Abstract
To determine the functional recovery, active reincorporation, and anteroposterior and rotational stability of patients undergoing anterior cruciate ligament (ACL) reconstruction using arthroscopy techniques with simple-bundle (SB) or double-bundle (DB). The following databases were searched: PubMed, Embase (Elsevier platform), the Cochrane Central Register of Controlled Trials (Wiley platform), Web of Science, and CINAHL. Level I and II studies involving anterior cruciate ligament arthroscopy were included in the search. Records were screened by title and abstract and assessed the risk of bias of selected studies. Meta-analyses using RevMan 5.3 software were conducted on the following outcomes: knee functionality, objective measurements of knee stability, rotational knee stability and knee anterior stability, sports reincorporation, and subjective assessments. Twenty-four studies of patients undergoing ACL reconstruction were included in the qualitative and quantitative synthesis (1707 patients) for Lysholm score, Subjective International Knee Documentation Committee (IKDC) score, Tegner score, KT-1000/2000, Lachman test, Objective IKDC score, and Pivot-Shift test. A return to pre-injury level showed a significant decrease in the Lysholm score (mean difference, − 0.99; 95% CI − 1.71 to − 0.40; P = 0.007) and Tegner score (mean difference, − 0.07; 95% CI, − 0.13 to − 0.01; P = 0.02) at DB reconstruction, similar to the knee functionality outcome of the subjective IKDC score (mean difference − 1.42; 95% CI − 2.46 to − 0.38; P = 0.007). There is no clear or significant difference in clinical stability and knee function or in sports incorporation with the true difference occurring in the subjective assessment.
Similar content being viewed by others
Introduction
Rupture of the anterior cruciate ligament (ACL) represent 50% of ligament injuries of the knee1,2. Seventy-five percent of these ruptures occur during sports activities such as football3,4, basketball5 or skiing6. In addition, the prevalence has increased in the latest trends due to increased activity of the population (as high as 3/10.000 individuals/year7), which implies a high cost in public health.
The arthroscopic single-bundle (SB) technique is the most common method used in ACL reconstruction8,9,10. This reconstruction technique may provide good clinical outcomes and restore anterior stability following an ACL injury11, improve joint stability, proprioceptive function, and balance ability12, but it may also be suboptimal concerning rotational function13. The arthroscopic double-bundle (DB) strategy, which was first described by Mott in 198314, technically reconstructs 2 functional bundles of the ACL and thereby more closely approximates the native anatomy. Moreover, it demonstrates less anterior laxity by using a KT-1000 arthrometer15 and increased objective tibial stability and objective IKDC scores compared to SB ACL reconstruction16.
An increasing number of studies and systematic reviews have compared the two surgical techniques, that is, SB versus DB procedures17,18,19. Several clinical studies have reported that anatomic DB ACL reconstruction might increase rotational and anterior stability of the knee20, improve graft-tunnel healing21 and decrease the rate of meniscal tears22,23. Several studies found no significant differences between clinical outcomes in either group with a long follow-up24,25,26. Several meta-analyses have also been published comparing the two procedures (SB vs. DB) and it remains unclear which one is superior in clinical outcomes. Moreover, this was determined when randomized controlled trials (RCTs) with a 3-year follow-up17,27,28 were included and jointly analysed meta-analysis presented functional recovery, active reincorporation, and anteroposterior and rotational stability.
Does the arthroscopic DB technique, compared to the arthroscopic SB technique, improve clinical outcomes in athletes?
Therefore, this meta-analysis aimed to determine the functional recovery and active reincorporation and the anteroposterior and rotational stability of patients undergoing anterior cruciate ligament (ACL) reconstruction using simple bundles (SB) or double bundles (DB).
Results
Study selection
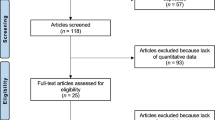
The search yielded 575 records (Fig. 1), which were screened by 2 investigators, including 130 records which were assessed for eligibility.

Adapted from Moher et al.65.
Study selection process. Our initial search of databases yielded 575 records. We searched the reference lists of relevant studies and related systematic reviews and found no additional records. After 445 records were excluded, 130 full-text articles were appraised. Thirty-eight were included in the qualitative synthesis and twenty-four were included in the quantitative analysis and meta-analyses. (CINAHL, Cumulative Index to Nursing and Allied Health Literature).
Qualitative systematic review
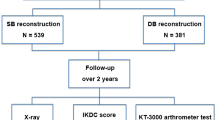
A total of 24 studies with 1707 patients were included in the qualitative systematic review29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52 (Table 1). All studies included patients undergoing ACL reconstruction. Of the studies, 22 used a randomized controlled trial design29,30,31,32,33,35,36,37,38,39,40,41,42,43,44,46,47,48,49,50,51,52, 1 used a nonrandomized design34 and 1 used a quasi-experimental design with 2 consecutive groups45. One group received single-bundle reconstruction while another group received double-bundle reconstruction of the ACL. In randomized controlled trials, both groups occurred at a 1:1 proportion. Six studies used semitendinosus autologous grafts for SB and DB reconstructions29,33,45,46,48,52 and 6 of them used both semitendinosus and gracilis grafts32,35,43,44,49. Three studies used tibial anterior allografts38,39,47, and one of them used frozen tibial anterior autologous allografts47. In 9 studies, the bone patellar tendon was used as the graft30,31,34,40,41,46,49,50,51. The outcomes presented in all studies were assessed in different follow-up periods with 13 short- and mid-term studies (less than 2 years)30,31,33,34,42,43,45,46,47,48,49,50,52, one preliminary study48, and 11 studies were long-term follow-ups (more than 2 years)29,32,35,36,37,38,39,40,41,44,51.
In the presented outcomes, most of the studies showed no differences; however, in 2 studies, the pivot-shift test showed better results in the double-bundle group as shown in (P < 0.001)40 and (P = 0.003)51. Two studies47,49 showed better grades of objective and subjective IKDC scores and presented high heterogeneity between the IKDC score objective studies. Koga et al.40 showed better results in the double-bundle group (P = 0.024) in the Lachman test, and KT measurements were better in the double-bundle group (mean, 1.4 mm vs. 2.7 mm; P = 0.0023). The Tegner score was also better in the double-bundle group (P = 0.033). Zaffagnini et al.51 showed that the double-bundle hamstring group had a significantly higher Tegner level (P = 0.0007) and a higher passive range of motion recovery (P = 0.0014). The side-to-side difference in posterior translation decreased in the double-bundle group with a significant difference between the 2 groups (P < 0.05).
Assessment of risk of bias
The risk of selection bias, related to a lack of random sequence generation and allocation concealment, was high in 5 studies using non-random group allocation31,34,40,45,47. Four studies used random allocation, but the method was unclear30,35,49,51, whereas the remainder used a random-numbers table29,32,33,36,38,39,41,43,44,46,48,50,52. Seven studies reported blinding of participants, personnel, and outcome assessors30,33,36,42,48, whereas in 2 studies, only the outcome assessors were blinded39,51. Blinding procedures were not reported in half of the studies31,32,34,38,43,44,45,46,49,50,52. The risk of attrition bias was deemed high in only 1 study because they lost participants in the follow-up that were needed for analysis45. The risk of reporting bias was unclear in half of the meta-analyses29,33,34,35,36,37,38,40,41,45,46,47 (Fig. 2).
Heterogeneity
We evaluated the clinical heterogeneity of 24 studies. Statistical heterogeneity was calculated for both continuous (Lysholm and Tegner score, internal rotation range, KT-1000/2000, and subjective IKDC score) and dichotomous (pivot shift, Lachman test, and objective IKDC score) variables.
In the 3 studies included in the internal rotation range, the heterogeneity was high (I2 = 73%)43,44,48. Heterogeneity was also high for the 6 studies included in the objective IKDC score (I2 = 91%)29,36,37,43,44,49 and for the 12 studies included in the pivot shift test (I2 = 64%)30,31,36,37,38,39,40,44,45,46,47,50. Among the 12 studies included in KT-1000/2000, the heterogeneity was moderate (I2 = 40%)29,30,31,33,34,35,36,37,39,40,42,45. Heterogeneity was low for 13 studies included in the Lysholm score (I2 = 42%)29,31,32,33,34,35,36,37,39,40,41,50,52 and for 13 studies included in the Tegner score (I2 = 8%)32,33,34,35,39,40,41,45,46,47,49,50,52. Heterogeneity was also low for 9 studies included in the subjective IKDC score (I2 = 0%)32,33,36,41,43,44,48,50 and for 8 studies included in the Lachman test (I2 = 1%)30,31,33,38,39,43,47,52. No studies were excluded due to a high risk of bias that could influence the presented heterogeneity.
Quantitative meta-analyses
A total of 24 studies with 1707 patients were included in the quantitative meta-analyses. We grouped studies for statistical analyses based on follow-up into the following categories: baseline, 6–12 months, 13–18 months, 19–24 months, 25–36 months and > 36 months. The aforementioned categories were used in each of the following outcome measures: Lysholm score (13 studies [5 subgroups] [22 comparisons], baseline period, n = 758 patients; 6–12 month period, n = 172 patients; 19–24 month period, n = 94 patients; 25–36 month period, n = 36 patients and > 36 month period, n = 561 patients); Internal rotation range (3 studies [4 subgroups] [7 comparisons], baseline period, n = 204 patients; 6–12 month period, n = 80 patients; 19–24 month period n = 142 patients and 25–36 month period, n = 62 patients); KT/1000–2000 (12 studies [5 subgroups] [20 comparisons], baseline period, n = 654 patients; 6–12 month period, n = 150 patients; 19–24 month period, n = 78 patients; 25–36 month period, n = 101 patients and > 36 month period, n = 536 patients); Tegner score (13 studies [5 subgroups] [22 comparisons], baseline period, n = 790 patients; 6–12 month period, n = 146 patients; 19–24 month period, n = 230 patients; 25–36 month period, n = 40 patients and > 36 month period, n = 232 patients); Subjective IKDC score (9 studies [5 subgroups] [17 comparisons], baseline period, n = 654 patients; 6–12 month period, n = 150 patients; 19–24 month period, n = 78 patients; 25–36 month period, n = 101 patients and > 36 month period, n = 536 patients); Lachman test (8 studies [5 subgroups] [14 comparisons] (baseline period, n = 476 patients; 6–12 month period, n = 170 patients; 19–24 month period, n = 251 patients; 25–36 month period, n = 84 patients and > 36 month period, n = 87 patients). Regarding continuous variables, the subjective IKDC score was lower in the SB group than in the DB group (mean difference, − 1.42; 95% CI − 2.46 to − 0.38; P = 0.007) (Fig. 3)32,33,36,41,43,44,48,50 and the Tegner score (mean difference, − 0.07; 95% CI − 0.13 to − 0.01; P = 0.02), which favoured SB in both outcomes (Fig. 4 A)32,33,34,35,39,40,41,45,46,47,49,50,52. In the internal rotation range, no differences were found between the two groups (mean difference, − 0.10 mm; 95% CI − 0.56 mm to 0.36 mm; P = 0.67)43,44,48 (Fig. 5) as KT/1000–2000 (mean difference, 0.16; 95% CI − 0.06 to 0.38; P = 0.15)29,30,31,33,34,35,36,37,39,40,42,45 (Fig. 6 B) (Table 2).
Forest plots of knee functionality data outcomes for single-bundle versus double-bundle reconstruction. Weights are from random-effects analysis. (A) Continuous data for the Subjective IKDC score (8 studies in the baseline period, 654 patients; 4 studies in the 6–12-month period, 150 patients; 1 study in the 19–24-month period, 78 patients; 2 studies in the 25–36-month period, 101 patients and 5 studies in the > 36-month period, 536 patients). Heterogeneity was low: τ2 = 0.00; χ2 = 11.86, df = 15 (P = 0.69); I2 = 0% (CI, confidence interval; IV, inverse variance). (B) Dichotomous data for the objective IKDC score (3 studies in the baseline period, 280 patients; 1 study in the 19–24-month period, 62 patients; 2 studies in the 25–36-month period, 102 patients and 1 study in the > 36-month period, 70 patients). The heterogeneity was high: τ2 = 0.02; χ2 = 69.84, df = 6 (P < 0.001); I2 = 91% (CI, confidence interval; M-H, Mantel–Haenszel). Data collected from RevMan 5.3 software.
Return to pre-injury level data forest plot outcomes for single-bundle versus double-bundle reconstruction. Weights from fixed effects for the Tegner score analysis and random effects for the Lysholm score analysis are presented. (A) Continuous data for the Tegner score (10 studies in the baseline period, 790 patients; 4 studies in the 6–12-month period, 146 patients; 2 studies in the 19–24-month period, 230 patients; 1 study in the 25–36-month period, 40 patients and 4 studies in the > 36-month period, 232 patients). Heterogeneity was low: χ2 = 20.64, df = 19 (P = 0.36); I2 = 8% (CI, confidence interval; IV, inverse variance). (B) Continuous data for the Lysholm score (9 studies in the baseline period, 758 patients; 4 studies in the 6–12-month period, 172 patients; 1 study in the 19–24-month period, 94 patients; 1 study in the 25–36-month period, 36 patients and 7 studies in the > 36-month period, 561 patients). Heterogeneity was low: τ2 = 0.00; χ2 = 17.84, df = 6 (P = 0.66); I2 = 0% (CI, confidence interval; IV, inverse variance). Data collected from RevMan 5.3 software.
Rotational knee stability data forest plot outcomes for single-bundle versus double-bundle reconstruction. Weights are from random-effects analysis. (A) Dichotomous data for the pivot shift test (9 studies in the baseline period, 842 patients; 4 studies in the 6–12-month period, 242 patients; 3 studies in the 19–24-month period, 296 patients; 1 study in the 25–36-month period, 84 patients and 5 studies in the > 36-month period, 493 patients). The heterogeneity was high: τ2 = 0.00; χ2 = 58.24, df = 21 (P = < 0.001); I2 = 64% (CI, confidence interval; M-H, Mantel–Haenszel). (B) Continuous data for the internal rotation range (3 studies in the baseline period, 204 patients; 1 study in the 6–12-month period, 80 patients; 2 studies in the 19–24-month period, 142 patients; and 1 study in the 25–36-month period, 62 patients). Heterogeneity was high: τ2 = 0.18; χ2 = 22.17, df = 6 (P < 0.001); I2 ¼ 73% (CI, confidence interval; IV, inverse variance). Data collected from RevMan 5.3 software.
Forest plots of knee anterior stability data for single-bundle versus double-bundle reconstruction. Weights are from fixed effects for the Lachman test analysis and random effects for the KT 1000/2000 analysis. (A) Dichotomous data for the Lachman test (6 studies in the baseline period, 476 patients; 3 studies in the 6–12-month period, 170 patients; 3 studies in the 19–24-month period, 251 patients; 1 study in the 25–36-month period, 84 patients and 1 study in the > 36-month period, 87 patients). The heterogeneity was low: χ2 = 13.07, df = 13 (P = 0.44); I2 = 1% (CI, confidence interval; M-H, Mantel–Haenszel). (B) Continuous data for KT-1000/2000 (8 studies in the baseline period, 654 patients; 4 studies in the 6–12-month period, 150 patients; 1 study in the 19–24-month period, 78 patients; 2 studies in the 25–36-month period, 101 patients and 5 studies in the > 36-month period, 536 patients). Heterogeneity was moderate: τ2 = 0.07; χ2 = 31.57, df = 19 (P = 0.03); I2 = 40% (CI, confidence interval; IV, inverse variance). Data collected from RevMan 5.3 software.
Regarding dichotomous variables, the Lachman test percentage no was higher in the double-bundle group than in the single-bundle group (RD, 0.01; 95% CI − 0.01 to 0.04; P = 0.13)30,31,33,38,39,43,47,52 (Fig. 6 A) (Table 3).
Data on the re-rupture rate in both techniques were not evaluated in the included studies.
Discussion
In this meta-analysis, we attempted to show whether there were significant differences between SB and DB interventions in the recovery of functionality after ACL tears, since previous studies did not demonstrate this result strongly enough. We found significant differences favourable to DB reconstruction in the return to the preinjury level according to the Lysholm score (P = 0.007) and the functionality of the knee according to the IKDC subjective score (P = 0.007).
Residual instability in reconstructive ACL surgery is the main cause of mechanical failure. Techniques that reduce this instability, mainly in the rotational plane, have been previously described and highlight those that involve the performance of a DB to reproduce the original anatomy of the ACL in the anteromedial (AM) and posterolateral (PL) bundles by arthroscopic surgery.
There are some differences between the technical aspects and tips but the real difference between the whole DB reconstruction surgery is the realization of an only tibial tunnel or double tibial tunnel as well, since all the DB are with two tunnels. Respect to the SB surgery it would come based on the use of the new concept of anatomical technique (or through anteromedial portal) or classic through transtibial, being a relatively new technique53,54. Mostly of the studies included in our systematic review showed highlight an improvement in rotational stability (based on exploratory manoeuvres) throughout the follow-up according to functional reincorporation by using DB reconstruction surgery.
This study was conducted to compare the early-, mid-, and long-term follow-up of patient operations using DB and SB techniques. The results show that there is no clear or significant difference in the clinical stability and knee function or in sports incorporation with the true difference being the subjective assessment by the patient. These results are consistent with those presented by another recent systematic review and adds subjective assessment data to previous datasets55. The non-differences in the previous laxity do not confirm previous findings. Björnsson et al.56 shows results with DB improvement, but this systematic review presents RCT, prospective and retrospectives studies with less evidence regarding this meta-analysis and in the context of rotational stability. Our findings stand out with a non-significant improvement (internal rotation and pivot shift), which seems to be in contrast with the technical gesture of adding a PL fascicle to the conventional technique. Perhaps the classic concept of injury of "the other" peripheral structures, such as the collateral ligaments and the muscles that cross the joint and play an important role in the concept of rotational stability55,57.
In Kongtharvonskul et al. study, clinical function showed a significant statistical difference between the DB and SB techniques in autologous ACL reconstruction58, results similar to those found in our meta-analysis.
The strengths of results present in this works are: 1. Although there do not seem to be any functional differences from the immediate postoperative period, in the return to physical and sports activity differences are shown at 18 months after the DB, which are also evident after 3 years for the Lysholm and Tegner score (Fig. 4). For sports, this is of the utmost importance and often not shown during these mid-term and long-term follow-ups, according to results shown by Xu et al.10. 2. Subjective assessment through the IKDC shows a higher score with a better feeling of stability from the subjective viewpoint in the mean score of the total in the DB vs. SB technique, which is the most statistically significant for the outcomes of the study. This analysis of the subjective feeling of the patient in favour of the DB technique allows the patient greater confidence in their return to physical activities in patients undergoing the DB technique. Furthermore, this disagrees with previous studies that found no differences in subjective outcome measures between DB and SB reconstruction10. These results were not seen in the objective IKDC score, but there was a significant and favourable trend toward the DB technique observed (P = 0.10) (Fig. 3), which agrees with Xu et al.’s meta-analysis10 and concludes that DB anterior cruciate ligament reconstruction resulted in significantly better anterior and rotational stability and higher IKDC objective scores than SB reconstruction. Therefore, the evaluation of the patient and activity levels could be the strength of choice when choosing the DB technique. 3. Lachman anteroposterior instability shows similar results in both techniques, which indicates that there is no advantage for any technique from the medical anteroposterior point of view using Lachman and KT-1000/2000, and different results from other systematic revisions (Fig. 6) showed statistically significant differences with less anterior laxity in 45% of studies that included the DB technique56,59. Based on current evidence, DB reconstruction appears to have fewer re-ruptures and less antero-posterior and rotatory laxity. 4. Rotational stability (internal rotation and pivot shift) is slightly better but not significant in DB reconstruction. This benefit is especially important regarding the concept of reinjury since the persistence of rotational instability has become evident as a cause of rupture. Therefore, although both patients needed to maintain “anti-rotational” muscle enhancement, this should be more demanding in patients with the SB technique. These results present controversy from previous systematic reviews showing that DB provided significantly better knee stability than the SB technique10,56,58,59. According to results presented by our work, DB was better in the long-term follow-up than the SB technique, but not in all follow-ups of the included studies. Similar to a previous systematic review58, heterogeneity was present in some outcomes, but there was no evidence of publication bias for any outcome. The double-bundle technique may be better than the single-bundle ACL reconstruction technique for rotational stability but not for function, translation, and complications.
As previously shown in studies and meta-analysis, there is a biomechanical improvement in postoperative knee stability by using DB reconstruction technique59,60,61. However, in the rotational stability, only 2 studies have shown statistical results in favour of the DB40,51, compared to several studies that present better objective scores46,49.
The need for this systematic review and meta-analysis is based on the joint interpretation of mid- and long-term clinical outcomes of knee functionality, objective measurements of knee stability, rotational knee stability and knee anterior stability, sports reincorporation and subjective assessments to confirm the current discordant results in SB and DB ACL reconstruction.
Limitations
Only studies published in English were included, and therefore, some relevant studies may have been missed. The “anatomical technique” that uses the anteromedial portal to perform femoral tunnels has not been included as a study variable as it is a relatively new technique and still without relevant RCTs to complete the meta-analysis proposed by the research team; there is a proposal for a future meta-analysis of the interventions with this new procedure. Associated complications that may influence the failure of the plasty and the assessment of future osteoarthritis were not assessed. The risk of bias was unclear, and heterogeneity was moderate to high in several outcomes.
Conclusion
Currently, there are no clear or significant differences in clinical stability and knee function or in sports incorporation for the recommendation of DB in the primary ACL. The true difference between both techniques is shown in the subjective assessment by the IKDC score reported by patients.
Methods
Systematic search
We used the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) to conduct this systematic review and meta-analysis62 in conformity with updated guidance of The Cochrane Collaboration Principles for Systematic Reviews63. Inclusion criteria were (1) participants older than 14 years with a ruptured ACL isolated or combined with other soft tissue injuries requiring ACL reconstruction; (2) randomized clinical trial design; (3) comparison of a single-bundle with a double-bundle (3 t or 4 t); and (4) main outcome measures such as measurements of knee functionality as measured by the patient or by the doctor (i.e. subjective and objective International Knee Documentation Committee Knee Form (IKDC) score) and a return to pre-injury activity levels (Tegner activity score and Lysholm score). Secondary outcome measures: objective measurements of knee stability (rotational knee stability (pivot-shift test and range of mobility of internal rotational)) and knee anterior stability was measured using the Lachman test and KT-1000/2000; and (5) publication between database inception and July 2019.
We developed comprehensive search strategies with the assistance of a health sciences documentalist with background in searching for systematic reviews including both index and keyword methods for PubMed, Embase (Elsevier platform), the Cochrane Central Register of Controlled Trials (Wiley platform), Web of Science, and CINAHL (Cumulative Index to Nursing and Allied Health Literature; EBSCO platform). To maximize sensitivity, no pre-set limits for the database were used. The PubMed search strategy was adapted for use with the other electronic databases. Complete search strategies are shown in Table 4.
The search was conducted in July 2019. In addition to the databases, we searched the reference lists of relevant studies and proceedings of orthopaedic conferences. The search results were exported to Excel (Microsoft Office 365 ProPlus) and duplicates were electronically removed.
Two investigators and one experienced senior orthopaedic surgeon independently screened records by title and abstract. In addition, records included by the first screening were assessed through a full-text review. Any discrepancies between the reviewers were resolved through discussion, and when necessary, a third reviewer was consulted.
Data extraction
Two investigators individually extracted data from eligible studies using a data collection form. Discrepancies were resolved through discussion with a third reviewer. The following data elements were extracted: the name of the first author, publication year, design, patient characteristics, interventions (single-bundle and double bundle), outcomes (Lysholm score, Pivot shift, Range of mobility (degrees), Internal rotational range (mm), KT-1000/2000, Tegner score, Lachman test, Subjective and Objective IKDC score, statistical analyses, and results.
Risk of bias assessment
The Cochrane Collaboration’s tool for assessing risk of bias (RoB) was used to evaluate the study risk of bias within the included randomized controlled trials63. Three investigators independently extracted information on randomization, allocation concealment, blinding, attrition, selective reporting, and other biases (manufacturer funding and statistical power) for each study. After discussion, categories for all included studies were graded as having a low, unclear, or high risk of bias.
Statistical analysis
We used Review Manager software (RevMan, version 5.3; The Cochrane Collaboration, Copenhagen, Denmark) to perform statistical analyses. Heterogeneity was evaluated using the I2 calculation. I2 values were interpreted using the Cochrane criteria for measuring heterogeneity64. We used random-effects models for studies and although similar to the surgical technique, they showed high heterogeneity and fixed-effects for studies with low heterogeneity. We also calculated mean differences for continuous data (Lysholm score, range of mobility, internal rotational range, KT-1000/2000, Tegner score and objective IKDC score) and pooled risk differences (RD) for dichotomous data (pivot shift, Lachman test and subjective IKDC score) with 95% confidence intervals (CIs); P ≤ 0.05 was considered statistically significant.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Mehl, J. et al. The ACL-deficient knee and the prevalence of meniscus and cartilage lesions: a systematic review and meta-analysis (CRD42017076897). Arch. Orthop. Trauma Surg. 139, 819–841. https://doi.org/10.1007/s00402-019-03128-4 (2019).
Sutton, K. M. & Bullock, J. M. Anterior cruciate ligament rupture: differences between males and females. J. Am. Acad. Orthop. Surg. 21, 41–50. https://doi.org/10.5435/jaaos-21-01-41 (2013).
Walden, M., Hagglund, M., Magnusson, H. & Ekstrand, J. ACL injuries in men’s professional football: a 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL rupture. Br. J. Sports Med. 50, 744–750. https://doi.org/10.1136/bjsports-2015-095952 (2016).
Roth, T. S. & Osbahr, D. C. Knee injuries in elite level soccer players. Am. J. Orthop. (Belle Mead NJ) https://doi.org/10.12788/ajo.2018.0088 (2018).
Benis, R. A. L. A. T. & Bonato, M. Anterior cruciate ligament injury profile in female elite Italian basketball league. J. Sports Med. Phys. Fitness 58, 280–286. https://doi.org/10.23736/s0022-4707.16.06663-9 (2018).
Csapo, R., Hoser, C., Gfoller, P., Raschner, C. & Fink, C. Fitness, knee function and competition performance in professional alpine skiers after ACL injury. J. Sci. Med. Sport 22(Suppl 1), S39-s43. https://doi.org/10.1016/j.jsams.2018.06.014 (2019).
Olsson, O., Isacsson, A., Englund, M. & Frobell, R. B. Epidemiology of intra- and peri-articular structural injuries in traumatic knee joint hemarthrosis-data from 1145 consecutive knees with subacute MRI. Osteoarthr. Cartilage 24, 1890–1897. https://doi.org/10.1016/j.joca.2016.06.006 (2016).
Youm, Y. S., Cho, S. D., Lee, S. H. & Youn, C. H. Modified transtibial versus anteromedial portal technique in anatomic single-bundle anterior cruciate ligament reconstruction: comparison of femoral tunnel position and clinical results. Am. J. Sports Med. 42, 2941–2947. https://doi.org/10.1177/0363546514551922 (2014).
Arno, S. et al. Does anteromedial portal drilling improve footprint placement in anterior cruciate ligament reconstruction?. Clin. Orthop. Relat. Res. 474, 1679–1689. https://doi.org/10.1007/s11999-016-4847-7 (2016).
Xu, M. et al. Outcomes of anterior cruciate ligament reconstruction using single-bundle versus double-bundle technique: meta-analysis of 19 randomized controlled trials. Arthroscopy 29, 357–365. https://doi.org/10.1016/j.arthro.2012.08.024 (2013).
Hoogeslag, R. A. G., Brouwer, R. W., Boer, B. C., de Vries, A. J. & Huis, I. V. R. Acute anterior cruciate ligament rupture: repair or reconstruction? Two-year results of a randomized controlled clinical trial. Am. J. Sports Med. 47, 567–577. https://doi.org/10.1177/0363546519825878 (2019).
Fu, C. L. et al. The effect of early whole-body vibration therapy on neuromuscular control after anterior cruciate ligament reconstruction: a randomized controlled trial. Am. J. Sports Med. 41, 804–814. https://doi.org/10.1177/0363546513476473 (2013).
Mutsuzaki, H., Kinugasa, T., Ikeda, K. & Sakane, M. Anatomic single-bundle anterior cruciate ligament reconstruction using a calcium phosphate-hybridized tendon graft: a randomized controlled trial with 2 years of follow-up. J. Orthop. Surg. Res. 13, 327. https://doi.org/10.1186/s13018-018-1045-1 (2018).
Mott, H. W. Semitendinosus anatomic reconstruction for cruciate ligament insufficiency. Clin. Orthop. Relat. Res. 20, 90–92 (1983).
Desai, N. et al. Anatomic single- versus double-bundle ACL reconstruction: a meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 22, 1009–1023. https://doi.org/10.1007/s00167-013-2811-6 (2014).
Aglietti, P. et al. Comparison between single-and double-bundle anterior cruciate ligament reconstruction: a prospective, randomized, single-blinded clinical trial. Am. J. Sports Med. 38, 25–34. https://doi.org/10.1177/0363546509347096 (2010).
Belk, J. W., Kraeutler, M. J., Houck, D. A. & McCarty, E. C. Knee osteoarthritis after single-bundle versus double-bundle anterior cruciate ligament reconstruction: a systematic review of randomized controlled trials. Arthroscopy 35, 996–1003. https://doi.org/10.1016/j.arthro.2018.10.127 (2019).
Kang, H., Zheng, R., Dai, Y., Lu, J. & Wang, F. Single- and double-bundle medial patellofemoral ligament reconstruction procedures result in similar recurrent dislocation rates and improvements in knee function: a systematic review. Knee Surg. Sports Traumatol. Arthrosc. 27, 827–836. https://doi.org/10.1007/s00167-018-5112-2 (2019).
Mayr, H. O. & Stoehr, A. Editorial commentary: no difference in knee osteoarthritis after single-bundle versus double-bundle anterior cruciate ligament reconstruction. Arthroscopy 35, 1004–1005. https://doi.org/10.1016/j.arthro.2018.12.029 (2019).
Chowdhury, A. Z. et al. Anterior cruciate ligament reconstruction using autologous hamstring double bundle graft compared with single bundle graft procedures. Mymensingh Med. J. 28, 126–136 (2019).
Inoue, T. et al. Anatomic oblong double bundle anterior cruciate ligament reconstruction. Kurume Med. J. 62, 53–58. https://doi.org/10.2739/kurumemedj.MS66002 (2016).
van Eck, C. F. et al. Single-bundle versus double-bundle reconstruction for anterior cruciate ligament rupture: a meta-analysis–does anatomy matter?. Arthroscopy 28, 405–424. https://doi.org/10.1016/j.arthro.2011.11.021 (2012).
Sun, R., Chen, B. C., Wang, F., Wang, X. F. & Chen, J. Q. Prospective randomized comparison of knee stability and joint degeneration for double- and single-bundle ACL reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 23, 1171–1178. https://doi.org/10.1007/s00167-014-2934-4 (2015).
Arciero, R. A. Double-bundle and single-bundle ACL reconstruction techniques did not differ in terms of clinical outcomes at 2 or 5 years. J. Bone Joint Surg. Am. 98, 1933–1934. https://doi.org/10.2106/jbjs.16.00883 (2016).
Gobbi, A., Mahajan, V., Karnatzikos, G. & Nakamura, N. Single- versus double-bundle ACL reconstruction: is there any difference in stability and function at 3-year followup?. Clin. Orthop. Relat. Res. 470, 824–834. https://doi.org/10.1007/s11999-011-1940-9 (2012).
Devgan, A. et al. A prospective study to evaluate the clinico-radiological outcomes of arthroscopic single bundle versus double bundle anterior cruciate ligament reconstruction. J. Clin. Orthop. Trauma 7, 236–242. https://doi.org/10.1016/j.jcot.2016.01.004 (2016).
Rodriguez-Merchan, E. C. Evidence-Based ACL reconstruction. Arch. Bone Surg. 3, 9–12 (2015).
Desai, N. et al. A systematic review of single- versus double-bundle ACL reconstruction using the anatomic anterior cruciate ligament reconstruction scoring checklist. Knee Surg. Sports Traumatol. Arthrosc. 24, 862–872. https://doi.org/10.1007/s00167-014-3393-7 (2016).
Adravanti, P., Dini, F., de Girolamo, L., Cattani, M. & Rosa, M. A. Single-bundle versus double-bundle anterior cruciate ligament reconstruction: a prospective randomized controlled trial with 6-year follow-up. J. Knee Surg. 30, 898–904. https://doi.org/10.1055/s-0037-1598176 (2017).
Ahldén, M., Sernert, N., Karlsson, J. & Kartus, J. A prospective randomized study comparing double- and single-bundle techniques for anterior cruciate ligament reconstruction. Am. J. Sports Med. 41, 2484–2491. https://doi.org/10.1177/0363546513497926 (2013).
Araki, D. et al. A prospective randomised study of anatomical single-bundle versus double-bundle anterior cruciate ligament reconstruction: quantitative evaluation using an electromagnetic measurement system. Int. Orthop. 35, 439–446. https://doi.org/10.1007/s00264-010-1110-9 (2011).
Beyaz, S. et al. Tunnel widening after single- versus double-bundle anterior cruciate ligament reconstruction: a randomized 8-year follow-up study. Arch. Orthop. Trauma Surg. 137, 1547–1555. https://doi.org/10.1007/s00402-017-2774-z (2017).
Bohn, M. B., Sørensen, H., Petersen, M. K., Søballe, K. & Lind, M. Rotational laxity after anatomical ACL reconstruction measured by 3-D motion analysis: a prospective randomized clinical trial comparing anatomic and nonanatomic ACL reconstruction techniques. Knee Surg. Sports Traumatol. Arthrosc. 23, 3473–3481. https://doi.org/10.1007/s00167-014-3156-5 (2015).
Ebert, A. & Frosch, K. H. Anterior cruciate ligament reconstruction-does the surgeon risk worsening of the clinical outcome during the learning curve if he switches from single bundle technique to double bundle technique?. Z. Orthop. Unfall 154, 449–456. https://doi.org/10.1055/s-0042-111441 (2016).
Fujita, N. et al. Comparison of the clinical outcome of double-bundle, anteromedial single-bundle, and posterolateral single-bundle anterior cruciate ligament reconstruction using hamstring tendon graft with minimum 2-year follow-up. Arthroscopy 27, 906–913. https://doi.org/10.1016/j.arthro.2011.02.015 (2011).
Hussein, M., van Eck, C. F., Cretnik, A., Dinevski, D. & Fu, F. H. Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3- to 5-year follow-up. Am. J. Sports Med. 40, 512–520. https://doi.org/10.1177/0363546511426416 (2012).
Järvelä, S., Kiekara, T., Suomalainen, P. & Järvelä, T. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomized study with 10-year results. Am. J. Sports Med. 45, 2578–2585. https://doi.org/10.1177/0363546517712231 (2017).
Kang, H. J. et al. Single-bundle modified patellar tendon versus double-bundle tibialis anterior allograft ACL reconstruction: a prospective randomized study. Knee Surg. Sports Traumatol Arthrosc. 23, 2244–2249. https://doi.org/10.1007/s00167-014-3021-6 (2015).
Karikis, I., Desai, N., Sernert, N., Rostgard-Christensen, L. & Kartus, J. Comparison of anatomic double- and single-bundle techniques for anterior cruciate ligament reconstruction using hamstring tendon autografts: a prospective randomized study with 5-year clinical and radiographic follow-up. Am. J. Sports Med. 44, 1225–1236. https://doi.org/10.1177/0363546515626543 (2016).
Koga, H. et al. Mid- to long-term results of single-bundle versus double-bundle anterior cruciate ligament reconstruction: randomized controlled trial. Arthroscopy 31, 69–76. https://doi.org/10.1016/j.arthro.2014.07.020 (2015).
Liu, Y., Cui, G., Yan, H., Yang, Y. & Ao, Y. Comparison between single- and double-bundle anterior cruciate ligament reconstruction with 6- to 8-stranded hamstring autograft: a prospective, randomized clinical trial. Am. J. Sports Med. 44, 2314–2322. https://doi.org/10.1177/0363546516650876 (2016).
Lui, P. P., Cheng, Y. Y., Yung, S. H., Hung, A. S. & Chan, K. M. A randomized controlled trial comparing bone mineral density changes of three different ACL reconstruction techniques. Knee 19, 779–785. https://doi.org/10.1016/j.knee.2012.02.005 (2012).
Mayr, H. O. et al. Single-bundle versus double-bundle anterior cruciate ligament reconstruction: a comparative 2-year follow-up. Arthroscopy 32, 34–42. https://doi.org/10.1016/j.arthro.2015.06.029 (2016).
Mayr, H. O. et al. Single-bundle versus double-bundle anterior cruciate ligament reconstruction-5-year results. Arthroscopy 34, 2647–2653. https://doi.org/10.1016/j.arthro.2018.03.034 (2018).
Misonoo, G., Kanamori, A., Ida, H., Miyakawa, S. & Ochiai, N. Evaluation of tibial rotational stability of single-bundle vs. anatomical double-bundle anterior cruciate ligament reconstruction during a high-demand activity-a quasi-randomized trial. Knee 19, 87–93. https://doi.org/10.1016/j.knee.2011.01.003 (2012).
Sasaki, S. et al. Prospective randomized study of objective and subjective clinical results between double-bundle and single-bundle anterior cruciate ligament reconstruction. Am. J. Sports Med. 44, 855–864. https://doi.org/10.1177/0363546515624471 (2016).
Song, E. K. et al. Progression of osteoarthritis after double- and single-bundle anterior cruciate ligament reconstruction. Am. J. Sports Med. 41, 2340–2346. https://doi.org/10.1177/0363546513498998 (2013).
Ventura, A. et al. Single-bundle versus double-bundle anterior cruciate ligament reconstruction: assessment with vertical jump test. Arthroscopy 29, 1201–1210. https://doi.org/10.1016/j.arthro.2013.04.010 (2013).
Volpi, P. et al. ACL reconstruction in sports active people: transtibial DB technique with ST/G vs. transtibial SB technique with BPTB: preliminary results. Injury 41, 1168–1171. https://doi.org/10.1016/j.injury.2010.09.029 (2010).
Xu, Y., Ao, Y. F., Wang, J. Q. & Cui, G. Q. Prospective randomized comparison of anatomic single- and double-bundle anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 22, 308–316. https://doi.org/10.1007/s00167-013-2398-y (2014).
Zaffagnini, S. et al. Single-bundle patellar tendon versus non-anatomical double-bundle hamstrings ACL reconstruction: a prospective randomized study at 8-year minimum follow-up. Knee Surg. Sports Traumatol. Arthrosc. 19, 390–397. https://doi.org/10.1007/s00167-010-1225-y (2011).
Zhang, Z., Gu, B., Zhu, W. & Zhu, L. Double-bundle versus single-bundle anterior cruciate ligament reconstructions: a prospective, randomized study with 2-year follow-up. Eur. J. Orthop. Surg. Traumatol. 24, 559–565. https://doi.org/10.1007/s00590-013-1221-2 (2014).
Xiang, X. et al. Single-tunnel anatomic double-bundle anterior cruciate ligament reconstruction has the same effectiveness as double femoral, double tibial tunnel: a prospective randomized study. Medicine (Baltimore) 98, e14851, doi:https://doi.org/10.1097/md.0000000000014851 (2019).
Maestro, A. et al. ACL reconstruction with single tibial tunnel: single versus double bundle. J. Knee Surg. 25, 237–243. https://doi.org/10.1055/s-0031-1299661 (2012).
Chen, H., Chen, B., Tie, K., Fu, Z. & Chen, L. Single-bundle versus double-bundle autologous anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials at 5-year minimum follow-up. J. Orthop. Surg. Res. 13, 50. https://doi.org/10.1186/s13018-018-0753-x (2018).
Bjornsson, H. et al. Is double-bundle anterior cruciate ligament reconstruction superior to single-bundle? A comprehensive systematic review. Knee Surg. Sports Traumatol. Arthrosc. 23, 696–739. https://doi.org/10.1007/s00167-013-2666-x (2015).
Dong, Z., Niu, Y., Qi, J., Song, Y. & Wang, F. Long term results after double and single bundle ACL reconstruction: Is there any difference? A meta-analysis of randomized controlled trials. Acta Orthop. Traumatol. Turc 53, 92–99. https://doi.org/10.1016/j.aott.2018.12.004 (2019).
Kongtharvonskul, J. et al. Clinical outcomes of double- vs single-bundle anterior cruciate ligament reconstruction: a systematic review of randomized control trials. Scand J. Med. Sci. Sports 23, 1–14. https://doi.org/10.1111/j.1600-0838.2011.01439.x (2013).
Mascarenhas, R. et al. Does double-bundle anterior cruciate ligament reconstruction improve postoperative knee stability compared with single-bundle techniques? a systematic review of overlapping meta-analyses. Arthroscopy 31, 1185–1196. https://doi.org/10.1016/j.arthro.2014.11.014 (2015).
Musahl, V. et al. Comparing stability of different single- and double-bundle anterior cruciate ligament reconstruction techniques: a cadaveric study using navigation. Arthroscopy 26, S41-48. https://doi.org/10.1016/j.arthro.2010.01.028 (2010).
Oh, J. Y. et al. Biomechanical comparison of single-bundle versus double-bundle anterior cruciate ligament reconstruction: a meta-analysis. Knee Surg. Relat. Res. 32, 14. https://doi.org/10.1186/s43019-020-00033-8 (2020).
McInnes, M. D. F. et al. Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: the PRISMA-DTA statement. JAMA 319, 388–396. https://doi.org/10.1001/jama.2017.19163 (2018).
Cumpston, M. et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev 10, Ed000142. https://doi.org/10.1002/14651858.ed000142 (2019).
Higgins, J., Thompson, S., Deeks, J. & Altman, D. Statistical heterogeneity in systematic reviews of clinical trials: a critical appraisal of guidelines and practice. J. Health Serv. Res. Policy 7, 51–61. https://doi.org/10.1258/1355819021927674 (2002).
Moher, D. et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 4, 1. https://doi.org/10.1186/2046-4053-4-1 (2015).
Author information
Authors and Affiliations
Contributions
A.M. had the idea for the article; I.H., D.V.D. and C.M.S. performed the literature search and data analysis; and A.M., I.H., D.V.D. and C.M.S. drafted and critically revised the work for acceptance.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maestro, A., Herruzo, I., Varillas-Delgado, D. et al. Subjective assessment reported by patients shows differences between single-bundle and double-bundle anterior cruciate ligament reconstruction, systematic review and meta-analysis. Sci Rep 11, 15385 (2021). https://doi.org/10.1038/s41598-021-94868-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-94868-0
This article is cited by
-
Double-bundle anterior cruciate ligament reconstruction resulted in better International Knee Documentation Committee objective grading at fifteen year follow-up compared to single-bundle reconstruction
International Orthopaedics (2024)
-
Current trends in the anterior cruciate ligament part 1: biology and biomechanics
Knee Surgery, Sports Traumatology, Arthroscopy (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.