Abstract
Emphysematous smokers with normal spirometry form a considerable proportion of the clinical population. However, despite presenting with respiratory symptoms and activity limitation, they cannot be diagnosed with chronic obstructive lung disease (COPD) according to current criteria. Thus, we aimed to determine whether emphysema in smokers has a different pathogenesis from that in patients with COPD. We compared 12 pairs of lung tissue samples from emphysematous patients with normal spirometry and COPD, and determined the degree of emphysema using computed tomography. With a focus on COPD-related pathogenesis, we independently assessed inflammatory response, protease-antiprotease balance, oxidative stress, and apoptosis in both groups. Both groups showed similar pathological changes at a comparable degree of emphysema; the expression of inflammatory factors was comparable, with overexpression of proteases and decreased levels of antiproteases. Moreover, there was no significant difference in the activities of glutathione and superoxide dismutase, and expression of apoptosis-related factors. In conclusion, emphysema in smokers with normal spirometry and in patients with COPD had similar pathogenesis. Forced expiratory volume in 1 second cannot be used as the sole diagnostic criterion in patients with COPD; early intervention is of great importance to such patients.
Similar content being viewed by others
Introduction
Chronic obstructive lung disease (COPD) is a chronic respiratory airway disease, with symptoms such as cough, sputum, and shortness of breath1. The two most prominent pathological changes associated with COPD are the structural destruction of lung tissue and airway remodelling2. Currently, spirometry is the sole diagnostic criterion for COPD1,3.
Forced expiratory volume in 1 second (FEV1) primarily reflects airflow obstruction and is therefore not suitable for assessing COPD symptoms such as emphysema4,5,6,7,8. Studies have shown that there is a poor correlation between FEV1 and COPD symptoms5,6, as well between FEV1 and the degree of emphysema, as assessed by computed tomography (CT)7,8.
Patients with COPD show high heterogeneity in terms of clinical symptoms, structural destruction, and airway damage9,10. In some patients, structural destruction of lung tissue is more prominent, and their emphysema severity develops progressively11. These patients are termed emphysema phenotype of COPD12,13, and their structure destruction can be assessed with chest CT scans14,15. However, chest CT scans have revealed that a considerable number of smokers with obvious emphysema and lung tissue damage show preserved pulmonary function14,15,16. According to the current diagnostic criteria, such emphysematous smokers cannot be diagnosed with COPD. If they have same pathogenesis as patients with emphysematous COPD, appropriate interventions to reduce the clinical symptoms and block emphysema progression would be challenging in emphysematous smokers5,17.
In this study, we hypothesized that emphysematous smokers with normal spirometry and emphysematous patients with COPD exhibit similar pathophysiological parameters. The appropriate diagnosis of emphysematous patients with normal spirometry cannot be achieved using only the ratio of forced expiratory volume in 1 second to forced vital capacity (FEV1/FVC)5,17, as it can delay their treatment and result in progression of structural destruction11. That will significantly affect the quality of life and survival time of patients6,7,8,18. To test this hypothesis, we collected lung tissue from emphysematous smokers with normal spirometry and emphysematous patients with COPD. Two groups of smokers and patients with COPD with similar emphysema scores were identified after screening. Finally, we examined the extent of inflammatory response, oxidative stress, protease-antiprotease balance, and apoptosis.
Results
Demographics of clinical subjects
We collected lung tissue from 140 emphysematous smokers and 81 emphysematous patients with COPD from 2016 to 2018, according to the inclusion criteria. After excluding subjects according to the exclusion criteria and CT emphysema score, only 13 emphysematous smokers with normal spirometry and 35 emphysematous patients with COPD were included in this study and categorized into the emphysematous smokers and emphysematous patient with COPD groups, respectively. According to the inter-group pairing criteria, 12 pairs (24 samples) of lung tissues were included in the experiment. The details of screening and inter-group pairing are shown in Fig. 1 and Table 1.
There were no significant differences in the demographics between both groups. For spirometry parameters, statistical difference was observed only for FEV1, FEV1%, FEV1/FVC between both groups (Table 2).
Identification of comparable degree of emphysema between emphysematous smokers and emphysematous patients with COPD
After preliminary screening by two experienced imaging specialists, the degree of emphysema in the subjects was analysed from chest CT scans using CT analysis software. The degree and distribution of emphysema were similar in both groups (Fig. 2). Among all analysed parameters, only the volume of air in emphysematous patients with COPD was slightly higher than that in emphysematous smokers (1951 ± 180.1 vs. 2525 ± 204.1, P = 0.047). Emphysema index (6.468 ± 2.14 vs. 8.936 ± 3.095, P = 0.513) and emphysema percentile density (−907.8 ± 10.95 vs. −930.4 ± 10.17, P = 0.149) were not statistically different between both groups (Table 3).
Representative chest CT images and HE images of lung sections. (a) Representative CT analysis images of emphysema in subjects. The left and right lungs are distinguished by surrounding lines of different colours (yellow, for left lung and green for right lung). Emphysema is represented by the green area in lungs. (b) Representative haematoxylin and eosin images of lung sections. Lung sections were stained with HE and examined under a light microscope. The magnification scale is indicated in each figure panel.
Additionally, haematoxyline-eosin (HE) staining revealed typical histological morphology of emphysema, such as obvious alveolar septal destruction, alveolar fusion, and pulmonary bullae formation, in both groups. The degree of pathological emphysema was also similar (Fig. 2).
Expression of inflammatory factors in emphysematous smokers and emphysematous patients with COPD patients is similar
There was no statistical difference in the expression levels of interleukin (IL)−6 (Fig. 3a; 0.57 ± 0.32 vs. 0.76 ± 0.18, P = 0.686), IL-10 (Fig. 3b; 1.43 ± 0.49 vs. 1.98 ± 0.64, P = 0.507), IL-1β (Fig. 3c; 1.52 ± 0.58 vs. 1.94 ± 0.51, P = 0.336), and tumour necrosis factor (TNF)-α (Fig. 3d; 1.46 ± 0.47 vs. 2.46 ± 0.69, P = 0.234), in lung tissue between both groups. However, the expression of inflammatory factors in the lung tissue of patients with COPD was higher than that in emphysematous smokers.
Expression of inflammatory factors in lung tissues. (a) IL-6 (n = 4 in each group), (b) IL-10 (n = 7 in each group), (c) IL-1b (n = 8 for smokers and 7 for patients with COPD), and (d) TNF-α (n = 7 for each group) mRNA expression in lung tissues was measured using real-time PCR. Data represent the mean ± SEM from three independent experiments.
Protease-antiprotease imbalance exists in both emphysematous smokers with normal spirometry and emphysematous patients with COPD
We determined the expression of representative factors that have opposing effects on the protease-antiprotease balance. There was no significant difference in the expression of neutrophil elastase (NE) (Fig. 4a,b; 0.87 ± 0.09 vs. 0.85 ± 0.08, P = 0.864), matrix metalloproteinase- 9 (MMP-9) (Fig. 4a,c; 1.07 ± 0.26 vs. 1.47 ± 0.47, P = 0.652) and MMP-12 (Fig. 4a,d; 1.94 ± 0.16 vs. 2.12 ± 0.35, P = 0.949) in lung tissue between both groups. Moreover, the expression of alpha-l antitrypsin (AAT) (Fig. 4a,e; 0.69 ± 0.16 vs. 0.78 ± 0.19, P = 0.693), secretory leukocyte peptidase inhibitor (SLPI) (Fig. 4a,f; 0.52 ± 0.19 vs. 0.50 ± 0.17, P = 0.945) and metalloproteinase −1 (TIMP-1) (Fig. 4a,g; 0.61 ± 0.11 vs. 0.55 ± 0.11, P = 0.721)—important anti-protease factors—were comparable in both groups.
Comparison of protease-antiprotease balance and expression of apoptotic factors between both groups. Western blot analysis of (a,b) NE (n = 11 in each group), (a,c) MMP-9 (n = 11 in each group), (a,d) MMP-12 (n = 11 in each group), (a,e)AAT (n = 11 in each group), (a,f) SLPI (n = 11 in each group), (a,g) TIMP-1 (n = 11 in each group), (a,h) Caspase-3 (n = 11 in each group), (a,i) Caspase-8 (n = 11 in each group), (a,j) Bax (n = 11 in each group), (a,k) Bcl-2 (n = 11 in each group) and (a,l) Survivin (n = 11 in each group) expression in lung tissues of emphysematous smokers and emphysematous patients with COPD. There was no significant difference between both. Data represent the mean ± SEM from three independent experiments. Full-length blots are presented in Supplementary Fig. S1.
Expression of apoptosis-related factors in emphysematous smokers and emphysematous patients with COPD is similar
The expression of apoptosis-related factors Caspase-3 (Fig. 4a,h; 0.68 ± 0.09 vs. 0.95 ± 0.12, P = 0.079), Caspase-8 (Fig. 4a,i; 2.07 ± 0.23 vs. 2.22 ± 0.19, P = 0.519), and Bax (Fig. 4a,j; 1.01 ± 0.04 vs. 1.20 ± 0.24, P = 0.748) was similar between both groups. Moreover, the expression of anti-apoptotic molecules Bcl-2 (Fig. 4a,k; 0.86 ± 0.19 vs. 0.65 ± 0.10, P = 0.519) and Survivin (Fig. 4a,l; 1.27 ± 0.11 vs. 1.47 ± 0.11, P = 0.217) was similar between both groups.
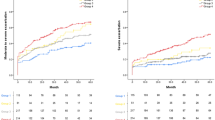
Emphysematous smokers and emphysematous patients with COPD exhibit similar levels of oxidative stress
We used an oxidative stress kit to detect oxidative stress response in both groups. The major indicators of oxidative stress included total glutathione (GSH), reduced GSH, and superoxide dismutase (SOD) activity. The levels of total GSH (Fig. 5a; 590.6 ± 197.8 vs. 190.9 ± 83.49, P = 0.20) and reduced GSH (Fig. 5b; 241.6 ± 72.43 vs. 108.4 ± 43.36, P = 0.20) were not significantly different between both groups, and SOD activity (Fig. 5c; 3.46 ± 0.18 vs. 4.74 ± 0.56, P = 0.142) was comparable. However, the oxidative stress-related index for the COPD group was higher than that for the normal spirometry group.
Discussion
COPD is a remarkably heterogeneous disease. CT identifying emphysema phenotype is one of the most important COPD sub-phenotypes. However, CT scan analysis has revealed that approximately 20% of the emphysematous smokers show preserved pulmonary function19. They might have significant respiratory symptoms (COPD Assessment Test scores ≥10), limitation of activity, and exacerbations of COPD; however, they did not meet the spirometric criteria of COPD20. More importantly, several studies have confirmed that emphysema is an independent risk factor for patient mortality, and is independent of airflow limitation7. Smokers without spirometrically diagnosed COPD have been overlooked in clinical practice5,21,22. Therefore, emphysematous smokers with normal spirometry should receive early intervention to prevent progression of structural destruction, improve their quality of life, and prolong their survival time5,6,7,8,23,24,25. Based on these clinical findings, we selected smokers with normal spirometry and patients with COPD showing a similar degree of emphysema, and determined inflammatory response, protease-antiprotease balance, oxidative stress levels, and apoptosis-related protein expression in their lung tissues, to identify pathophysiological differences between them.
Our results showed that the expression of IL-6, IL-10, IL-1β, and TNF-α did not significantly differ between both groups, indicative of comparable inflammatory response. The expression of IL-6 was lower than that of other inflammatory factors, which confirmed that the levels of inflammatory factors in lung tissue are different26. However, the expression of inflammatory factors in emphysematous patients with COPD was slightly higher than that in emphysematous smokers. This result is consistent with the view that smokers with high inflammatory levels are more likely to develop COPD26. NE, MMP-9 and MMP-12 are important protease family members, and AAT, SLPI and TIMP-1 plays an important role as an anti-protease9,27,28. The expression of these molecules was similar in both groups, suggesting that there is a significant protease-antiprotease imbalance in emphysematous smokers with normal spirometry. In addition, the level of reduced GSH was higher and SOD activity was lower in emphysematous smokers with normal spirometry than that in emphysematous patients with COPD. However, the difference was not statistically significant. We presume that oxidative stress might be one of the main reasons that caused differences in spirometry between both groups.
In order to perform comprehensive comparison, we assessed the expression of apoptosis-related proteins in both groups. The expression of Caspase-3, Caspasse-8, Bax, Bcl-2, and Survivin was not significantly different between both groups. However, the expression of Survivin in patients with COPD was relatively higher than that in emphysematous smokers, which is in contrast to the anti-apoptotic effect of Survivin. We speculate that the increased expression of Caspase family members might upregulate Survivin expression29. Moreover, the expression of Bcl-2, another anti-apoptotic factor, was relatively higher in emphysematous smokers than that in emphysematous patients with COPD. Studies have confirmed Bcl-2 expression does not correlate with Survivin expression, which may also explain the relatively higher expression of Survivin in patients with COPD30.
Our study demonstrates that smokers with normal spirometry and patients with COPD exhibit comparable inflammatory response, oxidative stress, protease-antiprotease balance, and apoptosis levels, under similar degree of emphysema. These results indicate that both groups of subjects exhibit similar pathophysiological parameters and therefore should be treated equally.
Previous studies have indicated that there is considerable proportion of emphysematous smokers with normal spirometry in clinical practice12,14,16. Emphysematous smokers develop more serious respiratory symptoms, have worse quality of life, and shorter survival time than other smokers5,6,7. However, a majority of these studies were clinical researches. In this study, we explored the intrinsic relationship between emphysematous smokers and emphysematous patients with COPD by examining major pathophysiological parameters, such as key molecules in inflammatory response, protease-antiprotease imbalance, oxidative stress, and apoptosis31. Our findings confirmed that both groups exhibit similar pathophysiological parameters. It indicated that emphysema patients with normal spirometry not only have structural destruction of lung tissue, but also had the pathological basis and disease development direction consistent with emphysema COPD patients.
As the emphysema sites might affect patient’s airflow diversely, both groups of patients revealed consistent pathological manifestations and variant airflow limitation degrees32. In addition, emphysematous patients in whom small airways are affected would be less sensitive to spirometry33, because FEV1 predominantly reflects the function of large airways. Consequently, FEV1 cannot determine the symptoms and severity of patients with COPD4,5,6. Hence, FEV1 result is not a sensitive indicator of emphysema and cannot be relied on to determine whether patients should receive intervention.
Using the pathogenesis of COPD and emphysema as the breakthrough point, we confirmed the close relation between emphysematous smokers and emphysematous patients with COPD at the molecular mechanism level, and provided strong evidence regarding similarities in the pathophysiological parameters and development direction between both groups, which compensate for inadequate in clinical trials. In addition, we analysed the degree of emphysema in terms of pathology and iconography. Image analysis software was used to analyse the degree of emphysema and to improve the accuracy of inter-group pairing. Considering the influence of systemic system on body fluids such as blood and sputum, we selected lung tissue as the experimental specimen to reflect the pathogenesis of emphysema in lungs. For the question of whether emphysematous patients with normal spirometry are really “disease-free” and “no treatment required”, we answered this question from a new perspective other than clinical research.
As COPD is not an indication for lobectomy, we strictly followed the criterion that only normal tissue located at more than 5 cm from the lesion site can be collected34,35. We performed strict inter-group matching in both groups to minimize the impact of the underlying disease on the experimental results. More than two respiratory physicians participated in history taking of the subjects to ensure the accuracy and credibility of the data.
This study has several limitations. Firstly, only 24 patients were included in the study because of the strict inclusion criteria and inter-group matching. Secondly, oxidative stress results may have been affected as the specimens were collected over 2 years for this study. In the future, the sample size may be increased to improve the accuracy of results. In addition, a recently published study confirmed that smoking-induced humoral immune mechanisms are involved in lung parenchymal damage, and B-cell may play an important role in the formation of emphysema. Therefore, relevant indicators should be considered in future experiments19.
In conclusion, emphysematous smokers that did not have significant airflow limitation showed similar pathophysiological characteristics to emphysematous patients with COPD, confirming the consistency of the pathogenesis and development direction of disease in both groups. Therefore, clinicians should relax the FEV1 criteria for emphysematous smokers with normal spirometry, and not consider them disease-free. In the future, attention must be given to early intervention for emphysematous smokers with normal spirometry to prevent progression of structural destruction, which ultimately affects their quality of life and survival time.
Methods
Subjects
Subjects were screened strictly according to the inclusion criteria and were grouped according to inter-group pairing.
The inclusion criteria were as follows:
(1) age of 40 to 80 years old; (2) a history of 10 or more pack-years of smoking; (3) patients with lung cancer preparing for chest surgery; (4) signed informed consent.
The exclusion criteria were as follows:
(1) bronchial asthma, bronchiectasis, active tuberculosis, or other respiratory diseases; (2) glomerulonephritis, nephrotic syndrome, Ig-A nephropathy, renal failure, or other chronic kidney diseases; (3) autoimmune liver disease, acute or chronic hepatitis, cirrhosis, ulcerative colitis, Crohn’s disease, and other chronic digestive diseases; (4) endocrine system diseases such as diabetes, hyperthyroidism, thyroiditis, or Graves’ disease; (5) various connective tissue diseases; (6) essential hypertension or primary pulmonary hypertension; (7) presence of tumour in the past or present besides lung cancer; (8) tumour had metastasized in lymph nodes or outside the lungs; (9) treated with steroids or other immunosuppressive agents for various reasons; and (10) haemophilia, hereditary spherocytosis, or other genetic diseases.
In order to ensure that the degree of emphysema is consistent between both groups, and reduce tissue heterogeneity caused by underlying diseases and surgical diseases, the following inter-group pairing criteria was implemented to screen specimens:
(1) showed a comparable degree of emphysema in chest CT scans; (2) same gender; (3) age difference of less than 10 years; (4) identical pathological tumour type; (5) similar differentiation degree of tumour; (6) similar position of sampling (accurate to the lobes of lungs); and (7) similar number of smoking pack-years.
Emphysema in chest CT scans was judged by two experienced imaging specialists and the degree of emphysema was validated using CT analysis software23,24. Comprehensive inquiries and spirometry tests using standard spirometric techniques were conducted by two respiratory physicians36.
Patients with COPD were diagnosed for respiratory symptoms, such as cough, sputum, and breathlessness, and those showing an FEV1/FVC ratio of <0.7 after short acting bronchodilator inhaled1. Emphysematous smokers were defined as current smokers with normal spirometry and emphysema detected in CT imaging.
This study was performed in accordance with the Declaration of Helsinki. The protocol for this study was approved by the Ethics Committee of Shengjing Hospital of China Medical University (Shenyang, China; ethical no.2016PS342K). Written informed consent was obtained from each participant prior to obtaining tissue samples and chest CT scans.
Image analysis for assessing the degree of emphysema
Chest CT scans at full inspiration were performed for all subjects using Philips Ingenuity Core 128 CT scanner (Philips, the Best, the Netherlands) or TOSHIBA Aquilion ONE (Toshiba, Tokyo, Japan). All images were acquired with the following parameters: tube voltage, 120 kV; tube current, 180 mA; slice thickness, 3 mm; and reconstruction matrix, 512 × 512. The details regarding CT acquisition parameters are listed in Supplementary Table S1. All patients were scanned craniocaudally in the supine position. Two radiologists performed the radiological measurements. Chest CT raw data sets were obtained from the CT workstation (Neusoft, Shenyang, China) and analyzed using Pulmonary Toolkit (PTK) in Matlab (R2016a) (The MathWorks, Inc., Natick, MA, USA)37. The analysis results were validated by visualization with NeuLungCARE in BW CT workstation (Neusoft, Shenyang, China). We employed a rule that when the CT value of a pixel is less than −950 HU, the software will determine the voxel as emphysema area. The emphysema index was determined as volume fraction of the lungs below −950 HU at full inspiration38,39. Emphysema percentile density was determined as the 15th percentile lung density (PD15) derived from the CT voxel distribution histogram of whole lung40. All CT images were input into the software in the form of raw data, and analysis results were obtained. Data analysis was completed using PTK. Visualization of the degree of emphysema and emphysema distribution were performed using NeuLungCARE.
Pulmonary function test
Spirometry parameters were measured in the subjects using the Medgraphics Platinum Elite DL Plethysmograph (St. Paul, Minneapolis, MN, USA). Pulmonary function tests were conducted by two respiratory physicians, and the results of measurement met the requirement of the American Thoracic Society. In brief, a minimum of three and a maximum of eight tests of lung function were performed for each subject, and there were more than two acceptable tests with repeatability within 150 ml. Acceptable tests were defined as follows: No medications in the past 24 h, subject exhaled quickly without hesitation, and showed explosive power. A good start of exhalation with extrapolated volume was defined as <5% of FVC or 150 ml, whichever was greater. The expiratory time was ≥6 s, and the expiratory platform (volume change <25 ml/s) in the time volume curve appeared for more than 1 s. The best value of FEV1, FVC in spirometry tests of each patient was taken. At an FEV1/FVC ratio <0.7, the subjects were administered with 400 mcg albuterol, reversibility tests were conducted after 15 min.
Preparation of lung tissue specimens
The lung tissues of subjects were prepared as previously described34,35. In brief, lung tissue specimens were excised as far as possible from the tumour (at least 5 cm from the lesion site). The specimens appeared as normal tissue. The location (peripheral tissue extending up to the pleural surface) and amount (~1 cm³) of each sample was standardized to ensure approximately equal amounts of lung parenchyma, small airways, and pulmonary vessels in specimens. After collection, lung tissue specimens were washed with normal saline and dried with sterile gauze to remove residual blood. Specimens were immediately frozen in liquid nitrogen and stored at −80 °C until use.
HE staining
HE staining was conducted according to routine protocols41. Briefly, lung tissues were dissected, fixed in 4% paraformaldehyde, embedded with paraffin after dehydration, and cut into 2.5-µm thick cross-sections. The paraffin-embedded sections were subjected to HE staining to visualize under light microscopy (Nikon, Japan) for lung morphology and Nis-Elements F3.0 (Nikon, Japan) software was used as image acquisition tool. The remaining tissue specimens were quickly frozen in liquid nitrogen for the analysis of protein and RNA expression.
Western blot analysis
Proteins were extracted from lung tissues and quantified using the BCA protein concentration assay kit (Solarbio, China). Equal amounts of protein were resolved on sodium dodecyl sulphate-polyacrylamide gel electrophoresis gels, and transferred to polyvinylidene fluoride membranes. The membranes were blocked with 5% non-fat milk in TBST (10 mM Tris-HCl pH 7.4, 100 mM NaCl, 0.5% Tween-20) for 2 h at room temperature and incubated overnight at 4 °C with primary antibodies. The following primary antibodies were used according to the manufacturer’s protocol: anti-MMP9 (ab76003), anti-TIMP1 (ab109125), and anti-Caspase3 (ab32351) from Abcam (Cambridge, Cambridgeshire, UK); anti-Bax (#2772) from Cell Signaling Technology (Danvers, MA, USA); anti-GAPDH from Proteintech (Chicago, IL,USA); anti-MMP12 (bs-1854R) from Bioss (Beijing, China), Anti-Caspase8(WL02434), anti-Bcl2 (WL01556), and anti-Survivin (WL01684) from Wanleibio (Shenyang, Liaoning, China). The membranes were washed in TBST and incubated with secondary antibodies for 1.5 h. After extensive washing, the membranes were visualized using enhanced chemiluminescence reagent. Final images were analyzed using ImageJ software.
Quantitative reverse transcriptase polymerase chain reaction
Total RNA was extracted from lung tissues using the RNAiso reagent (TaKaRa, Naha, Japan), according to the manufacturer’s protocol. RNA was reverse transcribed to cDNA using the TaKaRa reverse transcription kit. Finally, cDNAs were amplified and detected using the SYBR® Green PCR Kit (Takara, Naha, Japan) with a Roche 480 Real-Time PCR System (Roche, Basel, Switzerland). The amplification parameters were as follows: pre-incubation for 5 min at 95 °C, followed by 40 cycles of initial denaturation at 95 °C for 5 s and annealing at 60 °C for 30 s. Glyceraldehyde phosphate dehydrogenase (GAPDH) was used as reference gene. No signal was detected in the negative control (no template). The following primer sequences were used: IL-6, forward 5′-ACCCCCAATAAATATAGGACTGGA-3′, reverse 5′-GAGAAGGCAACTGGACCGAA-3′; IL-10, forward 5′-CAGAAGTACCTGAGCTCGCC-3′, reverse 5′-AGATTCGTAGCTGGATGCCG-3′; IL-1β, forward 5′-GCCAGTGAAATGATGGCTTATT-3′, reverse 5′-AGGAGCACTTCATCTGTTTAGG-3′; TNF-α, forward 5′-GCTGCACTTTGGAGTGATCG-3′, reverse 5′-TCACTCGGGGTTCGAGAAGA-3′; and GAPDH, forward 5′-CCTGGTATGACAACGAATTTG-3′, reverse 5′-CAGTGAGGGTCTCTCTCTTCC-3′.
Measurement of glutathione (GSH) and superoxide dismutase (SOD) levels
Total GSH and reduced GSH levels and SOD activity were measured using oxidative stress assay kits (Jiancheng, Nanjing, China), according to the manufacturer’s protocol.
Statistical analysis
Statistical analyses were performed using SPSS 22.0 software (SPSS, Inc., Chicago, IL, USA) and GraphPad Prism 7 (GraphPad, La Jolla, CA, USA). Data of continuous variables were expressed as the mean ± standard error of mean. The Student’s t-test was used to compare means between groups of data with normal distribution, and the Mann-Whitney U test was used to compare means between groups of data with non-normal distribution. Fisher’s exact probability was used to compare data of categorical variables. P < 0.05 was considered statistically significant.
Data availability
The datasets used during the current study are available from the corresponding author on reasonable request.
References
Vogelmeier, C. F. et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 Report. GOLD executive summary. Am. J. Respir. Crit. Care Med 195, 557–582, https://doi.org/10.1164/rccm.201701-0218PP (2017).
Mohamed Hoesein, F. A. et al. CT-quantified emphysema in male heavy smokers: association with lung function decline. Thorax 66, 782–787, https://doi.org/10.1136/thx.2010.145995 (2011).
Qaseem, A. et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann. Intern. Med. 155, 179–191, https://doi.org/10.7326/0003-4819-155-3-201108020-00008 (2011).
Jetmalani, K. et al. Peripheral airway dysfunction and relationship with symptoms in smokers with preserved spirometry. Respirology 23, 512–518, https://doi.org/10.1111/resp.13215 (2018).
Regan, E. A. et al. Clinical and radiologic disease in smokers with normal spirometry. JAMA Intern. Med. 175, 1539–1549, https://doi.org/10.1001/jamainternmed.2015.2735 (2015).
Vestbo, J. et al. Should we view chronic obstructive pulmonary disease differently after ECLIPSE? A clinical perspective from the study team. Am. J. Respir. Crit. Care Med. 189, 1022–1030, https://doi.org/10.1164/rccm.201311-2006PP (2014).
Oelsner, E. C. et al. Association between emphysema-like lung on cardiac computed tomography and mortality in persons without airflow obstruction: a cohort study. Ann. Intern. Med. 161, 863–873, https://doi.org/10.7326/m13-2570 (2014).
McAllister, D. A. et al. Emphysema predicts hospitalisation and incident airflow obstruction among older smokers: a prospective cohort study. PLoS One 9, e93221, https://doi.org/10.1371/journal.pone.0093221 (2014).
Koo, H. K., Hong, Y., Lim, M. N., Yim, J. J. & Kim, W. J. Relationship between plasma matrix metalloproteinase levels, pulmonary function, bronchodilator response, and emphysema severity. Int. J. Chron. Obstruct. Pulmon. Dis. 11, 1129–1137, https://doi.org/10.2147/copd.s103281 (2016).
Agusti, A. et al. Characterisation of COPD heterogeneity in the ECLIPSE cohort. Respir. Res. 11, 122, https://doi.org/10.1186/1465-9921-11-122 (2010).
Wille, M. M. et al. Emphysema progression is visually detectable in low-dose CT in continuous but not in former smokers. Eur. Radiol. 24, 2692–2699, https://doi.org/10.1007/s00330-014-3294-7 (2014).
Castaldi, P. J. et al. Cluster analysis in the COPDGene study identifies subtypes of smokers with distinct patterns of airway disease and emphysema. Thorax 69, 415–422, https://doi.org/10.1136/thoraxjnl-2013-203601 (2014).
Ziegler-Heitbrock, L. et al. The EvA study: aims and strategy. Eur. Respir. J. 40, 823–829, https://doi.org/10.1183/09031936.00142811 (2012).
Smith, B. M. et al. Impaired left ventricular filling in COPD and emphysema: is it the heart or the lungs? The multi-ethnic study of atherosclerosis COPD study. Chest 144, 1143–1151, https://doi.org/10.1378/chest.13-0183 (2013).
Castaldi, P. J. et al. Distinct quantitative computed tomography emphysema patterns are associated with physiology and function in smokers. Am. J. Respir. Crit. Care Med. 188, 1083–1090, https://doi.org/10.1164/rccm.201305-0873OC (2013).
Sheen, S. et al. Unique features of non-obstructive emphysema and pure airway obstruction. Int. J. Tuberc. Lung Dis. 18, 109–116, https://doi.org/10.5588/ijtld.13.0258 (2014).
Lindberg, A., Bjerg, A., Ronmark, E., Larsson, L. G. & Lundback, B. Prevalence and underdiagnosis of COPD by disease severity and the attributable fraction of smoking report from the obstructive lung disease in Northern Sweden studies. Respir. Med. 100, 264–272, https://doi.org/10.1016/j.rmed.2005.04.029 (2006).
Johannessen, A. et al. Mortality by level of emphysema and airway wall thickness. Am. J. Respir. Crit. Care Med. 187, 602–608, https://doi.org/10.1164/rccm.201209-1722OC (2013).
Sullivan, J. L. et al. B cell adaptive immune profile in emphysema-predominant COPD. Am. J. Respir. Crit. Care Med., https://doi.org/10.1164/rccm.201903-0632LE (2019).
Woodruff, P. G. et al. Clinical significance of symptoms in smokers with preserved pulmonary function. N. Engl. J. Med. 374, 1811–1821, https://doi.org/10.1056/NEJMoa1505971 (2016).
Soriano, J. B., Polverino, F. & Cosio, B. G. What is early COPD and why is it important? Eur. Respir. J. 52, https://doi.org/10.1183/13993003.01448-2018 (2018).
Barnes, P. J. et al. Current controversies in chronic obstructive pulmonary disease. A report from the Global Initiative for Chronic Obstructive Lung Disease Scientific Committee. Ann. Am. Thorac. Soc. 16, 29–39, https://doi.org/10.1513/AnnalsATS.201808-557PS (2019).
Subramanian, D. R. et al. Emphysema- and airway-dominant COPD phenotypes defined by standardised quantitative computed tomography. Eur. Respir. J. 48, 92–103, https://doi.org/10.1183/13993003.01878-2015 (2016).
Lee, J. H. et al. Responses to inhaled long-acting beta-agonist and corticosteroid according to COPD subtype. Respir. Med. 104, 542–549, https://doi.org/10.1016/j.rmed.2009.10.024 (2010).
Al-Kassimi, F. A. et al. Can computed tomography and carbon monoxide transfer coefficient diagnose an asthma-like phenotype in COPD? Respirology 22, 322–328, https://doi.org/10.1111/resp.12902 (2017).
Bade, G. et al. Serum cytokine profiling and enrichment analysis reveal the involvement of immunological and inflammatory pathways in stable patients with chronic obstructive pulmonary disease. Int. J. Chron. Obstruct. Pulmon. Dis. 9, 759–773, https://doi.org/10.2147/copd.s61347 (2014).
Genschmer, K. R. et al. Activated PMN Exosomes: Pathogenic Entities Causing Matrix Destruction and Disease in the Lung. Cell 176, 113–126.e115, https://doi.org/10.1016/j.cell.2018.12.002 (2019).
Betsuyaku, T., Takeyabu, K., Tanino, M. & Nishimura, M. Role of secretory leukocyte protease inhibitor in the development of subclinical emphysema. Eur Respir J 19, 1051–1057, https://doi.org/10.1183/09031936.02.00253202 (2002).
Liu, T. et al. Activation of dual apoptotic pathways in human melanocytes and protection by survivin. J. Invest. Dermatol. 126, 2247–2256, https://doi.org/10.1038/sj.jid.5700381 (2006).
Samuel, J., Kanwar, R. K., Kanwar, J. R., Khetan, V. & Krishnakumar, S. A study of gene expression of survivin, its antiapoptotic variants, and targeting survivin in vitro for therapy in retinoblastoma. J. Pediatr. Hematol. Oncol. 38, e230–e242, https://doi.org/10.1097/mph.0000000000000605 (2016).
Fischer, B. M., Pavlisko, E. & Voynow, J. A. Pathogenic triad in COPD: oxidative stress, protease-antiprotease imbalance, and inflammation. Int. J. Chron. Obstruct. Pulmon. Dis. 6, 413–421, https://doi.org/10.2147/copd.s10770 (2011).
Kirby, M. et al. On the role of abnormal DL(CO) in ex-smokers without airflow limitation: symptoms, exercise capacity and hyperpolarised helium-3 MRI. Thorax 68, 752–759, https://doi.org/10.1136/thoraxjnl-2012-203108 (2013).
McDonough, J. E. et al. Small-airway obstruction and emphysema in chronic obstructive pulmonary disease. N. Engl. J. Med. 365, 1567–1575, https://doi.org/10.1056/NEJMoa1106955 (2011).
Bi, H. et al. Microarray analysis of long non-coding RNAs in COPD lung tissue. Inflamm. Res. 64, 119–126, https://doi.org/10.1007/s00011-014-0790-9 (2015).
Pomerenke, A., Lea, S. R., Herrick, S., Lindsay, M. A. & Singh, D. Characterization of TLR-induced inflammatory responses in COPD and control lung tissue explants. Int. J. Chron. Obstruct. Pulmon. Dis. 11, 2409–2417, https://doi.org/10.2147/copd.s105156 (2016).
Miller, M. R. et al. Standardisation of spirometry. Eur. Respir. J. 26, 319–338, https://doi.org/10.1183/09031936.05.00034805 (2005).
Arns, A. et al. Towards clinical implementation of ultrafast combined kV-MV CBCT for IGRT of lung cancer: Evaluation of registration accuracy based on phantom study. Strahlenther. Onkol. 192, 312–321, https://doi.org/10.1007/s00066-016-0947-2 (2016).
Coxson, H. O., Leipsic, J., Parraga, G. & Sin, D. D. Using pulmonary imaging to move chronic obstructive pulmonary disease beyond FEV1. Am. J. Respir. Crit. Care Med. 190, 135–144, https://doi.org/10.1164/rccm.201402-0256PP (2014).
Camp, P. G. et al. Sex differences in emphysema and airway disease in smokers. Chest 136, 1480–1488, https://doi.org/10.1378/chest.09-0676 (2009).
Dirksen, A. et al. Exploring the role of CT densitometry: a randomised study of augmentation therapy in alpha1-antitrypsin deficiency. Eur. Respir. J. 33, 1345–1353, https://doi.org/10.1183/09031936.00159408 (2009).
Gao, S. et al. Evaluation of decalcification techniques for rat femurs using HE and immunohistochemical staining. Biomed. Res. Int. 2017, 9050754, https://doi.org/10.1155/2017/9050754 (2017).
Acknowledgements
The authors would like to thank the Biological Sample Library of Shengjing Hospital for help of getting tissue samples. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
S.B. and L.Z. substantially contributed to the conception and design of the manuscript. S.B., R.Y., C.W., P.S. and L.Z. contributed to the acquisition, analysis, and interpretation of data. S.B. and L.Z. drafted the article, and all authors have revised it critically and substantially. S.B., R.Y., C.W., P.S. and L.Z. have approved the final version and accepted accountability for all aspects of the study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bai, S., Ye, R., Wang, C. et al. Comparative analysis of pathophysiological parameters between emphysematous smokers and emphysematous patients with COPD. Sci Rep 10, 420 (2020). https://doi.org/10.1038/s41598-019-57354-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-57354-2
This article is cited by
-
Recent evidence from omic analysis for redox signalling and mitochondrial oxidative stress in COPD
Journal of Inflammation (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.