Abstract
Emphysema is a major pathological change in chronic obstructive pulmonary disease (COPD). However, the annual changes in the progression of emphysematous have not been investigated. We aimed to determine possible baseline predicting factors of the change in emphysematous progression in a subgroup of COPD patients who demonstrated rapid progression. In this observational study, we analyzed patients with COPD who were followed up by computed tomography (CT) at least two times over a 3-year period (n = 217). We divided the annual change in the low attenuation area percentage (LAA%) into quartiles and defined a rapid progression group (n = 54) and a non-progression group (n = 163). Predictors of future changes in emphysematous progression differed from predictors of high LAA% at baseline. On multivariate logistic regression analysis, low blood eosinophilic count (odds ratio [OR], 3.22; P = 0.04) and having osteoporosis (OR, 2.13; P = 0.03) were related to rapid changes in emphysematous progression. There was no difference in baseline nutritional parameters, but nutritional parameters deteriorated in parallel with changes in emphysematous progression. Herein, we clarified the predictors of changes in emphysematous progression and concomitant deterioration of nutritional status in COPD patients.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by persistent respiratory symptoms and airflow limitation1. Emphysema is a major pathological change of COPD that is characterized by abnormal and permanent enlargement of distal airspaces as well as by alveolar wall destruction2. Airflow limitation is the main characteristic of COPD, but the severity of emphysema differs significantly among individuals who have similar forced expiratory volume in 1 s (FEV1)3. Chest computed tomography (CT) has been the most accurate and minimally invasive technique used for the diagnosis of emphysema4, and CT-diagnosed emphysema is strongly associated with more rapid decline in FEV15, worse health status6, and increased mortality rates7.
Progression of emphysema was found to be more sensitive using chest CT than by using lung function parameters8 and reported the utility as treatment outcome in COPD patients9. It has been reported that the progression of emphysema, as well as pulmonary function decline, varies between patients10. Thus, factors that could predict emphysematous progression are required. A recent study showed that sex, smoking status, plasma levels of surfactant protein D (SP-D), soluble receptor for advanced glycation endproducts (sRAGE)10, and the leptin/adiponectin ratio11 were associated with changes in emphysematous progression. Several recent large-scale cohort studies evaluated the changes in emphysematous progression; however subjects underwent chest CT at baseline and 3- to 5-year follow-up in these studies10,12. Emphysema quantification is very sensitive to various conditions, including the level of inspiration. Thus, when assessing longitudinal changes by chest CT, the appropriate number of times, calibration of different CT scanners, and the scanning protocol used are important13. However, the annual changes in emphysematous progression on chest CT have not been assessed in COPD patients.
Systemic manifestations and comorbidities of COPD also contribute to the different clinical phenotypes and alterations in body weight and composition, from cachexia to obesity, demanding specific management14. Several previous reports have demonstrated the association among emphysema, low body mass index (BMI), and osteoporosis in COPD patients15,16,17. We hypothesized that low BMI and having osteoporosis could predict future changes in emphysematous progression and that the annual change in emphysema would correlate with the annual change in BMI and bone mineral density (BMD). Thus, the aims of this study were threefold: 1) to identify a subgroup of COPD patients who demonstrate rapid progression of emphysematous change during a 3-year follow-up period; 2) to identify possible baseline factors, including comorbidities, which could predict the rapid progression of emphysematous change; and 3) to assess factors that change synchronously with emphysematous progression in COPD patients.
Methods
Study population
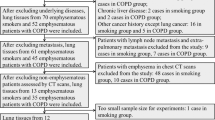
The overall design of the Keio COPD Comorbidity Research (K-CCR) has been published previously15,18. This study was a 3-year, prospective, observational study that enrolled 572 men and women, aged 40–91 years, diagnosed with COPD (n = 440) or as being at risk of COPD (n = 132) by pulmonary physicians, from April 2010 to December 2012. Data of COPD patients who underwent CT at least two times over a 3-year period (n = 217) were analyzed (Supplemental Fig. 1). All patients were clinically stable at all assessments and had no exacerbations for at least 1-month pre-enrollment.
Distribution of annual changes in LAA% and time-dependency over 3 years. (A) Distribution of the annual changes in LAA% over the 3-year period. The mean ± SD of ΔLAA%/year was 0.47 ± 2.28. We had arbitrarily defined the cut-off value of ΔLAA%/year, based on the upper quartile value, as 1.48%/year. (B) Overall time-dependent LAA% in the rapid progression and non-progression groups. Data are shown as mean ± SD. LAA low attenuation area.
Written informed consent for the use of data was obtained from each patient, and the study (University Hospital Medical Information Network; UMIN000003470) was approved by the ethics committees of Keio University and its affiliated hospitals (20,090,008). All methods were performed in accordance with the relevant guidelines and regulations.
Assessment of clinical parameters
At enrollment and annually, a full medical and smoking history, and current pharmacological treatment information, were obtained18. Comorbid conditions were diagnosed based on clinical history and physical examination, supported by medical record review18,19. Spirometry was performed in all patients using an electronic spirometer (CHESTAC-9800; CHEST, Tokyo, Japan) according to the American Thoracic Society guidelines20. Body mass composition, i.e., fat-free mass (FFM) and muscle mass (MM), was assessed using a Tanita BC-308/BC-309 bioelectrical impedance analyzer (Tanita, Inc., Tokyo, Japan)21. The FFM index (FFMI) was calculated as FFM divided by height-squared22.
Blood samples were collected at baseline and annually thereafter. A pre-specified eosinophil cut-off of 300 cells/μl was used to determine association with the change in emphysematous progression23,24.
The Japanese version of the COPD assessment test (CAT)25 and the St. George’s Respiratory Questionnaire (SGRQ)26,27,28 was performed at baseline. Independent investigators retrospectively judged the number and severity of exacerbations based on reviews of physicians’ medical records29.
Assessment of low attenuation areas and airway wall thickness on chest CT
CT was performed using four multi-detector CT scanners, including 64-detector CT (LightSpeed VCT and Discovery CT 750 HD, General Electric Medical Systems, Milwaukee, WI, USA, or Aquilion 64, Toshiba Medical Systems, Otawara, Japan) or 256-detector CT (Revolution CT, General Electric Medical Systems, Milwaukee, WI, USA) scanners. All subjects underwent volumetric CT at full inspiration and at the end of a normal expiration. Scanning parameters for each scanner were as follows: the detector collimation was 0.5–0.625 mm; beam pitch, 0.813–0.984; reconstruction thickness, 1.0–1.25 mm; reconstruction interval, 1.0–1.5 mm; rotation time, 0.35–0.5 s; tube voltage, 120 kVp; tube current, Auto mAs (standard deviation [SD] = 12–15); and reconstruction kernel, chest for GE machine or FC 50 for Toshiba machine. For calibration among four CT scanners, a test object (Multipurpose Chest Phantom N1; Kyoto Kagaku, Kyoto, Japan) was scanned at the start of the study using each scanner15. (Supplemental Fig. 2). The emphysema extent was quantified as the ratio of the low attenuation area to the total lung volume (LAA%), with Hounsfield units < − 950 (AZE Ltd., Tokyo, Japan)15.
As shown in Supplemental Fig. 2A below, the phantom was first scanned on one control CT scanner. The LAA% of this phantom varies depending on the cutoff HU value. When the cutoff LAA value was set at − 950 HU on the control CT scanner, LAA% was 76%. The same phantom was scanned on the other four scanners, and the cutoff HU level specific to each model by which LAA% became 76% was determined to allow adjustment (Supplemental Fig. 2B).
Dual X-ray absorptiometry
Dual X-ray absorptiometry (DXA) measurements of bone mineral density (BMD) were performed at both hips and lumbar spine using a Hologic 4500A Discovery bone densitometer (HOLOGIC, Bedford, MA). Osteoporosis diagnosis was based on the lowest T-score of these locations, according to World Health Organization criteria30.
Statistical analysis
Data were compared between two groups using Student’s t- and χ2 tests; three groups were compared by analysis of variance and χ2 tests. LAA%, BMD, and BMI were compared by percent changes from baseline values. Excel (Microsoft Inc. Redmond, WA) was used to calculate the linear regression through data points, including data in the middle31. Univariate and multivariate logistic regression analyses were performed to assess factors affecting change in emphysematous progression. Correlations between continuous variables were evaluated using Pearson’s correlation coefficient. Multivariate logistic regression analysis was performed using related factors that either reached significance or trended towards an association on univariate analyses. The changes of LAA%, BMI or BMD at each visit were estimated by a linear mixed effect model with groups; non-progression and rapid progression groups, time point, and time-by- groups interaction as fixed effects, subject as a random effect, to obtain point estimates and 95% confidence interval. The correlation structure was assumed as compound-symmetry structure. For all tests, two-sided p-values < 0.05 were considered significant. Data were analyzed using JMP 14 software (SAS Institute, Cary, NC).
Results
Clinical features of the study populations
Table 1 shows the baseline characteristics of the study participants. The average age of the COPD patients was 72.4 ± 8.4 years. The number of COPD patients in Global Initiative for Chronic Obstructive Lung Disease grades 1, 2, 3, and 4 were 30.8%, 47.0%, 17.5%, and 4.6%, respectively.
Distribution of annual changes in LAA% over a 3-year period
The annual changes in LAA% (ΔLAA%/year) is shown in Fig. 1A. The mean ΔLAA%/year was 0.47. We had arbitrarily defined the cut-off value of ΔLAA%/year based on an upper quartile value of 1.48%/year (Rapid progression group; n = 54, Non-progression group; n = 163). Figure 1B shows the longitudinal change in LAA% over the 3-year period in the two groups. The difference in the rate of LAA% change among the two groups was significant (P < 0.01). ΔLAA%/year significantly correlated with ΔLAA volume/year (r = 0.65, P < 0.01), but not ΔTotal lung volume (TLV)/year (r = 0.03, P = 0.77).
Baseline characteristics of COPD patients with emphysema and changes in emphysematous progression
The baseline characteristics of COPD patients, stratified by the baseline LAA% and annual change of LAA%, are shown in Table 2 and Supplemental Table 1. Patients with mild (LAA% ≥ 10% to < 20%) and moderate/severe(LAA% ≥ 20%) emphysema had lower lung function, lower BMI, more osteoporosis, and worse quality of life (QOL) scores than those without emphysema (LAA% < 10%) (Supplemental Table 1). In contrast, there were no differences in lung function, BMI, and QOL scores between the rapid progression group and the non-progression group. Additionally, the baseline LAA% and prevalence of interstitial pneumonia did not differ between these two groups (LAA%: P = 0.51; prevalence of interstitial pneumonia: P = 0.25). Interestingly, the eosinophil count was lower in the rapid emphysema group than in the non-progression group (eosinophil count: 150.7 ± 89.5 cells/mm3 vs. 226.9 ± 215.7 cells/mm3, P = 0.01) (Table 2). These results imply that baseline LAA% does not predict the rate of future changes in emphysematous progression and the related factors differ between baseline advanced emphysema and changes in emphysematous progression.
Relationships between nutritional status and changes in emphysematous progression in COPD patients
At baseline, there was no difference in BMI between the rapid progression group and the non-progression group (Fig. 2A). In contrast, follow-up analysis indicated that the difference in the rate of BMI change among the two groups was significant (P = 0.01) (Fig. 2B). As well as ΔBMI/year (r = − 0.21, P < 0.01), ΔFFMI/year (r = − 0.20, P < 0.01) and ΔMuscle mass/year (r = − 0.20, P < 0.01) correlated weakly but significantly with ΔLAA%/year. (Table 3).
Relationships between BMD and changes in emphysematous progression in COPD patients
The ratio of patients with osteoporosis and osteopenia was higher in COPD patients in the rapid progression group than in those in the non-progression group (osteoporosis: 22.5% vs. 10.3%; osteopenia: 36.7% vs. 29.5%, P = 0.03) (Fig. 3A). Additionally, the baseline BMD at all three parts of the body were significantly lower in the rapid progression group than in the non-progression group (lumbar spine: P = 0.03; right femur: P = 0.02; left femur: P = 0.03) (Fig. 3B, Supplemental Fig. 3A, B). Follow-up analysis over 3 years indicated that the difference in BMD between the two groups was statistically significant (lumbar spine: P < 0.01; right femur: P < 0.01; left femur: P < 0.01), but there was no significant difference in the rate of BMD change between the two groups (lumbar spine: P = 0.80; right femur: P = 0.88; left femur: P = 0.76) (Fig. 3C, Supplemental Fig. 3C, D).
Relationships between lumbar BMD and changes in emphysematous progression in COPD patients. (A) Frequency of osteopenia and osteoporosis in the non-progression group and rapid progression group. (B) Comparison of baseline T score in the lumbar spine between the two groups. (C) Annual change in BMD in the lumbar spine in the two groups over 3 years of follow-up. Data are shown as mean ± SD. BMD bone mineral density.
Predictors and factors showing synchronized progression with emphysematous change in COPD patients
We assessed the predictors of future changes in emphysematous progression using multivariate logistic analysis in which we included several factors that reached significance on univariate analysis (Tables 4). Low blood eosinophilia (< 300 cells/μl) (odds ratio [OR] 3.22, P = 0.04), having osteoporosis or osteopenia (OR 2.13, P = 0.03) independently predicted future changes in emphysematous progression. There was no difference in the incidence of moderate and severe exacerbations, change in smoking habits, or change in treatment between the rapid emphysema group and the non-progression group over the 3-year period (Supplemental Table 2). Also, there were no differences in the he annual ΔCAT score and ΔSGRQ total score between the two groups (Supplemental Fig. 4).
Ethics approval and consent to participate
Written informed consent for the use of data was obtained from each patient. This study was registered on the University Hospital Medical Information Network (UMIN000003470) and was approved by the ethics committees of Keio University and its affiliated hospitals (20,090,008).
Discussion
In this longitudinal study in patients with COPD, we identified possible baseline factors, including comorbidities, that could predict the rapid progression of emphysematous change at three time points; this has not been reported previously. We demonstrated that having osteoporosis and low blood eosinophilia were predictors of future rapid changes in emphysematous progression; additionally, cachexia and health status deteriorated with changes in emphysematous progression.
Previous studies, including our own, have shown an association between emphysema and osteoporosis15,16. However, the influence of having osteoporosis on changes in emphysematous progression has remained unclear. The present study showed that having osteoporosis is an important predictor of not only baseline emphysema presence, but also of future changes in emphysematous progression in COPD patients. These results imply that osteoporosis is closely related to emphysema. Systemic inflammation is a plausible mechanistic link between emphysema and osteoporosis32,33. However, this concept had not been considered in detail to date. Future studies should focus on the development of targeted therapies designed to prevent the progression of both these disease processes.
Cachexia and muscle wasting are well-recognized comorbidities in COPD patients, and a number of studies have reported that these comorbidities contribute to decreased QOL31 and increased mortality35,36. In a previous study, baseline BMI and FFMI were not related to baseline LAA%, but ΔBMI, ΔFFMI, and other nutrition indexes were correlated with changes in emphysematous progression. These results were in line with previous studies that demonstrated that lung volume reduction surgery (LVRS) significantly improved nutritional status37. Additionally, these results indicated that, even if nutritional status at enrollment is within the normal range, the nutritional status of COPD patients with changes in emphysematous progression deteriorates over time. An imbalance between protein synthesis and myogenesis has been proposed to underlie muscle wasting in COPD patients38, and nutritional supplementation promotes weight gain among COPD patients, especially if they are malnourished39. Patients who have related factors of changes in emphysematous progression might be requiring nutritional supplementation and targeted pharmacological interventions.
Recently, several studies have shown that the blood eosinophil count is predictive of exacerbations40 and a good response to inhaled corticosteroids41,42. Interestingly, even if they are within the normal range, the blood eosinophil count was significantly higher in the non-progression group than in the rapid progression group in the present study. This result is in line with previous studies showing that high eosinophil counts were related to less emphysema43, better survival22,44, and a slower annual FEV1 decline23. The specific cause and effect relationship between emphysema progression and low blood eosinophilia is unclear. Previous reports have demonstrated that T helper 1 and 17 cells are relatively abundant in lungs of patients with emphysema compared with those in lungs of former smokers without emphysema12. T helper 1-predominant inflammation appears to progress emphysema more rapidly compared to T helper 2-predominant inflammation, a difference that would be related to blood eosinophilia45. Blood eosinophil count is thus a simple and inexpensive biomarker predictive of future changes in emphysematous progression.
In COPD patients, the relative contributions of emphysema and small airway disease differ among patients3,46. Emphysema-predominance is reported to be associated with greater exercise limitation, reduced QOL47, and reduced mortality48.
Large clinical trials of COPD patients have shown that current pharmacological treatments have improved lung function49,50. Furthermore, Tanabe et al. reported the tiotropium-induced reduction of emphysema volume based on CT images9. However, the prognostic value thereof and appropriate therapy for progressive emphysema are unknown. These matters should be considered in future research.
Recent advance of CT metrics has improved phenotyping of COPD. For instance, parametric response mapping identified the extent of functional small airway disease and emphysema51. In addition, CT-derived pectoralis muscle area provides a relevant index of COPD morbidity52. Further studies that evaluate the relationship among changes in emphysematous progression and these new CT metrics are required.
This study has several strengths. First, the comprehensive assessment of comorbid factors in the K-CCR cohort study18,19. Second, assessment of changes in emphysematous progression was based on annual CT over 3 years. In this study, the ΔLAA%/year and not ΔTLV/year correlated with LAA volume. These results imply that the increase in ΔLAA%/year was due to the increase in ΔLAA volume/year, but not that of ΔTLV/year. Emphysema quantification is very sensitive to various conditions, including the level of inspiration, and this issue becomes more important when assessing longitudinal changes by chest CT13. Thus, we first carefully performed calibration using a lung phantom and annual CT. The distribution of ΔLAA% is diverse across the previous reports10,53,54. In this study, ΔLAA% was normally distributed and about 58.1% of participants were categorized in − 1 to 1 (ΔLAA%) / year. These results were consistent with the previous report53, but inconsistent with other report10. This discrepancy may be caused by differences in the inspiration levels or different machines.
There were several limitations to this study. First, Japanese COPD patients are reported to have a lower BMI and fewer exacerbations than COPD patients in other countries29,55. Thus, this study’s population may not reflect the general COPD population worldwide. Second, the number of females in this study was relatively small. It has been reported that male smokers are more likely to develop emphysema than female smokers56. Thus, the findings of our study may not be extrapolatable to female COPD patients. Third, we could not analyze the long-term follow-up outcome such as the rate of hospitalization or mortality. To date, the relationship between changes in of emphysematous progression and these outcomes are unknown. Further studies involving larger number of nested patients and longer follow-up are necessary. Fourth, we could not perform CT using a single CT scanner in this study. Although the calibration among four CT scanners was performed, the differences of CT values in the different scanners might have affected the results.
Conclusion
The rapid emphysema progression group exhibited a lower eosinophil count, and more often had osteoporosis than the non-progression group. Additionally, rapid progression of emphysema is associated with on-going deterioration of nutritional status in COPD patients. Future studies should focus on appropriate intervention for rapid changes in emphysematous progression and patients who are at risk of rapid emphysematous progression and might be requiring nutritional supplementation and targeted pharmacological interventions.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- LAA:
-
Low attenuation area
- ΔLAA%/year:
-
Annual changes in LAA%
- BMI:
-
Body mass index
- BMD:
-
Bone mineral density
- COPD:
-
Chronic obstructive pulmonary disease
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- CAT:
-
COPD assessment test
- CRP:
-
C-reactive protein
- DXA:
-
Dual X-ray absorptiometry
- FFM:
-
Fat-free mass
- FFMI:
-
FFM index
- FEV1 :
-
Forced expiratory volume in 1 s
- %FEV1 :
-
Forced expiratory volume in 1 s as a percentage of predicted forced expiratory volume in 1 s
- GOLD:
-
Global Initiative for Chronic Obstructive Lung Disease
- ICS:
-
Inhaled corticosteroids
- K-CCR:
-
Keio COPD Comorbidity Research
- LAA%:
-
Low attenuation area percentage
- LVRS:
-
Lung volume reduction surgery
- MM:
-
Muscle mass
- OR:
-
Odds ratio
- QOL:
-
Quality of life
- SAA:
-
Serum amyloid A
- sRAGE:
-
Soluble receptor for advanced glycation end products
- SGRQ:
-
St. George’s Respiratory Questionnaire
- SP-D:
-
Surfactant protein D (SP-D)
- TLV:
-
ΔTotal lung volume
- WA%:
-
The percentage of airway wall area
References
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management and prevention of COPD (2019 Report). Fontana, WI: Global Initiative for Chronic Obstructive Lung Disease (GOLD). https://goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf. Accessed March 25 2019.
Snider, G. L., Kleinerman, J., Thurlbeck, W. M. & Bengali, Z. H. The definition of emphysema. Report of a national heart, lung, and blood institute, division of lung diseases workshop. Am. Rev. Respir. Dis. 132, 182–185 (1985).
Makita, H. et al. Characterization of phenotypes based on severity of emphysema in chronic obstructive pulmonary disease. Thorax 62, 932–937 (2007).
Gould, G. A. et al. CT measurements of lung density in life can quantitate distal airspace enlargement–an essential defining feature of human emphysema. Am. Rev. Respir. Dis. 137, 380–392 (1988).
Nishimura, M. et al. Annual change in pulmonary function and clinical phenotype in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 185, 44–52 (2012).
Martinez, C. H. et al. Relationship between quantitative CT metrics and health status and BODE in chronic obstructive pulmonary disease. Thorax 67, 399–406 (2012).
Johannessen, A. et al. Mortality by level of emphysema and airway wall thickness. Am. J. Respir. Crit. Care Med. 187(6), 602–608 (2013).
Stolk, J. et al. Progression parameters for emphysema: a clinical investigation. Respir. Med. 101(9), 1924–1930 (2007).
Tanabe, N. et al. Computed tomography assessment of pharmacological lung volume reduction induced by bronchodilators in COPD. COPD 9, 401–408 (2012).
Coxson, H. O. et al. The presence and progression of emphysema in COPD as determined by CT scanning and biomarker expression: a prospective analysis from the ECLIPSE study. Lancet Respir. Med. 1, 129–136 (2013).
Oh, Y. M. et al. Association of plasma adipokines with chronic obstructive pulmonary disease severity and progression. Ann. Am. Thorac. Soc. 12, 1005–1012 (2015).
Pompe, E. et al. Five-year progression of emphysema and air trapping at CT in smokers with and those without chronic obstructive pulmonary disease: results from the COPDGene study. Radiology 295, 218–226 (2020).
Han, M. K. Clinical correlations of computed tomography imaging in chronic obstructive pulmonary disease. Ann. Am. Thorac. Soc. 10(Suppl 1), 131–137 (2013).
Vanfleteren, L. E. G. W., Spruit, M. A., Wouters, E. F. M. & Franssen, F. M. E. Management of chronic obstructive pulmonary disease beyond the lungs. Lancet Respir. Med. 4, 911–924 (2016).
Chubachi, S. et al. Polymorphism of LRP5 gene and emphysema severity are associated with osteoporosis in Japanese patients with or at risk for COPD. Respirology 20, 286–295 (2015).
Ohara, T. et al. Relationship between pulmonary emphysema and osteoporosis assessed by CT in patients with COPD. Chest 134, 1244–1249 (2008).
Ogawa, E. et al. Body mass index in male patients with COPD: correlation with low attenuation areas on CT. Thorax 64, 20–25 (2009).
Miyazaki, M. et al. Analysis of comorbid factors that increase the COPD assessment test scores. Respir. Res. 15, 13 (2014).
Chubachi, S. et al. Identification of five clusters of comorbidities in a longitudinal Japanese chronic obstructive pulmonary disease cohort. Respir. Med. 117, 272–279 (2016).
Miller, M. R. et al. Standardisation of spirometry. Eur. Respir. J. 26, 319–338 (2005).
Frits, M. et al. New reference values for body composition by bioelectrical impedance analysis in the general population: results from the UK Biobank. J. Am. Med. Dir. Assoc. 15(6), 448.e1–6 (2014).
Vahlberg, B., Zetterberg, L., Lindmark, B., Hellstrom, K. & Cederholm, T. Functional performance, nutritional status, and body composition in ambulant community-dwelling individuals 1–3 years after suffering from a cerebral infarction or intracerebral bleeding. BMC Geriatr. 16, 48 (2016).
Shin, S. H. et al. Serial blood eosinophils and clinical outcome in patients with chronic obstructive pulmonary disease. Respir. Res. 19, 134 (2018).
Suzuki, M. et al. Asthma-like features and clinical course of chronic obstructive pulmonary disease. An analysis from the Hokkaido COPD Cohort Study. Am. J. Respir. Crit. Care Med. 194, 1358–1365 (2016).
Jones, P. W. et al. Development and first validation of the COPD assessment test. Eur. Respir. J. 34, 648–654 (2009).
Hajiro, T. et al. Analysis of clinical methods used to evaluate dyspnea in patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 158, 1185–1189 (1998).
Hajiro, T. et al. Comparison of discriminative properties among disease-specific questionnaires for measuring health-related quality of life in patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 157(3 Pt 1), 785–790 (1998).
Jones, P. W., Quirk, F. H., Baveystock, C. M. & Littlejohns, P. A self-complete measure of health status for chronic airflow limitation. The St. George’s Respiratory Questionnaire. Am. Rev. Respir. Dis. 145, 1321–1327 (1992).
Sato, M. et al. Impact of mild exacerbation on COPD symptoms in a Japanese cohort. Int. J. Chron. Obstruct. Pulmon. Dis. 11, 1269–1278 (2016).
Prevention and management of osteoporosis. World Health Organ Tech. Rep. Ser. 921, 1–164 (2003).
Irie, H. et al. Characteristics of patients with increasing COPD assessment test scores within 3 years. Respir. Med. 131, 101–108 (2017).
Bai, P. et al. Disturbance of the OPG/RANK/RANKL pathway and systemic inflammation in COPD patients with emphysema and osteoporosis. Respir. Res. 12, 157 (2011).
Sabit, R. et al. Arterial stiffness and osteoporosis in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 175, 1259–1265 (2007).
Mostert, R., Goris, A., Weling-Scheepers, C., Wouters, E. F. & Schols, A. M. Tissue depletion and health related quality of life in patients with chronic obstructive pulmonary disease. Respir. Med. 94, 859–867 (2000).
Vestbo, J. et al. Body mass, fat-free body mass, and prognosis in patients with chronic obstructive pulmonary disease from a random population sample: findings from the Copenhagen City Heart Study. Am. J. Respir. Crit. Care Med. 173, 79–83 (2006).
Schols, A. M., Broekhuizen, R., Weling-Scheepers, C. A. & Wouters, E. F. Body composition and mortality in chronic obstructive pulmonary disease. Am. J. Clin. Nutr. 82, 53–59 (2005).
Mineo, T. C. et al. Bone mineral density improvement after lung volume reduction surgery for severe emphysema. Chest 127, 1960–1966 (2005).
Rutten, E. P. et al. Greater whole-body myofibrillar protein breakdown in cachectic patients with chronic obstructive pulmonary disease. Am. J. Clin. Nutr. 83, 829–834 (2006).
Ferreira, I. M., Brooks, D., White, J. & Goldstein, R. Nutritional supplementation for stable chronic obstructive pulmonary disease. Cochrane Database. Syst. Rev. 12, CD00098 (2012).
Vedel-Krogh, S., Nielsen, S. F., Lange, P., Vestbo, J. & Nordestgaard, B. G. Blood eosinophils and exacerbations in chronic obstructive pulmonary disease. The Copenhagen General Population Study. Am. J. Respir. Crit. Care Med. 193, 965–974 (2016).
Pascoe, S., Locantore, N., Dransfield, M. T., Barnes, N. C. & Pavord, I. D. Blood eosinophil counts, exacerbations, and response to the addition of inhaled fluticasone furoate to vilanterol in patients with chronic obstructive pulmonary disease: a secondary analysis of data from two parallel randomised controlled trials. Lancet Respir. Med. 3, 435–442 (2015).
Siddiqui, S. H. et al. Blood eosinophils: a biomarker of response to extrafine beclomethasone/formoterol in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 192, 523–525 (2015).
Singh, D. et al. Eosinophilic inflammation in COPD: prevalence and clinical characteristics. Eur. Respir. J. 44, 1697–1700 (2014).
Turato, G. et al. Blood eosinophilia neither reflects tissue eosinophils nor worsens clinical outcomes in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 197, 1216–1219 (2018).
Shan, M. et al. Lung myeloid dendritic cells coordinately induce TH1 and TH17 responses in human emphysema. Sci. Transl. Med. 1, 4ra10 (2009).
Galban, C. J. et al. Computed tomography-based biomarker provides unique signature for diagnosis of COPD phenotypes and disease progression. Nat. Med. 18, 1711–1715 (2012).
Hersh, C. P. et al. Non-emphysematous chronic obstructive pulmonary disease is associated with diabetes mellitus. BMC Pulm. Med. 14, 164 (2014).
Haruna, A. et al. CT scan findings of emphysema predict mortality in COPD. Chest 138, 635–640 (2010).
Antoniu, S. A. UPLIFT Study: the effects of long-term therapy with inhaled tiotropium in chronic obstructive pulmonary disease. Evaluation of: Tashkin DP, Celli B, Senn S et al.: A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N. Engl. J. Med. 359(15), 1543–1554 (2008).
Vogelmeier, C. F. et al. Efficacy and safety of once-daily QVA149 compared with twice-daily salmeterol-fluticasone in patients with chronic obstructive pulmonary disease (ILLUMINATE): a randomised, double-blind, parallel group study. Lancet Respir. Med. 1, 51–60 (2013).
Galbán, C. J. et al. Computed tomography-based biomarker provides unique signature for diagnosis of COPD phenotypes and disease progression. Nat. Med. 18, 1711–1715 (2002).
McDonald, M. L. et al. Quantitative computed tomography measures of pectoralis muscle area and disease severity in chronic obstructive pulmonary disease. A cross-sectional study. Ann. Am. Thorac. Soc. 11, 326–334 (2014).
Bhavani, S. et al. Clinical and immunological factors in emphysema progression. Five-year prospective longitudinal exacerbation study of chronic obstructive pulmonary disease (LES-COPD). Am. J. Respir. Crit. Care Med. 192(10), 1171–1178 (2015).
Tanabe, N. et al. Impact of exacerbations on emphysema progression in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 183(12), 1653–1659 (2011).
Fukuchi, Y. et al. Efficacy of tiotropium in COPD patients from Asia: a subgroup analysis from the UPLIFT trial. Respirology 16, 825–835 (2011).
Camp, P. G. et al. Sex differences in emphysema and airway disease in smokers. Chest 136, 1480–1488 (2009).
Acknowledgements
The authors would like to acknowledge Chiyomi Uemura for her contribution towards collecting data and all members of the Keio COPD Comorbidity Research (K-CCR) group for participation in this study. The authors would like to acknowledge Yasunori Sato for helping the statistical analysis.
Author information
Authors and Affiliations
Contributions
A.T. participated in the design of the study, performed the statistical analyses, and was a major contributor in writing the manuscript. S.C. planned the study design and contributed to interpretation of results. T.B. conceived the study, participated in its design and coordination, and helped draft the manuscript.A. T., S. C., H. I., M. S., Y. Y., H. S., M. J., H. N., K. A., T. B., and K. F. collected the cohort datasets and revised the manuscripts critically for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tsutsumi, A., Chubachi, S., Irie, H. et al. Characteristics of chronic obstructive pulmonary disease patients with robust progression of emphysematous change. Sci Rep 11, 9548 (2021). https://doi.org/10.1038/s41598-021-87724-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-87724-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.