Abstract
Hand-foot syndrome (HFS), also known as palmar-plantar erythrodysesthesia (PPE), is a major side effect of capecitabine. Although the pathogenesis of HFS remains unknown, some studies suggested a potential involvement of inflammation in its pathogenesis. Proton pump inhibitors (PPIs) have been reported to have anti-inflammatory effects. In this study, we investigated the ameliorative effects of omeprazole, a PPI on capecitabine-related HFS in mice model, and a real-world database. Repeated administration of capecitabine (200 mg/kg, p.o., five times a week for 3 weeks) increased fluid content, redness, and tumor necrosis factor (TNF)-α substance of the mice hind paw. Co-administration of omeprazole (20 mg/kg, p.o., at the same schedule) significantly inhibited these changes induced by capecitabine. Moreover, based on the clinical database analysis of the Food and Drug Administration Adverse Event Reporting System, the group that has used any PPIs had a lower reporting rate of capecitabine-related PPE than the group that has not used any PPIs. (6.25% vs. 8.31%, p < 0.0001, reporting odds ratio (ROR) 0.74, 95% confidence interval (CI) 0.65–0.83). Our results suggest that omeprazole may be a potential prophylactic agent for capecitabine-induced HFS.
Similar content being viewed by others
Introduction
Hand-foot syndrome (HFS), also known as palmar-plantar erythrodysesthesia (PPE), is a major side effect of antineoplastic drugs such as pyrimidine analogs (e.g., capecitabine), kinase inhibitors, and pegylated liposomal doxorubicin1,2,3,4. HFS frequently occurs on the palms and soles of the feet and starts with minor skin changes such as erythema and edema, and then, if severe, proceeds to painful edema, blisters, and fissures. Capecitabine is a prodrug of fluorouracil and is used to treat many cancers, including colorectal, gastric, and breast cancers5,6,7,8. About 50%–68% of patients who take capecitabine develop HFS. Moreover, 11%–24% of these patients have Grade 3 or more severe forms of HFS9,10,11,12. Besides reduced the quality of life, Grade 2 or more HFS requires discontinuation or reduced dose of capecitabine. Although the pathogenesis of HFS remains unknown, some clinical studies suggested celecoxib a cyclooxygenase-2 (COX-2) inhibitor had a preventive effect for capecitabine-induced HFS13,14,15. Moreover, the inflammatory symptoms, such as edema and reddening of the skin, are reported in capecitabine-induced HFS. The evaluation of the available studies strongly suggests the involvement of inflammation in the development of capecitabine-induced HFS16. On the other hand, proton pump inhibitors (PPIs), including omeprazole, are reported to have anti-inflammatory effects in several animal models17,18,19,20,21. We hypothesized that omeprazole, with its anti-inflammatory properties, may be effective in preventing or treating HFS. In this study, we investigated the possibility of the proton pump inhibitor omeprazole as prevention for capecitabine-induced HFS in mice model and the clinical database analysis using the Food and Drug Administration Adverse Event Reporting System (FAERS).
Results
Effect of omeprazole on HFS induced by capecitabine in mice
Pictures of the right hind limb plantar of the mice in each drug treatment group on day 19 are shown in Fig. 1A. Redness, a* in CIE Lab (L*a*b* color space), of the plantar, was significantly increased by the repeated administration of capecitabine (200 mg/kg, p.o.) compared with the vehicle treatment on day 19 (p < 0.05; Fig. 1B). Co-treatment with omeprazole (20 mg/kg, p.o.) significantly reduced the intensity of the redness induced by capecitabine (p < 0.05; Fig. 1B).
Effects of omeprazole on redness and edema of hind limb plantar induced by capecitabine of the mice. Capecitabine (200 mg/kg) was administered orally five times a week for three weeks. Omeprazole (20 mg/kg) was administered orally in the same way. Photographs of the hind limb plantar of the mice in each drug treatment group on day 19 are shown (A). Redness, the intensity of a* in CIE L*a*b* color space, was measured by Image J 1.51 software (B). The fluid contents in the plantar skin were measured to assess the edema (C). Data are expressed as the mean ± standard error of the mean (n = 5–6).*p < 0.05 compared with vehicle; †p < 0.05 compared with capecitabine-alone treatment.
The respective administration of capecitabine significantly increases the fluid content of the foot skin compared with the vehicle treatment on the same day (p < 0.05; Fig. 1C). Co-treatment with omeprazole significantly inhibited the increase in fluid content induced by capecitabine on day 19 (p < 0.05; Fig. 1C).
Omeprazole reduces inflammatory cytokines in the mouse model of HFS
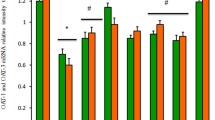
Tumor necrosis factor (TNF)-α content of hind limb plantar tissues were significantly increased in the capecitabine-treated group compared to the vehicle group (p < 0.05; Fig. 2A). The increase in TNF-α content was significantly inhibited in the omeprazole co-treatment group (p < 0.01; Fig. 2A). No significant differences in interleukin (IL)-1β contents were observed between the two groups (Fig. 2B).
Effects of omeprazole on inflammatory cytokines, TNF-α (A) and IL-1β (B) in hind limb plantar of the mice. Capecitabine (200 mg/kg) was administered orally five times a week for three weeks. Omeprazole (20 mg/kg) was administered orally in the same way. TNF-α and IL-1β contents were measured by ELISA. Data are expressed as the mean ± standard error of the mean (n = 8–9). †p < 0.05 compared with vehicle; **p < 0.01 compared with capecitabine-alone treatment.
Effects of PPIs on reporting rates of capecitabine-related PPE in FAERS database
Of the 60,668 capecitabine-associated adverse event reports from FAERS database, 4936 reports (8.14%) were PPE. Reporting odds ratios (RORs) of PPE were 0.77 [95% confidence interval (CI) 0.65–0.92], 0.62 [95% CI 0.49–0.79], and 0.75 [95% CI 0.57–0.99] in patients with omeprazole, pantoprazole, and lansoprazole, each respectively (Fig. 3A). The patients using any PPIs had a significantly lower reporting rate of PPE compared to the patients without any PPIs (6.25% vs. 8.31%, p < 0.0001, ROR: 0.74 [0.65–0.83]; Fig. 3A). In contrast, no significant difference in the reporting rate of PPE was observed between groups with and without any H2 blockers (8.13% vs. 8.14%, p = 0.9901, ROR = 1.00 [0.82–1.21]; Fig. 3B).
Effects of PPIs (A) and H2 blockers (B) on reporting rates of capecitabine-related PPE in the FAERS database. The report data were extracted using CzeekV Pro (version 5.0.23, INTAGE Healthcare Inc., Tokyo, Japan, accessed August 2020). Of the 12,752,146 adverse event reports from the FAERS between 1997 and the first quarter of 2020, we investigated the reporting rates and the RORs of the palmar-plantar erythrodysesthesia as adverse events after capecitabine use.
Discussion
The pathogenesis of capecitabine-induced HFS is still unknown. However, some studies indicate the involvement of inflammation in its pathogenesis13,14,15,16. In the present study, we evaluated the effect of omeprazole, a drug reported to have anti-inflammatory effects in the mouse model of capecitabine-induced HFS. Edema and erythema are the main symptoms of HFS. Therefore, we analyzed fluid content as an indicator of edema and redness as an indicator of erythema in a mouse model. Omeprazole treatment reduced edema and redness in the feet, which suggests omeprazole may exert a skin protective effect against capecitabine.
The same model was used to investigate the mechanism of action of how capecitabine exerts the skin protective effect by measuring the inflammatory cytokines productions from the skin of the feet. Omeprazole inhibited capecitabine-induced increases of the cytokine productions (IL-1β and TNF-α) from the skin. This observation suggests that anti-inflammatory effects may be involved in the protective effect of omeprazole on the skin. Omeprazole and esomeprazole, the S-isomer of omeprazole, have been reported to have anti-inflammatory effects. Moreover, some studies have reported esomeprazole to inhibit TNF-α and IL-1β and other inflammatory molecules such as IL-6, vascular cell adhesion molecule-1, and inducible nitric oxide synthase, which may contribute to the skin protective effect of omeprazole17,20,22,23.
Additionally, we investigated the effect of omeprazole on capecitabine-induced HFS in the clinical setting using the real-world database, FAERS. Besides omeprazole, other PPIs, including pantoprazole and lansoprazole, significantly suppressed the reporting rate of PPE. Moreover, the reporting rate of PPE in the group with any PPIs was also lower than it without any PPIs (6.25% vs. 8.31%, P < 0.0001, ROR = 0.74, 95% confidence interval (CI) 0.65–0.83). In sum, the anti-HFS action may be a class effect common to all PPIs. The effects of PPIs other than omeprazole were not tested in our animal model. Lugini and colleagues have reported that the potency of the action of each PPI depends on the hydrophilicity or lipophilicity of the PPI structures24. Thus, the difference in the potency of the effects on HFS needs to be examined in the future. Meanwhile, despite H2 blockers to have an inhibitory effect on gastric acid secretion like PPIs, the use of any H2 blockers did not have any effects on the reporting rate of PPE. Thus, effects other than the gastric acid suppression may be involved in the ameliorative effect of PPI on capecitabine-related HFS.
The effect of omeprazole on the antitumor effects of capecitabine was not examined in this study. Some reports suggest that omeprazole induces multidrug resistance-associated protein (MRP3), or known as ATP binding cassette subfamily C member (ABCC3) in the liver25. Pantoprazole, a drug in a class PPIs, has reported to suppress the MRP1 (ABCC1) signaling pathway and reduce cell survival in drug-resistant gastric adenocarcinoma cells26. Further studies should be required to determine the effect of omeprazole on the antitumor effects of capecitabine.
There are a series of clinical studies on the use of PPIs in the treatment of cancer patients27,28,29,30,31,32. Some of them are retrospective studies showing that PPIs may increase the efficacy of chemotherapy30 or prevent cancer31,32. Moreover, PPIs have also been reported to enhance the antitumor activity of carbonic anhydrase IX inhibitors and reverse transcriptase inhibitors in basic studies33,34. Furthermore, there is a general agreement on the possibility to repurpose PPIs in cancer treatments35,36,37. On the other hand, several clinical studies have recentry reported that gastric acid secretion inhibitors, including PPIs and H2 blockers, attenuate the effect of capecitabine38,39,40,41. Further information on the efficacy and safety of the combination of capecitabine and PPIs in cancer patients needs to be established. Nevertheless, the present study suggests that co-administration of omeprazole with capecitabine may prevent capecitabine-induced HFS in both animal models and clinical database analysis at least.
Methods
Animals
We used ICR mice (six-week-old, 30–35 g, Japan SLC, Inc., Shizuoka, Japan) for the experiments. Mice were bred in groups of 4–5 per cage, with a 12:12-h light–dark cycle. Animals were fed water and food ad libitum. All animal experiments were approved by the Experimental Animal Care and Use Committee of Kyushu University and conducted according to the guidelines of the National Institutes of Health. And all experiments were carried out in compliance with the ARRIVE guidelines.
Drugs
In the capecitabine-induced HFS model, capecitabine (200 mg/kg, Fluorochem, Ltd., Derbyshire, UK) or a vehicle (5% methylcellulose; MP Biomedicals, CA, USA) was administered orally (p.o.), five times a week for three weeks (days 1–5, 8–12, and 15–19). Omeprazole (20 mg/kg, FUJIFILM Wako Pure Chemical Corporation, Osaka, Japan) was administered orally (p.o.) at the same schedule. Each drug was administered at a volume of 10 mL/kg. The doses of these drugs were determined based on previous reports42,43,44.
Assessment of HFS in mice
The soles of the mouse's feet were photographed to assess the redness of the foot skin. The a*-intensity of the CIE L*a*b* color space of the captured images was measured by Image J 1.51 software (Wayne Rasband, National Institutes of Health, MD, USA). The skin of the hind limb plantar was collected to assess the edema. The fluid contents were calculated by Eq. (1).
In this formula, weight wet refers to sample weight immediately after the collection; weight dry refers to sample weight after drying at 65 °C for 48 h. Each test was conducted on the last day of the experiment (day 19).
Quantification of IL-1β and TNF-α in mice hind limb plantar
On day 19, the hind limb plantar tissue of the mice was collected and homogenized in buffer containing 1 mM phenylmethylsulfonyl fluoride (FUJIFILM Wako Pure Chemical Corporation,), and the content of IL-1β and TNF-α were analyzed using a commercial ELISA kit (Proteintech Group, Inc., IL, USA). The procedure followed the instructions of the kit.
Analysis of FAERS data
To investigate the efficacy of PPIs, including omeprazole, in reducing the incidence of HFS in a clinical setting, we analyzed the incidence of HFS in patients taking capecitabine using the FAERS database. The report data were extracted using CzeekV Pro (version 5.0.23, INTAGE Healthcare Inc., Tokyo, Japan, accessed August 2020). Of the 12,752,146 adverse event reports from the FAERS between 1997 and the first quarter of 2020, we investigated the reporting rates and the RORs of PPE as adverse events after capecitabine use. The RORs and 95% CIs were calculated by the Eqs. (2) and (3), respectively45.
In these formulas, n11 refers to patients who used PPIs or H2 blockers as a reference and reported the PPE; n12 refers to patients who used PPIs or H2 blockers but did not report the PPE; n21 refers to patients who did not use these drugs but reported the PPE, and n22 refers to patients who did not use these drugs and did not report the PPE.
Statistical analysis
The results are expressed as the mean ± standard error of the mean. Statistical analyzes were performed using a one-way analysis of variance followed by the Tukey–Kramer test and a chi-square test for the animal experiments and the FAERS analysis, respectively (Statview; Abacus Concepts, Berkeley, CA, USA). A probability level of p < 0.05 was accepted as statistically significant.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Bun, S. et al. Symptom management: The utility of regional cooling for hand-foot syndrome induced by pegylated liposomal doxorubicin in ovarian cancer. Support. Care Cancer 26, 2161–2166 (2018).
Shinagawa-Kobayashi, Y. et al. Effect of histidine on sorafenib-induced vascular damage: Analysis using novel medaka fish model. Biochem. Biophys. Res. Commun. 496, 556–561 (2018).
Lévy, E. et al. Toxicity of fluorouracil in patients with advanced colorectal cancer: Effect of administration schedule and prognostic factors. J. Clin. Oncol. 16, 3537–3541 (1998).
Van Cutsem, E. et al. Oral capecitabine compared with intravenous fluorouracil plus leucovorin in patients with metastatic colorectal cancer: Results of a large phase III study. J. Clin. Oncol. 19, 4097–4106 (2001).
Walko, C. M. & Lindley, C. Capecitabine: A review. Clin. Ther. 27, 23–44 (2005).
Arkenau, H. T. et al. Efficacy of oxaliplatin plus capecitabine or infusional fluorouracil/leucovorin in patients with metastatic colorectal cancer: A pooled analysis of randomized trials. J. Clin. Oncol. 26, 5910–5917 (2008). [published correction appears in J. Clin. Oncol. 27, 5859 (2009).]
Noh, S. H. et al. Adjuvant capecitabine plus oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): 5-year follow-up of an open-label, randomised phase 3 trial. Lancet Oncol. 15, 1389–1396 (2014).
Kaufman, P. A. et al. Phase III open-label randomized study of eribulin mesylate versus capecitabine in patients with locally advanced or metastatic breast cancer previously treated with an anthracycline and a taxane. J. Clin. Oncol. 33, 594–601 (2015).
Heo, Y. S. et al. Hand-foot syndrome in patients treated with capecitabine-containing combination chemotherapy. J. Clin. Pharmacol. 44, 1166–1172 (2004).
Abushullaih, S., Saad, E. D., Munsell, M. & Hoff, P. M. Incidence and severity of hand-foot syndrome in colorectal cancer patients treated with capecitabine: A single-institution experience. Cancer Invest. 20, 3–10 (2002).
Degen, A. et al. The hand-foot-syndrome associated with medical tumor therapy—classification and management. J. Dtsch. Dermatol. Ges. 8, 652–661 (2010).
Miller, K. K., Gorcey, L. & Mclellan, B. N. Chemotherapy-induced hand-foot syndrome and nail changes: A review of clinical presentation, etiology, pathogenesis, and management. J. Am. Acad. Dermatol. 71, 787–794 (2014).
Zhang, R. X. et al. Celecoxib can prevent capecitabine-related hand-foot syndrome in stage II and III colorectal cancer patients: Result of a single-center, prospective randomized phase III trial. Ann. Oncol. 23, 1348–1353 (2012).
Macedo, L. T., Lima, J. P., dos Santos, L. V. & Sasse, A. D. Prevention strategies for chemotherapy-induced hand–foot syndrome: A systematic review and meta-analysis of prospective randomised trials. Support. Care Cancer 22, 1585–1593 (2014).
Nikolaou, V., Syrigos, K. & Saif, M. W. Incidence and implications of chemotherapy related hand-foot syndrome. Expert. Opin. Drug Saf. 15, 1625–1633 (2016).
Lou, Y. et al. Possible pathways of capecitabine-induced hand-foot syndrome. Chem. Res. Toxicol. 29, 1591–1601 (2016).
Xie, W. et al. Esomeprazole alleviates the damage to stress ulcer in rats through not only its antisecretory effect but its antioxidant effect by inactivating the p38 MAPK and NF-κB signaling pathways. Drug Des. Devel. Ther. 13, 2969–2984 (2019).
Balza, E. et al. Proton pump inhibitors protect mice from acute systemic inflammation and induce long-term cross-tolerance. Cell Death Dis. 7, e2304 (2016).
Chanchal, S. K. et al. In vivo and in vitro protective effects of omeprazole against neuropathic pain. Sci. Rep. 6, 30007 (2016).
Yohannes, T. et al. Pleiotropic effect of the proton pump inhibitor esomeprazole leading to suppression of lung inflammation and fibrosis. J. Transl. Med. 13, 249 (2015).
Tanigawa, T. et al. Lansoprazole, a proton pump inhibitor, suppresses production of tumor necrosis factor-alpha and interleukin-1beta induced by lipopolysaccharide and Helicobacter Pylori bacterial components in human monocytic cells via inhibition of activation of nuclear factor-kappaB and extracellular signal-regulated kinase. J. Clin. Biochem. Nutr. 45, 86–92 (2009).
Gao, H. et al. Omeprazole protects against cisplatin-induced nephrotoxicity by alleviating oxidative stress, inflammation, and transporter-mediated cisplatin accumulation in rats and HK-2 cells. Chem. Biol. Interact. 297, 130–140 (2019).
Eltahir, H. M. & Nazmy, M. H. Esomeprazole ameliorates CCl4 induced liver fibrosis in rats via modulating oxidative stress, inflammatory, fibrogenic and apoptotic markers. Biomed. Pharmacother. 97, 1356–1365 (2018).
Lugini, L. et al. Proton pump inhibitors while belonging to the same family of generic drugs show different anti-tumor effect. J. Enzyme Inhib. Med. Chem. 31, 538–545 (2016).
Pan, Y. Q. et al. The molecular mechanism underlying the induction of hepatic MRP3 expression and function by omeprazole. Biopharm. Drug Dispos. 36, 232–244 (2015).
Chen, M. et al. Reversal effects of pantoprazole on multidrug resistance in human gastric adenocarcinoma cells by down-regulating the V-ATPases/mTOR/HIF-1α/P-gp and MRP1 signaling pathway in vitro and in vivo. J. Cell Biochem. 133, 2474–2487 (2012).
Wang, B. Y. et al. Intermittent high dose proton pump inhibitor enhances the antitumor effects of chemotherapy in metastatic breast cancer. J. Exp. Clin. Cancer Res. 34, 85 (2015).
Ferrari, S. et al. Proton pump inhibitor chemosensitization in human osteosarcoma: From the bench to the patients’ bed. J. Transl. Med. 11, 268 (2013).
Falcone, R. et al. High-doses of proton pump inhibitors in refractory gastro-intestinal cancer: A case series and the state of art. Dig. Liver Dis. 48, 1503–1505 (2016).
Papagerakis, S. et al. Proton pump inhibitors and histamine 2 blockers are associated with improved overall survival in patients with head and neck squamous carcinoma. Cancer Prev. Res. 7, 1258–1269 (2014).
Chen, C. H. et al. Negative association of proton pump inhibitors with subsequent development of breast cancer: A nationwide population-based study. J. Clin. Pharmacol. 59, 350–355 (2019).
Ding, D. C. et al. Proton pump inhibitors reduce breast cancer risk in gastric ulcer patients: A population-based cohort study. Breast J. 26, 474–478 (2020).
Federici, C. et al. Lansoprazole and carbonic anhydrase IX inhibitors sinergize against human melanoma cells. J. Enzyme Inhib. Med. Chem. 31, 119–125 (2016).
Lugini, L. et al. Antitumor effect of combination of the inhibitors of two new oncotargets: Proton pumps and reverse transcriptase. Oncotarget 8, 4147–4155 (2017).
Spugnini, E. P. & Fais, S. Drug repurposing for anticancer therapies. A lesson from proton pump inhibitors. Expert. Opin. Ther. Pat. 30, 15–25 (2020).
Ikemura, K., Hiramatsu, S. & Okuda, M. Drug repositioning of proton pump inhibitors for enhanced efficacy and safety of cancer chemotherapy. Front. Pharmacol. 8, 911 (2017).
Lu, Z. N., Tian, B. & Guo, X. L. Repositioning of proton pump inhibitors in cancer therapy. Cancer Chemother. Pharmacol. 80, 925–937 (2017).
Chu, M. P. et al. Association of proton pump inhibitors and capecitabine efficacy in advanced gastroesophageal cancer: Secondary analysis of the TRIO-013/LOGiC Randomized Clinical Trial. JAMA Oncol. 3, 767–773 (2017).
Rhinehart, H. E. et al. Evaluation of the clinical impact of concomitant acid suppression therapy in colorectal cancer patients treated with capecitabine monotherapy. J. Oncol. Pharm. Pract. 25, 1839–1845 (2019).
Wong, G. G. et al. Effects of proton pump inhibitors on FOLFOX and CapeOx regimens in colorectal cancer. Clin. Colorectal. Cancer 18, 72–79 (2019).
Kim, S. Y. et al. Proton pump inhibitor use and the efficacy of chemotherapy in metastatic colorectal cancer: A post hoc analysis of a randomized phase III trial (AXEPT). Oncologist 10, 1002 (2021).
Chen, M. et al. The contribution of keratinocytes in capecitabine-stimulated hand-foot-syndrome. Environ. Toxicol. Pharmacol. 49, 81–88 (2017).
da Silva, L. M. et al. Evidence of gastric ulcer healing activity of Maytenus robusta Reissek: In vitro and in vivo studies. J. Ethnopharmacol. 175, 75–85 (2015).
Majeed, W. et al. Histopathological evaluation of gastro protective effect of Berberis vulgaris (Zereshk) seeds against aspirin induced ulcer in albino mice. Pak. J. Pharm. Sci. 28, 1953–1958 (2015).
Suzuki, Y. et al. Analysis of the interaction between clopidogrel, aspirin, and proton pump inhibitors using the FDA Adverse Event Reporting System Database. Biol. Pharm. Bull. 38, 680–686 (2015).
Acknowledgements
This work was supported by JSPS KAKENHI (JP20K07198).
Author information
Authors and Affiliations
Contributions
S.H, T.K. and N.Y. designed and performed the experiments and analyzed the data. S.H. and T.K wrote the texts. D.K., K.M., M.I., M.U. and T.S. provided critical advice on the experiments and data interpretation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hiromoto, S., Kawashiri, T., Yamanaka, N. et al. Use of omeprazole, the proton pump inhibitor, as a potential therapy for the capecitabine-induced hand-foot syndrome. Sci Rep 11, 8964 (2021). https://doi.org/10.1038/s41598-021-88460-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-88460-9
This article is cited by
-
Association Between Antidiabetic Drugs and Delirium: A Study Based on the Adverse Drug Event Reporting Database in Japan
Clinical Drug Investigation (2024)
-
Extract of the bioconverted fine root of ginseng induces apoptosis and cell cycle arrest in mouse colon cancer cells
Applied Biological Chemistry (2023)
-
Re-thinking the possible interaction between proton pump inhibitors and capecitabine
Cancer Chemotherapy and Pharmacology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.