Abstract
Multiple sclerosis (MS) is a neurodegenerative disease of the central nervous system. An increase in MS incidence over time is reported in several regions of the world. We aimed to describe the evolution of the annual MS incidence in the Lorraine region, France, from 1996 to 2015 and to analyze potential components of a possible change by a temporal effect of age at MS onset, MS onset period, and birth cohort, overall and for each sex. Cases were identified from ReLSEP, a population-based registry of MS cases living in Lorraine, northeastern France, with MS onset between 1996 and 2015. Age-period-cohort modeling was used to describe trends in MS incidence. Annual age- and sex-standardized incidences were relatively stable: 6.76/100 000 population (95%CI [5.76–7.91]) in 1996 and 6.78/100 000 (95%CI [5.72–7.97]) in 2015. The incidence ratio between women and men was 2.4. For all time periods, the peak incidence occurred between ages 25 and 35 years. Age-period–adjusted cohort and age-cohort–adjusted period analyses did not reveal a period or cohort effect. The incidence of MS remained stable over the study period in Lorraine, and we could not identify any particular effect of disease onset period or birth period on this evolution.
Similar content being viewed by others
Background
The epidemiology of multiple sclerosis (MS) has changed since the middle of the twentieth century regarding temporal, geographical and demographic alterations in the patterns of disease, mortality rates and causes of death1. According to the Atlas of MS (2020), this neurodegenerative disease of the central nervous system reached a worldwide prevalence of 2.8 million in 20202. MS is the most common non-traumatic disabling disease with an irreversible character and affects young adults, in particular women3,4,5. A combination of environmental and genetic factors could be triggering factors6,7, and they affect the evolution of the risk of MS.
The global prevalence and incidence of MS is increasing in many countries8,9,10. MS represents a social burden in countries where its incidence is high11,12,13 linked to an early loss of productivity14, with life expectancy slightly reduced due to therapeutic progress15. In France, the average annual direct costs associated with MS were estimated at €12,296 in 2014, a global health cost of about €1.2 billion per year16.
The development of McDonald's diagnostic criteria in 200117, revised in 200518, 201018 and 201719 allowed for diagnosing MS earlier in the disease trajectory 20 and closer to symptom onset, which can affect morbidity indicators toward early diagnosis.
The distribution of MS in the France territory is heterogeneous, with a predominance in the northeast versus the southwest21. An increase in incidence has been reported since 1990 in some departments in Lorraine, in the northeast, the MS risk ranging from 3.7 to 7/100,000 during 1990–200022. In 2004, this region had a higher standardized incidence than the French average, which was 7.5/100,000 (7.3–7.6) in the same year, as assessed with national health insurance data23.
Understanding the temporal dynamics of the epidemiology of MS is important for investigations of potential etiological factors and for planning future service provision. Three distinct temporal factors are usually studied as risk factors in a population: age, period, and cohort effects. The effects of these factors tend to have different depictions and underlying biological interpretations for a disease with an undefined etiology. An age-specific effect would suggest that age-associated events and/or exposures affect the MS risk. A calendar period effect would imply different patterns of MS case ascertainment due to a particular exposure during the period and/or changing diagnostic criteria, and a differential birth cohort effect would suggest that risk factor profiles or exposure vary from one generation to the next. Thus, we simultaneously consider age, period and birth cohort as the three covariates affecting the risk of MS, as suggested by Clayton and Schifflers24. However, these three factors are not mutually exclusive because characterization of any two implies knowledge of the third. They can be studied together and then deconstructed independently of each other to assess the respective effect of each.
This study aimed to describe the evolution of the annual incidence of MS in the Lorraine region over the 20-year period from 1996 to 2015 and to analyze the potential components of the change in incidence by a temporal effect of age at disease onset, period of disease onset and birth cohort, for each sex.
Results
Description of the study population
A total of 3,525 incident MS cases were identified between January 1, 1996 and December 31, 2015 in the Lorraine area. The mean ± SD age at MS onset was 34.3 ± 11.3 years (range 5–74). The overall female-to-male ratio was 2.4. The relapsing–remitting MS (RR-MS) form occurred in 90.3% of women and 80.5% of men.
Cases were unequally distributed between age groups regardless of period, with a higher number of cases in young adults (Table 1).
Evolution of the annual incidence standardized by age and by sex
According to INSEE statistics, the population at risk of MS gradually declined, from 2,049,403 in 1996 to 1,992,170 in 2015 (i.e., a decrease of 2.65%). The female-to-male ratio ranged from 1.002 to 1.007. Over the 20 years, the overall trend in incidence of MS in Lorraine was relatively stable, with a difference in the distribution by sex (Fig. 1). The annual incidence rate per 100,000 inhabitants standardized for age and sex was 6.76 (95% CI [5.76–7.91]) in 1996 [women 9.66 (95% CI [7.99–11.63]) and men 3.83 (95% CI [2.81–5.27])] and 6.78 (95% CI [5.72–7.97]) in 2015 [women 9.31 (95% CI [7.57–11.34]) and men 4.20 (95% CI [3.07–5.62])]. It fluctuated between a minimum of 6.67/100,000 (95% CI [5.66–7.82]) in 2008 and a maximum of 9.02/100,000 (95% CI [7.85–10.34]) in 2002.
Age-period-cohort modeling
Relation between age and period, cohort and period and age and cohort:
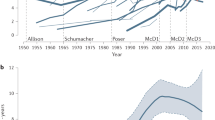
The distribution of the risk of MS in Lorraine was similar for all periods, as shown by the superposition of the age curves over the period brackets (Fig. 2a). There were peaks in the cumulative incidence rate at the key ages of the disease, between age 25 and 35 years (Fig. 2b,c).
Overall, the distribution by period according to cohorts did not show any variation (Fig. 3a). An analysis by sex found for men, for the period 2001–2005, a low incidence rate for the 1955 to 1970 cohorts compared to the other cohorts (Fig. 3b) as well as for women during 2006–2010 for the 1970–1985 cohorts (Fig. 3c). Rates for the 20- to 45-year age groups decreased during 2001–2005 (Fig. 3a) for both sexes and during 2006–2010 for women (Fig. 3c).
The age distribution of incidence rates had the same shape for the cohorts, with most people in the 20–40 age range during our study periods. For cohorts after 1996, our periods were too early to show peaks, and for cohorts before 1956, our periods were too late (Fig. 4).
Nested age-period-cohort analysis
Among the nested models (Table 2), the age-period-cohort model (p = 0.739), age-cohort model (p = 0.682), age-period model (p = 0.103), age-drift model (p = 0.098), and age alone model (p = 0.109) could not be rejected (p > 0.05), whereas the period-cohort model (p < 10–3) was rejected. Analysis of the specific model by sex (Table 3) had similar results. Neither the effect of the period of disease nor the effect of the birth cohort could be isolated, because none of the one-parameter models (Pd, Cd, P and C) fitted the data. We identified no trend by the different models.
On the basis of the AIC, the two best models were age and age-cohort (Table 2). Because as seen above, we found no cohort effect, the age-cohort model fit was probably a reflection of the age effect. Thus, the age-alone model was considered the best model, with neither a cohort nor period effect evidenced.
Discussion
The present study was conducted on incidence data collected from the population-based ReLSEP registry in Lorraine, France, over a period of 20 years (1996–2015). The temporal analysis of the age- and sex-standardized annual incidence showed a relative stability in the annual rates of MS, with no clear upward or downward trend. The age-standardized sex-specific time analysis gave similar results.
In contrast to our study, other studies showed an increasing trend in incidence rate in some countries. In western Norway, the annual incidence increased from 1.9/100.000 (95% CI [1.2–2.6]) during 1953–1957 to 7.2/100.000 (95% CI [6.0–8.5]) during 1978–1982 and 8.5/100.000 (95% CI [7.3–9.7]) during 2003–200710. Over 6 decades in Denmark, the incidence doubled in women, from 5.91/100,000 (95% CI [5.60–6.24]) to 12.33/100,000 (95% CI [11.91–12.75])9. However, in British Columbia, Canada, the incidence of MS was stable from 1996 to 2008, averaging 7.8/100,000 (95% CI [7.6–8.1]) per year25. British Columbia is among the regions with the highest incidence of MS in the world, as is the Lorraine region. Hence, the incidence of MS may not be sensitive to small changes in areas where the risk level is already high.
We found a predominance of RR-MS (87.4%), similar to most European studies26. The female-to-male ratio was 2.4 over the 20 years of our study. Overall the sex ratio was stable over the period, in contrast to other studies finding a marked increase in the female-to-male sex ratio of MS incidence in many countries over the past 50 years4,27,28. In Argentina, Rojas et al. found a variation of 1.8–2.7 over 50 years4, In Lithuania, Valadkeviciene et al. found a variation of 1.5–229. This change in the female-to-male ratio is generally driven by an increasing MS incidence in women rather than a decline in that of men. Palacios et al. found a significant association between ratios of smoking prevalence for women and men in different countries and birth cohorts and corresponding ratios in MS incidence. The authors had estimated that smoking was associated with a 40% average increase in risk of MS30. Before World War II, few women smoked, but the number of women smoking rapidly increased post-war in industrialized countries30. This discrepancy between our study and others could be explained by our relatively limited period of observation, during which environmental exposures did not really change. This is the case for smoking rates for women, which were quite stable over the last decades in France31.
The APC analysis of the distinct contributions of age at MS onset, period of MS onset, and birth cohort retained only the effect of age without a period or cohort effect and no linear and non-linear trend over 20 years. This effect of age on the incidence rate was expected, as observed in this study and in the literature, with a peak of incidence between age 25 and 35 years.
Changes in lifestyle and environmental factors such as smoking32,33,34, vitamin D deficiency35,36 and childhood obesity (strongly correlated with vitamin D deficiency)37,38,39 over the birth cohorts represented in our dataset could lead to a change in the risk of one cohort category over another. In our birth cohorts, ranging from 1926 to 2010, no major changes were found over the entire study period. This finding suggests that the factors affecting disease risk have not changed significantly to affect disease risk trends in the Lorraine region or that there are mitigating factors not yet identified within the region. We also took into account the fact that the present study was based on a quasi-exhaustive registry and identified cases in the affected region in the year corresponding to MS onset. Most studies found an increase in incidence based on the year of diagnosis8 because the change in criteria improved the early identification of cases as well as the multiplication of sources of case registration2, or studies based on the date of MS onset9,10 were conducted over a wider period than ours. In contrast, this mode of case identification is more constant over time and guarantees a more accurate approach for detecting, or not, a trend in incidence over time.
The strengths of this study lie in our studying a large population during a relatively long period and using a quasi-exhaustive registry, the ReLSEP being the only MS registry recognized in France. Also, diagnoses were based on the newest criteria available at the time and made by neurologists. We used the year of MS onset as the year of incidence and not the year of diagnosis. We also considered a 5-year backward step to cover cases reported late in the registry because of the interval between the onset of symptoms and the reporting of the disease40.
One limitation might be that the observation period necessary to identify a change in incidence over time in a high-risk area was not reached. We did not have complementary data such as data on certain demographic factors, diet, and lifestyle (smoking) to concomitantly evaluate their evolution over time in the study population and their possible effect on the stability of incidence in the region. Future perspectives would be to maintain the operation of the registry while enriching it with data that could allow for etiological investigations if, in the long run, a modification of the incidence was detected.
In conclusion, this population-based study in Lorraine, a region classified at high risk for MS in France, did not find any trend in MS incidence during 1996 to 2015. This incidence was relatively stable in men and women, with a similar age effect on the distribution of risk within the general population. We did not show an influence of study period or a temporal variation potentially related to the birth cohort effect. Further study after a longer period of time, while linking the registry with data on factors that may affect the incidence of the disease, would bring further insight.
Material and methods
This was an observational study based on the reporting of MS cases in Lorraine from January 1, 1996 to December 31, 2015 from a regional population-based quasi-exhaustive MS registry (ReLSEP: Registre Lorrain des Scléroses En Plaques).
Study setting
Lorraine is an administrative region located in the northeast of France that had four departments during the study period. Lorraine had 2,311,655 inhabitants on January 1, 199941. Since the end of the 1990s, the Lorraine region has been experiencing a dynamic population shift between a gain linked to a reduction in its migratory deficit, whereby it gained nearly 3400 inhabitants per year until 2011, and a slow decline linked to a low birth–death natural balance and a negative migration balance42.
Data sources, completeness and regulatory aspects
Created in 1996 and covering northeastern France, the ReLSEP registry received its certification from the French registry authorities in 2009 and authorization (No. DR-2014–501) from the French National Commission for Data Protection and Liberties (CNIL). It contains longitudinal clinical and demographic follow-up data for MS patients in the region. Data were collected by using the standardized European Database of Multiple Sclerosis (EDMUS) software43. Cases were identified from hospitals, neurologists in the region, physical medicine and rehabilitation facilities, the national health insurance data, cerebrospinal fluid biochemical analysis laboratories, and the regional MS care network with a quasi-exhaustive representation40 after the multiplication of sources in 201444. The onset of MS was medically confirmed according to the criteria of Poser et al. (1983) or McDonald et al. (2001) and modified by Polman et al. (2005, 2010). The procedure for identifying reported cases in Lorraine departments was extended to neighbouring departments. Each patient included in the ReLSEP was informed and asked to sign a written consent for reporting in the registry.
Data management
Inclusion criteria were classification as an incident MS case between 1996 and 2015 and living in Lorraine during the considered period. The forms of initial diagnosis were RR-MS and primary-progressive MS (PP-MS). We excluded patients with neuromyelitis optica and radiologically and clinically isolated syndromes not reported as MS.
Data concerning all cases identified over the study period were extracted by using EDMUS software on January 1, 2021. The variables of interest were demographic data (age, sex), date of MS onset represented by the first symptom corresponding to the year of incidence, and the MS type at the time of diagnosis (RR-MS, PP-MS).
Data on the Lorraine population per year, by age groups of 5 years stratified by sex were extracted from the national census at the National Institute of Statistics and Economic Studies (INSEE)45.
Statistical analysis
The MS cases and reference population data were classified into 12 age groups of 5 years each, from 5–9 to ≥ 60 years (i = 1, 2, 3, …I) and four periods of 5 years each from 1996–2000 to 2011–2015 (j = 1, 2,3, … J) based on their respective year of MS onset. This 5-year age and period classification was used to create K = 15 birth cohorts (K = I + J − 1)46. The corresponding population groups were constructed by averaging the population estimates on January 1 of the year under consideration and on January 1 of the following year to produce a relevant population denominator. The annual age- and sex-standardized incidence rates of MS were calculated from these data. The age-standardized sex-specific incidence rates were calculated by the direct standardization method47 with the French population structure on January 1, 1999, used as a standard. The confidence intervals for the standardized incidence rates were calculated with the Gamma distribution method48.
Age-period-cohort modeling
Age-period-cohort models have been widely used in epidemiology for several decades. The models have three variables: age, period and cohort. The incidence rate modeling uses a generalized linear model with a predictor of the following form49:
The predictor μi,k is constructed from time effects for age, αi; period, βj; and cohort, γk and an error term, δ. However, these time effects cannot be fully recovered from the predictor because of the identification problem. In other words, knowledge of the predictor from the likelihood, which is a function of the predictor, is not enough to reveal the time effects. This identification problem can be circumvented by a parsimonious parametrization50. This parametrization allowed for the formulation of 14 nested sub-models within the age-period-cohort model (Fig. 5). The deviance of the sub-models is calculated against a chi-square distribution, its p-value and the Akaike Information Criteria (AIC) associated with the log-likelihood ratio statistics for the sub-models against the age-period-cohort model.
Diagram of the age-period-cohort model and its sub-models. The models are nested from right to left. APC age-period-cohort model, AC age-cohort model, AP age-period model, Ad age-drift model, PC period-cohort model, Pd period-drift model, Cd cohort-drift model, A age model, P period model, C cohort model, A age model, t trend model, At age-trend model, Pt period-trend model, Ct cohort trend model, 1: intercept model. The term drift means that there must be some temporal variation in rates that cannot be interpreted as the effect of other non-specified parameters in the model.
Analyses were conducted with R 3.4.2. APC analyses were conducted with the apc package 2.0.0. All methods were carried out in accordance with relevant guidelines and regulations.
Ethics approval
The data are extracted from a population-based register certified by the French registry authorities in 2009 and approved by the French National Commission for Data Protection and Liberties (CNIL).
Data availability
All data are available from the authors on reasonable request.
References
Magyari, M. & Sorensen, P. S. The changing course of multiple sclerosis: rising incidence, change in geographic distribution, disease course, and prognosis. Curr. Opin. Neurol. 32, 320–326 (2019).
Atlas-3rd-Edition-Epidemiology-report-EN-updated-30-9-20.pdf.
Nakken, O., Lindstrøm, J. C. & Holmøy, T. Sex ratio in multiple sclerosis mortality over 65 years; an age-period-cohort analysis in Norway. J. Neurol. 265, 1295–1302 (2018).
Rojas, J. I. et al. Gender ratio trends over time in multiple sclerosis patients from Argentina. J. Clin. Neurosci. 38, 84–86 (2017).
Trojano, M. et al. Geographical variations in sex ratio trends over time in multiple sclerosis. PLoS ONE 7, e48078 (2012).
Handel, A. E., Handunnetthi, L., Giovannoni, G., Ebers, G. C. & Ramagopalan, S. V. Genetic and environmental factors and the distribution of multiple sclerosis in Europe. Eur. J. Neurol. 17, 1210–1214 (2010).
Michel, L. Environmental factors in the development of multiple sclerosis. Rev. Neurol. (Paris) 174, 372–377 (2018).
Salhofer-Polanyi, S. et al. Epidemiology of Multiple Sclerosis in Austria. Neuroepidemiology 49, 40–44 (2017).
Koch-Henriksen, N., Thygesen, L. C., Stenager, E., Laursen, B. & Magyari, M. Incidence of MS has increased markedly over six decades in Denmark particularly with late onset and in women. Neurology 90, e1954–e1963 (2018).
Grytten, N., Aarseth, J. H., Lunde, H. M. B. & Myhr, K. M. A 60-year follow-up of the incidence and prevalence of multiple sclerosis in Hordaland County, Western Norway. J. Neurol. Neurosurg. Psychiatry https://doi.org/10.1136/jnnp-2014-309906 (2015).
Ernstsson, O. et al. Cost of illness of multiple sclerosis - a systematic review. PLoS ONE 11, e0159129 (2016).
Paz-Zulueta, M., Parás-Bravo, P., Cantarero-Prieto, D., Blázquez-Fernández, C. & Oterino-Durán, A. A literature review of cost-of-illness studies on the economic burden of multiple sclerosis. Mult. Scler. Relat. Disord. 43, 102162 (2020).
Sicras-Mainar, A., Ruíz-Beato, E., Navarro-Artieda, R. & Maurino, J. Impact on healthcare resource utilization of multiple sclerosis in Spain. BMC Health Serv. Res. 17, 854 (2017).
Palmer, A. J. et al. Modelling the impact of multiple sclerosis on life expectancy, quality-adjusted life years and total lifetime costs: Evidence from Australia. Mult. Scler. 26, 411–420 (2020).
Leray, E. et al. Excess mortality in patients with multiple sclerosis starts at 20 years from clinical onset: data from a large-scale french observational study. PLoS ONE 10, e0132033 (2015).
Bruno, D. et al. Economic burden of multiple sclerosis in France estimated from a regional medical registry and national sick fund claims. Mult. Scler. Relat. Disord. 36, 101396 (2019).
McDonald, W. I. et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the international panel on the diagnosis of multiple sclerosis. Ann. Neurol. 50, 121–127 (2001).
Polman, C. H. et al. Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria”. Ann. Neurol. 58, 840–846 (2005).
Thompson, A. J. et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 17, 162–173 (2018).
Schwenkenbecher, P. et al. Impact of the McDonald criteria 2017 on early diagnosis of relapsing-remitting multiple sclerosis. Front. Neurol. 10, 188 (2019).
Pivot, D. et al. Geographical heterogeneity of multiple sclerosis prevalence in France. PLoS ONE 11, e0167556 (2016).
Debouverie, M., Pittion-Vouyovitch, S., Louis, S., Roederer, T. & Guillemin, F. Increasing incidence of multiple sclerosis among women in Lorraine, Eastern France. Mult. Scler. J. 13, 962–967 (2007).
Fromont, A. et al. Geographic variations of multiple sclerosis in France. Brain 133, 1889–1899 (2010).
Clayton, D. & Schifflers, E. Models for temporal variation in cancer rates. I: Age-period and age-cohort models. Stat. Med. 6, 449–467 (1987).
Kingwell, E. et al. High incidence and increasing prevalence of multiple sclerosis in British Columbia, Canada: findings from over two decades (1991–2010). J. Neurol. 262, 2352–2363 (2015).
Pugliatti, M. et al. The epidemiology of multiple sclerosis in Europe. Eur. J. Neurol. 13, 700–722 (2006).
Harbo, H. F., Gold, R. & Tintoré, M. Sex and gender issues in multiple sclerosis. Ther. Adv. Neurol. Disord. 6, 237–248 (2013).
Debouverie, M. Gender as a prognostic factor and its impact on the incidence of multiple sclerosis in Lorraine, France. J. Neurol. Sci. 286, 14–17 (2009).
Valadkeviciene, D., Kavaliunas, A., Kizlaitiene, R., Jocys, M. & Jatuzis, D. Incidence rate and sex ratio in multiple sclerosis in Lithuania. Brain Behav. 9, e01150 (2019).
Palacios, N., Alonso, A., Bronnum-Hansen, H. & Ascherio, A. Smoking and increased risk of multiple sclerosis: parallel trends in the sex ratio reinforce the evidence. Ann. Epidemiol. 21, 536–542 (2011).
Tableau de bord des indicateurs relatifs au tabac et au tabagisme en France - OFDT. https://www.ofdt.fr/statistiques-et-infographie/tableau-de-bord-tabac/.
Thompson, A. J., Baranzini, S. E., Geurts, J., Hemmer, B. & Ciccarelli, O. Multiple sclerosis. Lancet 391, 1622–1636 (2018).
Handel, A. E. et al. Smoking and multiple sclerosis: an updated meta-analysis. PLoS ONE 6, e16149 (2011).
Ramanujam, R. et al. Effect of smoking cessation on multiple sclerosis prognosis. JAMA Neurol. 72, 1117–1123 (2015).
Ascherio, A. Environmental factors in multiple sclerosis. Expert Rev. Neurother. 13, 3–9 (2013).
Pierrot-Deseilligny, C. & Souberbielle, J.-C. Vitamin D and multiple sclerosis: an update. Mult. Scler. Relat. Disord. 14, 35–45 (2017).
Pereira-Santos, M., Costa, P. R. F., Assis, A. M. O., Santos, C. A. S. T. & Santos, D. B. Obesity and vitamin D deficiency: a systematic review and meta-analysis. Obes. Rev. 16, 341–349 (2015).
Mokry, L. E. et al. Obesity and multiple sclerosis: a mendelian randomization study. PLoS Med. 13, e1002053 (2016).
Hedström, A. K., Olsson, T. & Alfredsson, L. High body mass index before age 20 is associated with increased risk for multiple sclerosis in both men and women. Mult. Scler. 18, 1334–1336 (2012).
El Adssi, H., Debouverie, M., Guillemin, F., & LORSEP Group. Estimating the prevalence and incidence of multiple sclerosis in the Lorraine region, France, by the capture-recapture method. Mult. Scler. 18, 1244–1250 (2012).
Estimation de la population au 1er janvier 2021 | Insee. https://www.insee.fr/fr/statistiques/1893198.
30 ans de démographie : la Lorraine réduit son déficit migratoire - Economie Lorraine | Insee. https://www.insee.fr/fr/statistiques/1292262.
Confavreux, C., Compston, D. A., Hommes, O. R., McDonald, W. I. & Thompson, A. J. EDMUS, a European database for multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 55, 671–676 (1992).
Debouverie, M., Pittion-Vouyovitch, S., Louis, S. & Guillemin, F. Natural history of multiple sclerosis in a population-based cohort. Eur. J. Neurol. 15, 916–921 (2008).
Insee - Institut national de la statistique et des études économiques. https://www.insee.fr/fr/accueil.
Nielsen, B. Deviance analysis of age-period-cohort models, No 2014-W03, Economics Papers, Economics Group, Nuffield College, University of Oxford (2014).
Fleiss, J. L., Levin, B. & Paik, M. C. The standardization of rates. In: Statistical methods for rates and proportions. J. Wiley. 3nd edn, 627–647 (2003).
Fay, M. P. & Feuer, E. J. Confidence intervals for directly standardized rates: a method based on the gamma distribution. Stat. Med. 16, 791–801 (1997).
Nielsen, B. apc: An R Package for Age-Period-Cohort Analysis. R J. 7, 52 (2015).
Kuang, D., Nielsen, B. & Nielsen, J. P. Identification of the age-period-cohort model and the extended chain-ladder model. Biometrika 95, 979–986 (2008).
Acknowledgements
On behalf of ReLSEP registry, the authors would like to thank all the collaborating institutions: the national health insurance fund, specialized biology laboratories, the Technical Agency of Information on Hospitalization (ATIH), the LORSEP and alSacEP networks, hospital and private neurologists, as well as the collaborators of the registry : Alfousseny Coly, Amandine Ziegler, Clotilde Latarche, Jean-Marc Virion, Marc Soudant, Nathalie Dumont, Nathalie Pierrez, Nadine Valentin, Samia Mahmoudi, Sandrine Grandclere, Sandrine Tyrode, Sylvie Klein, Tubanur Unal.
Funding
This research did not receive any specific funding from agencies/institutions in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
J.E., F.G., G.M., M.D. and B.G. contributed to the study conceptualization and design. M.S. led the preparation of the study data. B.G. performed the statistical analyses. All authors contributed to interpretation of the results. B.G., F.G., J.E., and G.M. drafted the manuscript. All authors contributed to the critical revision of the manuscript. All authors approved the final manuscript. F.G. is the guarantor for the study. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gbaguidi, B., Guillemin, F., Soudant, M. et al. Age-period-cohort analysis of the incidence of multiple sclerosis over twenty years in Lorraine, France. Sci Rep 12, 1001 (2022). https://doi.org/10.1038/s41598-022-04836-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-04836-5
This article is cited by
-
Inflammation as common link to progressive neurological diseases
Archives of Toxicology (2024)
-
Male sexual and reproductive health in multiple sclerosis: a scoping review
Journal of Neurology (2024)
-
Performance of administrative databases for identifying individuals with multiple sclerosis
Scientific Reports (2023)
-
The Use of Stem Cells as a Potential Treatment Method for Selected Neurodegenerative Diseases: Review
Cellular and Molecular Neurobiology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.