Abstract
Diagnosing stroke in patients experiencing dizziness without neurological deficits is challenging for physicians. The aim of this study was to evaluate the prevalence of acute stroke in patients who presented with isolated dizziness without neurological deficits at the emergency department (ED), and determine the relevant stroke predictors in this population. This was an observational, retrospective record review of consecutive 2215 adult patients presenting with dizziness at the ED between August 2019 and February 2020. Multivariate analysis was performed to identify risk factors for acute stroke. 1239 patients were enrolled and analyzed. Acute stroke was identified in 55 of 1239 patients (4.5%); most cases (96.3%) presented as ischemic stroke with frequent involvement (29.1%) of the cerebellum. In the multivariate analysis, the history of cerebrovascular injury (odds ratio [OR] 3.08 [95% confidence interval {CI} 1.24 to 7.67]) and an age of > 65 years (OR 3.01 [95% CI 1.33 to 6.83]) were the independent risk factors for predicting acute stroke. The combination of these two risks showed a higher specificity (94.26%) than that of each factor alone. High-risk patients, such as those aged over 65 years or with a history of cerebrovascular injury, may require further neuroimaging workup in the ED to rule out stroke.
Similar content being viewed by others
Introduction
Patients experiencing dizziness commonly present at the emergency department (ED), accounting for roughly 5% of total visits1. Only a small portion of these ED cases are related to dangerous cardiovascular or cerebrovascular injury2. Acute dizziness is most often caused by benign otovestibular origins, including benign paroxysmal positional vertigo, vestibular neuritis, and Ménière's disease; however, it has also been implemented in the onset of stroke. Stroke is commonly misdiagnosed, noted as the fourth most common diagnostic error reported by physicians. Failure to recognize acute stroke may result in worse patient outcomes due to missed opportunity for acute stroke therapies3. Stroke diagnosis is particularly challenging in patients experiencing dizziness who have presented to the ED without neurologic deficits. There is evidence from previous research that roughly only 20% of patients diagnosed with acute stroke had focal neurologic abnormalities, and the frequency of misdiagnosis for stroke was up to 13%4,5,6. Clinical tools can help to reduce the risk of stroke misdiagnosis, examples of these include diffusion-weighted imaging (DWI) and magnetic resonance imaging (MRI) as the gold standard.
MRI can be useful in the exclusion of the central origin of dizziness in these patients; however, controversy exists on whether immediate requirement of MRI in the ED is necessary for patients presenting solely with dizziness because of the associated cost and limited access7. Although previous studies have reported some predictors and physical examinations (e.g. HINTS) for medical decision making, they were limited by their small sample size, performed MRI for patients with definite neurologic deficits, or did not include detailed medical records or conduct physical exams8. Given the large number of patients with dizziness presenting to the ED, further study to identify the predictors related to stroke will be needed in this population. The objective of this study was to evaluate the incidence of patients with dizziness without definite neurologic signs, and identify the relevant risk factors.
Results
Study population and baseline characteristics
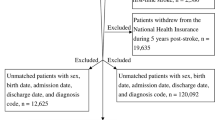
During the study period, 2215 adult patients presenting with dizziness visited the ED. After excluding 456 patients with confirmed neurologic deficits, 203 patients were evaluated and diagnosed with confirmed clinical dizziness induced by, for example, anemia, hypoglycemia, shock, and electrolyte imbalance; 305 patients did not have MRI data, and 9 patients were contraindicated for MRI. The remaining 1239 cases were enrolled in the final analysis (Fig. 1). Of these, about 4.5% (55/1239) of patients were diagnosed with acute stroke. The median age of this population was 64.0 years (IQR 56.0–72.0) and 537 patients (43.3%) were male.
Baseline characteristics were compared, with patients categorized as either ‘patients with acute stroke’ or ‘normal’ (Table 1). Patients with acute stroke were older (64.0 vs. 71.5 years, p < 0.01), but sex preponderance was not identified. Patients with hypertension and atrial fibrillation were shown to have an increased risk of stroke compared with those without (56.4% vs. 42.2%, respectively, p = 0.04; 12.7% vs. 4.4%, respectively, p < 0.01), along with other comorbidities. Patients with a history of cerebrovascular injury were shown to be significantly associated with an increased risk of stroke compared with patients without (21.8% vs. 7.8%, p < 0.01). Medical use of anti-platelet or anti-coagulation agents had no significant impact on patient risk of stroke. With regard to characteristics of dizziness, dizziness with non-whirling quality (47.7 vs 63.6%, p = 0.02) and irrelevant to head movement (56.3 vs 72.7%, p = 0.02) was associated with acute stroke, but not other symptoms. Duration of symptoms were shown to not be significantly associated with the risk of acute stroke. Laboratory results (Table 2) showed that patients diagnosed with acute stroke had increased serum glucose levels compared with those who were not (136.5 vs. 123.0 mg/dL, respectively; p = 0.05). Creatinine levels between the two patient groups were similar (0.8 vs. 0.8 mg/dL, p = 0.01).
The etiology based on Trial of ORG10172 in Acute Stroke Treatment (TOAST) classification, frequencies of vascular territories, and brain lesions are presented in Table 3. Of the total 55 patients, 52 (96.3%) experienced ischemic stroke. Large artery atherosclerosis was the most common subtype (40.8%), and vertebrobasilar artery (21.2%) was the most frequently involved culprit artery, followed by the middle cerebral artery (7.7%). The cerebellum was the most frequent brain lesion in acute stroke patients with isolated dizziness (29.1%), followed by pons (10.9%), and the frontal lobe (9.1%).
Risk factors for acute stroke
The results of our univariable and multivariable logistic regression analyses to explore and identify risk factors for acute stroke in patients with dizziness are presented in Table 4. A history of hypertension (OR 1.77; CI 1.02 to 3.05, p = 0.04), atrial fibrillation (OR 3.18; CI 1.37 to 7.36, p < 0.01), cerebrovascular injury (OR 3.31; CI 1.69 to 6.50, p < 0.01), non-whirling type vertigo (OR 1.92; CI 1.09 to 3.36, p = 0.02), dizziness irrespective of head movement (OR 2.07; CI 1.13 to 3.79, p = 0.02), and age above 65 years (OR 2.68; CI 1.48 to 4.85, p < 0.01) were all factors associated with acute stroke in univariable logistic regression. A history of cerebrovascular injury (OR 3.08; CI 1.24 to 7.67, p = 0.02), and age above 65 years (OR 3.01; CI 1.33 to 6.83, p < 0.01) were the significant independent risk factors for predicting acute stroke in the multivariable logistic regression model.
The evaluation of diagnostic values of identified risk factors for acute stroke is presented in Table 5. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (PLR) and negative likelihood ratio (NLR) of each risk factors were calculated. As predictive values for absence of acute stroke, history of without cerebrovascular injury showed high sensitivity of 78.18% but low specificity of 7.77%. Conversely, an age of under 65 years showed a sensitivity value of 36.36% and specificity value of 41.13%, which corresponds to a PPV and NPV of 2.79% and 93.30%, respectively. When the two risk factors were evaluated in combination, sensitivity performed better as a predictive factor (85.55%).
Discussion
In this study, acute stroke was found in 55 of 1239 patients (4.5%) who presented with dizziness without confirmed neurologic deficits, and most cases (96.3%) were diagnosed as ischemic stroke with a high rate of cerebellum involvement. Although symptom characteristics and laboratory examinations could not be helpful to determine whether further neuroimaging workup was required, an age of over 65 (OR 3.01; 95% CI 1.33 to 6.83) and a previous history of cerebrovascular injury (OR 3.08; 95% CI 1.24 to 7.67) were independent risk factors for onset of acute stroke in this patient population.
Differentiating central from peripheral origins in dizziness is frequently challenging for physicians. In the past, isolated dizziness was considered as a peripheral origin disorder, meaning that patients experiencing this symptom had been excluded from most previous studies on acute stroke research9. On the contrary, there is a growing body of evidence to suggest that this isolated symptom is in fact caused by a central origin10,11,12. A retrospective study by Navi et al. reported that 37 of 907 (4.1%) patients who presented with dizziness also had cerebrovascular injury12. These data are similar with the data reported in this study (4.5%); however, Navi et al. included all patients with dizziness, irrespective of confirmed neurologic symptoms. Moreover, they found only two patients with isolated dizziness who were diagnosed with stroke and were limited by performing neuroimaging on only 37% of patients. A recent, small retrospective study reported that the incidence of stroke in admitted patients with isolated vertigo was about 11% (25/103) and was higher than in the present study. However, the smaller sample sizes of patients whom underwent MRI make it difficult to quantify the true incidence of stroke in these patients without neurologic deficits.
In this study, most cases of acute stroke were ischemic, and hemorrhage was relatively rare. Among 3 patients with hemorrhage, only 1 patient presented with dizziness without a headache, and the remainder suffered from a headache combined with moderately high systolic blood pressure (above 180 mmHg) at initial presentation. Large cohorts or systematic studies reporting on vertigo caused by hemorrhage do not appear to exist in the literature13,14, implying that patients with isolated dizziness were considerably less likely to have a primary intracranial hemorrhage. We also found that large artery atherosclerosis was the most frequent classification followed by small vessel occlusion and embolic origin according to the TOAST criteria. The incidence rates of each subtype were different compared with a past population-based epidemiological study15, which may be a result of the varying distribution of risk factors, including hypertension, diabetes, smoking rates, and a history of cardiac disease. However, because outcome data could be not collected, the differences in survival or recurrence rate according to each subtype could not be confirmed. Nevertheless, our findings confirmed the findings of the previous analysis that the cerebellum was the predominant site of ischemic stroke16. Additional brain sites affected included the frontal lobe, pons, and parietal lobe; these results added to the recent knowledge that dizziness as a symptom alone could not exclude the occurrence of stroke17.
We did not find any statistical differences between symptom characteristics and associated presentations. Although non-whirling type dizziness and irrelevance to head positioning appeared to be more prevalent in patients with stroke, these differences were not detected in the multivariate analysis. These results reflect those of the previous study that the effectiveness of symptom assessment in regard to patients with dizziness may be predisposed to under-evaluation of high-risk patients18. Numerous bedside oculomotor and neurologic examinations, such as Dix-Hallpike, head thrust, and HINTS +, would be a useful method for predicting a serious neurologic disease19. Alternatively, the results of these examinations tended to be reliable when patients were examined by trained neuro-ophthalmologists, and the consultations to the neurologists for all patients with dizziness may not be available in most clinical fields. Furthermore, we investigated the laboratory results that were usually performed to exclude medical dizziness (e.g., anemia, hypoglycemia, or electrolyte imbalance), and found that none of the data could discriminate the presence of stroke.
The correlation between older patient age and increased risk of stroke, including in patients without confirmed neurologic symptoms, was as predicted. Chase et al. also noted similar findings in their prospective study of patients presenting to the ED20. Nevertheless, other well-known risk factors, including diabetes mellitus, hyperlipidemia, and protective agents, such as aspirin, warfarin, and new oral anticoagulants, showed an association with the development of stroke in this study. Although atrial fibrillation did not appear to independent risk factor of stroke, we did find a trend toward significant association (adjusted OR 2.40, 95% CI 0.82 to 7.01). Traditionally, atrial fibrillation itself increased the risk of stroke events and recurrence by up to 54.0% in a previous study21. In addition, we found that the patients with acute stroke had higher proportion of previous cerebrovascular injury. Interestingly, our study population only included patients who had no long-term neurologic deficit after initial stroke presentation, but the recurrence risk increased compared with in patients without previous history of cerebral infarct. Combination of older age under 65 and without history of stroke had high sensitivity, but low specificity for predicting absence of acute stroke. Hence, patients with dizziness who are aged over 65 years and have a history of cerebrovascular injury should be considered for further neuroimaging tests.
We note several limitations of this study. Firstly, the single-center, retrospective design, has meant that we could not generalize our results to the wider environments. Secondly, patients who did not visit the ED or had no MRI data could have led to selection bias. Thirdly, relatively small sample of the patients with acute strokes might affect sensitivity analysis. In addition, there was no standardized protocol for the making decision of patients with dizziness. Therefore, misdiagnoses or delayed presentation of cerebrovascular injury may not have been detected in this analysis. Lastly, unmeasured confounding variables, such as smoking history, could have influenced the results.
Conclusion
The incidence of acute stroke was 4.5% (n = 55/1239) in patients presenting to the ED with dizziness but without neurological deficits. Given the large number of these patients, it would be necessary to consider further neuroimaging workup in high-risk patients, such as those aged over 65 or those with a history of stroke, in order to rule out acute stroke as the cause.
Materials and methods
Study design and setting
This was a single-center, retrospective, observational study conducted in the ED of Asan Medical Center, an urban tertiary referral hospital in Seoul, Korea. Adult (> 18 years) patients who visited the ED with dizziness or related symptoms (e.g., vertigo, lightheadedness, disequilibrium, or gait instability) as the chief affliction between 1 August 2019 and 29 February 2020 were evaluated. The ED of the study facility is staffed 24 h a day by attending emergency medicine physicians and residents. Neurology consultants and neuroimaging facilities (brain computed tomography, MRI) are accessible around-the-clock. Patients who had triage complaints of dizziness were routinely evaluated with systemic history documentation, physical and neurologic examinations, and further laboratory tests; the necessity of follow-up neuroimaging examinations was determined by the primary emergency medicine physician on duty. All experiments were carried out in agreement with relevant described guidelines and regulations. This study was approved by the Research Ethics Committee of Asan Medical Center (no. 2020-0179) which waived the requirement for patient informed consent.
Study population and variables
Electronic medical records were reviewed by trained researchers (H.J.B., and J.S.K.) and all eligible adult patients with isolated dizziness or vertigo were included in the study. Exclusion criteria included patients with confirmed neurologic deficits at presentation, including hemiparesis, hemiplegia, dysarthria, facial droop, and a Glasgow Coma Scale score of less than 13; patients with dizziness as a result of external clinical factors (e.g., hypoglycemia, shock, symptomatic bradycardia, sepsis, or intoxication); and those without MRI data.
In all confirmed cases of acute ischemic stroke, magnetic resonance angiography was performed for evaluation of vascular abnormality. MRI scans were interpreted by qualified radiologists, and associations between the ischemic territory and culprit artery were also investigated. Old ischemic lesions were not considered to be acute central lesions relevant to the current case of stroke. The etiology of acute stroke was evaluated by experienced neurologists on duty by use of TOAST criteria22. Notes on vascular territory and TOAST criteria were also extracted from medical records.
DWI (5 mm slice thickness, an interslice gap of 2 mm, 20 axial slices, and a field of view of 250 mm) was performed on a 1.5 T MRI unit with echoplanar capability (Signa CV/i; GE Medical Systems, Milwaukee, Wisconsin, USA). DWI parameters included a repetition time of 7500 ms, an echo time of 84 ms, a matrix number of 128 × 128, and a b value of 1000 s/mm2.
Data collected for the patients in our study included demographics, underlying medical illnesses, any current use of anti-platelet or anti-coagulation agents, characteristics of dizziness and associated symptoms including headache, nausea, vomiting, and tinnitus. Because of the retrospective design, we did not have a standardized case report form. However, the electronic medical records included information about demographics, underlying medical illnesses, and routine medications. Moreover, experienced primary physicians on duty or neurologists were well-trained in routinely recording characteristics of dizziness and associated symptoms for patients with dizziness in medical charts. Laboratory data were also collected for analysis, including white blood cell counts, hemoglobin, glucose, blood urea nitrogen, creatinine, and electrolyte profile.
Statistical analysis
The continuous variables in the baseline demographics, clinical characteristics, and laboratory data were presented as medians with interquartile range (IQR) and as frequencies with percentages. The Kolmogorov–Smirnov test was used to validate the normality of distribution, and the Mann–Whitney U test was performed. Categorical variables were assessed using the chi-squared test or Fisher’s exact test, as appropriate. A stepwise multivariate logistic regression analysis was employed to identify risk factors that are predictive of acute stroke in patients experiencing dizziness. Variables with p values of less than 0.1 in univariable analyses were selected for the multivariable analysis. Cut-off values for continuous variables, including age and serum creatinine levels, were determined by use of the Youden index (sensitivity + specificity − 1), with a receiver operating characteristic curve. Sensitivity and specificity were calculated by use of the standard statistical method. p values lower than 0.05 were considered to indicate statistical significance in this study. All statistical analyses were performed using SPSS Statistics for Windows, version 26.0 (IBM Corp., Armonk, NY).
References
Ljunggren, M., Persson, J. & Salzer, J. Dizziness and the acute vestibular syndrome at the emergency department: A population-based descriptive study. Eur. Neurol. 79, 5–12 (2018).
Neuhauser, H. K. et al. Burden of dizziness and vertigo in the community. Arch. Intern. Med. 168, 2118–2124 (2008).
Schiff, G. D. et al. Diagnostic error in medicine: analysis of 583 physician-reported errors. Arch. Intern. Med 169, 1881–1887 (2009).
Newman-Toker, D. E., Moy, E., Valente, E., Coffey, R. & Hines, A. L. Missed diagnosis of stroke in the emergency department: A cross-sectional analysis of a large population-based sample. Diagnosis (Berl) 1, 155–166 (2014).
Newman-Toker, D. E. et al. Spectrum of dizziness visits to US emergency departments: cross-sectional analysis from a nationally representative sample. Mayo Clin. Proc. 83, 765–775 (2008).
Tarnutzer, A. A. et al. ED misdiagnosis of cerebrovascular events in the era of modern neuroimaging: A meta-analysis. Neurology 88, 1468–1477 (2017).
Saber Tehrani, A. S. et al. Rising annual costs of dizziness presentations to U.S. emergency departments. Acad. Emerg. Med. 20, 689–696 (2013).
Cheung, C. S. et al. Predictors of important neurological causes of dizziness among patients presenting to the emergency department. Emerg. Med. J 27, 517–521 (2010).
Caplan, L. R. Stroke classification: A personal view. Stroke 42, S3-6 (2011).
Lee, H. Isolated vascular vertigo. SJ. Stroke 16, 124–130 (2014).
Lee, H. et al. Cerebellar infarction presenting isolated vertigo: Frequency and vascular topographical patterns. Neurology 67, 1178–1183 (2006).
Navi, B. B. et al. Rate and predictors of serious neurologic causes of dizziness in the emergency department. Mayo Clin. Proc. 87, 1080–1088 (2012).
Kerber, K. A. et al. Does intracerebral haemorrhage mimic benign dizziness presentations? A population based study. Emerg. Med. J. 29, 43–46 (2012).
Armato, E., Ferri, E., Pinzani, A. & Ulmer, E. Cerebellar haemorrhage mimicking acute peripheral vestibulopathy: The role of the video head impulse test in differential diagnosis. Acta Otorhinolaryngol. Ital. 34, 288–291 (2014).
Kolominsky-Rabas, P. L., Weber, M., Gefeller, O., Neundoerfer, B. & Heuschmann, P. U. Epidemiology of ischemic stroke subtypes according to TOAST criteria: Incidence, recurrence, and long-term survival in ischemic stroke subtypes: A population-based study. Stroke 32, 2735–2740 (2001).
Doijiri, R., Uno, H., Miyashita, K., Ihara, M. & Nagatsuka, K. How commonly is stroke found in patients with isolated vertigo or dizziness attack?. J. Stroke Cerebrovasc. Dis. 25, 2549–2552 (2016).
Saber Tehrani, A. S. et al. Small strokes causing severe vertigo: Frequency of false-negative MRIs and nonlacunar mechanisms. Neurology 83, 169–173 (2014).
Stanton, V. A. et al. Overreliance on symptom quality in diagnosing dizziness: Results of a multicenter survey of emergency physicians. Mayo Clin. Proc. 82, 1319–1328 (2007).
Chase, M. et al. ED patients with vertigo: Can we identify clinical factors associated with acute stroke?. Am. J. Emerg. Med. 30, 587–591 (2012).
Chase, M. et al. A prospective pilot study of predictors of acute stroke in emergency department patients with dizziness. Mayo Clin. Proc. 89, 173–180 (2014).
Flach, C., Muruet, W., Wolfe, C. D. A., Bhalla, A. & Douiri, A. Risk and secondary prevention of stroke recurrence: A population-base cohort study. Stroke 51, 2435–2444 (2020).
Adams, H. P. Jr. et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24, 35–41 (1993).
Author information
Authors and Affiliations
Contributions
Conceptualization, W.Y.K.; Methodology, M.Y.K. and S.A.; Data curation, J.S.K. and H.J.B.; Writing—Original Draft Preparation, J.S.K. and H.J.B.; Writing—review & editing, C.H.S. and D.W.S.; Supervision, W.Y.K.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, Js., Bae, H.J., Kim, M. et al. Stroke prediction in patients presenting with isolated dizziness in the emergency department. Sci Rep 11, 6114 (2021). https://doi.org/10.1038/s41598-021-85725-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-85725-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.