Abstract
Diarrheagenic Escherichia coli are a number of pathogenic E. coli strains that cause diarrheal infection both in animal and human hosts due to their virulence factors. A cross sectional study was conducted between November, 2016 and April, 2017 to isolate and molecularly detect pathogenic E. coli from diarrheic calves to determine the pathogenic strains, antibiogram and associated risk factors in Jimma town. Purposive sampling technique was used to collect 112 fecal samples from diarrheic calves. Conventional culture and biochemical methods were conducted to isolate E. coli isolates. Molecular method was followed to identify virulence factors of pathogenic E. coli strains. Antimicrobial sensitivity patterns of the isolates were tested using the Kirby–Bauer disk diffusion method. A structured questionnaire was also used to collect information from dairy farms and socio-demographic data. The overall isolation rate of E. coli in calves was 51.8% (58/112) (95% CI 42.0–61.0). The occurrence of the bacterium differed significantly by age, colostrum feeding time, amount of milk given per time and navel treatment (P < 0.05). Multivariable analysis revealed that the odds of being infected was significantly highest in calves which fed 1–1.5 L amount of milk per a time (OR 5.38, 95% CI 1.66–17.45, P = 0.005). The overall virulence genes detection rate was 53.5% (95% CI 40.0–67.0). Eleven (19.6%) of eaeA, 6 (10.7%) of Stx1 and 13 (23.2%) of Stx2 genes were detected from calves isolates. Except ciprofloxacillin, all isolates were resistant to at least one drug. Multi drug resistance was recorded in 68.0% (38/56) of calves isolates. Neomycin, 83.3% (25/30), followed by amoxicillin, 53.3% (16/30) were the highest resisted virulence genes. The study demonstrated considerable isolation rate, multiple antimicrobial resistant isolates and high resistant virulent genes in diarrheic calves. It also indicated that the potential importance of calves as source of pathogenic E. coli strains and resistant genes for human diarrhea infection. Improving the hygienic practice of farms and wise use of antimicrobials could help to reduce the occurrence of pathogenic E. coli in farms. Hence, further studies are needed to describe all virulent factors and serotypes associated with the emergence of drug resistant pathogenic E. coli strains in calves.
Similar content being viewed by others
Background
Cattle production plays an important role in the economy and livelihood of farmers and pastoralists worldwide. Despite the large livestock population of Ethiopia, the economic benefits remain marginal due to prevailing diseases, poor nutrition, poor animal production systems, reproductive inefficiency, management constraints and general lack of veterinary care1. The future of any dairy and beef production depends on the successful raising of calves and heifers for replacement. The health and management of replacement animals are important components of total herd profitability. Diarrhea is one of the very common disease syndrome in neonatal calves in different countries and this can have severe impacts both economically and in terms of animal welfare2.
Calf diarrhea is a multifactorial disease which, despite decades of research in the topic, remains the most common cause of calf mortality3. There is multitude of interaction in the none infectious causes like gaps in management of animals, inadequate nutrition, exposure to severe environment, insufficient attention to the new borns, and the infectious diseases. According to Cho4, 80% of diarrheic calves tested were positive for at least one of the target enteric pathogens suggesting that infectious factor is still a major cause of calf diarrhea5. The prevalence, antibiogram and epidemiological features of E. coli as the causative agent of diarrhea vary from region to region around the world, and even between and within countries in the same geographical area6.
Neonatal diarrhea has been commonly attributed to multiple enteric pathogens of bacteria, protozoa and viruses7,8. Although co-infection considerably worsens the disease, sometimes single infection is recorded and many of the cases are predominantly related to bacterial pathogens9,10. Among the bacterial pathogens, diarrhea in calves due to E. coli remains common devastating disease all over the world, particularly in calves less than 3 months of age11,12. Although E. coli is the predominant member of the animal and human intestinal microflora, a number of strains have developed the ability to cause diseases particularly of the gastrointestinal in animal and human hosts13. Diarrheagenic strains of E. coli are categorized based on distinct epidemiological and clinical features, specific virulence determinants and association with certain serotypes14,15.
New strains of E. coli arise all the time from the natural biological process of genetic variability and hence monitoring the levels of E. coli contamination is important. The development of highly applicable nucleic acid based diagnostic analysis on the basis of culture media isolation and biochemical reactions enabled the detection of different pathotypes of diarrheagenic E. coli. Among these, PCR is a commonly used molecular method that gives rapid and reliable detection of pathogenic E. coli strains that could show the prevalence and distribution of these pathogens16,17.
The advent of advanced molecular studies showed that animal to human disease transmission is by cross infection in experimental models, animal handling and contaminated food consumption. The direct and indirect economic impacts of neonate animals is one of the most common and devastating conditions encountered in the animal agriculture industry18.
The high frequency and persistence of calf diarrhea in farms has gained the interest of many researches. In central and south eastern part of Ethiopia, limited researches indicate calf mortality rate and the supposed infectious agents. A few studies show mortality in the first 6 months of calf hood ranging from 7 to 25%18,19. E. coli isolates in calf diarrhea accounts 37% Gebregiorgis and Tessema20 in Kombolcha District, 50.9% Yakob21 in Arsi zone and 69.5% Yimer22 in North Shewa zone of Ethiopia. In south western part of the country, particularly in Jimma town and its surroundings, the information on cause of diarrhea in calves and its associated factors is minimal.
Understanding the population structure of pathogenic E. coli is important since it impacts the effectiveness of molecular epidemiological studies. Molecular detection of the supposed pathogenic E. coli strains isolated from calves in Ethiopia is limited. This hinders implementation of effective control and preventive measures. In addition, most pathogenic bacteria that are commonly involved in causing infection to animals and humans have shown considerable degree of resistance to commonly used antimicrobials in this country23. Uncontrolled application of antimicrobials is rooted from lack of particular pathogenic strain identification from a host at particular place that leads to an increase in the rate of antimicrobial resistance which has significant effect for the problem to persist. Therefore, this study was carried out to isolate and molecularly detect virulence genes of pathogenic E. coli strains, identifies their antibiogram and associated risk factors from diarrheic calves in dairy farms in Jimma town.
Results
Overall isolation of Escherichia coli in calf diarrhea
Escherichia coli was recovered in 58 (51.8%) out of the 112 diarrheic calves that showed calf diarrhea. In the present study, the occurrence of diarrhea due to E. coli differed significantly by age, colostrum feeding time, amount of milk given per time and navel treatment. A higher occurrence of diarrhea due to E. coli was detected in calves of 1–2 weeks old (29.5%), in calves first colostrum fed less than 6 h (37.5%), calves that fed 1–1.5 L of milk per a time (33.1%) and in not navel treated calves during birth (31.3%). Its occurrence did not differ by sex, breed and calving facility (Table 1).
Univariable and multivariable logistic regression analysis of risk factors associated with calf diarrhea
From univariable logistic regression analysis, independent variables such as age, first colostrum feeding time, amount of milk given per time and navel treatment were significantly associated with E. coli isolates (P < 0.05). On the other hand sex, breed and calving facility were not significantly associated with E. coli isolates as shown in Table 2. The variables with P value < 0.25 in univariable logistic regression analysis were taken to multivariable logistic regression analysis to control confounders. Followed, age, sex, time of first colostrum feeding, amount of milk given per time and navel treatment were entered to multivariable logistic analysis.
Multivariable logistic regression analysis was carried out to observe the independent effects of each risk factors in relation to the occurrence of E. coli isolates in diarrheic calves. Accordingly, variables such as age (P = 0.022), first colostrum feeding time (P = 0.048) and amount of milk given per time (P = 0.005) were identified as the significant independent predictors for occurrence of E. coli isolates in calf diarrhea. The log odds ratio indicates that calves within the age category between 1 and 2 weeks (AOR = 4.029,9 5% CI 1.22–13.27, P 0.022) are more susceptible to diarrhea due to E. coli compared to other age categories of diarrheic calves. Calves that were fed first colostrum in more than 6 h (AOR = 3.730, 95% CI 1.01–13.77, P = 0.048) were more susceptible than those fed before 6 h. The occurrence of the bacteria in calf diarrhea was also more likely in calves also significantly associated with thethat fed 1–1.5 litter amount of milk given per time (AOR = 5.38, 95% CI 1.66–17.45, P = 0.005) than those fed more. None of the variables found to be collinear and there was insignificance difference between the observed and the predicted values with Chi-square = 3.610, P = 0.890 which was fitted well with the data.
Description of dairy farms and owners based on questionnaire and observation
A total of 35 questions comprised five areas of interest namely farm characteristics, calving and care of the newborn, calf housing, calf feeding, weaning and calf disease in pre-weaned calves were administered. Owners of 54 farms used for sample collection were interviewed. The farms harbor cross Holstein Friesian 94 (83.9%) and local 18 (16.1%) breeds of calves. Seventeen (31.5%) of the farms in the study were intensively managed with an average number of 8 calves per herd and most of smallholder farms had 2 calves per herd.
More than three-forth of the dairy farmers had knowledge of the advantage of colostrum feeding. Ninety two (82.1%) out of 112 diarrheic caves fed first colostrum within less than 6 h and 46 (41.1%) of calves were kept in separated calving pen that were often not cleaned and disinfected regularly. Navel treatment during birth of calves was practiced in 58 (51.8%) of the visited farms. The practice of providing bedding for calves was limited in large dairy farms and none in small holders. All study farms fed whole milk for calves two times daily by bucket feeding with the exception of few small holder farms that allowed calves to suckle their dams. Special starter feed was not used in any of the farms rather straw, hay and concentrates that were given to cows were used for calves. Forty six (85.2%) of farms weaned calves at 3 months of age whereas 8 (14.8%) of them weaned at 4 months. In general, the weaning age was lower for male calves, mostly under 3 months. In all large dairy farms, there were vet personnel employed to deal with health aspects of the farms. Smallholder dairy farms call private veterinary practitioners whenever their animals face health problems. From farm managers or owners that mentioned calf health problems, majority of them complained that diarrheal and respiratory tract diseases were the most frequent diseases encountered in calves.
Polymerase chain reaction based detection of virulence genes
Of the total 112 fecal samples from diarrheic calves 58 isolates were presumed to be E. coli positive by biochemical tests. Fifty six isolates, two of the isolates were not recovered during DNA extraction, were then subjected to virulence genes specific PCR assays. The overall detection rate of the three genes tested from positive isolates in calves was 30 (53.5%).
Eleven (19.6%) of eaeA gene, 6 (10.7%) of stx1 gene and 13 (23.2%) of stx2 gene positive isolates were detected by PCR from diarrheic calves (Table 3) and illustrated by documented jell as in Fig. 1. All the virulence genes involved were significantly associated with diarrhea due to E. coli (P < 0.05).
(A–C) Amplification of virulence genes in E. coli isolates from diarrheic calves and the images are a product of time averaged data. M marker, N negative control, P positive control; Numbers = 1–11 representative sample numbers; (A) eaeA gene with 450 bp; (B) stx2 gene with 350 bp; (C) stx1 gene with 110 bp.
Antimicrobial resistance profiles of Escherichia coli
Mono drug resistance
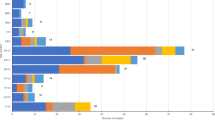
The antimicrobial susceptibility features of 56 isolates from diarrheic calves are given in Table 4. The highest sensitivity of ciprofloxacillin and norfloxacillin were recorded in 98.2% of the isolates. Norfloxacillin and oxytetracycllin for all isolates did not show intermediate resistance while another tested drugs was recorded as intermediate resistance in one or more of the tested isolates. The highest resistance isolates was recorded for neomycin (76.8%) followed by amoxicillin (48.2%). Resistance to chloramphenicol and norfloxacillin were observed in 1.8% of the isolates from calves isolates.
Multi drug resistance
The multi-drug resistance features of the E. coli isolates are shown in Table 5. Of the tested 56 isolates from calves, 38 (68.0%) were resistant to two or more (up to eight) antimicrobials. Twenty three multi drug resistance profiles were observed and the number of isolates resistant to two drugs were higher followed by four drugs resistant isolates. The NEO, AMC (7/38) phenotype occurred more frequently followed by the NEO, W, OT, S3 (3/38) phenotype from calves isolates.
Virulence genes resistance
The antimicrobial resistance profile of the pathogenic 30 E. coli strain genes is shown in Table 6. The highest resistance to the strains of sampled calves was recorded for neomycin 25 (83.3%) followed by amoxicillin 16 (53.3%) whereas resistance to norfloxacillin 1 (3.3%) showed least resistance.
Out of 30 calves isolated of E .coli genes, eaeA gene 9 (81.8%), stx1 gene 4 (66.6%) and stx2 gene 12 (92.3%) encoded isolates showed highest resistant for neomycine. On the other hand, streptomycine 2 (18.2%) for eaeA gene, amoxicillin and oxytetracycllin 1 (16.6%) for stx1 gene and norfloxacillin and streptomycin for stx2 gene showed all 1 (7.7%) least resistant from calves isolates. Chloramphenicol, ciprofloxacillin and gentamycin in diarrheic calves isolates did not show resistance to the identified virulent genes of E. coli.
Discussion
This study was conducted to assess the overall isolation rate, virulence factors of pathogenic strains and antibiogram profile of E. coli isolated from diarrheic calves in Jimma town. The importance of detecting pathogenic E. coli from diarrheic calves has great significance. Calf morbidity and mortality result in great economic losses as calves are replacement stocks in a cattle production system and diarrheic calves are also potential source of the bacterium for human infection. In this study, the overall isolation rate of E. coli in calves was 51.8% and significantly differed by age, time of first colostrum feeding, amount of milk given per time and navel treatment during birth. Furthermore, pathogenic E. coli strains were detected molecularly and antimicrobial susceptibility patterns of the isolates were also investigated.
Overall isolation of Escherichia coli in calf diarrhea
The overall isolation rate of E. coli in diarrheic calves was 51.8%. This isolation rate was in agreement with the findings of Yakob21 in Arsi Zone (50.9%), Ghada et al.24 in Egypt (50%) and Hossain et al.25 in Bngladish (49%) from diarrheic calves. The result obtained was lower than the findings of Dawit26 in Addis Ababa and Debre Zeit (64%), Yimer22 in North Shewa (69.5%) and Sunday et al.27 in Nigeria (63.2%). In contrast, this finding was higher than the reports of Abdisa and Minda28 in Holeta (12.5%), Gebregiorgis and Tessema20 in Kombolcha (36.8%) and Bekele et al.19 in Hawasa (37%). The variation in isolation rates could be due to difference in sample size, age of the calves, geography, management of the farms and the isolation methods used. In a study that looked at equal 50 dairy farms in Ohio and Norway, E. coli was not found in any of the Norwegian farms but was found in 4 of the Ohio farms indicated that its prevalence may be affected by geography and management variations6.
Risk factors associated with calf diarrhea
The occurrence of E. coli causing calf diarrhea was associated with many risk factors that were found to be significantly associated but some were not. E. coli in diarrheic calves was isolated from all age groups examined, but the odds of being infected was high among age category of 1–2 weeks. The association between the age level and diarrhea was being curvilinear as observed elsewhere20,22,29. This could be related to the beginning of stress due to environmental exposure and infection pressure when the immune system of the calves is still developing30. Neonatal calves under 1 week of age are particularly susceptible because of incomplete establishment of the normal flora of the intestine, the presence of naive immune system and access of receptors for the adhesions of E. coli on the first week of life of the calves. The isolation rates of the bacterium in the subsequent age groups were shown to decrease as supported by the literature31.
Calving management and care of the newborn are important for the calves’ health. In the present study, the occurrence of E. coli in diarrheic calves due to the time of first colostrum feeding was considered and significantly differed (P < 0.05). The isolation rate of E. coli isolates was significantly higher in calves that fed first colostrum in more than 6 h than those fed before 6 h early. This is in accordance with study performed in North Showa in which the isolation rate of E. coli was 100% out of 23 diarrheic calves that fed first colostrum in more than 6 h22. Klein et al.32 in Austria also indicated that the importance of early colostrum management concerning the diarrheal infection in neonates. Matte et al.33 found that 61% of colostral immunoglobulin containing 80 mg/ml of IgG is absorbed in 6 h and decreases sharply thereafter. By 24 h, the gut can absorb only 11% of what it originally could have absorbed at birth and digestive enzymes break down and digest all of the antibodies34. This indicates that the first 6 h are the period in which maximum absorption of colostral immunoglobulin takes place. For adequate passive transfer of immunoglobulin, in addition to time, quantity and quality of the immunoglobulin fed to the calf plays an important role32.
The occurrence of E. coli in diarrheic calves was also significantly associated with the amount of milk given to the calves per time (P < 0.05). Thus, diarrheic calves that fed less (1–1.5 litter) milk per time were highly infected with E. coli than those fed more milk. The finding is in line with the idea feeding sufficient amounts of milk as per the calf body weight has more benefit on health, growth and performance later in life than reduced milk feeding35.
Furthermore, the isolation rate of the bacterium was significantly higher in calves which did not get navel treatment during birth. This could be as the contaminated umbilicus provides the bacterium with an easy route of entry to the neonatal calf’s bloodstream and body. When a calf has septicemia due to E. coli, as the bacterium or its toxins presented in blood, the infection disseminates and damages many different organs and develops diseases including diarrhea as documented by Walter36. However, in the multivariable logistic regression analysis, the association of navel treatment was not significant (P > 0.05). In the present study sex, breed and calving facility of calves were not significantly associated with the occurrence of E. coli in calf diarrhea which is similar with the finding of Yimer22 and Klein et al.32.
Detection of virulence genes of Escherichia coli
Detailed studies of the virulence factors produced by E. coli strains in farm animals are needed. In this study, 30 (53.5%) pathogenic E. coli strains out of 56 isolates in diarrheic calves were positive for at least one of the virulence factors involved and significantly associated (P < 0.05). Eleven (19.6%), 6 (10.7%) and 13 (23.2%) positive strains for eaeA, stx1 and stx2 genes, respectively were found positive. The occurrence of E. coli eaeA virulent genes in this study was significantly associated with E. coli infection in calf diarrhea. The result obtained is comparable with the findings of Hur et al.37 in Korea (17%) and Andrade et al.38 in Brazil (24.3%) eaeA gene. Reports of Tan et al.39 in Vietnam (9.8%) and Islam et al.29 in Bangladish (12.5%) showed lower isolation rate of the same gene isolated from diarrheic calves. In contrary, higher prevalence of eaeA gene was reported by Dastmalchi and Ayremlou40 in Iran (26.9%) and 100% eaeA gene prevalence in Iraq41 of the same gene from diarrheic calves.
Shiga toxin producing E. coli strains from diarrheic calves isolates were 33.9% (10.7% of stx1 gene and 23.2% of stx2 gene). The presence of stx1 gene (10.7%) found in this study was significantly associated with calf diarrhea due to E. coli. The occurrence of stx1 gene coincided with the report of Tahamtan42 (2010) in Iran (10.3%) calf isolates. The current finding was different from lower report of Askari et al.43 in Iran (5%); and higher reports of Yahya et al.44 in Turkey (42.8%), Tan et al.39 in Vietnam (46%) and Andrade et al.38 in Brazil (82.8%). The present finding on stx2 gene (23.2%) was also significantly associated with calf diarrhea due to E. coli in calves. The result was in agreement with the report of Orden et al.45 for stx2 gene in Iran (20.9%) diarrheic caves; however, it was higher than that of Andrade et al.38 report from Brazil (4%). In contrast, it is lower than the reports of Yahya et al.44 from Turkey (71.4%) and Tan et al.39 from Vietnam (73%).
In this study, higher frequency of stx2 (23.2%) genes than stx1 gene (10.7%) was observed which is in agreement with Dastmalchi and Ayremlou40 who reported stx2 (30%) and stx1 (10%) in diarrheic calves in Iran. However, it is contrary to the observations of Srivani et al.46 who reported predominance of stx1 (16.04%) over stx2 (12.64%) in diarrheic calves in India. The relative occurrence of STEC virulence factors changed as calves aged with stx1 positive isolates replaced by stx2 positive isolates47. The differences of the virulent genes were likely due to geographical as per LeJeune et al.6, season of sample taken as Fernandez et al.48, sample size or number of experimented isolates, age of samples and the calves and differences in detection methods47. High rates of pathogenic E. coli strain colonization found in cattle in many countries indicate that cattle are important reservoir of different E. coli pathotypes49. The current study suggests that calves could serve as important reservoir for pathogenic E. coli strains or human infection in Ethiopia.
The virulence factors found from the present study indicated that diarrhea in calves due to E. coli could be ascribed mainly to Enteropathogenic E. coli (EPEC) consisted eaeA genes and Enterohaemorrhagic E. coli (EHEC) of shiga toxin producing E. coli pathotypes which was supported by Alikhani et al.50. The present investigation of the virulent genes was restricted to individual genes due to resource limitation. However, E. coli strains in others previously done studies harbored the eaeA, stx1 and stx2 genes were found alone as well as in combination51. Some groups and strains of E. coli could share similar virulence traits and there are many overlaps in the mechanisms of pathogenesis for various pathotypes. The virulence genes carried by these pathogenic E. coli groups are contained within mobile genetic elements and can be transferred between strains to create “emerging” strains as documented by Lucia et al.52. The relatively high occurrence of the stx2 gene comparing to stx1 gene in this study suggests that E. coli carrying a combination of the eaeA and stx2 genes is more common than the combination of eaeA and stx1 genes. The virulence factors eaeA, stx1 and stx2 genes were indicated as important diarrhea causative pathogens of the neonates and other extra enteric severe human illnesses like haemolytic uraemic syndrome53. However, the present study could not screen all the remained virulence genes of the pathotypes and serotype characterization.
Antimicrobial resistance profiles of Escherichia coli isolates
Antimicrobial resistance levels have markedly increased over the years that could be due to indiscriminate and widespread uses of antimicrobials both in the veterinary and public health practices54. The highest sensitivity for ciprofloxacillin and norfloxacillin were recorded in 98.2% of isolates from diarrheic calves. This finding was consistence with high susceptibility finding of E. coli isolates to norfloxacillin (98%) as Ewa et al.55. reported in Poland, and ciprofloxacillin (98.8%) and norfloxacillin (100%) found in Bangladish56. The high sensitivity to the mentioned drugs might be attributed to recent development of the drugs and their seldom use in treatment of enteric infections57,58.
Except ciprofloxacillin, all isolates were resistant to at least a single antimicrobial agent. Neomycin (76.8%) was the antimicrobial that presented the higher frequency of resistance among E. coli isolates, followed by amoxacillin (48.2%). Resistance to neomycin in calves isolates was in agreement with Ewa et al.55 who reported 76% resistance in Poland dairy farms. The present neomycin resistance level was higher than the report of Rigobelo et al.59 in Brazil (26%). The resistance level of the calves isolates to amoxacillin in this study was higher than the resistance repots of Yimer22 who noted 39.7% resistant isolates from diarrheic calves. Contrarily, higher resistance (100%) of E. coli isolates to amoxacillin was found by Taye et al.60 in Haromaya and Ewa et al.55 in Netherland dairy farms.
Resistance to sulfonamide (39.3%) in calves isolates, was one of the most common resistance profiles identified among the current isolates. A report in USA indicated that sulfonamides (93.1%) was resisted by E. coli isolates and the resistance genes were commonly associated with mobile genetic elements61. That report also documented that sulfonamides resistant E. coli isolates were also co-transferred to tetracycline and streptomycin.
Moderate rate of resistance to oxytetracycline (26.8%) in calves isolates were obtained in this study. The finding was closer to the 33.3% report of Taye et al.60 in Haromaya of the same isolates. Although 100% sensitivity of tetracycline was reported by Hossain et al.25 in Bangaladish, the resistance of the isolates to tetracycline was found higher elsewhere as Yimer22 found 74% in North Shewa, 61.4% in Bangladish by Islam et al.29 and 100% resistance in Indian report of Malik et al.12 from diarrheic calves.
Escherichia coli isolated from calves also showed moderate 8.9% resistance level to streptomycin. In contrast, Yimer22 found that the resistance of streptomycin to E. coli isolates was 74% in North Shewa and 29.7% resistance was recorded by Tadesse et al.61 in USA calves isolates. The variation of the resistance level could be due to methods of susceptibility used with different break points and frequency of use of the drug in the study areas. Although tetracycline and streptomycin had moderate resistance in this study, they are routine chemoprophylaxis used among livestock in Ethiopia. They are readily available in different dosage forms and in combination with other antibiotics and vitamins. The resistance of E. coli isolates to the relatively cheaper and commonly available antimicrobials is disturbing as the resistance causes more expensive therapies and longer duration of sickness62.
This study showed the presence of multidrug resistant E. coli in diarrheic calves. A considerably higher proportion of the isolates 38 (68%) out of 56 were resistant to two or more of the antimicrobials. Twenty three multi drug resistance profiles were observed. Multi drug resistance was considered when an isolate is resistant simultaneously to two or more drugs63. The number of isolates resistant to two drugs was higher followed by four drugs resistant isolates. In general, as the number of drugs got higher the number of resistant isolates decreased that indicates combined use of antimicrobials may be useful for effective treatment. Different multidrug resistance profile for which E. coli isolates were resistant in this study were reported earlier from Ethiopia22,64, in other parts of African58,65 and European countries38,42 from different food animals, food products and humans. The increasing development of multidrug resistant bacteria is signaling a serious alarm from treatment point of view or the possible transfer of resistance genes to other related pathogens66.
In the present study, isolates were also assessed for the presence of resistance among the virulent genes. The highest resistance in isolates from calves was recorded for neomycin 25 (83.3%) followed by amoxicillin 16 (53.3%). Isolates possessing the virulence factors eaeA gene 9(81.8%), stx1 gene 4 (66.6%) and stx2 gene 12 (92.3%) encoded isolates showed highest resistant for neomycine. Resistance to norfloxacillin 1 (3.3%) was the least in isolates carrying all the three virulence genes; while chloramphenicol, ciprofloxacillin and gentamycin resistance was not shown in calves isolates possessing all the three virulent genes.
Neomycin resistance of the strains of E. coli virulence genes in this study approached to the 100% neomycine resistance E. coli finding of Anshu et al.67 in Indian isolated from animal and human hosts. Contrarily, this resistance finding is higher than the 39% neomycin resistant stx encoded E. coli strains isolated from cattle and human in Germany68. The variation could be due to the method of sensitivity test used and the frequency of the drugs used in the areas as well as difference in involved molecular mechanisms and transfer of antibiotic resistance genes among isolates from different localities69.
In general, the present study indicated that resistance of stx2 positive E. coli predominated over the resistance profile of stx1 and eaeA positive E. coli from the diarrheic calves isolates as supported by previous report70. High frequency of antimicrobial resistance among pathogenic E. coli strains isolated from calves was observed. This could indicate drug resistance E. coli isolates from farm animals as potential reservoirs for resistance genes in human as supported by Call et al.71. Antimicrobial resistance profile of non specified E. coli isolates which were not encoded with the virulence factor genes involved were also considered and considerable resistance isolates were found. Commensally existing E. coli could be a potential reservoir for resistance genes in farm animals as the resistance genes could be transferred between bacteria, environments and food products72. Resistance development also related to exchange of resistance factors between related bacteria that could disseminate multiple antimicrobial resistance genes in E. coli isolates73. Therefore, identifying these commensally reservoirs and mechanisms of persistence could be a key to reducing the load of resistant pathogenic strains.
Conclusion and recommendations
The study was the first conducted to determine pathogenic E. coli strains and their antibiogram, as well as associated risk factors from diarrheic calves in Jimma town. The isolation rate of E. coli from diarrheic calves was found to be high and significant proportion of pathogenic E. coli strains were identified. Calf and managemental factors were found to be independent predictors for occurrence of E. coli associated diarrhea in calves. Higher rate of stx2 positive E. coli strains were detected than stx1 and eaeA genes. Considerable rate of mono and multidrug resistance to commonly prescribed antimicrobials was observed in calves isolates. The overall high isolation rate of E. coli from calves indicates that the infection is widely distributed in the area. Calf diarrhea can cause economic losses in livestock production in the area. Diarrheic calves could be also potential reservoirs of pathogenic strains and resistant genes carrying E. coli strains to humans. This study has limitations as all the virulence genes and serotypes were not described because of time and resource limitation. As a recommendation, attention should be paid on proper dairy farm management practices and care of the newborns to protect calf health. eaeA of EPEC and STEC of EHEC pathotypes are prevalent in diarrheic calves and could be considered in designing control and preventive measures. Proper antibiotic prescription in veterinary and human practices and continuous monitoring of the resistance patterns in bacterial pathogens, in general, and in E. coli, in particular, is mandatory to guide appropriate antimicrobial therapy. Further studies are needed to describe all the virulence genes and serotypes of pathogenic E. coli strains in calves that favor the emergence of drug resistant isolates and developing preventive measure.
Methods
Description of the study area
The study was conducted between November, 2016 and April, 2017 on dairy farms found in Jimma town, Oromia Regional State, Ethiopia. Jimma town covers 19, 305.5 km2, which is the capital of Jimma zone and is 352 km Southwest of Addis Ababa, capital city of Ethiopia. The zone bordered in Northwest by Illubabor, in East by Shewa Zone, in West by Wellega, and in South by Southern Nations and Nationalities People's Regional State. In general, the zone lies at 7° 40′ 43″ N latitude and of 36° 50′ 18″ E longitude. The elevation of the town is 1704 m above sea level while in the zone the altitude varies from 1000 to 3360 m above sea level with maximum and minimum temperatures in range of 25–30 °C and 7–12 °C, respectively. The area has chromic nitosol, combisol and fluvisol soil types74 having sub-humid tropical climate with average annual rainfall ranging from 1200 to 2800 mm. Approximately, 70% of the total annual rainfall is received during the main rainy season, which lasts from June to September75.
According to the 2007 Population and Housing Census of Ethiopia, the total population of the Jimma zone was 2,642,114, from these Jimma town populations accounts 177,900, with 49.7% and 49.3% females and males, respectively76 Among this, 2,204,225 (88.66%) is the rural population which directly depends on agricultural activities for domestic use and exchange of commodities with the urban residents. The predominant economic activities involve mixed farming, which broadly includes cultivation of cereal crops, cash crops including primarily coffee and production of livestock. According to the Central Statistical Agency Agricultural Sample Survey 2011 of Ethiopia, Jimma zone has an estimated 2,317,678 heads of cattle, 824,485 sheep, 310,642 goats, 97,716 horses, 72,667 donkeys, 23,638 mules, 1,804,739 poultry and 479,703 beehives population77. The present study was conducted on dairy farms found in Jimma town. The map of the town is shown in Fig. 2.
Map of the study area. (Generated by Destaw A. Ali using QGIS 2.18 software. https://qgis.org/en/site/forusers/visualchangelog218/index.html.
Study subjects
Animals that included in this study were local and cross breeds of dairy calves of both sexes up to 4 months of age that were clinically affected with diarrhea and exhibited signs of systemic disease (poor appetite, fever, sunken eye, dehydration, reduced suckle reflex, and defecate pasty watery feces). In the study area there are few relatively large dairy farms and many market oriented smallholder dairy farms. During the study, 54 out of the total 74 dairy farms, 3 institutional and 71 composed of large and smallholder dairy farms registered at Jimma town Bureau of Urban Agriculture Development were included. The majority of market oriented small scale dairy farms were organized under dairy cooperatives in their respective localities and the farms kept local and crosses of Holstein breed of calves. Ages of diarrheic calves were categorized into three groups: 1–2 weeks, 3–8 weeks and 9–16 weeks of age based on post-natal silent stress response coupled with lack of immunocompetence, pre-weaning and post weaning strategies in which calves are often susceptible to enteric disease 78,79.
Inclusion and exclusion criteria
Diarrheic calves aged less than or equal to 4 months at dairy farms in Jimma town and owners willing to provide sample from their claves were included as the population of this study. Whereas, calves aged above 4 months, that were on antibiotic therapy for 2 weeks and those whose owners did not agree to allow samples taken were excluded from this study.
Study design and sampling methodology
Study type, type of sampling and source of samples
Cross sectional study type was conducted in dairy farms. Selection of farms were done purposively based on the availability of clinical case (diarrheic calves) in the farms and based on willingness of the owners of the calves. The health status of each calf was evaluated by clinical examination. Calves free from diarrhea were classified as healthy whereas sick calves that show abnormal stool consistency and/or signs of dehydration, sunken eye, diarrhea and weakness were classified as diarrheic. Description of fecal amount, type, consistency, color, smell and mixtures (presence of blood or particles of undigested food, blood clots or pieces of intestinal tissue) were recorded. In addition, farm management practices were assessed. The pre-tested and structured questionnaire surveys were distributed and collected on owners during the time of sample collection in the study period to assess relevant information of the farm management system. The questionnaires were developed in accordance with the objectives of the study and designed in a simple manner to get accurate information from the dairy farm owners.
Sample size determination
Non-probability purposive sampling was used for the selection of farms as well for calf sample. The sample size was determined based on availability of clinical case (diarrheic calves) and on willingness of the owners in the farms. Based on that 112 diarrheic calves were included in the study.
Sample collection procedure
Fecal samples were collected directly from rectum of non treated diarrheic calves preferably soon after onset of diarrhea. The samples were collected from all diarrheic calves aged from newborn to 4 months of age present on the farm at the time of the visit and on emergency calls from the farm owners. Sufficient amount (25–50 g) of fecal samples were collected directly from the rectum using gloved hands and transferred to 50 ml sterile wide mouth screw caped universal bottles. Sterile swabs were used to scratch inside the rectum of the calves whenever there were insufficient amount of feces is obtained from diarrheic calves. The bottles were clearly labeled with information on date of sampling, age, sex and breed of the calves. The samples were transported under cold conditions in ice box to Microbiology Laboratory of School of Veterinary Medicine, College of Agriculture and Veterinary Medicine of Jimma University.
Study methodology
Cultural procedures for isolation of Escherichia coli
Isolation and identification of E. coli were conducted following standard procedures described in Quinn et al.80 and the technique recommended by the International Organization for Standardization ISO-1665481. Upon arrival at the laboratory, immediately or after overnight storage in refrigerator at 4 °C and thawing at room temperature, the samples were manually homogenized by using vortex mixer for approximately 30 s. Twenty five gram of fecal sample was stirred in to 225 ml of sterile buffered peptone water (Himedia, India), or at 1:9 ratio whenever there is little amount of sample present, in a sterile flask. The pre-enriched samples were homogenized for two minutes in the flask and were incubated aerobically at 37 °C for 24 h. All the media used for the study were prepared following the instructions of the manufacturers.
Pre-enriched broth of 0.1 ml (a loop full) sample dilution was inoculated aseptically onto sterile MacConkey agar (Himedia, India) and incubated at 37 °C overnight. From each plate isolates of lactose fermenting colonies were inoculated on Eosin Methylene Blue (EMB) agar medium (Himedia, India). Preliminary characterization and colonies showing characteristic metallic sheen on EMB agar were then picked up and considered as presumptive E. coli. The isolated characteristic colonies of E. coli were stored in nutrient broth for further identification by biochemical tests and other studies. All the isolates were stained by Gram stain to determine the cell morphology and purity of the isolates82.
Biochemical characterization for identification of Escherichia coli
Escherichia coli isolates were identified preliminarily by using indole, methyl red, Voges Proskauer and citrate utilization (IMViC) biochemical tests. In these tests, indole production from tryptophan (indole test), production of strong acid causing red color in methyl red indicator (methyl red test), production of acetoine (Voges Proskauer test) and use of citrate as the only carbon source (citrate test) were conducted. The isolates which exhibited IMViC pattern (++−−) were presumed as E. coli isolates. Then after, the presumed isolates that kept cold in ice packed box were transported to Institute of Biotechnology, Addis Ababa University for PCR based detection of the possible pathogenic E. coli pathotypes and to observe their antimicrobial resistance profile.
Polymerase chain reaction
DNA extraction
Escherichia coli isolates were grown in nutrient broth at 37 °C overnight. exactly 1.5 ml of the culture was pipetted and spun by centrifugation at 13,000 rpm for 10 min in autoclaved eppendorf tube. The bacterial pellet was lysed by boiling in 50 µl of nucleus free water in a water bath at 95 °C for ten minutes. The lysate was centrifuged again as before and an aliquot of supernatant was transferred to another autoclaved eppendorf tube and then 3 µl of the extracted DNA was used directly as template for PCR amplification83.
After extraction of the target DNA, E. coli isolates were subjected to PCR for the presence of virulent genes. According to the component optimization of the compatible enzyme used, three types of PCR assays were performed.
The first two PCR assay were carried out independently to detect the presence of eaeA and stx1 genes in a 22 µl master mix reaction volume. The mix contained 12 µl of nucleus free water, 1 µl of 0.5 µmol of each primer ( EAEF, EAER and EVSF, EVCR), 2.5 µl of PCR buffer with 2 µl of 1.5 mmol MgCl2, 2 µl of solution S, 1 µl of 0.35 mmol of dNTPs (dATP, dCTP, dGTP, dTTP), 0.5 µl of 1U Taq polymerase enzyme (Solis Biodine), and 3 µl of template DNA.
The third PCR assay was performed similarly in a 22 µl master mix reaction volume to detect stx2 gene with a different source of Taq polymerase enzyme, the PCR buffer and MgCl2 used (Himedia, India). The reaction volume contained 14 µl of nucleus free water, 1 µl of 0.5 µmol of each primer (EVTF, EVTR), 2.5 µl of PCR buffer with 2 µl of 1.5 mmol MgCl2, 1 µl of 0.35 mmol of each dNTPs (dATP, dCTP, dGTP, dTTP), 0.5 µl of 1U Taq polymerase enzyme (Himedia, India), and 3 µl of template DNA.
The reaction mixtures of both assays were amplified with 35 cycles, each consisting of 3 min initial denaturation at 95 °C, 60 s denaturation at 95 °C, 60 s annealinig at 55 °C and 60 s elongation at 72 °C in thermal cycler (TC-412; Version 34.11)84. For all the PCR reactions, additional extension step of 10 min at 72 °C were performed. Negative control (PCR grade water in place of the template) and known pooled positive E. coli genes as positive control for each primer involved were also placed along with the samples.
Detection of PCR products / Agarose gel electrophoresis
Amplified PCR products (expected 110-450 bp) were analyzed by gel electrophoresis at 120 V for 45 min in 2% agarose (Conda, cat.8010.11) made in 1 × tris acetate buffer (EDTA) containing ethidium bromide (0.5 µg ml−1) using a marker DNA ladder of 100 bp85. The products were visualized on ultraviolet illuminator and imaged with gel documentation system (BIO-RAD). Details of primer gene sequences and the different reaction temperatures that were carried out in the PCR assays are indicated in Table 7.
Antimicrobial susceptibility testing
The antimicrobial susceptibility testing of the E. coli isolates were performed using panel of commonly used antimicrobials using Kirby–Bauer disk diffusion test according to the Clinical and Laboratory Standard Institute guideline (CLSI) (M100-S25)88. From each isolate, four to five well isolated colonies recovered and grown on EMB agar were aseptically transferred into test tubes containing 5 ml of nutrient broth. The broth cultures were incubated at 37 °C for 24 h and the turbidity of the broth suspension were adjusted by normal 0.9% saline solution with visual comparison of 0.5 McFarland turbidity standards (Remel, USA). Sterile cotton swab was dipped into the suspension, rotated several times, pressing firmly on the inside wall of the tube above the fluid level to remove excess inoculums and swabbed uniformly over the surface of Muller Hinton agar plate. The plates were held at room temperature for 10 min to allow drying. Then eleven antibiotic discs with known concentration of antimicrobials were placed on the cultured Muller Hinton agar plate of appropriate distance of each disc with flamed forceps, inverted and incubated with agar side up for 16–18 h at 37 °C. Following incubation, the diameters of zone of inhibitions were measured with a ruler to the nearest millimeter. Interpretation of the results depended on categorization of isolates into susceptible, intermediate or resistant according to CLSI guidelines36.
Questionnaire survey
Informed consent was obtained from the owners and the permission was granted by the owners to perform experiment on their calves. Pre-tested structured questionnaire was administered to dairy farm owners or farm managers during the time of sample collection in the study period to assess relevant information on calf husbandry practices and the general farm management system. The questionnaires were developed in accordance with the objectives of the study and designed in a simple manner to get accurate information from the dairy farm owners. The questionnaires included practices in the farm which can have impact on the proper rearing of calves associated with risk factors responsible for calf diarrhea. These include age of calf, farm size, colostrum feeding, general health care, animal housing, hygiene and sanitation of farms, occurrence of calf diarrhea, disease preventive and control measures practiced in the farms.
Data management and statistical analysis
All the data obtained from questionnaires and laboratory describing the conditions of the study suggestive of E. coli infection on calves along with the risk factors were filtered, coded and entered in to Microsoft Excels pread sheet 2007. The collected data were computed by using SPSS version 20.0 software (SPSS INC. Chicago, IL) for appropriate statistical analysis. Descriptive analysis was used to describe the study population in relation to risk factors. The point prevalence was calculated as the number of infected individuals divided by the number of individuals sampled times 100. The associations between occurrence of E. coli isolates and the risk factors, as well the presence of the different virulent genes detected by PCR and diarrheal infection due to positive E. coli were analyzed using person’s χ2 test. Variables with P value < 0.25, for controlling the possible effect of confounders, in univariable logistic regression were fitted into multivariable logistic regression model to observe the strength of the association between risk factors and the outcome. The suitability of the model was checked by multicollinearity diagnosis among independent variables by contingency coefficient. The goodness of fit of the model with the data was assessed by Hosmer and Lemeshow test. After selecting the final model of multivariable logistic regression, the beta (β) coefficients of each independent variable were observed to estimate odds ratio (OR) which is used for assessing strength of association. Effects were reported as statistically significant as P value was less than 0.05.
Ethics approval and consent to participate
The incorporated work was ethically cleared from the Institutional Review Board (HIRPG/248/07) of Jimma University Institute of Health Sciences. All methods were carried out in accordance with relevant guidelines and regulations, on involving humans and animals in the study. Informed consent was obtained from the farm owners and the permission was granted by the owners to perform experiment on their calves. No fees were requested.
Data availability
The data sets used during the current study are available from the corresponding author on reasonable request.
Change history
14 September 2021
This article has been retracted. Please see the Retraction Notice for more detail: https://doi.org/10.1038/s41598-021-98353-6
Abbreviations
- AMGPT:
-
Amount of milk given per time
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- CF:
-
Calving facilities
- CLSI:
-
Clinical Laboratory and Standard Institute
- COR:
-
Crude odds ratio
- CSA:
-
Central Statistical Agency
- CSAASS:
-
Central Statistical Agency Agricultural Sample Survey
- DACA:
-
Drug Administration and Control Authority
- dNTP:
-
Deoxyribo nucleotide triphosphate
- EIAR:
-
Ethiopian Institute of Agricultural Research
- EVT:
-
EnteroVero toxin
- FCFT:
-
First colostrum feeding time
- IgG:
-
Immunoglobulin G
- ISO:
-
International Organizations for Standardization
- OIE:
-
Office International des Epizooties
- OPEDJZ:
-
Office of Planning and Economic Development for Jimma Zone
- P :
-
Probability
- PCR:
-
Polymerase chain reaction
- SPSS:
-
Software Package for Social Science
- USDA:
-
United State Department of Agriculture
- χ2 :
-
Chi-square
References
Sissay, M., Uggla, A. & Waller, P. Prevalence and seasonal incidence of larvaland adult cestode infections of sheep and goats in Eastern Ethiopia. Trop. Anim. Health Prod.40, 387–394 (2008).
USDA Dairy. Part II. Changes in the U.S. dairy cattle industry, 1991–2007. USDA-APHIS-VS, CEAH, Fort Collins 57–61 (2007).
Uhde, F. et al. Prevalence of four enteropathogens in the faeces of young diarrheic dairy calves in Switzerland. Vet. Rec.163, 362–366 (2008).
Cho, Y. Ecology of calf diarrhea in cow-calf operations. Iowa State University Graduate theses and dissertation paper 126–142 (2012).
Blanchard, P. Diagnostics of dairy and beef cattle diarrhea. Vet. Clin. N. Am. Food Anim. Pract.28, 443–464 (2012).
LeJeune, T., Hancock, D., Wasteson, Y., Skjerve, E. & Urdahl, A. Comparison of E. coli O157 and Shiga toxin-encoding genes (stx) prevalence between Ohio, USA and Norwegian dairy cattle. Int. J. Food Microbiol.109, 19–24 (2006).
Smith, G. Treatment of calf diarrhea: Oral fluid therapy. Vet. Clin. N. Am. Food Anim. Pract.25, 55–72 (2009).
Izzo, M. et al. Prevalence of major enteric pathogens in Australian dairy calves with diarrhea. Aust. Vet. J.89, 167–173 (2012).
Kumar, A., Taneja, N., Singhi, S. & Sharma, R. Haemolytic uraemic syndrome in India due to Shiga toxigenic Escherichia coli. J. Med. Microbiol.62, 157–160 (2012).
Cho, Y. & Yoon, K. An overview of calf diarrhea-infectious etiology, diagnosis, and intervention. J. Vet. Sci.15, 1–17 (2014).
Boschi-Pinto, C., Velebit, L. & Shibuya, K. Estimating child mortality due to diarrhoea in developing countries. Bull. WHO86, 710–717 (2008).
Malik, S. et al. Haematological profile and blood chemistry in diarrhoeic calves affected with colibacillosis. J. Anim. Health Prod.1, 10–14 (2011).
Lorenz, I., Fagan, J. & More, S. Calf health from birth to weaning. Ii. Management of diarrhoea in pre-weaned calves. Ir. Vet. J.64, 9 (2011).
Guardabassi, L. & Courvalin, P. Modes of antimicrobial action and mechanisms of bacterial resistance: Chapter 1. In Antimicrobial Resistance in Bacteria of Animal Origin (ed. Aarestrup, F.) 1–18 (ASM Press, 2006).
Claeys, W. et al. Raw or heated cow milk consumption: review of risks and benefits. Food Control31, 251–262 (2013).
Shibata, S. et al. Complete genome sequence of a novel GV.2 sapovirus strain, NGY-1, detected from a suspected food borne gastroenteritis outbreak. Genome Announc.3, 1 (2015).
Bas, B., Oude, M. & van der Lia, H. Viruses causing gastroenteritis: The known, the new and those beyond. Viruses8, 42 (2016).
Wudu, T., Kelay, B., Mekonnen, H. & Tesfu, K. Calf morbidity and mortality in smallholder dairy farms in Ada’a Liben district of Oromia, Ethiopia. Trop. Anim. Health Prod.40, 369–376 (2008).
Bekele, M. et al. Prevalence and incidence rates of calf morbidity and mortality and associated risk factors in smallholder dairy farms in Hawassa, Ethiopia. Ethiop. Vet. J.13, 59–68 (2009).
Gebregiorgis, A. & Tessema, S. Characterization of Escherichia coli isolated from calf diarrhea in and around Kombolcha, South Wollo, Amhara Region, Ethiopia. Trop. Anim. Health Prod.48, 273–281 (2016).
Yakob, B. A Study On Major Enteropathogens of Calf Diarrhoea in Dairy Farms of Assela and Its Surroundings Arsi Zone Oromya Region, M.Sc. Thesis (Addis Ababa University, 2014).
Yimer, M. Major Enteropathogenes Associated in Calf Diarrhea, With an Emphasis on E. coli and Salmonella Species in Dairy Farms of Muke Turi, Debre Stige and Fitche Towns North Shewa, Ethiopia. M.Sc. thesis 135 (Addis Ababa University, 2014).
DACA. Antimcirobials Use, Resistance and Containment Baseline Survey Syntheses of Findings. Drug Administration and Control Authority of Ethiopia in collaboration with Management Sciences for Health, Strengthening Pharmaceutical Systems (MSH/SPS) August 2009, Addis Ababa.
Ghada, A., Amr, M. & Ahmed, A. Prevalence of enteropathogens associated with neonatal calf scour in cattle and buffalo calves using (Fastest® Strips) rapid field test. Assiut Vet. Med.59, 813 (2013).
Hossain, M., Rahma, M., Nahar, A., Khair, A. & Alam, M. Isolation and identification of diarrheagenic Escherichia Coli causing colibacillosis in calf in selective areas of Bangladesh. Bangl. J. Vet. Med.11, 145–149 (2013).
Dawit, M. Isolation and Identification of Enterotoxigenic Escherichia Coli strengthen from Diarrheic Calf faeces in Addiss Ababa and Debre Zeit, Ethiopia (unpublished M.Sc thesis, Addis Ababa University, 2012).
Sunday, C., Olalekan, T., Afusat, J. & Olaoluwa, O. Calf diarrhea: Epidemiological prevalence and bacterial load in Oyo and Ogun States, Nigeria. Alex. J. Vet. Sci.1, 90–96 (2016).
Abdisa, B. & Minda, A. Major calf health problems and exposing risk factors at Holeta Agriculture Research Center Dairy Farm, Holeta, Ethiopia. Glob. Vet.17, 05–14 (2016).
Islam, A., Rahman, M., Nahar, A., Khair, A. & Alam, M. Investigation of pathogenic Escherichia coli from diarrheic calves in selective area of Bangladesh. Bangl. J. Vet. Med.13, 45–51 (2015).
Radostits, O.M., Gay, C.C., Hichcliff, K.W. & Constable, P.D. Veterinary Medicine. A Textbook of the Diseases of Cattle, Sheep, Pigs, Goats and Horses. 10th ed. 673–762 (Elsevier, 2007).
Villarroel, A. Scours in Beef Calves, Causes and treatments, 2009 (Retrieved on May 2013). http://whatcom.wsu.edu/ag/documents/beef/ScoursBeefCalves_OSUem8977-e.pdf). Accessed on 20 Sept 2016.
Klein, D., Tim, A., Franz, S., Michael, I. & Marc, D. Results of an online questionnaire to survey calf management practices on dairy cattle breeding farms in Austria and to estimate differences in disease incidences depending on farm structure and management practices. Acta Vet Scand.57, 44 (2015).
Matte, J., Girard, G., Seosne, J. & Brisson, G. Absorption of colostral immunoglobulin G in new born dairy calf. J. Dairy Sci.65, 1765–1770 (1982).
Donna, M., Amaral, P., Patty, B., John, T. & Sharon, F. Feeding and Managing Baby Calves from Birth to 3 Months of Age (Director of Cooperative Extension Service, University of Kentucky College of Agriculture, 2006).
Khan, M., Weary, D. & von Keyserlingk, M. Invited review. Effects of milk ration on solid feed intake, weaning and performance in dairy heifers. J. Dairy Sci.94, 1071–1081 (2011).
Walter, G. Intestinal Diseases in Ruminants Diarrhea in Neonatal Ruminants (Scours): The Merck Veterinary Manual (Merck Sharp & Dohme Corp, a subsidiary of Merck & Co. Inc., Kenilworth, 2014).
Hur, J., Jawale, C. & Lee, J. A review: Antimicrobial resistance of Salmonella isolated from food animals. Food Res. Int.45, 819–830 (2013).
Andrade, G. et al. Heinemann: Identification of virulence factors by multiplex PCR in Escherichia coli isolated from calves in Minas Gerais, Brazil. Trop. Anim. Health Prod.4, 1783–1790 (2012).
Tan Duc, N. & Thin, T. Hung Vu-K: Virulence factors in Escherichia coli isolated from calves with diarrhea in Vietnam. J. Vet. Sci.12, 159–164 (2011).
Dastmalchi, H. & Ayremlou, N. Characterization of Shiga toxin-producing E coli (STEC) in feces of healthy and diarrheic calves in Urmia region, Iran. Iran. J. Microbiol.4, 63–69 (2012).
Yousif, A. & Hussein, M. Prevalence and molecular detection of intimin (eaeA) virulence gene in E. coli O157:H7 in calves. Res. J. Vet. Pract.3, 47–52 (2015).
Tahamtan, Y., Hayati, M. & Namavari, M. Prevalence and distribution of the stx1, stx2 genes in STEC isolates from cattle. Iran. J. Microbiol.2, 8–13 (2010).
Askari, M., Zahraei, T., Rabbani, M., Tadjbakhsh, H. & Nikbakht, G. Occurrence and characterisation of EHEC isolates from diarrhoeic calves. Comp. Clin. Pathol.9, 201–205 (2009).
Yahya, K., Esra, S., Cevdet, U., Baris, S. & Selahattin, K. Virulence genes of Shiga toxin-producing E. coli O157:H7 strains isolated from calves and cattle. Ankara Üniv. Vet. Fak. Derg.58, 255–260 (2011).
Orden, J. et al. Verotoxin-producing Escherichia coli (VTEC) and eae- positive non-VTEC in 1–30-days-old diarrhoeic dairy calves. Vet. Microbiol.63, 239 (1998).
Srivani, M., Narasimha Reddy, Y., Subramanyam, K., Ramakoti, V. & Srinivasa, T. Prevalence and antimicrobial resistance pattern of Shiga toxigenic Escherichia coli in diarrheic buffalo calves. Vet. World10, 774–778 (2017).
Shaw, D. et al. Shedding patterns of verocytotoxin-producing Escherichia coli strains in a cohort of calves and their dams on a Scottish beef farm. Appl. Environ. Microbiol.70, 7456–7765 (2004).
Fernández, D., Rodríguez, E. M., Arroyo, G. H., Padola, N. L. & Parma, A. E. Seasonal variation of Shiga toxin-encoding genes (stx) and detection of E. coli O157 in dairy cattle from Argentina. J. Appl. Microbiol.106, 1260–1267 (2009).
Katani, R. et al. Complete genomesequence of SS52, a strain of E. coli O157:H7recovered from super shedder cattle. Gen. Announc.3, 19 (2015).
Alikhani, M., Mirsalehian, A., Fatollahzadeh, B., Pourshafie, M. & Aslani, M. Prevalence of enteropathogenic and shiga toxin-producing E. coli among children with and without diarrhea in Iran. J. Popul. Nutr.25, 88–93 (2007).
Pejman, A., Mohammad, K., Jalal, M., Sadegh, G. & Mohammad, A. Characterization of STEC and enteropathogenic E. coli (EPEC) using multiplex Real-Time PCR assays for stx1, stx2 and eaeA. Iran. J. Microbiol.6, 169–174 (2014).
Lucia, R., Glen, E., Kari, G. & Narelle, F. Detection and typing strategies for pathogenic E. coli: Introduction to pathogenic E. coli. Springer Briefs in Food, Health, and Nutrition 1–38 (University of Wisconsin, Madison, USA, 2015).
Ochoa, T. & Contreras, C. EPEC infection in children. Curr. Opin. Infect. Dis.24, 478–483 (2011).
European Medicines Agency. European Surveillance of Veterinary Antimicrobial Consumption: ‘Sales of veterinary antimicrobial agents in 26 EU/EEA countries in 2013’ (EMA/387934/2015) (2015).
Ewa, B., Justyna, M., Michał, S., Magdalena, W. & Katarzyna, B. Prevalence of virulence determinants and antimicrobial resistance among commensal Escherichia coli derived from dairy and beef cattle. Int. J. Environ. Res. Public Health12, 970–985 (2015).
Begum, F. et al. Molecular identification and antibiogram profiles of E. coli isolated from apparently healthy and diarrheic goats. Bangl. J. Vet. Med.14, 203–208 (2016).
Mark, G. & Joseph, T. Maing the Best First Choice Antibiotic Selections. Animal Pharmacology: The North American Veterinary Conference—2005. Proceedings. www.ivis.org. Accessed on 25 Aug 2017.
Shah, M. et al. Prevalence, seasonal variation, and antibiotic resistance pattern of enteric bacterial pathogens among hospitalized diarrheic children in suburban regions of central Kenya. Trop. Med. Health44, 39 (2016).
Rigobelo, E. et al. Virulence factors of Escherichia coli isolated from diarrheic calves. Arq. Bras. Med. Vet. Zootec.58, 305–310 (2006).
Taye, M., Berhanu, T., Berhanu, Y., Tamiru, F. & Terefe, D. Study on carcass contaminating E. coli in apparently healthy slaughtered cattle in Haramaya University slaughter house with special emphasis on Escherichia coli O157:H7, Ethiopia. J. Vet. Sci. Technol.4, 132 (2013).
Tadesse, D. et al. Antimicrobial drug resistance in Escherichia coli from humans and food animals, United States, 1950–2002. Emerg. Infect. Dis.18, 742–749 (2012).
OIE. Antimicrobial Resistance and the Prudent Use of Antimicrobials. The OIE Strategy; 2016. www.oie.int/antimicrobial-resistance. Accessed on: 24 May 2017.
Tavares, W. Manual of Antibiotics and Chemotherapeutics of Infections, 3rd ed, edited by Atheneu. Sao Paulo (2001).
Ayrikim, A., Mulugeta, K., Bayeh, A., Endalkachew, N. & Melaku, A. Antibiogram of E. coli serotypes isolated from children aged under five with acute diarrhea in Bahir Dar town. Afr. Health Sci.15, 2 (2015).
Osman, K., Mustafa, A., Elhariri, M. & El-Hamed, G. The distribution of Escherichia coli serovars, virulence genes, gene association and combinations and virulence genes encoding serotypes in pathogenic E. coli recovered from diarrhoeic calves, sheep and goat. Trans. Bound. Emerg. Dis.60, 69–78 (2013).
Osaili, T., Alaboudi, A. & Rahahla, M. Prevalence and antimicrobial susceptibility of E. coli O157:H7 on beef cattle slaughtered in Amman abattoir. Meat Sci.93, 463–468 (2013).
Anshu, P., Namita, J., Joshi, R., Rajeev, P. & Ankita, S. Virulence attributes and antibiotic resistance pattern of E. coli isolated from human and animals. Asian J. Anim. Vet. Adv.11, 67–72 (2016).
Guerra, B., Junker, E. & Schroeter, A. Phenotypic and genotypic characterization of antimicrobial resistance in E. coli O111 isolates. J. Antimicrob. Chemother.57, 1210–1214 (2006).
Jose, M. & Cesar, A. Mechanisms of antibiotic resistance. Microbiol Spectr.4, 10 (2006).
Colello, R. et al. Antibiotic resistance and integrons in Shiga toxin-producing Escherichia coli (STEC). Braz. J Microbiol.46, 1–5 (2015).
Call, D., Davis, M. & Sawant, A. Antimicrobial resistance in beef and dairy cattle production. Anim. Health Res.9, 159–167 (2008).
O’Brien, T. Emergence, spread, and environmental effect of antimicrobial resistance: How use of an antimicrobial anywhere can increase resistance to any antimicrobial anywhere else. Clin. Infect Dis.34, 78–84 (2002).
Kozak, G. et al. Distribution of sulfonamide resistance genes in E. coli and Salmonella isolates from swine and chickens at abattoirs in Ontario and Québec Canada. Appl. Environ Microbiol.75, 5999–6001 (2009).
Ethiopian Institute of Agricultural Research (EIAR). Soil type and coverage. Jimma Agricultural Research Center. http://www.eiar.gov.et/index.php/jimma-agricultural-research-center. Accessed on: 28 Aug 2017.
OPEDJZ. International Livestock Center for Africa (ILCA), Addis Ababa, Ethiopia Statistical Abstract. Jimma, Oromia, Ethiopia (2002).
CSA. Summary and statistical report of the 2007 population and housing census results. Addis Ababa: EFDRE, Population census commission 25–27. CSA 2008.
CSAASS. Agricultural Sample Survey 2014/15 [2007 E.C.]. Vol.II Report on Livestock And Livestock Characteristics (Private Peasant Holdings) Statistical Bulletin 505. VII, Addis Ababa, Ethiopia (2011).
Morel, F. et al. Pre-weaning modulation of intestinal microbiota by oligosaccharides or amoxicillin can contribute to programming of adult microbiota in rats. Nutrition31, 515–522 (2015).
Lindsey, E. & Sonia, J. Stress, immunity, and the management of calves. J. Dairy Sci.99, 3199–3216 (2016).
Quinn, P., Markey, B., Carter, M., Donnelly, W. & Leonard, F. Veterinary Microbiology and Bacterial Disease 1–648 (Black Well Science, 2002).
International Organization for Standardization. ISO 16654:2001 Microbiology of Food and Animal Feeding Stuffs- Horizontal Method for the Detection of Escherichia coli O157 1st ed. Int Orga Standa, Geneva, Switzerland, 2011.
Sagar, A. Bacterial Identification: Biochemical Test and Identification of E. coli. Online Microbiology Notes 2015.https://microbiologyinfo.com/biochemical-test-and-identification-of-e-coli/. Accessed on 15 Jan 2017.
He, F. Escherichia coli genomic DNA extraction. Bio-protocol Bio 101: e97. https://doi.org/10.21769/BioProtoc.97 (2011). www.bio-protocol.org/e97.
Labnet. Labnet International, Inc, 31 Mayfield Ave., Edison, NJ 08837 USA (2002).
HiMedia. HiMedia Products Catalogue 2012–2013. Laboratories Pvt. Limited, India (2012).
Khan, A., Das S., Ramamurthy, T., Sikdar, A., Khanam, J., Yamasaki, S., Takeda, Y. & Nair, G. Antibiotic resistance, virulence gene, and molecular profiles of Shiga toxin-producing E. coli isolates from diverse sources in Calcutta, India. J. Clin. Micro.40, 2009–2015 (2002).
Pal, A., Ghosh, S., Ramamurthy, T., Yamasaki, S., Tsukamoto, T., Bhattachary, S., Takeda, Y. & Nair, G. Shiga-toxin producing E. coli from healthy cattle in a semi-urban community in Calcutta, India. Indian J. Med. Res.110, 83–85 (1999).
CLSI. Performance Standards for Antimicrobial Susceptibility Testing. Twenty-Fifth Informational Supplement. Approved standard CLSI document M100-S25, 950 West ValleyRoad, Suite 2500, Wayne, Pennsylvania 19087 USA., vol. 35, no. 3 (2015).
Acknowledgements
The work incorporated in this research was undertaken using the research grant allocated by Ethiopian Institute of Agriculture Research, Jimma University College of Agriculture and Veterinary Medicine and Institute of Biotechnology, Addis Ababa University (AAU). Specifically the AAU TR project entitled “Biotechnological Approaches to Harness Microbe-Host-Environment interactions for Sustainable Development of Health and Agricultural Productivity; Ref. No. VPRTT/LT-030/08/15”. We very grateful to the Institution and the Universities. All participants of the study such as farm owners, technical assistances and grant sources are duly acknowledged.
Author information
Authors and Affiliations
Contributions
D.A.A. was prior responsible for collecting the samples, processing all the laboratory works and writing up the paper work and shaping of this manuscript to be submitted. Y.D.B was closely monitoring and guiding the work in addition to shaping the paper and managing part of the afforded costs. T.S.T. was chief responsible for guiding the entire work, managing all the resources and shaping of this manuscript to be submitted.
Corresponding author
Ethics declarations
Competing of interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been retracted. Please see the retraction notice for more detail:https://doi.org/10.1038/s41598-021-98353-6
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ali, D.A., Tesema, T.S. & Belachew, Y.D. RETRACTED ARTICLE: Molecular detection of pathogenic Escherichia coli strains and their antibiogram associated with risk factors from diarrheic calves in Jimma Ethiopia. Sci Rep 11, 14356 (2021). https://doi.org/10.1038/s41598-021-93688-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-93688-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.