cases and 3/15(20%) bilateral tumours (Fig. 3). Perhaps due to the smaller number of tumours in this group, a statistically significant difference between GSS categories was not proven in the overall analysis (p = 0.219). LCNS showed ≥2 mm growth in 17/62(27%) cases over a 39 month mean follow-up, with growing tumours increasing at 1.9 mm/year on average (range 0.4–7.6 mm/year). All other LCNS were stable.
Discussion
This study identified 458 tumours in 153 patients. This was possible in part due to centralisation of NF2 services in the UK with four designated centres receiving referrals from wide catchment populations [26, 27]. The most striking finding was the significant association between GSS and VS growth rate (Tables 3 and 4), particularly as this may understate the true figure due to the higher proportion of tumours excluded because of previous treatment (and therefore inevitably growing) from the higher GSS patients (Fig. 1). The prevalence of TS was also significantly associated with GSS (Fig. 2). LCNS had a relatively low prevalence in comparison with TS and VS, with <50% of patients affected even in the high GSS categories (Fig. 3). Although a trend towards greater prevalence with increasing GSS can be seen, a larger cohort would be required to reach statistical significance.
Vestibular schwannomas
Direct comparison of VS growth rates with previously published data is challenging. Studies have used different inclusion criteria, measurement strategies, follow-up periods and definitions of growth [13, 15, 16, 28]. Where linear measurements are reported, results are broadly in keeping with our data. Slattery et. al. report an average growth rate of 1.9 mm/year, although the proportion of tumours growing was lower than in our study (13% vs 33% after adjusting our data to match their 5 mm growth threshold). In addition, as in our study, no relationship was found between the size of tumour at baseline and subsequent growth rate [16].
Tumours with the highest growth rates of >4 mm/year were only seen in patients under the age of 25 (Fig. 4). It must be emphasised that this is mean growth over several years. We did still see people with higher VS growth rates in the older population in tumours that were previously indolent, and these were sometimes subsequently treated. The relationship between VS growth, age-at-study-enrollment and GSS is complex and previous literature is contradictory. This seems to be due to the facts that VS growth rate is often variable and may be saltatory and that such studies involved small numbers and heterogenous inclusion criteria. Baser et al. [28] for example included 31 VS and found younger patients tended to have higher growth rates but they were unable to demonstrate a link with PVs. Gugel et al. [20] only included tumours in patients under 25 years of age that had required surgery, inevitably therefore including only people with the most aggressive disease. They found that truncating mutations had faster growth rates than those with splicing mutations, roughly equivalent to GSS 3 vs 2a and 2b, but this was only in the postoperative evaluation, not preoperative.
In our study mean age-at-study-enrollment and age-at-diagnosis for patients with GSS 1a is 56.7 years and 52.8 years respectively, whereas for GSS 3 it is 21.0 years and 15.5 years (Table 1). Younger patients were more likely to have severe genetic PVs, to have tumours present from a younger age, and aggressive disease that is reflected in the observed increased growth rate of tumours. Nevertheless, there appears to be a trend for increased growth rate with younger age even within GSS categories, most noticeable for GSS 2a and 2b (Fig. 4) and it may be that age is an independent factor for VS growth rate in its own right. Equally it could be that biologically aggressive tumours were inevitably treated and so became less relevant in the older age groups. In addition, evidence is increasingly emerging of the relevance of inflammatory factors in determining VS growth rates and it may be that these are as important or even more so than age or the underlying PV [29].
Trigeminal schwannomas
Three previous studies report the prevalence of TS in NF2. Mautner et. al. report 17% unilateral, and 13% bilateral tumours (n = 46) [6]. Bakir et al. found 14% of patients had unilateral tumours and 17% bilateral tumours (n = 83) [10]. Fisher et. al. report 46 TS in a cohort of 83 patients without specifying whether unilateral or bilateral [9]. Our study found an overall higher prevalence of TS with 25% unilateral and 18% bilateral tumours.
Bakir et al. propose that TS have an indolent course radiologically based on 26 patients in which only 2 tumours showed growth over a mean 5-year period [10]. Fisher et. al support this finding with 1/27 tumours showing growth over a 3-year period [9]. Our data show a greater proportion of TS growing, with 31% increasing by ≥2 mm in diameter during the follow-up period of 43 months. No TS required treatment either prior to or during our study period.
Lower cranial nerve schwannomas
Compared to VS and TS, there is a relative paucity of data for LCNS. Mautner et al. report 16% unilateral schwannoma prevalence and 5% bilateral (if hypoglossal and vagal are combined), whereas Fisher et al. report 7% and 0% respectively [6, 9]. Our prevalence results show 18% unilateral tumours and 12% bilateral. The reason for the increased prevalence of LCNS (and TS) in our series is unclear, the mean age of patients is broadly similar between studies.
Regarding growth, Fisher et al. reported no growth in 6 LCNS observed. A series of sporadic schwannomas reported 2/4 LCNS growing over a 3 year period, although there may be selection bias as these were symptomatic tumours in non-NF2 patients [21]. Our data shows 27% of LCNS growing over a 39-month follow-up period. The higher rates of TS and LCNS growth in this study when compared to the aforementioned literature are supported by Dirks et al. who noted growth in 82% of non-VS over a mean 9.5-year period [7]. They suggest growth occurs in a ‘saltatory’ stop-start pattern and that growth is best appreciated over a longer time course. Only two LCNS required treatment in our series, one prior to the observation period and one during. Nevertheless, lower cranial nerve palsies associated with these tumours represent significant morbidity therefore their development is relevant [9].
Genotype/phenotype correlations with TS and LCNS
The ‘severe’ clinical phenotype (defined as age <20 at diagnosis or multiple NF2 related tumours) has previously been associated with increased prevalence of non-VS [6]. More recently nonsense or frameshift PVs (associated with truncated protein and more severe clinical phenotype) have been associated with increased prevalence of non-vestibular cranial nerve schwannomas [18]. Our prevalence analyses for TS and LCNS would support this and show that further sub-categorisations of PV type have prognostic value. Neither TS nor LCNS growth rates were associated with GSS in this study which might be due to several factors. There were relatively small numbers, particularly in the lower GSS groups. Both TS and LCNS are relatively indolent and our experience is that they are very unlikely to require treatment, even in the higher GSS groups. This means that it is likely that they undergo saltatory growth patterns with long periods of stability. In addition the occasional tumour that was undergoing fast growth during the study period disproportionately affected the analysis.
Limitations of data set, potential confounders
Linear measurements were used in accordance with a defined protocol to ensure accurate and reproducible results between patients. Our measurement strategy is the same as the American Academy of Otolaryngology – Head and Neck Surgery, Committee on Hearing and Equilibrium 1995 [30]. For VS, the decision to combine the intra-cranial and intra-canalicular components of larger tumours into a single OL measurement was taken deliberately to allow cross comparison of a larger number of tumours at different stages of growth. Collision tumours presented a difficult challenge with measuring some tumours, especially VS and TS. Careful analysis of tumour change over time allowed us to distinguish meningiomas from schwannomas in many cases but this clearly represents a source of bias and it is possible that some growth reflects change in meningioma rather than schwannoma. While volumetric measurements in combination with a high spatial resolution MR acquisition have been shown to be more precise and repeatable in detecting tumour growth when compared to linear measurements [31, 32], the two strategies show good correlation. Use of volumetric measures may have increased the significance of the analysed associations and this could be considered by future publications. Linear measurements were also mandated by practical considerations in this study due to limited availability and as some early scans did not have the required slice thickness for meaningful volumetric interpretation. A significant methodological challenge when interpreting the findings from any observational study is the potential for results to be influenced by selection bias [33]. While we aimed to assess the natural history of intracranial schwannomas, patients underwent treatment or intervention when clinically indicated. 96 of a possible 299 VS were excluded due to treatment prior to the study period. These were treated for either ongoing growth or massive size with severe brainstem compression on initial presentation. Rapidly growing tumours in young patients were treated and removed from the data set during the study for the same reasons. These issues potentially contribute to the trend for slower growing tumours with increasing age. This is mitigated by the cross-sectional analysis of a large number of patients so that similar tumours (that will require treatment in future) should have been captured at an earlier point in their clinical course. The tendency to treat tumours more conservatively in NF2 (compared to sporadic tumours) means that most tumours would undergo at least some period of observation. Nevertheless, our finding that 35% of tumours were static is therefore probably on overestimate and the true figure is likely to be lower. Figure 4 demonstrates this well across the different GSS.
The inter-related nature of age and GSS as variables presents a significant obstacle to inferring causality in relation to schwannoma growth patterns and is particularly relevant to our VS growth rate findings. GSS and age-at-study-enrollment are by their nature, and by the nature of the study design, entangled to the point that it was impossible to make definitive statements about their causal structure. With this comes many risks of adjusting/not adjusting for appropriate confounders/colliders, therefore we can only summarise these findings in a broad sense.
In our series, patients with GSS 1a had a greater age-at-study-enrollment (mean age = 56.7 years) than patients with GSS 3 (mean age = 21.0 years), and this difference is also reflected in age-at-diagnosis (Table 3). There are several possible reasons for this. Genetic testing of relatives may lead to the inclusion of younger patients who do not have mosaicism and so lower the mean age of patients in categories 2a, 2b, and 3. Reduced life expectancy with more severe PVs may result in a relative paucity of patients reaching the older age groups. Patients in higher GSS categories become symptomatic at a younger age and are therefore diagnosed and undergo regular surveillance imaging earlier in life. The last two factors have been shown to be significant in a previous study of the UK NF2 GSS [19].
Conclusion
Non-vestibular cranial nerve schwannomas (TS and LCNS) increased in prevalence with increasing severity of genetic PV. Although growth rates in growing tumours were similar between VS, TS and LCNS, a greater proportion of VS underwent growth, particularly in the higher GSS groups. VS growth likelihood and growth rate were associated with increasing GSS. TS and LCNS growth rates were not clearly associated with GSS. They very rarely required treatment so it seems likely that their growth patterns are saltatory with long static periods.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Lloyd SK, Evans DG. Neurofibromatosis type 2 (NF2): diagnosis and management. Handb Clin Neurol. 2013;115:957–67.
Evans DG, Bowers NL, Tobi S, Hartley C, Wallace A, King A, et al. Schwannomatosis: a genetic and epidemiological study. J Neurol Neurosurg Psychiatry. 2018;89:1215–9.
Evans DG, King AT, Tobi S, Wallace AJ, Perry M, Anup R, et al. Identifying the deficiencies of current diagnostic criteria for neurofibromatosis 2 using databases of 2777 individuals with molecular testing. Genet Med. 2019;21:1525–33.
Giovannini M, Robanus-Maandag E, Niwa-Kawakita M, Van der Valk M, Woodruff JM, Goutebroze L, et al. Schwann cell hyperplasia and tumours in transgenic mice expressing a naturally occurring mutant NF2 protein. Genes Dev. 1999;13:978–86.
Welling DB, Packer MD, Chang LS. Molecular studies of vestibular schwannomas: a review. Curr Opin Otolaryngol Head Neck Surg. 2007;15:341–6.
Mautner V, Lindenau M, Baser M, Hazim W, Tatagiba M, Hasse W, et al. The Neuroimaging and Clinical Spectrum of Neurofibromatosis 2. Neurosurgery. 1996;38:880–6.
Dirks MS, Butman JA, Kim HJ, Wu T, Morgan K, Tran AP, et al. Long-term natural history of neurofibromatosis Type 2—associated intracranial tumors. J Neurosurg. 2012;117:109–17.
Evans DG. Neurofibromatosis type 2 (NF2): a clinical and molecular review. Orphanet J Rare Dis. 2009;4:16.
Fisher L, Doherty J, Lev M, Slattery W. Distribution of Nonvestibular Cranial Nerve Schwannomas in Neurofibromatosis 2. Otol Neurotol. 2007;28:1083–90.
Bakir M, Connor S, Thomas N, Barazi S. Trigeminal Schwannomas in Neurofibromatosis 2. J Neurol Surg B Skull Base. 2012;73 - A280 https://doi.org/10.1055/s-0032-1314195.
Moffat D, Kasbekar A, Axon P, Lloyd S. Growth Characteristics of Vestibular Schwannomas. Otol Neurotol. 2012;33:1053–8.
Stangerup S, Caye-Thomasen P, Tos M, Thomsen J. The Natural History of Vestibular Schwannoma. Otol Neurotol. 2006;27:547–52.
Mautner VF, Baser ME, Thakkar SD, Feigen UM, Friedman JM, Kluwe L. Vestibular schwannoma growth in patients with neurofibromatosis Type 2: a longitudinal study. J Neurosurg. 2002;96:223–8.
Harris GJ, Plotkin SR, MacCollin M, Bhat S, Urban T, Lev MH, et al. Three-Dimensional Volumetrics for Tracking Vestibular Schwannoma Growth in Neurofibromatosis Type 2. Neurosurgery. 2008;62:1314–9.
Picry A, Bonne NX, Ding J, Aboukais R, Lejeune JP, Baroncini M, et al. Long-term Growth Rate of Vestibular Schwannoma in Neurofibromatosis 2: A Volumetric Consideration. Laryngoscope. 2016;126:2358–62.
Slattery WH, Fisher LM, Iqbal Z, Oppenheimer M. Vestibular Schwannoma Growth Rates in Neurofibromatosis Type 2 Natural History Consortium Subjects. Otol Neurotol. 2004;25:811–7.
Ruttledge MH, Andermann AA, Phelan CM, Claudio JO, Han F, Chretien N, et al. Type of Mutation in the Neurofibromatosis Type 2 Gene (NF2) Frequently Determines Severity of Disease. Am J Hum Genet. 1996;59:331–42.
Selvanathan SK, Shenton A, Ferner R, Wallace AJ, Huson SM, Ramsden RT, et al. Further genotype-phenotype correlations in neurofibromatosis 2. Clin Genet. 2010;77:163–70.
Halliday D, Emmanouil B, Pretorius P, Mackeith S, Painter S, Tomkins H, et al. Genetic Severity Score predicts clinical phenotype in NF2. J Med Genet. 2017;54:657–64.
Gugel I, Grimm F, Teuber C, Kluwe L, Mautner VF, Tatagiba M, et al. Management of NF2-associated vestibular schwannomas in children and young adults: influence of surgery and clinical factors on tumor volume and growth rate. J Neurosurg Pediatr 2019;24:584–92.
O’Reilly BF, Mehanna H, Kishore A, Crowther JA. Growth rate of non-vestibular intracranial schwannomas. Clin Otolaryngol. 2004;29:94–97.
Fucci M, Buchman C, Brackman D, Berliner K. Acoustic Tumour Growth: Implications for Treatment Choices. Am J Otol. 1999;20:495–9.
Marshall A, Owen V, Nikolopoulos T, O’Donoghue G. Acoustic Schwannomas: Awareness Of Radiologic Error Will Reduce Unnecessary Treatment. Otol Neurotol. 2005;26:512–5.
DS S. 2x3 Contingency Table Exact Test Calculator. [Online];Date accessed May 2020. http://www.analyticscalculators.com.
Freeman G, Halton J. Note on an exact treatment of contingency, goodness of fit and other problems of significance. Biometrika 1951;1:141–9.
Neurofibromatosis Type 2 Service (All Ages). In: Highly Specialised Services 2018. NHS England. pp 52–3.
Lloyd SK, Evans DG. Neurofibromatosis type 2 service delivery in England. Neurochirurgie. 2018;64:375–80.
Baser ME, Makariou EV, Parry DM. Predictors of vestibular schwannoma growth in patients with neurofibromatosis Type 2. J Neurosurg. 2002;96:217–22.
Lewis D, Donofrio CA, O’Leary C, Li KL, Zhu X, Williams R, et al. The microenvironment in sporadic and neurofibromatosis type II-related vestibular schwannoma: the same tumor or different? A comparative imaging and neuropathology study. J Neurosurg. 2020; 134:1–11.
Equilibrium CoHa. Committee on Hearing and Equilibrium guidelines for the evaluation of hearing preservation in acoustic neuroma [vestibular schwannoma]. Otolaryngol Head Neck Surg. 1995;113:179–80.
Mackeith S, Das T, Graves M, Patterson A, Donnelly N, Mannion R, et al. A comparison of semi-automated volumetric vs linear measurement of small vestibular schwannomas. Eur Arch Otorhinolaryngol. 2018;275:867–74.
Morris KA, Parry A, Pretorius PM. Comparing the sensitivity of linear and volumetric MRI measurements to detect changes in the size of vestibular schwannomas in patients with neurofibromatosis type 2 on bevacizumab treatment. Br J Radio. 2016;89:20160110.
Baser ME, Mautner VF, Parry DM, Evans DG. Methodological issues in longitudinal studies: vestibular schwannoma growth rates in neurofibromatosis 2. J Med Genet. 2005;42:903–6.
Author information
Authors and Affiliations
Contributions
Study conception and design: SRF, JW, OT, SKL, SAR, ES, CHW, ONP, RL, MJS, AJW, MK, DGE, and ATK. Data collection: DM, JW, OT, RS, CC, RL, and SRF. Data analysis: DM, JW, OT, CH, and SRF. Results interpretation: SRF, DM, JW, OT, SKL, SAR, ES, CHW, ONP, RL, MJS, AJW, MK, DGE, and ATK. Drafting the manuscript: DM, and JW. Manuscript revision and approval: all authors.
Corresponding author
Ethics declarations
Competing interests
DGE, SKL and MJS are supported by the all Manchester NIHR Biomedical Research Centre (IS-BRC-1215-20007). The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Moualed, D., Wong, J., Thomas, O. et al. Prevalence and natural history of schwannomas in neurofibromatosis type 2 (NF2): the influence of pathogenic variants. Eur J Hum Genet 30, 458–464 (2022). https://doi.org/10.1038/s41431-021-01029-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-021-01029-y
This article is cited by
-
Imaging as an early biomarker to predict sensitivity to everolimus for progressive NF2-related vestibular schwannoma
Journal of Neuro-Oncology (2024)
-
Incidence and prevalence of neurofibromatosis type 1 and 2: a systematic review and meta-analysis
Orphanet Journal of Rare Diseases (2023)
-
2022: the year that was in the European Journal of Human Genetics
European Journal of Human Genetics (2023)
-
No April fools in clinical genomics
European Journal of Human Genetics (2022)