Abstract
Posterior cruciate ligament (PCL) reconstruction can be performed using single bundle (SB) and double bundle (DB) techniques. The present study investigated whether DB PCL reconstruction is superior to SB reconstruction in terms of patient reported outcome measures (PROMs) and joint stability. In December 2021 Embase, Google Scholar, Pubmed, Scopus databases were accessed. All clinical trials comparing SB versus DB reconstruction to address PCL insufficiency in skeletally mature patients were considered. Data from 483 procedures were retrieved. The mean follow-up was 31.0 (28.0 to 107.6) months, and the mean timespan between injury and surgery was 11.3 (6 to 37) months. The mean age of the patients was 29.3 ± 3.8 years. 85 of 483 patients (18%) were women. At a mean of 31.0 months post reconstruction, ROM (P = 0.03) was slightly greater in the SB group, while the Tegner score (P = 0.03) and the Telos stress (P = 0.04) were more favorable in the DB cohort. Similarity was found in instrumental laxity (P = 0.4) and Lysholm score (P = 0.3). The current evidence does not support the use of DB techniques for PCL reconstruction. Both methods could restore knee stability and motion with satisfactory short term patient reported outcome measures. Further high quality clinical trials are required to validate these results on a larger scale.
Similar content being viewed by others
Introduction
The posterior cruciate ligament (PCL) restrains posterior tibial translation, preventing external rotation of the tibia1,2. The PCL inserts on the intercondylar eminence of the tibia through an anterolateral and a posteromedial bundle1,2. These bundles have distinct fibres orientation and tensioning patterns throughout the range of motion of the knee3,4,5,6. The two bundles synergistically stabilize the knee during the whole range of motion4,7,8,9. The anterolateral bundle is more tense in flexion, and the posteromedial bundle is more tense in extension10,11. The anterolateral bundle plays an important role in constraining the mediolateral translation, while the posteromedial bundle controls the anteroposterior translation of the tibia on the femur7. An isolated rupture of either bundle does not result in a clinically significant laxity8,12,13,14. On the other hand, when both bundles are injured, the PCL can no longer stabilize the joint, and, if clinical evident instability develops, surgical reconstruction may be indicated15,16,17,18,19. Both single bundle (SB) and double bundle (DB) techniques for PCL reconstruction have been described20,21,22,23. The DB reconstruction technique should more closely replicate the two native bundles of the PCL and the physiological biomechanics of the knee joint. Biomechanically, DB reconstruction better restores the antero-posterior stability than SB techniques24,25. However, it is unclear whether DB PCL reconstruction results in better stability and patient reported outcome measures (PROMs) than the SB technique26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43. There are no guidelines in support of the number of PCL bundles to reconstruct when undertaking procedure to restore stability. Results from previous meta-analyses and systematic reviews on the topic are inconsistent44,45,46,47. Recently, clinical studies including a large population which were not been considered in previous reviews have been published46,48,49. Increasing pooling data may support clinicians to choose the appropriate treatment for PCL reconstruction. Thus, a meta-analysis was conducted to investigate whether DB PCL reconstruction is superior to the SB technique in terms of patient reported outcome measures (PROMs) and joint stability. We hypothesised that, though DB PCL reconstruction is believed to achieve better knee biomechanics, it does not results in better outcomes following reconstruction of the PCL.
Material and methods
Search strategy
This meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA guidelines50. The PICO algorithm was followed:
-
P (Population): PCL tears;
-
I (Intervention): isolated PCL reconstruction;
-
C (Comparison): SB versus DB;
-
O (Outcomes): PROMs and stability.
Data source and extraction
Two authors (F.M. and A.P.) independently performed the literature search in December 2021. The PubMed, Embase, Scopus and Google Scholar electronic databases were accessed. The following keywords were used in combination: knee, posterior cruciate ligament, pcl, reconstruction, arthroscopy, bundle, double, single, strand, clinical outcome, injury, isolated, tendon, hamstring, quadriceps, achilles, tibialis anterior, PROMs, patient reported outcome measures, stability, laxity, complication, instability. If the title and abstract matched the topic, the full-text of the article was accessed. The bibliographies were screened to identify additional articles. Disagreements were resolved by a third author (N.M.).
Eligibility criteria
All the clinical studies comparing SB versus DB for PCL reconstruction were accessed. Given the authors language capabilities, articles in English, German, Italian, French and Spanish were eligible. Articles with Level I to IV of evidence, according to Oxford Centre of Evidence-Based Medicine51, were considered. Editorials, cohort studies, systematic reviews and meta-analyses, technical notes, narrative reviews, expert opinion and letters were excluded. Animal, biomechanics, and cadaveric studies were also excluded. Articles combining PCL with anterior cruciate ligament (ACL) reconstruction were excluded, as were studies on multiligament injuries. Only studies reporting a minimum of 12 months follow-up were included. Studies involving skeletally immature patients were not eligible. Only articles reporting quantitative data under the outcomes of interest were considered for inclusion.
Outcomes of interest
Two authors (F.M. and A.P.) independently performed data extraction. The following data were collected: generalities (author, year, type of study), demographic baseline (number of samples, mean age), mean follow-up, time from injury to surgery, type of graft. Data concerning the following outcomes of interest were collected: Lysholm Knee Scoring score, Tegner activity score, visual analogue scale (VAS), IKDC, range of motion (ROM), grade of displacement (Telos stress radiography, KT-1000/2000 arthrometer).
Methodology quality assessment
The methodological quality assessment was performed by a single author (A.P.) using the Coleman Methodology Score (CMS) The CMS is a reliable and validated tool to evaluate the methodological quality of articles included in systematic reviews and meta-analyses52, evaluating the population size, length of follow-up, surgical approach used, study design, description of diagnosis, surgical technique, and rehabilitation. Additionally, outcome criteria assessment and the subject selection process were also evaluated. The quality of the studies is scored between 0 (poor) and 100 (excellent), with values > 60 considered satisfactory.
Statistical analysis
The statistical analyses were performed by the main author (F.M.). To assess baseline comparability, the unpaired t-test was performed using the IBM SPSS version 25. Values of P > 0.05 indicated similarity between the two groups. The meta-analyses were performed using the Editorial Manager Software version 5.3 (The Nordic Cochrane Collaboration, Copenhagen). Continuous data were analyzed using the inverse variance method, with mean difference (MD) effect measure. Dichotomic data were analyzed using the Mantel–Haenszel method and odd ratio (OR) effect measure. The confidence interval was set at 95% in all the comparison. A fixed model effect was set as default. If moderate or high heterogeneity was detected, a random model effect was adopted. Heterogeneity was evaluated through Higgins-I2 and \(\chi\) 2 tests. Values of Higgins-I2 were interpreted as low (< 30%), moderate (30% to 60%), high (> 60%). Forest and funnel plot were performed. Values of P > 0.05 were considered statistically significant.
Ethical approval
This study complies with ethical standards.
Results
Search result
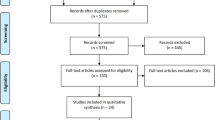
The literature search resulted in 175 articles. After removal of duplicates (N = 57), a further 118 articles were not eligible: language limitations (N = 3), study design (N = 85), combined PCL/ACL reconstruction (N = 7), involving skeletally immature patients (N = 2), short follow-up (N = 6), lacking of quantitative data under the endpoints of interest (N = 15). Finally, 10 comparative clinical studies were included in the present investigation: three randomized controlled trials, one prospective investigation, and six retrospective cohort studies. The literature search results are shown in Fig. 1.
Methodological quality assessment
According to the CMS, the study size and length of follow-up were adequate. Surgical approach, diagnosis, and rehabilitation were well described in most articles. Outcome measures and timing of assessment were frequently defined, providing moderate reliability. The procedures for assessing outcomes, along with subject selection were often biased and poorly described. Concluding, the CMS scored 49.7 points, attesting the fair quality of the methodological assessment of the articles included in the present meta-analysis (Table 1).
Risk of publication bias
The funnel plot of the most commonly reported outcome (Lysholm score) was used to investigate the risk of publication bias. The plot evidenced a very good symmetrical disposition of the referral points. No study was located outside the shapes, increasing the reliability of the plot. Concluding, the risk of publication bias was low (Fig. 2).
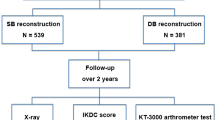
Patient demographics
Data from 483 procedures were retrieved. The mean follow-up was 31.0 ± 49.4 months, and the mean timespan between injury and surgery was 11.3 ± 39.1 months. The mean age of the patients was 29.3 ± 3.8 years. 85 of 483 patients (18%) were women. Good comparability was found at baseline between the two groups in terms of length of follow-up (P = 0.9), timespan form injury to surgery (P = 0.9), mean age (P = 0.4), women (P = 0.08), Lysholm scale (P = 0.7), ROM (P = 0.6), Tegner (P = 0.9), Telos stress radiography (P = 0.7), arthrometer laxity (P = 0.9). Generalities and baseline characteristics of the included studies are shown in Table 2.
Outcomes of interest
ROM (MD 2.00; 95% CI 0.22, 3.78; P = 0.03) was greater in the SB group, while the Tegner score (MD − 0.46; 95% CI − 0.87, − 0.05; P = 0.03) and the Telos stress (MD 0.57; 95% CI 0.03, 1.10; P = 0.04), were favorable in the DB cohort. Similarity was found between the techniques in terms of instrumental laxity (MD 0.88; 95% CI − 0.96, 2.71; P = 0.4) and Lysholm score (MD − 0.77; 95% CI − 2.14 0.60; P = 0.3). The forest plots of each comparison are shown in Fig. 3.
Discussion
This meta-analysis confirmed our hypothesis of similarity between PCL reconstruction using a SB or a DB graft. DB evidenced minimally greater Telos stress and Tegner score, along with a slightly lower range of motion than the SB. No difference was found in the instrumental laxity and Lysholm score.
The Tegner activity scale is a validated PROM to evaluate the level of activity of the patients53,54,55. Stress radiographs with the Telos stress device are widely employed to evaluate laxity of cruciate ligaments56,57,58. Our results indicated that the Tegner score and the results of the Telos stress were favorable in to the DB cohort; however, the clinical impact of these differences was minimal. Indeed, the MD between the two groups did not overcome the minimum clinically important difference of the Tegner scale, which was estimated between 0.5 and 1 point59,60,61. The instrumental laxity using the AK-1000/2000 and the functional assessment using Lysholm score were also similar, suggesting comparability between the two techniques. Several biomechanical studies stated that DB PCL reconstruction better restore antero-posterior stability than SB techniques9,12,24,25,62,63,64,65. A recent biomechanical study demonstrated that a DB PCL reconstruction could better restore knee stability across the full ROM, while SB leads to high graft tension during extension and laxity during flexion66. Harner et al.8 evaluated SB and DB transtibial PCL reconstructions in a cadaveric setting, concluding that DB reconstruction could mimic more closely the physiological knee biomechanics. These results explain partially the findings of the present study. DB reconstruction achieves greater stability according to the Telos stress test, allowing patients to increase their activity level or to quickly return to preinjury level of activity67, but also reducing the range of motion. However, the clinical relevance of these findings is questionable, especially in light of the similarity evidenced by the Lysholm score and instrumental laxity. Concluding, even though biomechanical results are encouraging, the clinical outcomes are similar for SB and DB PCL reconstruction. To establish the optimal number of bundles which should be reconstructed, the rate of complications should be investigated. Given the lack of quantitative data concerning the rate of complications experienced by patients after SB and DB PCL reconstruction, no further analyses can be inferred. Only two studies reported data concerning complications after PCL reconstruction surgery48,49. Jain et al.49 reported four patients with residual laxity and persistent sensation of instability in the SB group; however, only the 5% (1 of 22 patients) underwent revision surgery. Yoon et al.48 reported that four patients underwent additional surgeries: one in the SB, and three in DB group. In clinical practice, DB PCL reconstruction present some disadvantages which are worthy of discussion. DB techniques theoretically expose the patients to higher risk of complications, as four drill holes and four fixation devices are required, and pitfalls are possible. Moreover, surgeons must be aware that revision surgery after DB failure may be challenging. Indeed, removal of DB grafts results in bigger bone defects than in SB reconstruction: they can necessitate larger implants for revision, two stage surgeries, higher costs and patient morbidity. Thus, given the similar outcomes, a SB PCL reconstruction may be encouraged as primary choice. It is unclear whether DB should be reserved for revision surgeries.
The retrospective nature of most of the included studies is an important limitation of this eneavour. Unfortunately, only three studies were randomized clinical trials68,69,70, which represents an important source of selection bias. Eligibility criteria and allocation concealment between SB and DB were not clearly stated, and often biased by the studies. The analyses were conducted irrespective of the type of graft used for reconstruction and the tensioning protocol associated with the procedure, representing other important limitations. Instrumental laxity was evaluated regardless to the type of arthrometer (KT-1000 and/or 2000); however, both the instruments provide a static force to the translational displacement of 134 N. The difference between the two instruments is the duration of the test (KT-1000: 2 min and 15 s versus KT-2000: 2 min and 3 s), and the methodology of saving the resulting data (KT-1000: manual versus KT-2000: digital). Postoperative rehabilitation pattern may also change the biomechanical results, especially at last follow up71. However, the rehabilitation process was often biased, and only minimal between-group differences were detectable. Given these limitations, the results from the present study must be interpreted with caution. Finally, further high-quality clinical trials providing long-term follow-up are strongly recommended to establish whether this minimal greater stability affects chondral degeneration, secondary meniscus lesions, onset of osteoarthritis, and to establish the rate of complications of failure of the two bundles.
Conclusion
Current evidence does not support the use of DB techniques for PCL reconstruction. Both methods could restore knee stability and motion with satisfactory short term patient reported outcome measures. Further high quality clinical trials are required to validate these results on a larger scale.
Data availability
The datasets generated during and/or analysed during the current study are available throughout the manuscript.
References
Arthur, J. R., Haglin, J. M., Makovicka, J. L. & Chhabra, A. Anatomy and biomechanics of the posterior cruciate ligament and their surgical implications. Sports Med. Arthrosc. Rev. 28(1), e1–e10. https://doi.org/10.1097/JSA.0000000000000267 (2020).
LaPrade, C. M., Civitarese, D. M., Rasmussen, M. T. & LaPrade, R. F. Emerging updates on the posterior cruciate ligament: A review of the current literature. Am. J. Sports Med. 43(12), 3077–3092. https://doi.org/10.1177/0363546515572770 (2015).
Tucker, C. J., Joyner, P. W. & Endres, N. K. Single versus double-bundle PCL reconstruction: Scientific rationale and clinical evidence. Curr. Rev. Musculoskelet Med. 11(2), 285–289. https://doi.org/10.1007/s12178-018-9486-z (2018).
Ahmad, C. S. et al. Codominance of the individual posterior cruciate ligament bundles. An analysis of bundle lengths and orientation. Am. J. Sports Med. 31(2), 221–225. https://doi.org/10.1177/03635465030310021101 (2003).
Edwards, A., Bull, A. M. & Amis, A. A. The attachments of the fiber bundles of the posterior cruciate ligament: An anatomic study. Arthroscopy 23(3), 284–290. https://doi.org/10.1016/j.arthro.2006.11.005 (2007).
Forsythe, B. et al. Topography of the femoral attachment of the posterior cruciate ligament. Surgical technique. J. Bone Joint Surg. Am. 91, 89–100. https://doi.org/10.2106/JBJS.H.01514 (2009).
Papannagari, R. et al. Function of posterior cruciate ligament bundles during in vivo knee flexion. Am. J. Sports Med. 35(9), 1507–1512. https://doi.org/10.1177/0363546507300061 (2007).
Harner, C. D. et al. Biomechanical analysis of a double-bundle posterior cruciate ligament reconstruction. Am. J. Sports Med. 28(2), 144–151. https://doi.org/10.1177/03635465000280020201 (2000).
Kennedy, N. I. et al. Posterior cruciate ligament graft fixation angles, part 2: Biomechanical evaluation for anatomic double-bundle reconstruction. Am. J. Sports Med. 42(10), 2346–2355. https://doi.org/10.1177/0363546514541226 (2014).
Sekiya, J. K. et al. Clinical outcomes after isolated arthroscopic single-bundle posterior cruciate ligament reconstruction. Arthroscopy 21(9), 1042–1050. https://doi.org/10.1016/j.arthro.2005.05.023 (2005).
Lee, D. C., Shon, O. J., Kwack, B. H. & Lee, S. J. Proprioception and clinical results of anterolateral single-bundle posterior cruciate ligament reconstruction with remnant preservation. Knee Surg. Relat. Res. 25(3), 126–132. https://doi.org/10.5792/ksrr.2013.25.3.126 (2013).
Kennedy, N. I. et al. Posterior cruciate ligament graft fixation angles, part 1: Biomechanical evaluation for anatomic single-bundle reconstruction. Am. J. Sports Med. 42(10), 2338–2345. https://doi.org/10.1177/0363546514541225 (2014).
Petrillo, S., Volpi, P., Papalia, R., Maffulli, N. & Denaro, V. Management of combined injuries of the posterior cruciate ligament and posterolateral corner of the knee: A systematic review. Br. Med. Bull. 123(1), 47–57. https://doi.org/10.1093/bmb/ldx014 (2017).
Papalia, R., Osti, L., Del Buono, A., Denaro, V. & Maffulli, N. Tibial inlay for posterior cruciate ligament reconstruction: A systematic review. Knee 17(4), 264–269. https://doi.org/10.1016/j.knee.2010.02.006 (2010).
Razi, M. et al. Allograft or autograft in skeletally immature anterior cruciate ligament reconstruction: A prospective evaluation using both partial and complete transphyseal techniques. J. Orthop. Surg. Res. 14(1), 85. https://doi.org/10.1186/s13018-019-1128-7 (2019).
Xue, X. H., Lin, J., Qi, W. H. & Pan, X. Y. A technique combining “U” shape suture and shared tunneling to treat the posterior cruciate ligament rupture and posterior root tears of the medial meniscus. J. Orthop. Surg. Res. 13(1), 265. https://doi.org/10.1186/s13018-018-0973-0 (2018).
Deng, Z., Li, Y., Lin, Z., Zhu, Y. & Zhao, R. The biomechanical and histological effects of posterior cruciate ligament rupture on the medial tibial plateau. J. Orthop. Surg. Res. 12(1), 48. https://doi.org/10.1186/s13018-017-0551-x (2017).
Chan, T. W., Kong, C. C., Del Buono, A. & Maffulli, N. Acute augmentation for interstitial insufficiency of the posterior cruciate ligament. A two to five year clinical and radiographic study. Muscles Ligaments Tendons J. 6(1), 58–63. https://doi.org/10.11138/mltj/2016.6.1.058 (2016).
Del Buono, A., Radmilovic, J., Gargano, G., Gatto, S. & Maffulli, N. Augmentation or reconstruction of PCL? A quantitative review. Knee Surg. Sports Traumatol. Arthrosc. 21(5), 1050–1063. https://doi.org/10.1007/s00167-013-2418-y (2013).
Garofalo, R., Jolles, B. M., Moretti, B. & Siegrist, O. Double-bundle transtibial posterior cruciate ligament reconstruction with a tendon-patellar bone-semitendinosus tendon autograft: Clinical results with a minimum of 2 years’ follow-up. Arthroscopy 22(12), 1331-1338 e1331. https://doi.org/10.1016/j.arthro.2006.08.003 (2006).
Hatayama, K. et al. A comparison of arthroscopic single- and double-bundle posterior cruciate ligament reconstruction: Review of 20 cases. Am. J. Orthop. (Belle Mead NJ) 35(12), 568–571 (2006).
Houe, T. & Jorgensen, U. Arthroscopic posterior cruciate ligament reconstruction: One- vs. two-tunnel technique. Scand J. Med. Sci. Sports 14(2), 107–111. https://doi.org/10.1111/j.1600-0838.2003.00318.x (2004).
Wang, C. J., Weng, L. H., Hsu, C. C. & Chan, Y. S. Arthroscopic single- versus double-bundle posterior cruciate ligament reconstructions using hamstring autograft. Injury 35(12), 1293–1299. https://doi.org/10.1016/j.injury.2003.10.033 (2004).
Lee, D. Y. et al. Biomechanical comparison of single-bundle and double-bundle posterior cruciate ligament reconstruction: A systematic review and meta-analysis. JBJS Rev. 5(10), e6. https://doi.org/10.2106/JBJS.RVW.17.00008 (2017).
Nuelle, C. W. et al. Biomechanical comparison of five posterior cruciate ligament reconstruction techniques. J. Knee Surg. 30(6), 523–531. https://doi.org/10.1055/s-0036-1593625 (2017).
Kang, S. H. et al. Arthroscopic posterior cruciate ligament reconstruction: The achilles tendon allograft versus the quadriceps tendon allograft. J. Knee Surg. 33(6), 553–559. https://doi.org/10.1055/s-0039-1681029 (2020).
Sun, X., Zhang, J., Qu, X. & Zheng, Y. Arthroscopic posterior cruciate ligament reconstruction with allograft versus autograft. Arch. Med. Sci. 11(2), 395–401. https://doi.org/10.5114/aoms.2015.50971 (2015).
Ochiai, S., Hagino, T., Senga, S., Yamashita, T. & Haro, H. Treatment outcome of reconstruction for isolated posterior cruciate injury: Subjective and objective evaluations. J. Knee Surg. 32(6), 506–512. https://doi.org/10.1055/s-0038-1653947 (2019).
Hermans, S., Corten, K. & Bellemans, J. Long-term results of isolated anterolateral bundle reconstructions of the posterior cruciate ligament: A 6- to 12-year follow-up study. Am. J. Sports Med. 37(8), 1499–1507. https://doi.org/10.1177/0363546509333479 (2009).
Setyawan, R., Soekarno, N. R., Asikin, A. I. Z. & Rhatomy, S. Posterior Cruciate Ligament reconstruction with peroneus longus tendon graft: 2-Years follow-up. Ann. Med. Surg. (Lond) 43, 38–43. https://doi.org/10.1016/j.amsu.2019.05.009 (2019).
Norbakhsh, S. T., Zafarani, Z., Najafi, A. & Aslani, H. Arthroscopic posterior cruciate ligament reconstruction by using hamstring tendon autograft and transosseous screw fixation: Minimal 3 years follow-up. Arch. Orthop. Trauma Surg. 134(12), 1723–1730. https://doi.org/10.1007/s00402-014-2082-9 (2014).
Yang, J. H. et al. Second-look arthroscopic assessment of arthroscopic single-bundle posterior cruciate ligament reconstruction: Comparison of mixed graft versus achilles tendon allograft. Am. J. Sports Med. 40(9), 2052–2060. https://doi.org/10.1177/0363546512454532 (2012).
Jackson, W. F., van der Tempel, W. M., Salmon, L. J., Williams, H. A. & Pinczewski, L. A. Endoscopically-assisted single-bundle posterior cruciate ligament reconstruction: Results at minimum ten-year follow-up. J. Bone Joint Surg. Br. 90(10), 1328–1333. https://doi.org/10.1302/0301-620X.90B10.20517 (2008).
Cury Rde, P. et al. Posterior cruciate ligament reconstruction with autograft of the double semitendinosus muscles and middle third of the quadriceps tendon with double femoral and single tibial tunnels: Clinical results in two years follow up. Rev. Bras Ortop. 47(1), 57–65. https://doi.org/10.1016/S2255-4971(15)30346-3 (2012).
Fanelli, G. C. & Edson, C. J. Combined posterior cruciate ligament-posterolateral reconstructions with Achilles tendon allograft and biceps femoris tendon tenodesis: 2- to 10-year follow-up. Arthroscopy 20(4), 339–345. https://doi.org/10.1016/j.arthro.2004.01.034 (2004).
Cury Rde, P. et al. Double-bundle PCL reconstruction using autogenous quadriceps tendon and semitendinous graft: Surgical technique with 2-year follow-up clinical results. Knee 21(3), 763–768. https://doi.org/10.1016/j.knee.2014.02.021 (2014).
Cury, R. P. et al. Double-bundle PCL reconstruction using autologous hamstring tendons: Outcome with a minimum 2-year follow-up. Rev. Bras Ortop. 52(2), 203–209. https://doi.org/10.1016/j.rboe.2017.02.006 (2017).
Saragaglia, D. et al. Posterior cruciate ligament reconstruction for chronic lesions: Clinical experience with hamstring versus ligament advanced reinforcement system as graft. Int. Orthop. 44(1), 179–185. https://doi.org/10.1007/s00264-019-04434-7 (2020).
LaPrade, R. F. et al. Double-bundle posterior cruciate ligament reconstruction in 100 patients at a mean 3 years’ follow-up: Outcomes were comparable to anterior cruciate ligament reconstructions. Am. J. Sports Med. 46(8), 1809–1818. https://doi.org/10.1177/0363546517750855 (2018).
Razi, M. et al. An evaluation of posterior cruciate ligament reconstruction surgery. BMC Musculoskelet Disord. 21(1), 526. https://doi.org/10.1186/s12891-020-03533-6 (2020).
Chen, C. P. et al. Outcomes of arthroscopic double-bundle PCL reconstruction using the LARS artificial ligament. Orthopedics 35(6), e800-806. https://doi.org/10.3928/01477447-20120525-16 (2012).
Min, B. H., Lee, Y. S., Lee, Y. S., Jin, C. Z. & Son, K. H. Evaluation of transtibial double-bundle posterior cruciate ligament reconstruction using a single-sling method with a tibialis anterior allograft. Am. J. Sports Med. 39(2), 374–379. https://doi.org/10.1177/0363546510382207 (2011).
Bait, C. et al. Posterior cruciate ligament reconstruction with “all-inside” technique: A technical note. Muscles Ligaments Tendons J. 4(4), 467–470 (2014).
Zhao, J. X. et al. Outcome of posterior cruciate ligament reconstruction using the single- versus double bundle technique: A meta-analysis. J. Int. Med. Res. 43(2), 149–160. https://doi.org/10.1177/0300060514564474 (2015).
Chahla, J. et al. Single-bundle and double-bundle posterior cruciate ligament reconstructions: A systematic review and meta-analysis of 441 patients at a minimum 2 years’ follow-up. Arthroscopy 33(11), 2066–2080. https://doi.org/10.1016/j.arthro.2017.06.049 (2017).
Xu, M. et al. Double bundle versus single bundle reconstruction in the treatment of posterior cruciate ligament injury: A prospective comparative study. Indian J. Orthop. 53(2), 297–303. https://doi.org/10.4103/ortho.IJOrtho_430_17 (2019).
Qi, Y. S. et al. A systematic review of double-bundle versus single-bundle posterior cruciate ligament reconstruction. BMC Musculoskelet Disord. 17, 45. https://doi.org/10.1186/s12891-016-0896-z (2016).
Yoon, K. H., Kim, E. J., Kwon, Y. B. & Kim, S. G. Minimum 10-year results of single- versus double-bundle posterior cruciate ligament reconstruction: Clinical, radiologic, and survivorship outcomes. Am. J. Sports Med. 47(4), 822–827. https://doi.org/10.1177/0363546518825257 (2019).
Jain, V. et al. A comparative analysis of arthroscopic double-bundle versus single-bundle posterior cruciate ligament reconstruction using hamstring tendon autograft. Arch Orthop Trauma Surg 136(11), 1555–1561. https://doi.org/10.1007/s00402-016-2512-y (2016).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 339, b2535. https://doi.org/10.1136/bmj.b2535 (2009).
Howick, J. C., Glasziou, P., Greenhalgh, T., Carl, H., Liberati, A., Moschetti, I., Phillips, B., Thornton, H., Goddard, O., & Hodgkinson, M. The 2011 Oxford CEBM Levels of Evidence. Oxford Centre for Evidence-Based Medicine Available at http://www.cebm.net/index.aspx?o=5653 (2011)
Coleman, B. D., Khan, K. M., Maffulli, N., Cook, J. L. & Wark, J. D. Studies of surgical outcome after patellar tendinopathy: Clinical significance of methodological deficiencies and guidelines for future studies Victorian. Institute of Sport Tendon Study Group. Scand J. Med. Sci. Sports 10(1), 2–11. https://doi.org/10.1034/j.1600-0838.2000.010001002.x (2000).
Briggs, K. K. et al. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am. J. Sports Med. 37(5), 890–897. https://doi.org/10.1177/0363546508330143 (2009).
Rodriguez-Roiz, J. M., Sastre-Solsona, S., Popescu, D., Montanana-Burillo, J. & Combalia-Aleu, A. The relationship between ACL reconstruction and meniscal repair: Quality of life, sports return, and meniscal failure rate-2- to 12-year follow-up. J. Orthop. Surg. Res. 15(1), 361. https://doi.org/10.1186/s13018-020-01878-1 (2020).
Ren, S. et al. Clinical and radiologic outcomes after a modified bone plug technique with anatomical meniscal root reinsertion for meniscal allograft transplantation and a minimum 18-month follow-up. J. Orthop. Surg. Res. 13(1), 97. https://doi.org/10.1186/s13018-018-0776-3 (2018).
Reverte-Vinaixa, M. M. et al. Outcomes of posterior cruciate ligament tibial avulsion treated with staple fixation: Stress TELOS X-ray evaluation. Eur. J. Orthop. Surg. Traumatol. 29(4), 883–891. https://doi.org/10.1007/s00590-019-02371-0 (2019).
Panisset, J. C., Ntagiopoulos, P. G., Saggin, P. R. & Dejour, D. A comparison of Telos stress radiography versus Rolimeter in the diagnosis of different patterns of anterior cruciate ligament tears. Orthop. Traumatol. Surg. Res. 98(7), 751–758. https://doi.org/10.1016/j.otsr.2012.07.003 (2012).
Beldame, J. et al. Laxity measurements using stress radiography to assess anterior cruciate ligament tears. Orthop. Traumatol. Surg. Res. 97(1), 34–43. https://doi.org/10.1016/j.otsr.2010.08.004 (2011).
Mostafaee, N. et al. Responsiveness of a Persian version of Knee Injury and Osteoarthritis Outcome Score and Tegner activity scale in athletes with anterior cruciate ligament reconstruction following physiotherapy treatment. Physiother. Theory Pract. 36(9), 1019–1026. https://doi.org/10.1080/09593985.2018.1548672 (2020).
Weng, C. J. et al. Clinical and functional outcomes of anterior cruciate ligament reconstruction with autologous hamstring tendon in patients aged 50 years or older. Arthroscopy 36(2), 558–562. https://doi.org/10.1016/j.arthro.2019.08.047 (2020).
Harris, J. D., Brand, J. C., Cote, M. P., Faucett, S. C. & Dhawan, A. Research pearls: The significance of statistics and perils of pooling. Part 1: Clinical versus statistical significance. Arthroscopy 33(6), 1102–1112. https://doi.org/10.1016/j.arthro.2017.01.053 (2017).
Wiley, W. B., Askew, M. J., Melby, A. 3rd. & Noe, D. A. Kinematics of the posterior cruciate ligament/posterolateral corner-injured knee after reconstruction by single- and double-bundle intra-articular grafts. Am. J. Sports Med. 34(5), 741–748. https://doi.org/10.1177/0363546505282615 (2006).
Markolf, K. L., Feeley, B. T., Jackson, S. R. & McAllister, D. R. Biomechanical studies of double-bundle posterior cruciate ligament reconstructions. J. Bone Joint Surg. Am. 88(8), 1788–1794. https://doi.org/10.2106/JBJS.E.00427 (2006).
Xie, W. Q. et al. The effects of posterior cruciate ligament rupture on the biomechanical and histological characteristics of the medial collateral ligament: An animal study. J. Orthop. Surg. Res. 16(1), 330. https://doi.org/10.1186/s13018-021-02443-0 (2021).
Savarese, E., Bisicchia, S., Romeo, R. & Amendola, A. Role of high tibial osteotomy in chronic injuries of posterior cruciate ligament and posterolateral corner. J. Orthop. Traumatol. 12(1), 1–17. https://doi.org/10.1007/s10195-010-0120-0 (2011).
Race, A. & Amis, A. A. PCL reconstruction. In vitro biomechanical comparison of “isometric” versus single and double-bundled “anatomic” grafts. J Bone Joint Surg Br 80(1), 173–179. https://doi.org/10.1302/0301-620x.80b1.7453 (1998).
Fanelli, G. C., Beck, J. D. & Edson, C. J. Single compared to double-bundle PCL reconstruction using allograft tissue. J. Knee Surg. 25(1), 59–64. https://doi.org/10.1055/s-0031-1299665 (2012).
Li, Y., Li, J., Wang, J., Gao, S. & Zhang, Y. Comparison of single-bundle and double-bundle isolated posterior cruciate ligament reconstruction with allograft: A prospective, randomized study. Arthroscopy 30(6), 695–700. https://doi.org/10.1016/j.arthro.2014.02.035 (2014).
Yoon, K. H., Bae, D. K., Song, S. J., Cho, H. J. & Lee, J. H. A prospective randomized study comparing arthroscopic single-bundle and double-bundle posterior cruciate ligament reconstructions preserving remnant fibers. Am. J. Sports Med. 39(3), 474–480. https://doi.org/10.1177/0363546510382206 (2011).
Tornese, D. et al. Patellar tendon graft vs. Semitendinosus and Gracilis graft for posterior cruciate ligament reconstruction: An isokinetic and functional study one year after the operation. Isokinetics Exercise Sci. 16, 133–137 (2008).
Senese, M., Greenberg, E., Todd Lawrence, J. & Ganley, T. Rehabilitation following isolated posterior cruciate ligament reconstruction: A literature review of published protocols. Int. J. Sports Phys. Ther. 13(4), 737–751 (2018).
Deie, M., Adachi, N., Nakamae, A., Takazawa, K. & Ochi, M. Evaluation of single-bundle versus double-bundle PCL reconstructions with more than 10-year follow-up. Sci. World J. 2015, 751465. https://doi.org/10.1155/2015/751465 (2015).
Shon, O. J., Lee, D. C., Park, C. H., Kim, W. H. & Jung, K. A. A comparison of arthroscopically assisted single and double bundle tibial inlay reconstruction for isolated posterior cruciate ligament injury. Clin. Orthop. Surg. 2(2), 76–84. https://doi.org/10.4055/cios.2010.2.2.76 (2010).
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
F.M.: literature search, data extraction, methodological quality assessment, statistical analyses, writing; N.M.: supervision, revision, final approval; A.P.: literature search, data extraction, methodological quality assessment; F.H.: supervision; F.O.: supervision F.S.: supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Migliorini, F., Pintore, A., Spiezia, F. et al. Single versus double bundle in posterior cruciate ligament (PCL) reconstruction: a meta-analysis. Sci Rep 12, 4160 (2022). https://doi.org/10.1038/s41598-022-07976-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-07976-w
This article is cited by
-
Einzelbündelrekonstruktion des hinteren Kreuzbandes – Banderhaltende Technik mit einem autologen Semitendinosus‑/Gracilissehnentransplantat
Knie Journal (2023)
-
Similar rate of return to sports activity between posterior-stabilised and cruciate-retaining primary total knee arthroplasty in young and active patient
Knee Surgery, Sports Traumatology, Arthroscopy (2023)
-
Allografts as alternative to autografts in primary posterior cruciate ligament reconstruction: a systematic review and meta-analysis
Knee Surgery, Sports Traumatology, Arthroscopy (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.