Abstract
Frailty in older patients is associated with poor postoperative outcomes. The use of uncomplicated frailty measurement tools is preferred in busy clinical settings. Therefore, we validated the frailty index using routine laboratory data and the surgical outcomes of older patients with cancer who underwent cancer resection. We retrospectively analyzed 9015 patients aged 65 years and older who underwent cancer resection at a single tertiary hospital. Based on electronic-medical-record data regarding preoperative blood test results and vital signs, Laboratory Frailty Index (FI-Lab) scores were generated to measure preoperative frailty. The associations of FI-Lab with postoperative length of stay (LOS), readmission within 30 days, intensive care unit (ICU) admission within 30 days, and mortality were evaluated. The mean FI-Lab score of the 9015 patients was 0.20 ± 0.10. Increased FI-Lab scores (0.25–0.4; > 0.4) were associated with longer LOS, increased readmission within 30 days of surgery, ICU admission, and increased mortality, compared with FI-Lab scores < 0.25. The FI-Lab score, as a frailty indicator, was able to predict the risk of poor postoperative outcomes. Therefore, the FI-Lab is a potentially useful tool for assessing preoperative frailty in older patients with cancer in acute clinical setting.
Similar content being viewed by others
Introduction
Surgery is considered the optimal treatment for solid tumors; however, it can increase the postoperative risk of morbidity and mortality in older patients with cancer1. Therefore, factors other than age should be considered when predicting postoperative recovery in older patients with cancer1,2. Frailty is a clinical syndrome defined as condition that is vulnerable to maintaining homeostasis to stressors due to reduced physiological capacity3,4,5. Preoperative frailty in older patients with cancer has been found to be associated with poor surgical outcomes, such as greater length of hospital stay, complications, and mortality6,7,8,9. Several tools have been developed to measure frailty; nonetheless, there is no consensus regarding which tools are most useful in surgical patients. Among them, the frailty phenotype method2, and frailty index10,11,12,13 are widely used. However, both evaluation methods require skilled medical personnel; further, due to the long evaluation time and limited resources, it is difficult to apply them preoperatively in clinical practice to older patients with cancer1,14.
In recent years, to identify early frailty states that can increase the risk of clinically detectable frailty, a new indicator, the Laboratory Frailty Index (FI-Lab) score, has emerged and it is based solely on biomarkers of vital signs and the results of general blood tests, such as albumin, hemoglobin, cholesterol, sodium, and potassium15,16,17,18,19,20. This tool is well established in a sample of community residents17,18,19 and has been widely used to measure biological age in both western and eastern countries15,16,21. Studies have reported that, the FI-Lab demonstrated favorable consistency with the clinical frailty index16,20 in predicting mortality, number of hospitalization days, and frequency of hospital visits15,16,17,18,20, and the risk of mortality has reportedly increased with increasing FI-Lab scores in asymptomatic patients without clinically expressed frailty17,18,22. In addition, the FI-Lab score contributes to further quantification of risk beyond clinical evaluation for frailty15,17,20,23. Given these points, FI-Lab may potentially be a more objective measure than the frailty tools, which relies on subjective self-reported data. In acute care settings where various laboratory investigations are routinely performed and readily available in electronic health records, the FI-Lab captures frailty in a standardized way. Thus, FI-Lab can be easily applied to patients who are in the acute phase of surgery so that plans can be made to prevent complications and promote rapid recovery. Although many studies to date have reported frailty in cancer patients as a potential predictor24,25, few studies have measured frailty with the FI-Lab.
The aim of this study was to investigate the association between preoperative frailty and postoperative clinical outcomes and mortality in elderly patients with cancer. The FI-Lab scores were generated based on electronic-medical-record data. The following research questions were posed:
-
(1)
In elderly patients with cancer, can preoperative FI-Lab measure clinically indistinguishable frailty?
-
(2)
How is frailty in cancer patients identified by the FI-Lab related to postoperative length of stay (LOS), readmission within 30 days, intensive care unit (ICU) admission within 30 days, and mortality?
Methods
This study was approved by the Institutional Review Board of Yonsei University Health System (Y-2020-0178). All methods were performed in accordance with the relevant guidelines and regulations, and informed consent was not required because anonymized data was used.
Study design and participants
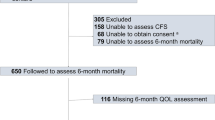
Between September 2015 and August 2019, this retrospective cohort study analyzed the electronic medical records of patients aged 65 years or older who underwent cancer resection at the Severance Hospital in South Korea. Although the highest incidence of thyroid cancer in Korea, people diagnosed with thyroid cancer were not included in this study because the 5-year relative survival rate was 100%26. Excluding those diagnosed with thyroid cancer, 17,288 patients aged 65 and older were confirmed to have undergone surgery. A total of 5582 patients who did not undergo cancer resection (examination or procedure) were excluded, and the FI-Lab scores of 2690 patients could not be calculated due to missing data. One patient who died on the day of surgery was excluded. The study’s final sample size was 9015 (Fig. 1).
Laboratory frailty index
Frailty was assessed using FI-Lab scores15 generated based on previous reports from the Canadian Study of Health (CSHA)18 and the European Male Aging Study17. Abnormal levels of physiological parameters such as vital signs, routine blood and urine tests including creatinine, potassium, blood sugar, cholesterol, etc., are associated with health conditions and aging-related dysregulation of multiple organ systems (e.g., renal, liver, thyroid, hematological, inflammatory, coagulation, electrolyte)27,28. We identified 32 deficits from common blood test results and vital signs. Preoperative blood test results and vital-sign records measured initially on the day of surgery were used. Each deficit was coded using the normal reference range15 for each of the 32 variables (Appendix 1). If it was outside the normal range, it was assigned a score of “1”; if otherwise, it was assigned a scored as “0.” The FI-Lab score was obtained by summing the variable-deficit scores and dividing the total by the number of variables. For example, a person with a deficit in ten variables and no deficits in the other 21 variables of the 31-item FI-Lab tool would have an FI-lab score of 0.32 (10 divided by 31). FI-Lab scores range from 0 to 1; a higher score indicates greater frailty15,18. Frailty scores were categorized as follows: < 0.25, 0.25–0.4, and > 0.415,19. FI-Lab scores were only calculated for subjects (at least 23 items out of a total of 32 items had to be measured) for whom < 30% of the variables were missing16,18.
Postoperative health outcomes
Surgical outcomes included the following: postoperative LOS, readmission and ICU admission within 30 days after surgery, and overall survival. Based on a database recording secondary postoperative events that occurred within the first 30 days after surgery for surgical quality improvement29, readmissions and ICU admissions were defined within 30 days after surgery this study.
Statistical analysis
The demographic and clinical characteristics of subjects are represented as means, standard deviations (SDs), frequencies and percentages using descriptive statistics. The comparison across groups were used to verify normality with QQ-plot, followed by analysis of variance and chi-square tests. Adjustments were made for age at surgery, sex, number of comorbidities, operating room duration, and cancer stage based on existing literature and clinical importance15,30. Postoperative LOS was defined as the number of days from the operation day to the discharge date, and linear regression analysis was used. Logistic regression analysis was performed in cases of unplanned readmission or ICU admission within 30 days of surgery considered to have an event. After checking assumption of proportionality, the effect of FI-Lab scores on mortality was investigated using Cox’s regression model. The Kaplan–Meier survival curve was plotted by FI-Lab group from the day of surgery to the day of death, and statistical significance was evaluated using the log-rank test. Statistical significance was offset at a two-tailed p value < 0.05. All analyses were conducted using SPSS software (version 26.0; IBM Corp., Armonk, NY, USA).
Results
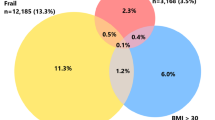
A total of 9015 subjects were included in the analysis. The mean age at the time of surgery was 72.3 years (standard deviation [SD] 5.3), and 65.5% of the patients were men. The FI-Lab mean was 0.20 (SD 0.10). The observed FI-Lab score range was 0.00–0.71; 6291 (69.8%), 2364 (26.2%), and 360 (4%) patients had scores within the “< 0.25”, “0.25 – 0.4”, and “> 0.4” categories, respectively. Of all patients, 47.8% had gastrointestinal cancer, and 17.4% had malignant neoplasms of the genital organs. The higher the FI-Lab score, the greater the frequency of patients with malignant neoplasms of gastrointestinal and genital organs (Table 1).
The mean (SD) postoperative LOS was 8.2 (11.1) days. Higher FI-Lab scores (FI-Lab score of 0.25–0.4: adjusted β 1.41, 95% confidence interval [CI] 0.95–1.88; FI-Lab scores > 0.4: adjusted β 9.45, 95% CI 8.40–10.50) were associated with longer LOS than FI-Lab scores < 0.25 after adjusting for age at surgery, sex, number of comorbidities, operating room duration, and cancer stage (Table 2).
Within 30 days of surgery, 1229 patients (13.6%) were unplanned readmitted. After adjusting for age at surgery, sex, number of comorbidities, operating room duration, and cancer stage, FI-Lab scores of 0.25–0.4 and > 0.4 were associated with readmission after surgery within 30 days (adjusted odds ratio [OR] 1.20, 95% CI 1.04–1.38, and 1.49, 95% CI 1.12–1.98, respectively) compared those > 0.25 (Table 2).
Within 30 days of surgery, 1,170 patients (13.0%) were admitted to the ICU, and the mean (SD) LOS was 2.2 (4.9) days. This outcome was observed in 40.0% (n = 144) and 19.0% (n = 448) of patients with frailty scores in the > 0.40 and 0.25–0.40 categories, respectively; however, it was observed in only 9.2% (n = 578) of patients with frailty scores < 0.25 (p < 0.001; Table 2). In the adjusted analysis, FI-Lab scores of 0.25–0.4 (adjusted OR 1.70, 95% CI 1.47–1.97) and > 0.4 (adjusted OR 3.58, 95% CI 2.77–4.63) were associated with postoperative ICU admission within 30 days (Table 2).
During the follow-up period, 8.0% (n = 725) of the participants died. The mean (range) postoperative follow-up period for survivors was 34.7 (0.1–60.9) months. After adjusting for age at surgery, sex, number of comorbidities, operating room duration, and cancer stage, FI-Lab scores of 0.25–0.4 and > 0.4 were associated with an increased risk of mortality about twice (adjusted hazard ratio [HR] 1.75, 95% CI 1.49–2.06) and four times (adjusted HR 4.29, 95% CI 3.41–5.40), respectively, compared to FI-Lab scores < 0.25 (Table 2; Fig. 2).
Discussion
This study had that patients’ frailty status may serve as an important preoperative indicator of postoperative patient outcomes in older patients undergoing cancer resection. FI-Lab scores, based on 32 routine blood tests and vital signs, were used to assess preoperative frailty in 9015 older patients who underwent cancer resection. A higher FI-Lab score was found to be associated with increased postoperative LOS, unplanned readmission and admission to ICU within 30 days, and mortality risk. Consequently, the FI-Lab score can be regarded as an effective tool as a prognostic factor in elderly patients considering cancer surgery. It also highlights the need to develop and evaluate strategies to improve outcomes by stratifying preoperative frailty to improve outcomes in cancer surgery patients in the presence of frailty.
A few previous studies conducted in surgical settings, it is widely accepted that frailty is a risk factor or unplanned readmission, postoperative complications, and high mortality31,32,33; however, most of them measured clinical frailty. For example, in a 2018 study of patients aged 65 years and older who underwent emergency abdominal surgery, frail patients, as defined using the clinical frailty scale, were predicted to be at four and three times the risk of 30 days and 6 months of readmission or death, respectively8. In the oncologic setting, compared comprehensive geriatric assessment (CGA) and FI, which are widely used for preoperative clinical frailty evaluation in patients with colon cancer. CGA predicted short-term surgical risk and survival, and FI as compared to CGA showed prognostic accuracy in predicting surgical 1-year mortality34. In addition, the modified frailty index derived from the cumulative deficit model was associated with increased major complications and readmissions within 30 days after surgery in colorectal cancer patients35. Few studies have evaluated cancer patient outcomes using the FI-Lab score. In a study of 306 patients aged 65 years and older who were hospitalized in elderly wards, both FI-Lab and clinical frailty scores (FI-CGA) were used20. A clear relationship between the FI-Lab score and mortality was reported, and FI-Lab demonstrated the main characteristics of clinical frailty. In addition, older patients hospitalized in general internal medicine wards found that higher FI-Lab scores were associated with increased hospitalization days, readmission rates, and mortality risk16. Our findings corroborate and expand existing evidence regarding FI-Lab yielded from previous studies conducted in acute care settings.
Some studies have reported that higher FI-Lab scores increase the risk of mortality, even in people with few clinical detectable deficits17,18,22. FI-Lab scores based on biochemical/physiological markers are believed to represent the burden of preclinical or subclinical deficits17. Eastern Cooperative Oncology Group (ECOG) performance status is a widely used method to evaluate the functional status of cancer patients as a major prognostic factor36,37. Performance status selects and stratifies patients for inclusion in treatment trials, and evaluates the quality of survival and prognosis of cancer patients37. In our study, 86% of patients in the group with the highest frailty exhibited grade 0 ECOG Performance Status of fully active persons (able to carry on all pre-disease performance without restriction)37. In a sense, asymptomatic dysregulation measured using FI-Lab, provides intermediate link within cellular level damage, indicating that it can eventually extending to clinically detectable deficits23,38. Therefore, the FI-Lab score is believed to have the potential to identify early-stage frailty before more advanced symptoms develop.
Laboratory testing is an objective measure that does not impose no extra strain on health care providers for data collection. Measured more often when a patient experiences a health condition (e.g., preoperative) that may attract more attention to treat and care39. Abnormalities in laboratory tests may reflect unhealthy conditions and dysfunction of organ systems that contribute to the risk of death. Therefore, preoperative stratification using the FI-Lab can help clinicians monitor patients' medical condition to identify high-risk patients to devise better treatment strategies. It can guide discussions among surgeons, anesthesiologists, patients, and their families to optimize perioperative management, as well as screening the effects of pre-habilitation to reduce vulnerability to surgery and increase patient recovery40,41. Quantifying frailty using FI-Lab may be a useful tool for evaluating frailty in older patients with cancer in various institutions and surgical services, given its ease of use, sensitivity to change and generalizability.
In addition, extensive evidence shows the importance of sex differences in frailty42,43,44. Female are known to have a higher degree of frailty than male at all ages43. Frail female have a higher risk of readmission and lower survival rate than frail male43. However, a recent study estimating sex-specific mortality using frailty index in a population of Korean adults, it was reported that although female had a higher frailty index than male, the survival probability was significantly lower in male than in female44. Perhaps this association suggests that characteristics of biological, behavioral, and social sex may affect biological health outcomes. However, sex differences with frailty in cancer patients have been relatively unexplored. Therefore, further studies are needed to investigate the association between FI-Lab and sex-specific surgical outcomes in elderly cancer patients, and to identify different cut off values for FI-Lab for gender categories45.
This study has certain limitations. First, since all cancer resections, except for thyroid cancer, were targeted, further studies are required to generalize the results to specific cancer. Second, this study analyzed the medical records of a single institution’s comprehensive cancer hospital. Considering surgical specialization, the number of patients, the treatment of older patients with cancer, and other resources that may not be present in other institutions, the association between frailty and surgical outcomes might have been underestimated. Further, in our multivariable model, neoadjuvant or adjuvant treatments (chemotherapy, radiotherapy, etc.) that potentially affect the mortality rate of patients undergoing cancer resection were not included. Future investigation is needed to evaluate the outcome after more homogeneous cancer resection based on the FI-Lab score and neoadjuvant or adjuvant treatment.
It is difficult to assess clinical frailty in acute care hospitals. Our results demonstrated the usefulness of the FI-Lab score, where preoperative frailty proved helpful in the early identification of surgical outcomes. Frailty in older patients, as evaluated by FI-Lab, demonstrated higher risks of hospitalization after cancer resection, ICU admission, unplanned readmission within 30 days, and death. This indicates the possibility of evaluating a surgical patient’s frailty more accurately and optimizing the feasibility of surgery. Moreover, our findings motivate further research in this area.
Data availability
The datasets generated during and analyzed during the current study are not publicly available due to medical records but are available from the corresponding author on reasonable request.
References
Korc-Grodzicki, B. et al. Surgical considerations in older adults with cancer. J. Clin. Oncol. 32, 2647–2653 (2014).
Fried, L. P. et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 56, M146-156 (2001).
Clegg, A., Young, J., Iliffe, S., Rikkert, M. O. & Rockwood, K. Frailty in elderly people. Lancet 381, 752–762 (2013).
Handforth, C. et al. The prevalence and outcomes of frailty in older cancer patients: A systematic review. Ann. Oncol. 26, 1091–1101 (2015).
Morley, J. E. et al. Frailty consensus: A call to action. J. Am. Med. Dir. Assoc. 14, 392–397 (2013).
Joseph, B. et al. Superiority of frailty over age in predicting outcomes among geriatric trauma patients: A prospective analysis. JAMA Surg. 149, 766–772 (2014).
Rocha, V., Marmelo, F., Leite-Moreira, A. & Moreira-Gonçalves, D. Clinical utility of frailty scales for the prediction of postoperative complications: Systematic review and meta-analysis. Rev. Port. Cir. Cardiotorac. Vasc. 24, 132 (2017).
Li, Y. et al. Impact of frailty on outcomes after discharge in older surgical patients: A prospective cohort study. CMAJ 190, E184-e190 (2018).
Lee, K. C. et al. The impact of frailty on long-term patient-oriented outcomes after emergency general surgery: A retrospective cohort study. J. Am. Geriatr. Soc. 68, 1037–1043 (2020).
Rockwood, K. et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 173, 489–495 (2005).
Mitnitski, A. B., Mogilner, A. J. & Rockwood, K. Accumulation of deficits as a proxy measure of aging. Sci. World J. 1, 323–336 (2001).
Rockwood, K., Song, X. & Mitnitski, A. Changes in relative fitness and frailty across the adult lifespan: Evidence from the Canadian National Population Health Survey. CMAJ 183, E487-494 (2011).
Mitnitski, A. B., Graham, J. E., Mogilner, A. J. & Rockwood, K. Frailty, fitness and late-life mortality in relation to chronological and biological age. BMC Geriatr. 2, 1 (2002).
Ghignone, F. et al. The assessment and management of older cancer patients: A SIOG surgical task force survey on surgeons’ attitudes. Eur J Surg Oncol 42, 297–302 (2016).
Blodgett, J. M., Theou, O., Howlett, S. E. & Rockwood, K. A frailty index from common clinical and laboratory tests predicts increased risk of death across the life course. Geroscience 39, 447–455 (2017).
Ellis, H. L. et al. Complementing chronic frailty assessment at hospital admission with an electronic frailty index (FI-Laboratory) comprising routine blood test results. CMAJ 192, E3-e8 (2020).
Blodgett, J. M., Theou, O., Howlett, S. E., Wu, F. C. & Rockwood, K. A frailty index based on laboratory deficits in community-dwelling men predicted their risk of adverse health outcomes. Age Ageing 45, 463–468 (2016).
Howlett, S. E., Rockwood, M. R., Mitnitski, A. & Rockwood, K. Standard laboratory tests to identify older adults at increased risk of death. BMC Med. 12, 171 (2014).
Bello, G. A. et al. Development of a physiological frailty index for the World Trade Center General Responder Cohort. Curr. Gerontol. Geriatr. Res. 2018, 3725926 (2018).
Ritt, M., Jäger, J., Ritt, J. I., Sieber, C. C. & Gaßmann, K. G. Operationalizing a frailty index using routine blood and urine tests. Clin. Interv. Aging 12, 1029–1040 (2017).
Sohn, B. et al. Frailty index is associated with adverse outcomes after aortic valve replacement in elderly patients. J. Korean Med. Sci. 34, e205 (2019).
Klausen, H. H. et al. Association between routine laboratory tests and long-term mortality among acutely admitted older medical patients: A cohort study. BMC Geriatr. 17, 62 (2017).
Rockwood, K., McMillan, M., Mitnitski, A. & Howlett, S. E. A frailty index based on common laboratory tests in comparison with a clinical frailty index for older adults in long-term care facilities. J. Am. Med. Dir. Assoc. 16, 842–847 (2015).
Shaw, J. F., Budiansky, D., Sharif, F. & McIsaac, D. I. The association of frailty with outcomes after cancer surgery: A systematic review and metaanalysis. Ann. Surg. Oncol. https://doi.org/10.1245/s10434-021-11321-2 (2022).
Fagard, K. et al. The impact of frailty on postoperative outcomes in individuals aged 65 and over undergoing elective surgery for colorectal cancer: A systematic review. J. Geriatr. Oncol. 7, 479–491 (2016).
National Cancer Information Center. Cancer Prevalence. https://www.cancer.go.kr/ (2020).
Li, Q. et al. Homeostatic dysregulation proceeds in parallel in multiple physiological systems. Aging Cell 14, 1103–1112 (2015).
Searle, S. D., Mitnitski, A., Gahbauer, E. A., Gill, T. M. & Rockwood, K. A standard procedure for creating a frailty index. BMC Geriatr. 8, 24 (2008).
Strong, V. E. et al. Development and assessment of Memorial Sloan Kettering Cancer Center’s Surgical Secondary Events grading system. Ann. Surg. Oncol. 22, 1061–1067 (2015).
Shahrokni, A. et al. Development and evaluation of a new frailty index for older surgical patients with cancer. JAMA Netw. Open 2, e193545 (2019).
Sioutas, G. & Tsoulfas, G. Frailty assessment and postoperative outcomes among patients undergoing general surgery. Surgeon 18, e55–e66 (2020).
Anand, A. et al. The relationship between preoperative frailty and outcomes following transcatheter aortic valve implantation: A systematic review and meta-analysis. Eur. Heart J. Qual. Care Clin. Outcomes 3, 123–132 (2017).
Ornaghi, P. I. et al. Frailty impact on postoperative complications and early mortality rates in patients undergoing radical cystectomy for bladder cancer: A systematic review. Arab. J. Urol. 19, 9–23 (2020).
Giannotti, C. et al. Frailty assessment in elective gastrointestinal oncogeriatric surgery: Predictors of one-year mortality and functional status. J. Geriatr. Oncol. 10, 716–723 (2019).
Gearhart, S. L., Do, E. M., Owodunni, O., Gabre-Kidan, A. A. & Magnuson, T. Loss of independence in older patients after operation for colorectal cancer. J. Am. Coll. Surg. 230, 573–582 (2020).
Oken, M. M. et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am. J. Clin. Oncol. 5, 649–655 (1982).
Buccheri, G., Ferrigno, D. & Tamburini, M. Karnofsky and ECOG performance status scoring in lung cancer: A prospective, longitudinal study of 536 patients from a single institution. Eur. J. Cancer 32a, 1135–1141 (1996).
Zaslavsky, O. et al. Frailty: A review of the first decade of research. Biol. Res. Nurs. 15, 422–432 (2013).
Hripcsak, G., Albers, D. J. & Perotte, A. Parameterizing time in electronic health record studies. J. Am. Med. Inform. Assoc. 22, 794–804 (2015).
Gill, T. M. et al. A prehabilitation program for physically frail community-living older persons. Arch. Phys. Med. Rehabil. 84, 394–404 (2003).
Nidadavolu, L. S., Ehrlich, A. L., Sieber, F. E. & Oh, E. S. Preoperative evaluation of the frail patient. Anesth. Analg. 130, 1493–1503 (2020).
Hoogendijk, E. O. et al. Operationalization of a frailty index among older adults in the InCHIANTI study: Predictive ability for all-cause and cardiovascular disease mortality. Aging Clin. Exp. Res. 32, 1025–1034 (2020).
Zhang, Q., Guo, H., Gu, H. & Zhao, X. Gender-associated factors for frailty and their impact on hospitalization and mortality among community-dwelling older adults: A cross-sectional population-based study. PeerJ 6, e4326 (2018).
Baek, W. & Min, A. Frailty index and gender-specific mortality in Korean adults: Findings from the Korean Longitudinal Study of Aging (2006–2018). J. Adv. Nurs. https://doi.org/10.1111/jan.15168 (2022).
Morley, J. E., Malmstrom, T. K. & Miller, D. K. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J. Nutr. Health Aging 16, 601–608 (2012).
Acknowledgements
This work was supported by the Student-Faculty Research Grant of Yonsei University College of Nursing [6-2020-0197] to YK and HL, and Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education [No. 2020R1A6A1A03041989] to KS and HL.
Author information
Authors and Affiliations
Contributions
Y.K. and H.L. contributed to the design and conception of the study. Y.K., K.S., C.M.K. and H.L. contributed to study implementation and analysis of the results. Y.K. and H.L. wrote the manuscript. Y.K., K.S., C.M.K. and H.L. reviewed the manuscript and provided revisions. All authors contributed to the article and read and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, Y., Song, K., Kang, C.M. et al. Impact of preoperative laboratory frailty index on mortality and clinical outcomes in older surgical patients with cancer. Sci Rep 12, 9200 (2022). https://doi.org/10.1038/s41598-022-13426-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-13426-4
This article is cited by
-
Developing and validating an electronic health record-based frailty index in pre-operative settings using machine learning
Journal of Intelligent Information Systems (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.