Abstract
Low birth weight is a newborn delivered with birth weight of less than 2500 g regardless of gestational age is called. It is a significant issue affecting over 30 million infants worldwide. Thus, the study determine factors associated with low birth weight among newborns delivered at Mettu Karl Comprehensive Specialized Hospital, Southwest Ethiopia. A facility-based case–control study was conducted with 336 newborns (112 cases and 224 controls) from September 12 to December 23, 2022. The study population was newborns with birth weights of 2500 g to 4000 g as controls and newborns with birth weights < 2500 g were cases. Simple random sampling techniques were used to recruit study participants with a ratio of 1 to 3 cases to controls, respectively. Data was collected by interviews and a checklist. Data were entered and analysed using SPSS version 23. Binary and multivariate logistic regression analyses were computed to identify factors associated with low birth weight, a p-value less than 0.05 was used to declare the strength of statistical significance. A total of 327 newborns were contacted, yielding a 97% response rate. MUAC < 23 cm (AOR = 2.72, 95% CI 1.24 to 6.19), inadequate diet diversification (AOR = 4.19, 95% CI 2.04 to 8.60), lack of iron and folic acid supplementation (AOR = 2.94, 95% CI 1.25 to 6.88), history of hypertension (AOR = 2.55, 95% CI 1.09 to 6.00), and lack of nutritional counselling (AOR = 4.63, 95% CI 2.22 to 9.64) were determinants of low birth weight. Low birth weight is linked to residence, maternal MUAC, hypertension history, and ANC visit. Lifestyle modifications, early detection, management, and nutrition information can reduce risk.
Similar content being viewed by others
Introduction
Low birth weight (LBW) is a baby delivered with a birth weight of less than 2500 g (5.5 pounds), regardless of gestational age1. A large group of infants are born preterm, intrauterine growth-restricted, or both preterm and intrauterine growth-restricted1,2. Birth weight is a predictor of perinatal and infant survival, morbidity and mortality, and later risk for developmental disabilities in their lives3,4
Globally, more than 30 million newborns are delivered annually; of this, almost one-quarter of them have low birth weight 1. The majority of births occur in south-central Asia, with one-third of them weighing less than 2500 g4,5. Low birth weight: in Sub-Saharan Africa, 15 percent of them grow up as stunted children, developing different complicated infections that require later hospital admission3,6.
Low birth weight is primarily determined by maternal health condition and nutrition status in developing countries, unlike in developed countries, where usually cigarette smoking during pregnancy is the primary cause of low birth weight7. Additionally, genetic, socio-demographic, maternal medical illness, intrauterine fetal complications, and environmental factors are predictors of low birth weight across the world6,8. In Ethiopia, low birth weights ranged from (10.4 to 17.3%) and this makes Ethiopia grouped under five countries that are accountable for half of global neonatal deaths among Sub-Saharan Africa9,10,11.
The World Health Organisation is set to reduce the burden of low birth weight by as little as 30% by 2025 through nutritional policies on getting affordable, accessible, and appropriate health care for preventing and treating low birth weight1. Based on WHO reccomendation, the Ethiopian government declares different strategies to reduce low birth weight and neonatal death12. The burden of low birth weight still remained high in Ethiopia9,10,11. The available studies were mainly focuses on the prevalence of low birth weight. therefore, these studies account some of the factors linked with LBW such asnutritional-related factors and nutritional assessment in the the study area. Thus, the study was conducted to determine factors associated with low birth weight among newborns delivered at Mettu Karl Comprehensive Specialised Hospital,South West Ethiopia.
Methods and materials
Study design, setting, and period
A facility-based, unmatched case–control study was conducted at Mettu Karl Comprehensive Specialised Hospital from September 12 to December 23, 2022. The hospital is located in Mettu town about 600 km from Addis Ababa, the capital city of Ethiopia. The hospital provides service for in patients and out patients, maternal and child health as well as ART services for patients in the ilu abba bor zone, south-western Ethiopia and Gambella regional states, with a catchment population of more than 2.4 million in 2007 G.C.
Sourse and study population
The cases were a single alive newborns whose birth weight < 2500 g and had not gross congeital anomalies at Mettu Karl Comprehensive Specialised Hospital (MKCSH) between September 12, 2022 and Decemember 23, 2022. Whereas the controlswere a single alive ewborns weight ≥ 2500 g, but ≤ 4000 g of who were delivered in the same health facilities within 24 h of the delivery of cases and had not gross congeital anomalies.
Sample size determination
The sample size was determined by using double population proportion formula. By the following assumptions a cases to controls ratio of 1:2. Power = 80%, Zβ = 0.84 for 0.05 significance level, Zα = 1.96 OR = Minimal detectable odds ratio is 2, P1 = proportion of exposure among the cases = 40.9% P2 = the proportion exposed in the control = 24.8%13
Sampling procedures
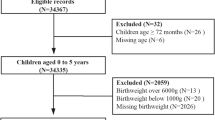
After additional consideration of the non-response rate of 5%, the total sample size was 336 (112 cases and 224 controls). A simple random sampling techiques were used to select cases. Whereas controls were selected consequatively at the same and same day of delivey with the ratio of 1 to 2 case to controls within 24 h after delivery. Data was collected each time a low birth weight baby had been delivered until the required sample size was attained.
Operational defiitions
Minimum dietary diversity for women (MDD-W)
The amounts of woman consumes from 10 dietary diversity food groups.
Adequate dietary diversity for women
If women consumed at least five different food groups during the previous day or night, from ten food groups.
Inadequate dietary diversity for women
If women consumed less than five different food groups during the previous day or night, from ten food groups.
Antenatal care (ANC) visits
Which was dichotomized as Yes if a woman has at least one Antenatal care visits and No if a woman has no any Antenatal care visits during the last pregnancy.
Study variables
Sociodemographic factors
Maternal age, educational status, family income, place of residence, occupation, and family size.
Obstetric factors
ANC visit, Gravidity, Parity, Gestational age, Pregnancy-induced Hypertension, Labor complication, and vaginal bleeding.
Maternal nutritional associated factors
Maternal dietary diversity (MDD-women), Maternal Anthropometric measurements, nutritional counseling during pregnancy, IFA, and Micronutrient supplementations.
Maternal medical/lifestyle factors
History of chronic diseases like Hypertension, Diabetes Mellitus, Anemia, TB, Malaria, History of Smoking, Chewing chat, and severe physical work during pregnancy.
Data collection tools and management procedures
The data were collected through interviews, structured questionnaires, and medical record reviews. The newborn's weight was measured using a balanced Seca scale (German) to the nearest 0.01 g within 1 h of birth. To assure the quality of data two days of training was given to data collectors and supervisors. Trainings started before actual data collection regarding how to approach the study subjects, how to use questionnaires, the data collection procedures, the context of specific questions, and the anthropometric measurement procedures. Minimum Dietary Diversity for Women (MDD-W) was measured by the ten questions developed by FAO and FANTA as a proxy indicator to reflect the micronutrient adequacy of women’s diets. The MDD-W indicator is dichotomous, it returns the value Yes or No. The woman achieves minimum dietary diversity, i.e. Yes, if she consumed at least five different food groups during the previous day or night, and No otherwise (1) Grains, white roots and tubers, and plantains, (2) Pulses (beans, peas and lentils), (3) Nuts and seeds, (4) Milk and milk products, (5) Meat, poultry and fish. (6) Eggs, (7) Dark green leafy vegetables, (8) Other vitamin A-rich fruits and vegetables, (9) Other vegetables, (10) Other fruits14. Mid-upper arm circumference (MUAC) was also measured using a non-stretchable MUAC tape according to procedures. The questionaries’ was adapted by reviewing different related literature reviews15,16,17,18,19,20.
Data processing and analysis
Data were checked for completeness, accuracy, and then cleaned, coded, and were entered to Epi data version 7.0 then exported to SPSS version 23.0 for statistical analysis. Descriptive statistics such as frequency,and percentages were used to describe the study subjects. Binary and multivariate logistic regression analayis was computed to identify factors associated with LBW and a p-value less than 0.05 were used to declare the strength of statistical significances.
Ethical consideration
This research was performed in accordance with the Helsinki Declaration of Principles. A letter of ethical clearance was obtained from the ethics committee of the College of Health Science at Mattu University, with a reference letter of DPH/157/2022.
Consent to participate
All the study participants were informed about the purpose of the study and their right to refuse participation or terminate their involvement during the study. Written informed consent was obtained from each study participant.. Information was provided to each study participant before signing the informed consent form on the purpose of the study, data handling, and confidentiality of the information.
Results
Socio-demographic characteristics of study participants
A total of 327 were contacted (109 cases and 218 controls) agreed to take part in the study, yielding a 97% response rate. Male constituted in the majority 54% and 59.2% of cases and controls respectively in the study. From the study participants, 35 (32.1%) of the case and 11 (5%) of the control of mothers age were under 20 years (Table 1).
Obstetrics, medical, and nutritional related factors of study participants
In this study, majority of study partcipants 73.3% case and 88.9% control have ANC visits, whereas, 26.7% of cases and 11.1% of controls has no ANC visits. Among study participants 49.5% of cases have no IFA supplementation, whereas 87.6% of controls have IFA supplementation. However only 50.5% of cases have IFA supplementation and 12.4% of control has no IFA supplementation (Table 2).
Logestics regression analysis
A significant association were identified between low birth weight were living the rural area, lack of nutritional counseling History of Hypertension, Having ANC visits, Inadequate minimum MDD-women (Table 3).
Discussion
This study reveals that rural women have a higher odds of having a low birth weight than urban mothers. This agreed with individuals reside influences their behaviours, income, and, most significantly, their health and nutrition15. The findings are comparable with studies undertaken in Bale, Oromia, Ethiopia, Malaysia, and Yemen, which found that rural pregnant women are more likely to have low birth weights than urban pregnant women13,16,17. However, a study conducted in the Jimma Zone found that women living in urban areas had a higher risk of having low-birth-weight babies18. This disparity could be attributed to differences in study design, health awareness, geographical location, and demographic features of study participants.
Odds of pregnancy-induced hypertension more risk of developing low birth weight than women who do not have a history of pregnancy-induced hypertension. In fact, high blood pressure may reduce blood flow to the placenta, and as a result, the fetus may not get enough of the nutrients and oxygen needed to grow15. Our findings, consistent with studies conducted in north Shewa, Addis Ababa, and Malaysia, showed that pregnant mothers who have a history of pregnancy-induced hypertension were at higher risk of developing low birth weight than pregnant women who have no history of hypertension9,18,21 respectively. The possible consistency of the finding could be that hypertension in pregnancy causes narrowing placental blood vessels, will be complicated by utero placental insufficiency, and increases the risk of low birth weight outcomes9. However, a study conducted in China showed that hypertensive mothers did not show an increased risk for lowbirth weight16. This discrepancy may be due to differences in the study setting, methods, and sociodemographics of the subjects. Additionally, women who were not counselled about nutritional intake during pregnancy had higher odds of having a low birth weight than pregnant women who had been counselled about nutritional intake. Our finding are consistent with a study conducted in North Shewa, Dessie town, Dire Dawa, and Hawassa Ethiopia10,11,21,22 respectively. The possible consistency of nutritional counselling may improve their intake habits, and having information about eating a healthy diet can reduce the chance of fetal growth restriction and high blood pressure, reducing the risk of low birth weight in pregnant women15.
Iron and folic acid supplementation showed significant assocaiation in this study. Pregnant women who do not receive iron and folic acid supplements have a higher odds of developing low birth weight than their counterparts. Our finding agreed with a study in Nekemte town and north Shewa, Ethiopia21,23. This is supported by evidence that IFA supplementation protects against low birth weight as a multiple micronutrient supplement19. Additionally, having IFA supplementation during pregnancy decreases the odds of developing a low birth weight compared to the uterine parts of pregnant women9,20,24. The possible outcomes could be additional intakes of supplementation, reducing morbidities and risks of congenital malformation.
This study discovered that mothers whose MUAC is less than 23 cm have a higher risk of developing a low birth weight than mothers whose MUAC is greater than or equal to 23 cm. This is supported by a study conducted in the Sidama Zone in south Ethiopia, Yemen, and India3,17,25 respectively. This consistency was supported by the available evidence. Low birth weight is a result of undernutrition and the health status of the mother during her pregnancy; MUAC less than normal affects birth weight outcomes15.
Inadequate minimum women's dietary diversification increases the risk of being exposed to low birth weight compared to those who had adequate minimum women's dietary diversification during pregnancy. Our findings aligned with a study conducted in Ghana, systematic review reports where women's dietary diversity scores and dietary patterns were found to be protective against low birth weight26,27. This consistency could be due to similarities in background characteristics, study design, and study population.
Lastly, women who have antenatal care are 89 percent more protected from low birth than mothers who had non-ANC visits during their recent pregnancy. This is also consistent with studies in Sidama, Bale, Gondar Shewa, Ethiopia, and Italy3,13,28,29 respectively. This could be due to the fact that the World Health Organisation strongly recommends during pregnancy the utilisation of antenatal care used for early identification of risky pregnancy and screening for pregnancy complications, as well as early treatments that improve the birth outcomes of pregnancy.
Strength and limitation of the study
The data was collected with consistent inclusion and exclusion criteria from cases and controls by case control study design to minimise selection bias. Self-reporting methods may lead to recall bias and subjective diagnosis, which may affect the generaliability of findings but not the quality of the study.
Conclusions
Low birth weight was significantly associated with residence, maternal MUAC, non-compliance with IFA supplementation, hypertension history, nutiritonal counselling, minimum MDD-women, and ANC visit of the mother. Life style Modification, early detection, and management of maternal hypertension, as well as strengthening nutrition information and counselling during pregnancy, will help minimise the risk of low birth weight.
Data availability
Data we used in this manuscript were available on behalf of corresponding authors based on reseanble requests.
References
WHO. Global nutrition targets 2025. Low Birth Weight Policy Brief 14(5), 1–8 (2014).
Musoke, R. N. Low birthweight. East Afr. Med. J. 63, 89–90 (1986).
Bekela, M. B. et al. Determinants of low birth weight among newborns delivered at public hospitals in Sidama Zone, South Ethiopia: Unmatched case-control study. J. Pregnancy 2020, 4675701 (2020).
Hughes, M. M., Black, R. E. & Katz, J. 2500-g low birth weight cutoff: History and implications for future research and policy. Matern. Child Health J. 21(2), 283–289 (2017).
Blencowe, H. et al. National, regional, and worldwide estimates of low birthweight in 2015, with trends from 2000: A systematic analysis. Lancet Glob. Heal. 7(7), e849–e860 (2019).
Barros, F. C. et al. How many low birthweight babies in low- and middle-income countries are preterm?. Rev Saude Publica 45(3), 607–616 (2011).
Talie, A., Taddele, M. & Alemayehu, M. Magnitude of low birth weight and associated factors among newborns delivered in Dangla Primary Hospital, Amhara Regional State, Northwest Ethiopia, 2017. J. Pregnancy 2019, 3587239 (2019).
Takatori, K. Mendeley; Reference manager. J. Inst. Image Inf. Telev. Eng. 70, 320–323 (2016).
Roudbari, M., Yaghmaei, M. & Soheili, M. Prevalence and risk factors of low-birth-weight infants in Zahedan, Islamic Republic of Iran. East Mediterr Heal. J. 13(4), 838–845 (2007).
Ahmed, S., Hassen, K. & Wakayo, T. A health facility based case-control study on determinants of low birth weight in Dassie town, Northeast Ethiopia: The role of nutritional factors. Nutr. J. 17(1), 1–10 (2018).
Ibrahim, M. O. Determinants of low birth weight in dire-dawa city public health facility Eastern Ethiopia—Unmatched Case Control Study. Res Sq. (2021).
Ethiopian Public Health Institute (EPHI), ICF. Ethiopia Mini Demographic and Health Survey 2019: Final Report 1–207 (2021).
Demelash, H., Motbainor, A., Nigatu, D., Gashaw, K. & Melese, A. Risk factors for low birth weight in Bale zone hospitals, South-East Ethiopia : A case-control study. BMC Pregnancy Childbirth 15, 264 (2015).
FAO, 360 FHI. Minimum Dietary Diversity for Women: A Guide for Measurement (2016).
FAO, IFAD UW and W. Food security and nutrition in the world. Safeguarding against economic slowdowns and downturns, Rome, Italy.
Kaur, S. et al. Risk factors for low birth weight among rural and urban Malaysian women. BMC Public Health 19(Suppl 4), 1–10 (2019).
Muftah, S. Maternal under-nutrition and anaemia factors associated with low birth weight babies in Yemen. Int. J. Commun. Med. Public Heal. 3(10), 2749–2756 (2016).
Tema, T. Prevalence and determinants of low birth weight in Jimma Zone, Southwest Ethiopia. East Afr. Med. J. 83(7), 366–371 (2006).
Ramakrishnan, U., González-Cossío, T., Neufeld, L. M., Rivera, J. & Martorell, R. Multiple micronutrient supplementation during pregnancy does not lead to greater infant birth size than does iron-only supplementation: A randomized controlled trial in a semirural community in Mexico. Am. J. Clin. Nutr. 77(3), 720–725 (2003).
Zenebe, A., Tegegne, K. T., Bifato, B. & Assefa, A. A. Association between iron and folic acid supplementation and birth weight in Ethiopia: Systemic review and meta analysis. Bull. Natl. Res. Cent. 45(1), 1–10 (2021).
Gizaw, B. & Gebremedhin, S. Factors associated with low birthweight in North Shewa zone, Central Ethiopia: Case-control study. Ital. J. Pediatr. 44(1), 1–9 (2018).
Siyoum, M. & Melese, T. Factors associated with low birth weight among babies born at Hawassa University Comprehensive Specialized Hospital, Hawassa, Ethiopia. Ital. J. Pediatr. 45(1), 1–7 (2019).
Kaewkiattikun, K. Effects of immediate postpartum contraceptive counseling on long-acting reversible contraceptive use in adolescents. Adolesc. Health Med. Therap. 8, 115–123 (2017).
Matin, A. et al. Maternal socioeconomic and nutritional determinants of low birth weight in Urban area of Bangladesh. J. Dhaka Med. Coll. 17(2), 83–87 (1970).
Vasundhara, D. et al. Maternal MUAC and fetal outcome in an Indian tertiary care hospital: A prospective observational study. Matern. Child Nutr. 16(2), 1–8 (2020).
Sharma, S. R. et al. Low birth weight at term and its determinants in a tertiary hospital of nepal: A case-control study. PLoS One 10(4), 1–10 (2015).
Kheirouri, S. & Alizadeh, M. Maternal dietary diversity during pregnancy and risk of low birth weight in newborns: A systematic review. Public Health Nutr. 24(14), 4671–4681 (2021).
Edris, M. & Erakli, G. The prevalence of low birth weight and factors associated with low birth weight delivery in Gondar Region, north west Ethiopia. Ethiop. J. Heal. Dev. 10(3), 149–152 (2017).
Nobile, C. G. A., Raffaele, G., Altomare, C. & Pavia, M. Influence of maternal and social factors as predictors of low birth weight in Italy. BMC Public Health 7, 1–9 (2007).
Acknowledgements
First of all we would like to thank data collectors and supervisors, and study participants for their cooperation through data collection time. Likewise, we thank our families and friends who gave support and inspiration without them nothing is accomplished.
Author information
Authors and Affiliations
Contributions
S.E., M.A., B.T. inception designed the proposal, data analysis, interpretation, manuscript draft, revised the manuscript, and wrote the paper. K.B. participates in data collection, entry, and wrote reports. S.E. and B.T. participated in the analysis. All Authors read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ejeta Chibsa, S., Adem Hussen, M., Bayisa, K. et al. Determinants of low birth weight among newborns delivered at Mettu Karl comprehensive specialized hospital, southwest Ethiopia: a case–control study. Sci Rep 14, 4399 (2024). https://doi.org/10.1038/s41598-024-54248-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-54248-w
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.