Abstract
Background
To investigate the effect of frailty on short-term postoperative outcomes in patients with prostate cancer treated with radical prostatectomy (RP).
Methods
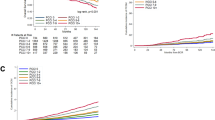
Within the National Inpatient Sample database, we identified 91,618 RP patients treated between 2008 and 2015. The Johns Hopkins Adjusted Clinical Groups frailty-defining indicator was applied, and we examined the rates of frailty over time, as well as its effect on overall complications, major complications, nonhome-based discharge, length of stay (LOS), and total hospital charges (THCs). Time trends and multivariable logistic, Poisson and linear regression models were applied.
Results
Overall, 12,185 (13.3%) patients were frail. Rates of frail patients increased over time (from 10.3 to 18.2%; p < 0.001). Frail patients had higher rates of overall complications (16.6 vs. 8.6%), major complications (4.9 vs. 2.6%), nonhome-based discharge (5.9 vs. 5%), longer LOS (2 vs. 1), and higher THCs ($37,186 vs. $35,241) (all p < 0.001). Moreover, frailty was an independent predictor of overall complications (OR: 1.95), major complications (OR: 1.76), nonhome-based discharge (OR: 1.20), longer LOS (RR: 1.19), and higher THCs (RR: $3160) (all p < 0.001). Of frail patients, 10,418 (85.5%) neither exhibited body mass index ≥ 30 nor Charlson comorbidity index ≥ 2.
Conclusions
On average, every seventh RP patient is frail and that proportion is on the rise. Frail individuals are at higher risk of adverse short-term postoperative outcomes, that cannot be predicted by other risk factors, such as obesity or comorbidities.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Code availability
The data that support the findings of this study are openly available in the Surveillance, Epidemiology, and End Results Program at https://seer.cancer.gov.
References
Canda AE, Tilki D, Mottrie A. Rectal injury during radical prostatectomy: focus on robotic surgery. Eur Urol Oncol. 2018;1:507–9.
Johansson E, Steineck G, Holmberg L, Johansson J-E, Nyberg T, Bill-Axelson A, et al. Quality of life after radical prostatectomy or watchful waiting with or without androgen deprivation therapy: the SPCG-4 randomized trial. Eur Urol Oncol. 2018;1:134–42.
Gandaglia G, Bravi CA, Dell’Oglio P, Mazzone E, Fossati N, Scuderi S, et al. The impact of implementation of the European Association of Urology Guidelines Panel recommendations on reporting and grading complications on perioperative outcomes after robot-assisted radical prostatectomy. Eur Urol. 2018;74:4–7.
Knipper S, Mazzone E, Mistretta FA, Palumbo C, Tian Z, Briganti A, et al. Impact of obesity on perioperative outcomes at robotic-assisted and open radical prostatectomy: results from the National Inpatient Sample. Urology. 2019;133:135–44.
Monn MF, Jaqua KR, Calaway AC, Mellon MJ, Koch MO, Boris RS. Impact of obesity on wound complications following radical prostatectomy is mitigated by robotic technique. J Endourol. 2016;30:890–5.
Vidal AC, Howard LE, Sun SX, Cooperberg MR, Kane CJ, Aronson WJ, et al. Obesity and prostate cancer-specific mortality after radical prostatectomy: results from the Shared Equal Access Regional Cancer Hospital (SEARCH) database. Prostate Cancer Prostatic Dis. 2017;20:72–8.
Maj-Hes AB, Mathieu R, Özsoy M, Soria F, Moschini M, Abufaraj M, et al. Obesity is associated with biochemical recurrence after radical prostatectomy: a multi-institutional extended validation study. Urol Oncol. 2017;35:460.e1–8.
Sivaraman A, Ordaz Jurado G, Cathelineau X, Barret E, Dell’Oglio P, Joniau S, et al. Older patients with low Charlson score and high-risk prostate cancer benefit from radical prostatectomy. World J Urol. 2016;34:1367–72.
Lee JY, Kang HW, Rha KH, Cho NH, Choi YD, Hong SJ, et al. Age-adjusted Charlson comorbidity index is a significant prognostic factor for long-term survival of patients with high-risk prostate cancer after radical prostatectomy: a Bayesian model averaging approach. J Cancer Res Clin Oncol. 2016;142:849–58.
Froehner M, Koch R, Litz RJ, Oehlschlaeger S, Twelker L, Hakenberg OW, et al. Detailed analysis of Charlson comorbidity score as predictor of mortality after radical prostatectomy. Urology. 2008;72:1252–7.
Briganti A, Fossati N, Catto JWF, Cornford P, Montorsi F, Mottet N, et al. Active surveillance for low-risk prostate cancer: the European Association of Urology position in 2018. Eur Urol. 2018;74:357–68.
Wilt TJ, Brawer MK, Jones KM, Barry MJ, Aronson WJ, Fox S, et al. Radical prostatectomy versus observation for localized prostate cancer. N Engl J Med. 2012;367:203–13.
Sandini M, Pinotti E, Persico I, Picone D, Bellelli G, Gianotti L. Systematic review and meta-analysis of frailty as a predictor of morbidity and mortality after major abdominal surgery. BJS Open. 2017;1:128–37.
McIsaac DI, Bryson GL, van Walraven C. Association of frailty and 1-year postoperative mortality following major elective noncardiac surgery: a population-based cohort study. JAMA Surg. 2016;151:538–45.
Palumbo C, Knipper S, Pecoraro A, Rosiello G, Luzzago S, Deuker M, et al. Patient frailty predicts worse perioperative outcomes and higher cost after radical cystectomy worse radical cystectomy outcomes in frails. Surg Oncol. 2019;32:8–13.
Taylor BL, Xia L, Guzzo TJ, Scherr DS, Hu JC. Frailty and greater health care resource utilization following major urologic oncology surgery. Eur Urol Oncol. 2019;2:21–7.
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet Lond Engl. 2013;381:752–62.
The Johns Hopkins ACG® system excerpt from version 11.0 technical reference guide. 2015. p. 36. https://www.healthpartners.com/ucm/groups/public/@hp/@public/documents/documents/cntrb_035024.pdf.
Barashi NS, Pearce SM, Cohen AJ, Pariser JJ, Packiam VT, Eggener SE. Incidence, risk factors, and outcomes for rectal injury during radical prostatectomy: a population-based study. Eur Urol Oncol. 2018;1:501–6.
Zaffuto E, Bandini M, Moschini M, Leyh-Bannurah S-R, Gazdovich S, Dell’Oglio P, et al. Location of metastatic bladder cancer as a determinant of in-hospital mortality after radical cystectomy. Eur Urol Oncol. 2018;1:169–75.
National (Nationwide) Inpatient Sample (NIS). 2019. https://www.hcup-us.ahrq.gov/news/exhibit_booth/nis_brochure.jsp.
Development and evaluation of the Johns Hopkins University risk adjustment models for Medicare+Choice plan payment. Johns Hopkins ACG® System. 2019. https://www.hopkinsacg.org/document/development-and-evaluation-of-the-johns-hopkins-university-risk-adjustment-models-for-medicarechoice-plan-payment/.
Kim DH, Schneeweiss S. Measuring frailty using claims data for pharmacoepidemiologic studies of mortality in older adults: evidence and recommendations. Pharmacoepidemiol Drug Saf. 2014;23:891–901.
Sternberg SA, Bentur N, Abrams C, Spalter T, Karpati T, Lemberger J, et al. Identifying frail older people using predictive modeling. Am J Manag Care. 2012;18:e392–7.
Nieman CL, Pitman KT, Tufaro AP, Eisele DW, Frick KD, Gourin CG. The effect of frailty on short-term outcomes after head and neck cancer surgery: frailty and outcomes in head and neck surgery. Laryngoscope. 2018;128:102–10.
WHO | Obesity. 2019. https://www.who.int/topics/obesity/en/.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9.
Palumbo C, Knipper S, Dzyuba-Negrean C, Pecoraro A, Rosiello G, Tian Z, et al. Complication rates, failure to rescue and in-hospital mortality after cytoreductive nephrectomy in the older patients. J Geriatr Oncol. 2019:S1879406819301961. (in press).
Adedayo P, Resnick K, Singh S. Preoperative frailty is a risk factor for non-home discharge in patients undergoing surgery for endometrial cancer. J Geriatr Oncol. 2018;9:513–5.
HCUP-US NIS Overview. 2019. https://www.hcup-us.ahrq.gov/nisoverview.jsp.
Suskind AM, Walter LC, Jin C, Boscardin J, Sen S, Cooperberg MR, et al. Impact of frailty on complications in patients undergoing common urological procedures: a study from the American College of Surgeons National Surgical Quality Improvement database. BJU Int. 2016;117:836–42.
Levy I, Finkelstein M, Bilal KH, Palese M. Modified frailty index associated with Clavien-Dindo IV complications in robot-assisted radical prostatectomies: a retrospective study. Urol Oncol. 2017;35:425–31.
Acknowledgements
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Rosiello, G., Palumbo, C., Knipper, S. et al. Preoperative frailty predicts adverse short-term postoperative outcomes in patients treated with radical prostatectomy. Prostate Cancer Prostatic Dis 23, 573–580 (2020). https://doi.org/10.1038/s41391-020-0225-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-020-0225-3
This article is cited by
-
Comprehensive geriatric assessment predicts radiation-induced acute toxicity in prostate cancer patients
Strahlentherapie und Onkologie (2024)
-
The 5-Factor Modified Frailty Index is effective in treatment decision and the determination of perioperative complications in patients with localized prostate cancer
Supportive Care in Cancer (2023)
-
Does the 5-item Frailty Index predict surgical complications of endoscopic surgical management for benign prostatic obstruction? An analysis of the ACS-NSQIP
World Journal of Urology (2022)