Abstract
Low birthweight (LBW) is a worldwide problem that particularly affects developing countries. However, limited information is available on its magnitude in rural area of Burkina Faso. This study aimed to estimate the prevalence of low birthweight and to identify its associated factors in Nanoro health district. A secondary analysis of data collected during a cross-sectional survey was conducted to assess the prevalence of low birthweight in Nanoro health and demographic surveillance system area (HDSS). Maternal characteristics extracted from antenatal care books or by interview, completed by malaria diagnosis were examined through a multi-level logistic regression to estimate odd-ratios of association with low birthweight. Significance level was set at 5%. Of the 291 neonates examined, the prevalence of low birthweight was 12%. After adjustment for socio-demographic, obstetric and malaria prevention variables, being primigravid (OR = 8.84, [95% CI: 3.72–21.01]), or multigravid with history of stillbirth (OR = 5.03, [95% CI: 1.54–16.40]), as well as the lack of long-lasting insecticide treated bed net use by the mother the night preceding the admission for delivery (OR = 2.5, [95% CI: 1.1–5.9]) were significantly associated with neonate low birthweight. The number of antenatal visits however did not confer any direct benefit on birthweight status within this study area. The prevalence of low birthweight was high in the study area and represents an important public health problem in Burkina Faso. In light of these results, a redefinition of the content of the antenatal care package is needed.
Similar content being viewed by others
Introduction
Despite halving the global neonatal mortality rate from 36.6 to 18.0 per 1000 live births between 1990 and 20171, an estimated 2.5 million neonates died in the world in 2018, mainly among low birthweight neonates (LBW)2. Indeed, low birthweight—a birthweight below 2500 g—is an important risk factor for neonatal deaths3, which particularly affects developing countries where malaria transmission is endemic4. Sub-Saharan Africa is particularly affected due to the high risk of maternal infections during pregnancy5,6. Malaria, an example of these infections, causes up to 20% of all low birthweights in this region and 6% of neonatal deaths7. Thus, potentially, 100,000 infant lives could be saved each year if adequate malaria prevention measures were implemented. In Burkina Faso, malaria is the primary reason for seeking health care, and pregnant women are particularly affected.
To reduce malaria-related low birthweights in Sub-Saharan Africa, the World health organization (WHO) recommends a set of measures for pregnant women during antenatal care visits, which include the intermittent preventive treatment of malaria using sulfadoxine-pyrimethamine (IPTp-SP)8. IPTp-SP consists of monthly administration of sulfadoxine-pyrimethamine (SP) in pregnant women from the second trimester until delivery8. The strategy is effective in reducing malaria incidence and its consequences9. Burkina Faso adopted the strategy in 2005, with a minimum of three doses of sulfadoxine-pyrimethamine administered under the supervision of a healthcare worker10.
Although low birthweight adverse effects on neonatal survival have been well established3, little information is available on its prevalence in developing countries such as Burkina Faso. Indeed, at the start of the IPTp-SP policy in Burkina Faso, the prevalence of low birthweight was 15.8%11. Five years later, an evaluation reported a prevalence of 13.4%12. Since then, no other evaluation was conducted despite the numerous concerns raised by the low coverage of IPTp-SP strategy13 and the spread of Plasmodium falciparum resistance to sulfadoxine-pyrimethamine throughout the African continent14. Thus, a re-evaluation of the prevalence of adverse birth outcomes is necessary to timely seek alternative approaches. Therefore, this study aimed to assess the prevalence of low birthweight in rural Burkina Faso ten years after the IPTp-SP policy was adopted.
Methods
Study settings
The study was conducted in all eight peripheral health centers of the Nanoro health and demographic surveillance system (HDSS) area15. Nanoro is situated in the centre-west region of Burkina Faso at about 90 km from Ouagadougou, the capital city, and has a population of 63,000 inhabitants15. Malaria transmission is holo-endemic, with peak transmission overlapping with the rainy season (June-November). The commonest malaria vectors are Anopheles gambiae, A. funestus, A. arabiensis and P. falciparum is the predominant malaria parasite. Malaria is the main reason for visiting health centres with a case-fatality rate between 5 and 30%16.
Study design
We conducted a secondary analysis of data collected among pregnant women attending health centers for delivery in the Nanoro HDSS area from September 2013 to April 2014. The primary study of this analysis was an ancillary topic annexed to a main project (NCT01703884) entitled ‘ANC & Malaria Diagnostic in Pregnancy” and aimed to improve the quality of antenatal care and diagnostic services for malaria in pregnancy17. All eight peripheral health centers of the HDSS were included. The study site’s map is described elsewhere15. For each enrolled pregnant woman, their babies were assessed within 24 h of delivery. Demographic, gyneco-obstetric, and relevant medical history data were collected from antenatal care books or face-to-face interviews with the mother during both high and low malaria transmission seasons.
Study participants
Pregnant women aged 15–45 years, attending the health center for delivery with a gestational age of at least 37 weeks, living in the Nanoro HDSS area, and that provided written informed consent were eligible for inclusion. Those who delivered non-singleton babies, not willing to participate, or whose neonate was transferred before documentation of birthweight were not included. Of the 323 women included in the primary study, 9.9% (32/323) were excluded (4 non-singleton pregnancies, 6 stillbirths, 3 neonate deaths, 2 very ill newborns that were referred before clinical examination, 5 missing birthweights, 3 concurrent participations to other study and 9 preterm deliveries) and 291 (90.1%) were included.
Sample size
At the time of policy change, term LBW proportion was 15.8% of all live births11. We hypothesized that the new policy would reduce the low birthweight proportion to 10% after ten-year of widespread implementation. The Cochran formula n = Z2 *p*(1-p)/i2 was used to calculate the sample size where p = 10% is the expected proportion, i = 3.5%, represents the margin of error, Z the z-score that corresponds to the 95% confidence interval (1.96), n is the minimal sample size. The minimum required sample size was 282. This was a secondary analysis of database collected on 291 participants.
Data collection procedures and variables collected
Data were extracted from antenatal care books and by face-to-face interviews. Maternal age, educational level, occupation, and sulfadoxine-pyrimethamine uptake were collected from the antenatal care books. The use of insecticide-treated net (ITN) the night before visiting the health facility for delivery or any other variables not available in the antenatal care book were obtained by interview of the mother. Gestational age was estimated using the knowledge of the last menstrual period (LMP), or the Ballard score whenever LMP was unknown. Neonate examination was conducted within 24 h of delivery either in the health facility or at home by trained midwives. Birthweight was measured using a calibrated electronic scale with 10 g resolution and a precision less than 10 g (seca gmbh & co. kg, Germany). In addition, a malaria test using peripheral blood was performed by rapid diagnostic tests SD-Bioline Malaria Antigen Pf® test strips (sensitivity 99.7% and specificity of 99.5%). Table 1 presents the list, definitions, and grouping of variables. The outcome variable was birthweight at term categorized as normal birthweight (≥ 2500 g) and low birthweight (< 2500 g)18,19.
Data processing and analysis
Data were collected on a paper-based questionnaire by trained midwives and double-entered onto Redcap (Research—Electronic Data Capture) data collection tool, then imported into Stata version 15 (StataCorp. 2017, TX, USA) for cleaning and analysis. Categorical variables were summarized on frequency tables. Mean or median with respective measures of spread, including standard deviations and quartiles, were used to summarize numerical variables. Odds ratios (OR) and 95% confidence intervals (95% CI) were calculated according to each maternal factor using univariate logistic regression. Adjusted odds ratios (aOR) and 95% CI were derived by a backward multivariate logistic regression analysis of variables with statistically significant p-values at the univariate analysis, except for malaria. The final model retained variables which p-values were statistically significant. Variable age was not included due to its strong correlation with gravidity. A p-value < 0.05 was considered statistically significant.
Consent to publication
All data were anonymized before publication, thus consent for publication was not applicable.
Ethical considerations
Ethical clearance for this study was obtained from the National Ethics Committee of Burkina Faso. All data were anonymized before analysis. All participants or their authorized legally representatives provided a written informed consent prior to their participation. All methods were performed in accordance with the relevant guidelines and regulations.
Results
Study participants’ characteristics
Table 2 summarizes study participants’ background characteristics. Of the 291 mothers included, the mean age ± standard deviation was 26 ± 6 years, and most of them were unemployed (85.2%). Fourteen percent (14%) of women received at least three doses of sulfadoxine-pyrimethamine. Malaria infection was detected in one-third of the participants.
Low birthweight prevalence and associated factors
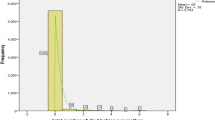
Of the 291 neonates, the mean birth weight (± standard deviation) was 2933 ± 390 g and 12.0% (35/291) live births were low birthweight. Table 3 presents the proportions of low birthweight and the maternal sociodemographic characteristics, obstetrical history as well as the univariate and adjusted odds ratios. Being primigravid or multigravid with an obstetrical history of stillbirth, and the lack of long-lasting insecticide-treated bed net use were significantly associated with low birthweight. However, the number of antenatal care visits performed did not show any link with the prevalence of low birthweight.
Multi-level logistic regression analysis included variable gravidity, the use of insecticide-treated bed nets the night before hospital admission for delivery, and malaria test results. Being primigravid (OR = 8.83, [95% CI: 3.71–21.01]), multigravid with an obstetrical history of stillbirth (OR = 5.03, [95% CI: 1.54–16.40]) and the lack of bed net use (OR = 2.5, [95% CI: 1.1–5.9]) were significantly associated with higher proportion of low birthweight among neonates.
Discussion
Low birthweight prevalence was high in Nanoro given that those from preterm births were not included in this analysis. However, the report showed a substantial decrease (3.8 percentage points) from its level at the start of the IPTp-SP strategy11. Several factors, including the mother's socioeconomic status, obstetrical characteristics, and malaria prevention methods, influence low birthweight prevalence, and those factors differed from each setting. Indeed, lower low birthweight rates were observed in Ethiopia (10%)20 and in Nigeria (7%)21. However, these estimates were understated as the Nigerian’s study used data collected retrospectively from the routine surveillance system, which is not adapted to SSA as half of neonate birthweights are not recorded due to weaknesses of the reporting system4. Also, the study in Ethiopia was conducted in urban areas where women's economic level tends to be higher than those from the rural areas, and the impact of socioeconomic status on the prevalence of low birthweight is well established22,23.
In contrast, rates in excess were reported in South Africa (38.5%)24 and in a study conducted in Zimbabwe (16.7%)25. These could be related to the higher prevalence of human immuno-deficiency virus (HIV) infection26. Indeed, HIV is considered an important risk factor of LBW, although the mechanism is not yet fully elucidated25,27.
It is reported that maternal obstetrical history and events occurring during pregnancy impact the outcome of pregnancies, although those factors are not always identified28.
We found that the order of pregnancy was significantly associated with low birthweight and first pregnancy infants were at higher risk than others. The biological ground for first pregnancy neonates to be at higher risk of low birthweight may be related to the susceptibility of first pregnancy placentas to parasite-infected red blood cells sequestration, disrupting fetus nutrients supply29 and increasing risk of low birthweight, or because some physiologic changes are less efficient during first pregnancies thus increasing the risk of low birthweight30. Indeed, uteroplacental blood flow, responsible for delivering oxygen and nutrients to the fetus, is greater during subsequent pregnancies than in the first pregnancy31,32. Also, we have noted that mothers with multiple pregnancies were also at higher risk if there was an obstetrical history of stillbirth. Chen et al. in 2018 and Rozi et al. in 2016 made such observations in their respective studies33,34, while Ahrens et al. went further to notice that the risk was highest after a history of three stillbirths35. Particular attention should be paid to pregnant women with such background characteristics during their antenatal care visits.
As expected, the lack of long-lasting insecticide-treated bed net usage was associated with an increased risk of low birthweight36. Bed net usage has long been recommended in areas with sustained malaria transmission as an effective tool to prevent malaria-related adverse birth outcomes, including low birthweight37. Although bed net is freely provided to pregnant women during the first antenatal care visit in Burkina Faso, a high proportion of women (up to 20%) were not covered, and actions toward improving bed net usage are required.
The number of antenatal care visits performed and the intermittent preventive treatment of malaria in pregnancy did not directly influence the prevalence of low birthweight in this study. Although the limited sample size did not allow an accurate evaluation of all low birthweight factors, Plasmodium falciparum resistance to sulfadoxine pyrimethamine reported in many parts of sub-Saharan Africa and Burkina Faso could be a limiting factor of the efficacy of IPTp-SP strategy38,39,40,41. Indeed, the high number of triple mutants, and the presence of quintuple mutants (triple dhfr and double dhps mutations) reported in Burkina Faso may have decreased the efficacy of sulfadoxine-pyrimethamine on P. falciparum in the study settings, and thus the effects of the IPTp-SP strategy on low birthweight42.
Contrary to what is reported in the literature, malaria was not associated with low birthweight in the current study. The use of malaria rapid diagnosis test could have understated the actual extent of malaria infection in the study population and thus, underestimated the extent of malaria negative effects on the fetus43. Studies building on the most accurate diagnosis methods are needed in this study setting.
A number of limitations in this study are worth noting and taken into consideration. The study was conducted on term pregnancies excluding low birthweight from preterm deliveries, which could understate the problem's actual extent. It remains to bear in mind that gestational age was dated from parental knowledge of the last menstrual period (LMP) or the Ballard score, which could be prone to some errors. The use of malaria RDT for the diagnosis in peripheral blood sample could have understated the extent of malaria infection in the study population and thus undermine the strength of association with low birthweight. Although the analysis had limitations, it depicted the overall picture of the magnitude of low birthweight in rural Burkina Faso.
Conclusion
Low birthweight prevalence was high in Nanoro and required more effective policies. Exploring novel approaches or improving current approaches is needed. But first, quality data building on larger sample size are necessary to update maternal risk factors of low birthweight.
Data availability
The dataset used and analyzed during the current study is available from the corresponding author.
Abbreviations
- SP:
-
Sulfadoxine pyrimethamine
- IPTp:
-
Intermittent preventive treatment of malaria in pregnancy
- LBW:
-
Low birthweight
- ANC:
-
Antenatal care
- OR:
-
Odds ratio
- aOR:
-
Adjusted odds ratio
- CI:
-
Confident interval
- SDG:
-
Sustainable development goals
- NMR:
-
Neonatal mortality rate
- HDSS:
-
Health and demographic surveillance system
- HIV:
-
Human immunodeficiency virus
- WHO:
-
World health organization
- LMP:
-
Last menstrual period
References
Hug, L., Alexander, M., You, D. & Alkema, L. National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: A systematic analysis. Lancet Glob. Health 7, e710–e720 (2019).
WHO-Newborns: Reducing Mortality 2019. https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality. Accessed 30 Oct 2020.
Katz, J. et al. Mortality risk in preterm and small-for-gestational-age infants in low-income and middle-income countries: A pooled country analysis. Lancet 382, 417–425 (2013).
UNICEF-Low Birthweight. 2019. https://data.unicef.org/topic/nutrition/low-birthweight/. Accessed 23 May 2020.
Lee, A. C. et al. National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle-income countries in 2010. Lancet Glob. Health 1, e26-36 (2013).
Lawn, J. E. et al. Every newborn: Progress, priorities, and potential beyond survival. Lancet 384, 189–205 (2014).
Guyatt, H. L. & Snow, R. W. Impact of malaria during pregnancy on low birth weight in Sub-Saharan Africa. Clin. Microbiol. Rev. 17, 760–769 (2004).
WHO | Intermittent Preventive Treatment in Pregnancy (IPTp). 2019. https://www.who.int/malaria/areas/preventive_therapies/pregnancy/en/. Accessed 4 May 2020.
Kassoum, K. et al. Intermittent preventive therapy for malaria during pregnancy using 2 vs 3 or more doses of sulfadoxine-pyrimethamine and risk of low birth weight in Africa: Systematic review and meta-analysis. JAMA 309, 594–604 (2015).
Gansané, A. et al. Change of antimalarial first-line treatment in Burkina Faso in 2005. Bull Soc. Pathol. Exot. 102, 31–35 (2009).
Kabore, P., Donnen, P. & Dramaix-wilmet, M. Obstetrical risk factors for lowbirth-weight in a rural Sahelian area. Sante Publ. (Paris). 19, 489–497 (2007).
He, Z. et al. Prevalence of low birth weight and its association with maternal body weight status in selected countries in Africa: A cross-sectional study. BMJ Open 8, 1–8 (2018).
Yaya, S., Uthman, O. A., Amouzou, A. & Bishwajit, G. Use of intermittent preventive treatment among pregnant women in sub-Saharan Africa: Evidence from malaria indicator surveys. Trop. Med. Infect. Dis. 2018, 3 (2018).
van Eijk, A. M. et al. Effect of Plasmodium falciparum sulfadoxine-pyrimethamine resistance on the effectiveness of intermittent preventive therapy for malaria in pregnancy in Africa: A systematic review and meta-analysis. Lancet Infect. Dis. 19, 546–556 (2019).
Derra, K. et al. Profile: Nanoro health and demographic surveillance system. Int. J. Epidemiol. 41, 1293–1301 (2012).
WHO-Burkina Faso African Region. 2019. https://www.who.int/malaria/publications/country-profiles/profile_bfa_en.pdf?ua=1. Accessed 30 Nov 2020.
ANC & Malaria Diagnostic in Pregnancy-Full Text View-ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT01703884. Accessed 18 Sep 2021.
Rosenberg, R. E. et al. Determining gestational age in a low-resource setting validity of last menstrual period. J. Health Popul. Nutr. 27, 332–338 (2009).
Cutland, C. L. et al. Low birth weight: Case definition & guidelines for data collection, analysis, and presentation of maternal immunization safety data. Vaccine. 35, 6492–6500 (2017).
Gebregzabiherher, Y., Haftu, A., Weldemariam, S. & Gebrehiwet, H. The prevalence and risk factors for low birth weight among term newborns in Adwa general hospital, northern Ethiopia. Obstet. Gynecol. Int. 2017, 7 (2017).
Dahlui, M., Azahar, N., Oche, O. M. & Aziz, N. A. Risk factors for low birth weight in Nigeria: Evidence from the 2013 Nigeria demographic and health survey. Glob. Health Action. 9, 28822 (2016).
Kaur, S. et al. Risk factors for low birth weight among rural and urban Malaysian women. BMC Public Health 19, 1–10 (2019).
Rezende Chrisman, J. et al. Prevalence of very low birthweight, malformation, and low Apgar score among newborns in Brazil according to maternal urban or rural residence at birth. J. Obstet. Gynaecol. Res. 42, 496–504 (2016).
Tshotetsi, L., Dzikiti, L., Hajison, P. & Feresu, S. Maternal factors contributing to low birth weight deliveries in Tshwane district, South Africa. PLoS ONE 14, 1–13 (2019).
Feresu, S. A., Harlow, S. D. & Woelk, G. B. Risk factors for low birthweight in Zimbabwean women: A secondary data analysis. PLoS ONE 10, 1–17 (2015).
Eaton, J. W. et al. Recent HIV prevalence trends among pregnant women and all women in sub-Saharan Africa. AIDS 28, S507–S514 (2014).
Hoque, M. E., Towbola, O. A., Mashamba, T. J. & Monokoane, T. Comparison of adverse pregnancy outcome between teenage and adult women at a tertiary hospital in South Africa. Biomed. Res. 25, 167–172 (2014).
Scrimshaw, S.C., & Backes, E.P. Committee on Assessing Health Outcomes by Birth Settings A Consensus Study Report. 2020. https://doi.org/10.17226/25636. Accessed 11 Oct 2020.
Duffy, P. E. Plasmodium in the placenta: Parasites, parity, protection, prevention and possibly preeclampsia. Parasitology 134, 1877–1881 (2007).
Soma-Pillay, P., Nelson-Piercy, C., Tolppanen, H. & Mebazaa, A. Physiological changes in pregnancy. Cardiovasc. J. Afr. 27, 89–94 (2016).
Clapp, J. F. & Capeless, E. Cardiovascular function before, during, and after the first and subsequent pregnancies. Am. J. Cardiol. 80, 1469–1473 (1997).
Prefumo, F. et al. Effect of parity on second-trimester uterine artery Doppler flow velocity and waveforms. Ultrasound Obstet. Gynecol. 23, 46–49 (2004).
Rozi, S., Butt, Z. A., Zahid, N., Wasim, S. & Shafique, K. Association of tobacco use and other determinants with pregnancy outcomes: a multicentre hospital-based case-control study in Karachi, Pakistan. BMJ Open 6, e012045 (2016).
Chen, S. et al. Both maternal and paternal risk factors for term singleton low birthweight infants in rural Chinese population: A population-based, retrospective cohort study. Sci. Rep. 8, 1–7 (2018).
Ahrens, K. A., Rossen, L. M. & Branum, A. M. Pregnancy loss history at first parity and selected adverse pregnancy outcomes. Ann. Epidemiol. 26, 474-481.e9 (2016).
Pryce, J., Richardson, M. & Lengeler, C. Insecticide-treated nets for preventing malaria. Cochrane Database Syst. Rev. 1, 2018 (2018).
Gamble, C., Ekwaru, J. P. & ter Kuile, F. O. Insectide-treated nets for preventing malaria in pregnancy. Cochrane Database Syst. Rev. 38, 34–35 (2009).
Mandoko, P. N. et al. Prevalence of P falciparum parasites resistant to sulfadoxine/pyrimethamine in the democratic republic of the congo: Emergence of highly resistant PfdHFR/PfdHps alleles. J. Antimicrob. Chemother. 73, 2704–2715 (2018).
Minja, D. T. R. et al. P falciparum mutant haplotype infection during pregnancy associated with reduced birthweight, Tanzania. Emerg. Infect. Dis. 19, 1446–1454 (2013).
Mbonye, A. K. et al. Prevalence of P falciparum resistance markers to sulfadoxine-pyrimethamine among pregnant women receiving intermittent preventive treatment for malaria in Uganda. Antimicrob. Agents Chemother. 59, 5475–5482 (2015).
Xu, C. et al. Mutation profile of pfdhfr and pfdhps in P. falciparum among returned Chinese migrant workers from Africa. Antimicrob. Agents Chemother. 63, 1–6 (2019).
Ruizendaal, E. et al. Increase in the prevalence of mutations associated with sulfadoxine-pyrimethamine resistance in Plasmodium falciparum isolates collected from early to late pregnancy in Nanoro, Burkina Faso. Malar. J. 16, 1–15 (2017).
Fried, M., Muehlenbachs, A. & Duffy, P. E. Diagnosing malaria in pregnancy: An update. Expert Rev. Anti Infect. Ther. 10, 1177–1187 (2012).
Acknowledgements
We thank the study participants and the health staff of Nanoro Health District. This manuscript was presented in Research Square as a Preprint (https://www.researchsquare.com/article/rs-61707/v1).
Funding
The field work in this project was supported by the Clinical Research Unit of Nanoro, Burkina Faso. ML and HSZ are supported by a PhD scholarship from the Belgian Universities Cooperation for the Development (https://www.ares-ac.be/fr/cooperation-au-developpement). The funding bodies had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
M.L., D.V., I.V. and H.T. have conducted the study, conceptualized and written large parts of the manuscript. M.L., M.S., M.W.D., and A.R. performed the statistical work. M.S., S.O.S. A.R., M.W.D. and D.P. have made important comments to the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lingani, M., Zango, S.H., Valéa, I. et al. Magnitude of low birthweight in malaria endemic settings of Nanoro, rural Burkina Faso: a secondary data analysis. Sci Rep 11, 21332 (2021). https://doi.org/10.1038/s41598-021-00881-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-00881-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.