Abstract
Sepsis is a systemic reaction to an infection and resulting in excessive production of inflammatory cytokines and chemokines. It sometimes results in septic shock. The present study aimed to identify quinolone antibiotics that can reduce tumor necrosis factor alpha (TNFα) production and to elucidate mechanisms underlying inhibition of TNFα production. We identified quinolone antibiotics reduced TNFα production in lipopolysaccharide (LPS)-stimulated THP-1 cells. Sitafloxacin (STFX) is a broad-spectrum antibiotic of the quinolone class. STFX effectively suppressed TNFα production in LPS-stimulated THP-1 cells in a dose-dependent manner and increased extracellular signal-regulated kinase (ERK) phosphorylation. The percentage of intracellular TNFα increased in LPS-stimulated cells with STFX compared with that in LPS-stimulated cells. TNFα converting enzyme (TACE) released TNFα from the cells, and STFX suppressed TACE phosphorylation and activity. To conclude, one of the mechanisms underlying inhibition of TNFα production in LPS-stimulated THP-1 cells treated with STFX is the inhibition of TNFα release from cells via the suppression of TACE phosphorylation and activity. STFX may kill bacteria and suppress inflammation. Therefore, it can be effective for sepsis treatment.
Similar content being viewed by others
Introduction
Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection1. Sepsis was first defined as sepsis-1 in 1991 and was redefined as sepsis-3 in 2016. Sepsis was further defined as a systemic inflammatory response syndrome caused by infection2. Particularly during gram-negative bacterial infection, lipopolysaccharide (LPS) stimulates cells to produce inflammatory cytokines and chemokines, which can sometimes result in septic shock. Inflammatory cytokines lower the blood pressure via blood vessels dilation and blood clotting within the capillaries of organs. These effects can aid the immune system in fighting infection, but can also be harmful. Thus, drugs that are not only effective against bacterial infections but also reduce inflammatory cytokines are required to avoid such harmful effects.
Treatment with such drugs may help prevent septic shock and reduce mortality. Some antibiotics such as tetracycline3,4, macrolide5,6,7 and oxazolidinone8,9 have effectively reduced the production of inflammatory cytokines.
Quinolones such as garenoxacin or moxifloxacin have also been reported to reduce inflammatory cytokines10,11.
Sitafloxacin (STFX) is a broad-spectrum antimicrobial agent12. STFX is effective against pneumococcal infections, and incidence of drug-resistant mutants is low in vitro conditions13. STFX was effective against Haemophilus influenzae pneumonia in a murine model14.
In a clinical study, STFX was also proven effective and safe in elderly patients with pneumonia including aspiration pneumonia in nursing homes15. STFX treatment was effective in patients with both acute complicated urinary tract infection and pyelonephritis caused by Escherichia coli producing extended-spectrum beta-lactamase (ESBL)16. Another study also reported that STFX was effective against the E. coli producing ESBL following 3 days of carbapenem therapy17.
STFX, a broad-spectrum oral fluoroquinolone, has been approved in Japan for the treatment of respiratory and urinary tract infections. However, whether STFX can be used for treating patients with sepsis or whether it suppresses the production of inflammatory cytokines and chemokines is unknown, which we aimed to determine in the present study.
Results
Tumor necrosis factor alpha (TNFα concentration was high in supernatants of 4 h LPS-stimulated THP-1 cells
TNFα concentration in the supernatants of THP-1 cells stimulated by LPS for 4 h, 12 h, 24 h or 48 h was 1135.21 ± 116.24 pg/mL, 1180.39 ± 148.17 pg/mL, 1078.65 ± 143.12 pg/mL, or 1116.81 ± 89.16 pg/mL, respectively (Fig. 1). TNFα concentration at 4 h was not significantly lower than that at 12 h, 24 h, or 48 h.
STFX inhibited TNFα production significantly compared with other quinolones
We examined which quinolones can inhibit TNFα production by determining of TNFα concentration in the supernatant of LPS-stimulated THP-1 cells treated with 50 µg/mL quinolone antibiotics. TNFα concentrations in these supernatants after moxifloxacin (MFLX), levofloxacin (LVFX), garenoxacin (GRNX), ciprofloxacin (CPFX) and STFX treatment were 1007.81 ± 79.92 pg/mL, 932.73 ± 99.14 pg/mL, 747.19 ± 27.76 pg/mL, 613.90 ± 67.56 pg/mL, or 316.90 ± 57.69 pg/mL, respectively. MFLX and LVFX treatments significantly reduced TNFα concentration than LPS treatment alone did (1173.49 ± 162.51 pg/mL) (p < 0.05). GRNX, CPFX, and STFX treatments significantly reduced TNFα concentrations than LPS alone treatment did (control) (p < 0.01). TNFα concentrations following LPS and STFX treatments were significantly lower than those following LPS and MFLX, LVFX, GRNX, or CPFX (p < 0.01), and STFX reduced TNFα concentration the most (Fig. 2).
Sitafloxacin significantly reduced TNFα production. THP-1 cells (2 × 105/mL) were stimulated by LPS (0.1 µg/mL) with several different quinolone antibiotics (50 µg/mL) for 4 h. Data are presented as mean ± SD of 6 independent experiments. *p < 0.05 vs. LPS alone. **p < 0.01 vs. LPS alone. ***p < 0.01 vs. MFLX, LVFX, GRNX, or CPFX. LPS lipopolysaccharide, MFLX moxifloxacin, LVFX levofloxacin, GRNX garenoxacin, CPFX ciprofloxacin, STFX sitafloxacin.
STFX inhibited TNFα production in a dose-dependent manner
Concentrations of TNFα in the supernatants of only LPS-stimulated THP-1 cells was 1057.80 ± 125.80 pg/mL Concentrations of TNFα in the supernatants of LPS-stimulated THP-1 cells in the presence of 1, 10, 30, and 50 µg/mL STFX were 903.26 ± 61.56 pg/mL (p < 0.05 vs. LPS alone), 803.20 ± 64.52 pg/mL (p < 0.01 vs. LPS alone), 622.61 ± 56.64 pg/mL (p < 0.01 vs. LPS alone), and 303.92 ± 63.42 pg/mL (p < 0.01 vs. LPS alone), respectively (Fig. 3).
Sitafloxacin reduced TNFα in a dose-dependent manner. THP-1 cells (2 × 105/mL) were stimulated by LPS (0.1 µg/mL) in the presence of various concentrations of STFX (1, 10, 30, and 50 µg/mL) for 4 h. Data are presented as the mean ± SD of 6 independent experiments. *p < 0.05, **p < 0.01 vs. LPS alone. STFX sitafloxacin.
STFX inhibited the production of chemokines
STFX inhibited not only TNFα production but also chemokines production, as indicated by additional experiments with LPS-stimulated THP-1 cells. The concentration of interleukin-8 (IL-8) in the supernatants of cells treated with 50 µg/mL STFX was significantly decreased to 10,472.00 ± 474.67 pg/mL compared with that of LPS alone (17,802.33 ± 190.07 pg/mL) (p < 0.01) (Fig. 4a). The concentrations of interferon inducible protein (IP-10) in the supernatants of cells treated with 50 µg/mL STFX was significantly decreased to 77.83 ± 9.70 pg/mL compared with that of the cells treated with LPS alone (3649.00 ± 377.59 pg/mL) (p < 0.01) (Fig. 4b). The concentration of monocyte chemoattractant protein-1 (MCP-1) in cell supernatants in the presence of 50 µg/mL STFX was also significantly decreased to 161.67 ± 11.59 pg/mL compared with that of LPS alone (3453.00 ± 148.55 pg/mL) (p < 0.01) (Fig. 4c). Furthermore, macrophage inflammatory protein-1α (MIP-1α concentrations in the supernatants of cells followed by treatment with 50 µg/mL STFX were significantly decreased to 9336.67 ± 206.50 pg/mL compared with that of the cells treated with LPS alone (20,859.33 ± 196.41 p/mL) (p < 0.01) (Fig. 4d). The supernatant concentration of macrophage inflammatory protein-1β (MIP-1β from the cells treated with 50 µg/mL STFX was also significantly decreased to 2844.67 ± 135.43 pg/mL compared with that of the cells treated with LPS alone (12,950.67 ± 409.62 pg/mL) (p < 0.01) (Fig. 4e).
STFX reduced the levels of inflammatory chemokines. THP-1 cells (2 × 105/mL) were stimulated by LPS (0.1 µg/mL) with STFX (50 µg/mL) for 4 h. Concentrations of IL-8 (a), IP-10 (b), MCP-1 (c), MIP-1α (d) and MIP-1β (e) were measured via multiplex bead immunoassays. Data are presented as the mean ± SD of 3 independent experiments. *p < 0.01 vs. LPS alone. IL-8 interleukin-8, IP-10 interferon inducible protein, MCP-1 monocyte chemoattractant protein-1, MIP-1α macrophage inflammatory protein-1α, MIP-1β macrophage inflammatory protein-1β.
The phosphorylated form of extracellular signal-regulated kinase (ERK) increased treated with STFX
THP-1 cells (2 × 105/mL) were stimulated with LPS (0.1 µg/mL) with or without the presence of STFX (50 µg/mL) for 30 min and 60 min. The phosphorylated form of ERK increased after treatment with STFX and LPS compared with treatment with LPS alone. The phosphorylated forms of nuclear factor kappa B (NF-κB) and p38 did not decrease in the cells treated with STFX and LPS compared with those treated with LPS alone (Fig. 5). Supplementary Fig. S1 presents the full-length blot and image (online).
STFX did not inhibit signaling of TNFα production. THP-1 cells (2 × 105/mL) were stimulated by LPS (0.1 µg/mL) with or without STFX (50 µg/mL) for 30 min or 60 min. NF-κB, ERK and p38, and the phosphorylation of NF-κB, ERK and p38 were evaluated by western blotting. The data are representative of 3 independent experiments. NF-κB Nuclear factor-kappa B, ERK extracellular signal-regulated kinase.
STFX inhibited TNFα release from cells
THP-1 cells (2 × 105/mL) were stimulated by LPS (0.1 µg/mL) with or without STFX (50 µg/mL). After 4 h of incubation, intracellular TNFα was stained with anti-TNFα antibody PE. The percentage of intracellular TNFα in the cells treated with STFX and LPS increased from 4.4 to 16.2% compared with that of the cells treated with LPS alone (Fig. 6).
Intracellular TNFα levels increased with STFX. THP-1 cells (2 × 105/mL) were stimulated by LPS (0.1 µg/mL) with or without STFX (50 µg/mL). After 4 h incubation, intracellular TNFα was stained with anti-TNFα antibody PE. The percentage of intracellular TNFα in LPS-stimulated cells in the presence or absence of STFX was evaluated by flow cytometry. The data are representative of 3 independent experiments.
STFX reduced phosphorylation of TNFα converting enzyme (TACE) and TACE activity
THP-1 cells (2 × 105/mL) were stimulated by LPS (0.1 µg/mL) with or without STFX (50 µg/mL) for 30 and 60 min. The phosphorylated form of TACE decreased after STFX and LPS treatment compared with LPS treatment alone. (Fig. 7a). Supplementary Fig. S2 presents the full-length blot and image (online). TACE activity of the cells treated for 60 min with STFX and LPS (244,805.70 ± 27,083.11 RFU/mg Protein) significantly decreased (p < 0.05) compared to TACE activity for 0 min (430,018.30 ± 149,978.40 RFU/mg protein) (Fig. 7b).
STFX reduced TACE phosphorylation and activity. THP-1 cells (2 × 105/mL) were stimulated by LPS (0.1 µg/mL) with or without STFX (50 µg/mL) for 30 min or 60 min. (a) TACE or the phosphorylation of TACE was evaluated by western blotting. The data are representative of 3 independent experiments. (b) THP-1 cells (2 × 105/mL) were stimulated by LPS (0.1 µg/mL) with or without STFX (50 µg/mL) for 30 min or 60 min. TACE activity was evaluated by ELISA. Data are presented the mean ± SD of 6 independent experiments.
Discussion
TNFα plays an important role in sepsis. TNFα blocking protected mice from sepsis symptoms18. Some clinical studies investigating the monoclonal antibodies produced against TNFα in patients with sepsis or septic shock have been reported19,20,21. The modulation of TNFα and other inflammatory cytokines and chemokines is considered important in the treatment of severe infectious diseases, especially sepsis or septic shock.
In the present study, TNFα concentration in the supernatant of LPS-stimulated THP-1 cells for 4 h was not significantly different from that of the cells treated for 12 h, 24 h, or 48 h. Some researchers have cultured THP-1 cells with LPS for 4 h and assessed TNFα concentration in the supernatant4,22. The authors of these papers revealed that TNFα level reached a maximum for 4 h incubation4,22. Therefore, we performed concentration experiments after 4 h of incubation. The concentration of TNFα in the supernatant at 4 h was a result of what happened in the cells earlier. Hence, we evaluated signaling pathway and TACE activity in the cells at 30 and 60 min.
STFX significantly reduced the concentration of TNFα in the supernatants of LPS-stimulated THP-1 cells than other quinolone antibiotics did; STFX also reduced the levels of IL-8, IP-10, MCP-1, MIP-1α and MIP-1β.
Some types of antibiotics can modulate inflammatory cytokines, but the mechanisms of cytokine inhibition may vary. A study has reported that minocycline inhibits IκB kinase α/β phosphorylation of NF-κB pathway in THP-1 cells4. Another study has reported that clarithromycin attenuates STAT6 phosphorylation5. Other studies have reported that macrolide antibiotics inhibited ERK and NF-κB signaling pathways6,7. GRNX and MFLX inhibited these signaling pathways to suppress the production of inflammatory cytokines. GRNX significantly inhibited the transcription and secretion of IL-8 induced by LPS-stimulated THP-1 cells by inhibiting ERK1/2 phosphorylation10. Furthermore, MFLX inhibited ERK1/2, JNK, and NF-κB activation in the cystic fibrosis epithelial cell line11.
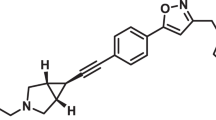
Even when using similar quinolone antibacterial drugs, the mechanism of cytokine suppression differs depending on the characteristics of each drug. Previous studies have reported that quinolones with a cyclopropyl group at the N1 position and/or a piperazinyl group at the C7 position, can regulate inflammatory responses23,24,25. STFX consists of a fluorocyclopropene at the 1-position of the quinolone skeleton, a chlorine group at the 8-position, a spiroheptane group at the 7-position, and a quinolone with a chlorine group introduced at the 8-position. Such characteristics may cause differences in the spectrum of antibacterial activity and may also cause differences in anti-inflammatory effects.
In the present study, STFX suppressed TNFα production more strongly than the other quinolone antibiotics. It did not suppress the signaling pathways that produced TNFα but increased phosphorylated ERK. Flow cytometry analysis suggested that STFX inhibited the extracellular release of TNFα. TACE specifically cleaves pro-TNFα to release TNFα from cells26,27. Our study revealed that STFX reduced the phosphorylation and activity of TACE. One of the mechanisms inhibiting TNFα production by STFX might be interference with TNFα release from cells via the inhibition of TACE activity and phosphorylation but not the inhibition of signaling pathways.
STFX may be an effective drug for patients with bacterial infections because of its antimicrobial action and the simultaneous reduction of TNFα. STFX has been approved as an oral antibacterial drug and can be used to treat patients with sepsis or septic shock.
Methods
Reagents
Roswell Park Memorial Institute (RPMI) 1640 medium and fetal bovine serum (FBS) were purchased from Sigma-Aldrich (St. Louis, MO, USA). MFLX, GRNX and CPFX were purchased from FUJIFILM Wako Pure Chemical Corporation (Osaka, Japan). LVFX and STFX were provided by Daiichi Sankyo Company Limited. These antibiotics were diluted with RPMI 1640 at a concentration of 1.0 mg/mL to use as stock solutions. LPS from Pseudomonas aeruginosa serotype 10 (Sigma-Aldrich) was used to induce inflammatory responses. LPS was dissolved in RPMI 1640 medium at a concentration of 1.0 mg/mL and stored at – 80 °C until use.
Cell culture and exposures
The human monocyte THP-1 cell line was purchased from the RIKEN Cell Bank (Ibaragi, Japan). The cells were cultured in RPMI 1640 medium supplemented with 10% FBS at 37 °C in humidified air with 5% CO2 and only exponentially growing cells were used for experiments. THP-1 cells (2 × 105 cells/mL) were cultured with 0.1 µg/mL of LPS for 4 h, 12 h, 24 h, or 48 h. Data are presented as the mean ± standard deviation (SD) of 6 independent experiments.
THP-1 cells (2 × 105 cells/mL) were cultured with LPS (0.1 µg/mL) in the presence or absence of antibiotics (MFLX, LVFX, GRNX, CPFX, and STFX) for 4 h. Following the incubation, supernatants were collected via centrifugation at 1500 rpm for 2 min at room temperature and stored at − 80 °C until further analysis. Data are presented as the mean ± SD of 6 independent experiments.
ELISA
ELISA was performed using TNFα Human ELISA Kit (Invitrogen, Carlsbad, CA, USA) to determine TNFα concentration. The samples were read using an automated plate reader (Multiskan Spectrum; Thermo Scientific, Waltham MA, USA). Data are expressed as the mean ± SD of 6 independent experiments.
Multiplex bead immunoassays
Multiplex bead immunoassays (Bio-Plex Suspension Array System, BIO-RAD Laboratories, Inc., CA, USA), which incorporate novel technology with color-coded beads and permits the simultaneous detection of up to 100 cytokines and chemokines in a single well of a 96-well microplate, was used for the simultaneous quantification of the following chemokines: IL-8, IP-10, MCP-1, MIP-1α and MIP-1β. Data expressed the mean ± SD of 3 independent experiments.
Western blot analysis
Total protein was extracted from LPS-stimulated cells treated with antibiotics by using 200 µL of radioimmunoprecipitation assay buffer (FUJIFILM Wako, Osaka, Japan) containing a protease inhibitor cocktail (Nakalai Tesque, Kyoto, Japan) and the lysates were clarified by centrifugation (15,000 rpm, 10 min, 4 °C). Protein concentration was determined using Pierce 660 nm Protein Assay Kit (Thermo Scientific, Rockford, USA). Samples containing 10 µg of protein were run on a 10% polyacrylamide gel and electrotransferred onto a membrane filter (Immobilon-P; Millipore, Bedford, MA, USA). The membrane was blocked Blocking One (Nacalai Tesque) for 30 min, followed by incubation at room temperature for 1 h with a rabbit polyclonal antibody (Cell Signaling, Danvers, MA, USA) phospho-NF-κB p65, NF-κB p65, phospho-ERK, ERK, phospho-p38, p38, TACE and phospho-TACE (Abcam, Cambridge, UK). The membrane was then incubated at room temperature for 30 min with horseradish peroxidase-conjugated anti-mouse or anti-rabbit immunoglobulin G antibodies (GE Healthcare Bio-Science, Little Chalfont, England). Immunoreactive bands were visualized using enhanced chemiluminescence ImmunoStar LD (FUJIFILM Wako) and a FUSION-SOLO.7S.EDGE Chemilluminescence Imaging System (Vilber-Lourmat, 24 rue de Lamirault, 77090 Collégien, France). The data shown are representative of 3 independent experiments.
Flow cytometry analysis of intracellular TNFα staining
THP-1 cells (2 × 105/mL) were stimulated by LPS (0.1 µg/mL) with or without STFX (50 µg/mL) for 4 h. After incubation, the cells were fixed and permeabilized using a Fixation/Permeabilization Solution Kit (BD Biosciences, San Jose, CA, USA) according to the manufacturer’s protocol. Intracellular TNFα was stained using anti-TNFα antibody PE (BD Biosciences) for 1 h. The cells were washed and resuspended in phosphate-buffered saline (PBS) supplemented with 2% FBS and 0.05% NaN3. Intracellular TNFα was evaluated using FACS Canto II (BD Biosciences). Data shown are representative of 3 independent experiments.
TACE activity
TACE activity was measured using SensoLyte 520 TACE (α-Secretase) Activity Assay Kit (Anaspec, Inc. CA, USA) according to manufacturer’s protocol. THP-1 cells (2 × 105/mL) stimulated using LPS with or without STFX were washed with PBS. Assay buffer containing 0.1% Triton-X 100 was added to the cells or cell pellets. The cell suspension was collected in a microcentrifuge tube. The cell suspension was incubated at 4 °C for 10 min and then centrifuged for 10 min at 2500×g, at 4 °C. The supernatant was collected and stored at − 80 °C until use. Data are presented as the mean ± SD of 6 independent experiments.
Statistical analysis
The values are expressed as the mean ± SD. Data were analyzed by Student’s t-test using a statistical software (Microsoft Excel 2008; Microsoft Corporation, Redmond, WA, USA), in which a p-value < 0.05 was considered statistically significant.
Data availability
All data generated or analyzed during this study are included in this article.
Abbreviations
- CPFX:
-
Ciprofloxacin
- ESBL:
-
Extended-spectrum beta-lactamase
- ERK:
-
Extracellular signal-regulated kinase
- GRNX:
-
Garenoxacin
- IL-8:
-
Interleukin-8
- IP-10:
-
Interferon inducible protein
- LPS:
-
Lipopolysaccharide
- LVFX:
-
Levofloxacin
- MCP-1:
-
Monocyte chemoattractant protein-1
- MIP-1α:
-
Macrophage inflammatory protein-1α
- MIP-1β:
-
Macrophage inflammatory protein-1β
- MFLX:
-
Moxifloxacin
- NF-κB:
-
Nuclear factor-kappa B
- RIPA:
-
Radioimmunoprecipitation assay
- SIRS:
-
Systemic inflammatory response syndrome
- STFX:
-
Sitafloxacin
- TACE:
-
Tumor necrosis factor α converting enzyme
- TNFα:
-
Tumor necrosis factor alfa
References
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315, 801–810. https://doi.org/10.1001/jama.2016.0287 (2016).
Bone, R. C. et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101, 1644–1655. https://doi.org/10.1378/chest.101.6.1644 (1992).
Cazalis, J., Bodet, C., Gagnon, G. & Grenier, D. Doxycycline reduces lipopolysaccharide-induced inflammatory mediator secretion in macrophage and ex vivo human whole blood models. J. Periodontol. 79, 1762–1768. https://doi.org/10.1902/jop.2008.080051 (2008).
Tai, K., Iwasaki, H., Ikegaya, S. & Ueda, T. Minocycline modulates cytokine and chemokine production in lipopolysaccharide-stimulated THP-1 monocytic cells by inhibiting IκB kinase α/β phosphorylation. Transl. Res. 161, 99–109. https://doi.org/10.1016/j.trsl.2012.10.001 (2013).
Komiya, K. et al. Clarithromycin attenuates IL-13-induced periostin production in human lung fibroblasts. Respir. Res. 18, 37. https://doi.org/10.1186/s12931-017-0519-8 (2017).
Shinkai, M., Foster, G. H. & Rubin, B. K. Macrolide antibiotics modulate ERK phosphorylation and IL-8 and GM-CSF production by human bronchial epithelial cells. Am. J. Physiol. Lung Cell. Mol. Physiol. 290, 75–85. https://doi.org/10.1152/ajplung.00093.2005 (2006).
Tanabe, T. et al. Clarithromycin Inhibits interleukin-13-induced goblet cell hyperplasia in human airway cells. Am. J. Respir. Cell Mol. Biol. 45, 1075–1083. https://doi.org/10.1165/rcmb.2010-0327OC (2011).
Garcia-Roca, P., Mancilla-Ramirez, J., Santos-Segura, A., Fernández-Avilés, M. & Calderon-Jaimes, E. Linezolid diminishes inflammatory cytokine production from human peripheral blood mononuclear cells. Arch. Med. Res. 37, 31–35. https://doi.org/10.1016/j.arcmed.2005.05.022 (2006).
Kaku, N. et al. Antimicrobial and immunomodulatory effects of tedizolid against methicillin-resistant Staphylococcus aureus in a murine model of hematogenous pulmonary infection. Int. J. Med. Microbiol. 306, 421–428. https://doi.org/10.1016/j.ijmm.2016.05.010 (2016).
Hara, S. et al. Anti-inflammatory effects of garenoxacin on IL-8 production and ERK1/2 activation induced by lipopolysaccharides in A549 and THP-1 cells. Eur. J. Pharmacol. 668, 264–270. https://doi.org/10.1016/j.ejphar.2011.06.046 (2011).
Blau, H., Klein, K., Shalit, I., Halperin, D. & Fabian, I. Moxifloxacin but not ciprofloxacin or azithromycin selectively inhibits IL-8, IL-6, ERK1/2, JNK, and NF-kappaB activation in a cystic fibrosis epithelial cell line. Am. J. Physiol. Lung Cell. Mol. Physiol. 292, 343–352. https://doi.org/10.1152/ajplung.00030.2006 (2007).
Sato, K., Hoshino, K., Tanaka, M., Hayakawa, I. & Osada, Y. Antimicrobial activity of DU-6859, a new potent fluoroquinolone, against clinical isolates. Antimicrob. Agents Chemother. 36, 1491–1498. https://doi.org/10.1128/AAC.36.7.1491 (1992).
Onodera, Y., Uchida, Y., Tanaka, M. & Sato, K. Dual inhibitory activity of sitafloxacin (DU-6859a) against DNA gyrase and topoisomerase IV of Streptococcus pneumoniae. J. Antimicrob. Chemother. 44, 533–536. https://doi.org/10.1093/jac/44.4.533 (1999).
Nakamura, S. et al. In vivo efficacy of sitafloxacin in a new murine model of non-typeable Haemophilus influenzae pneumonia by sterile intratracheal tube. Int. J. Antimicrob. Agents 34, 210–214. https://doi.org/10.1016/j.ijantimicag.2009.03.011 (2009).
Miyazaki, T. et al. The efficacy and safety of sitafloxacin and garenoxacin for the treatment of pneumonia in elderly patients: A randomized, multicenter, open-label trial. J. Infect. Chemother. 25, 886–893. https://doi.org/10.1016/j.jiac.2019.04.019 (2019).
Manosuthi, W. & Wiboonchutikul, S. Treatment outcomes of oral sitafloxacin in acute complicated urinary tract infection and pyelonephritis. Springerplus 5, 410. https://doi.org/10.1186/s40064-016-2044-5 (2016).
Malaisri, C., Phuphuakrat, A., Wibulpolprasert, A., Santanirand, P. & Kiertiburanakul, S. A randomized controlled trial of sitafloxacin vs. ertapenem as a switch therapy after treatment for acute pyelonephritis caused by extended-spectrum β-lactamase-producing Escherichia coli: A pilot study. J. Infect. Chemother. 23, 556–562. https://doi.org/10.1016/j.jiac.2017.05.005 (2017).
Beutler, B., Milsark, I. W. & Cerami, A. C. Passive immunization Against cachectin/tumor necrosis factor protects mice From lethal effect of endotoxin. Science 229, 869–871. https://doi.org/10.1126/science.3895437 (1985).
Abraham, E. et al. Efficacy and safety of monoclonal antibody to human tumor necrosis factor alpha in patients with sepsis syndrome. A randomized, controlled, double-blind, multicenter clinical trial TNF-alpha MAb Sepsis Study Group. JAMA 273, 934–941. https://doi.org/10.1001/jama.1995.03520360048038 (1995).
Cohen, J. & Carlet, J. INTERSEPT: An international, multicenter, placebo-controlled trial of monoclonal antibody to human tumor necrosis factor-alpha in patients. With sepsis: International sepsis trial study group. Crit. Care Med. 24, 1431–1440. https://doi.org/10.1097/00003246-199609000-00002 (1996).
Abraham, E. et al. Double-blind randomised controlled trial of monoclonal antibody to human tumour necrosis factor in treatment of septic shock. Lancet 351, 929–933. https://doi.org/10.1016/S0140-6736(05)60602-2 (1998).
Kinoshita, K., Iwasaki, H., Uzui, H. & Ueda, T. Candin family antifungal agent Micafungin (FK463) modulates the inflammatory cytokine production stimulated by lipopolysaccharide in THP-1 cells. Transl. Res. 148, 207–213. https://doi.org/10.1016/j.trsl.2006.07.001 (2006).
Dalhoff, A. & Shalit, I. Jmmunomodulatory effects of quinolones. Lancet Infect. Dis. 3, 359–371. https://doi.org/10.1016/S1473-3099(03)00658-3 (2003).
Dalhoff, A. Immunomodulatory activities of fluoroquinolones. Infection 33(Suppl 2), 55–70. https://doi.org/10.1007/s15010-005-8209-8 (2005).
Ogino, H. et al. In vivo and in vitro effects of fluoroquinolones on lipopolysaccharide-induced pro-inflammatory cytokine production. J. Infect. Chemother. 15, 168–173. https://doi.org/10.1007/s10156-009-0680-1 (2009).
Black, R. A. et al. A metalloproteinase disintegrin that releases tumour-necrosis factor-alpha from cells. Nature 385, 729–733. https://doi.org/10.1038/385729a0 (1997).
Moss, M. L. et al. Cloning of a disintegrin metalloproteinase that processes precursor tumour-necrosis factor-alpha. Nature 385, 733–736. https://doi.org/10.1038/385733a0 (1997).
Acknowledgements
The authors would like to thank Ms. Maika Sugano for technical assistance with the experiments.
Funding
This work was supported by Grant-in-Aid for Scientific Research (C), No. 26461500.
Author information
Authors and Affiliations
Contributions
I.S., M.F., Y.Y. and H.I. designed the study. I.S., M.F., W.O., Y.T., K.I. and K.T. performed the experiments. I.S., M.F., W.O. and H.I. collected the data and wrote the manuscript. All authors have reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sakamaki, I., Fukushi, M., Ohashi, W. et al. Sitafloxacin reduces tumor necrosis factor alpha (TNFα) converting enzyme (TACE) phosphorylation and activity to inhibit TNFα release from lipopolysaccharide-stimulated THP-1 cells. Sci Rep 11, 24154 (2021). https://doi.org/10.1038/s41598-021-03511-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-03511-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.