Abstract
Neonatal mortality within the first few days of life is a pressing issue in sub-Saharan Africa, including Ethiopia. Despite efforts to achieve the targets set by the Sustainable Development Goals, the rate of neonatal mortality in Ethiopia has increased from 29 to 33 deaths per 1000 live births. This study aimed to investigate and identify significant determinants of neonatal mortality within the first 72 h of life in Ethiopia. Utilizing data from the 2019 Ethiopia Demographic and Health Survey, we employed Generalized Poisson regression analysis following rigorous model fitness assessment. Our study encompassed 5527 weighted live-born neonates. Among women in their reproductive years, 3.1% (n = 174) experienced at least one very early neonatal death. Multiple births (Incidence Risk Ratio (IRR) = 3.48; CI = 1.76, 6.887) and birth order six or above (IRR = 2.23; CI = 1.008, 4.916) were associated with an increased risk of neonatal death within the first 72 h. Conversely, household size (IRR = 0.72; CI = 0.586, 0.885) and additional feeding practices (IRR = 0.33; CI = 0.188, 0.579) were found to mitigate the risk of very early neonatal mortality per mother in Ethiopia. Interventions targeting the identified risk factors and promoting protective factors can contribute to reducing very early neonatal mortality rates and improving the well-being of mothers and their newborns. Further research and implementation of evidence-based strategies are needed to address these challenges and ensure better neonatal outcomes in Ethiopia.
Similar content being viewed by others
Introduction
Mortality in the neonatal period, spanning the first 28 days of life, is a crucial indicator of a population’s overall health and well-being, reflecting its socioeconomic status1. Despite significant global declines in neonatal mortality over the past few decades, developing countries continue to face substantial challenges in this area. In 2020, an estimated 5.0 million children under the age of five and 2.4 million infants lost their lives, with newborns accounting for half of these fatalities2. This alarming reality underscores the urgent need for research and intervention to address neonatal mortality, attracting the attention of academics, policymakers, and public health practitioners worldwide3.
Among the Sustainable Development Goals (SDGs) set forth by the United Nations is a specific target to reduce the neonatal mortality rate to 25 per 1000 live births by 20304. Achieving this ambitious goal hinges on effectively addressing neonatal mortality in high-risk countries, particularly in developing nations where 98% of neonatal deaths occur2.
Ethiopia, the second most populous nation in Africa, has witnessed a decline in both neonatal and under-five mortality rates. However, significant regional disparities persist, potentially attributed to variations in cultural practices, socioeconomic levels, and environmental conditions5,6.
Studies have consistently shown that approximately three-quarters of neonatal deaths occur within the first week of life, known as the early neonatal period7,8,9. This critical phase emphasizes the importance of concentrated efforts to improve neonatal survival during this vulnerable period. A concerning reality is that many neonatal deaths in underserved communities remain unrecorded or unregistered, as parents may not seek timely medical attention due to fear or lack of access to healthcare facilities10.
While researchers have dedicated efforts to understanding the causes of neonatal and perinatal mortality in Ethiopia, studies have largely overlooked a crucial aspect for policymakers: the distinct circumstances surrounding neonatal deaths within the first 72 h of life. This gap in knowledge hinders effective intervention strategies.
Our study addresses this critical gap by employing count regression models to analyze the impact of various factors on neonatal mortality within the first 72 h of life in Ethiopia. By identifying the individual risk factors associated with mortality, we aim to inform targeted interventions and improve neonatal survival outcomes.
Methods
Data source and preparation
This study utilized data from the 2019 Ethiopian Demographic and Health Survey (EDHS), the country’s second Mini Demographic and Health Survey (EMDHS) and fifth DHS overall. The survey, conducted by the Ethiopian Public Health Institute (EPHI) in collaboration with the Federal Ministry of Health, the Central Statistical Agency (CSA), and ICF, employed a nationally representative sample of 8663 households, or 8855 women of reproductive age (aged 15 to 49). Data collection took place between March 21 and June 28, 2019, generating estimates for both urban and rural areas, as well as at the national and regional levels. Comprehensive data on respondents’ background characteristics, fertility factors, marriage, family planning knowledge and practices, child feeding customs, children’s nutritional status, childhood mortality, and height and weight of infants aged 0–59 months were collected5. This study includes full survey results for Ethiopia’s nine regional states, two municipal administrations, and the country as a whole. The DHS website (http://dhsprogram.com) provides access to the datasets used in this study.
Study sample for this analysis, a total weighted sample of 5527 completed individual responses from mothers within the reproductive age group who were interviewed about neonatal deaths (deaths of newly born babies within the first 72 h of age) occurring in the preceding five years before the survey was included. Finally, the Ethiopian Public Health Institute’s rules and recommendations were rigorously followed for all methodological components used in this study.
Variables in the study
The dependent variable (Yi) for this study is the number of newborn infant deaths within the first 72 h of life that each mother has encountered throughout her reproductive life, and it is assumed to have values of 0, 1, 2, 3…. Explanatory variables (i.e., mortality determinants) are listed in Table 1 along with their definitions and categories (Table 1).
Operational definition
Very early neonatal mortality—deaths of the newly born babies before 72 h of their postnatal age recorded in the data set.
Additional feeding—provision of anything other than breast milk (such as, formula milk plain water, sugar water).
Risk fertility behavior—those mothers who have High-risk fertility behaviors too young (under age 18) or too old (over age 34), short birth interval (less than 24 months after the preceding birth), and high parity (more than three children).
Statistical method
When dealing with count data as the dependent variable, it is important to employ non-linear models that are based on non-normal distributions to describe the relationship with a group of predictor factors. Several widely used models for elucidating the association between an outcome variable and a set of explanatory variables in count data include Poisson regression, negative binomial regression, zero-inflated Poisson regression, zero-inflated negative binomial regression, and generalized Poisson regression models. These models are specifically designed to handle count data and offer effective means to analyze the relationship between the response variable and the predictors. By utilizing these models, researchers can accurately capture the complexities inherent in count data and gain valuable insights into the factors influencing the outcome variable.
Poisson regression
When our outcome is a count variable that we can assume will follow a Poisson distribution around a predicted mean, Poisson regression is appropriate. The definition of Poisson regression is as follows:
where the symbol ~ means ‘is distributed as’ That is, we assume that our count outcome, Yi, has a Poisson distribution with mean µi, where µi depends on the values of X1, X2,… and their coefficients. The outcome is usually log transformed, since this often better represents the relationships between the outcome and the predictors, compared to a model without a transformation. Equivalently, we can write the Poisson model equation as
We derive this equation by exponentiating both sides of the previous equation. In Poisson regression, we assume that the observed numbers of events follow a Poisson distribution around the predicted mean. This has some interesting implications. In particular, recall the Poisson distribution’s property of equi-dispersion: the variance is equal to the mean. This implies that in a Poisson regression we expect the observations to have a variance equal to their predicted mean. use the method of maximum likelihood to find the coefficient estimates11.
Negative binomial regression
When the assumption of equi-dispersion is not realistic – that is, if our outcome is over-dispersed a Poisson model may not be adequate. Instead, negative binomial regression model may best.
This negative binomial model looks very similar to a Poisson model. Again, we are using a logarithmic transformation of the outcome. The difference is that here we are expecting the observed numbers of events to follow a negative binomial distribution, rather than a Poisson distribution. Negative binomial distribution has two parameters, µ and α. Usually, only the mean µ is expected to be related to the predictors, but the dispersion parameter α is also estimated.vi The model must specify how we expect α to relate to the variance. Here I choose to specify that var (Yi) = μi + αμi2. This is called the NB2-parameterisation. At any rate, in negative binomial regression the predicted variance var (Yi) depends on both α and the predicted mean. This implies that we expect observations around the predicted mean to be heteroscedastic12.
Too many zeroes: zero-inflation
Sometimes we encounter situations where the count outcome we wish to model seems to follow a Poisson or a negative binomial distribution, except that the number of zeroes is much larger than expected under either of those models. In such a situation, statisticians say that the count variable has excess zeroes. Sometimes, a Poisson or negative binomial regression model can fit such data well this is the case if one of our covariates identifies a group of cases with a very low mean count, and if many of the zeroes come from this group. Then, although the outcome variable taken on its own seems to have excess zeroes, once the effects of the predictors have been taken into account, the distribution of counts around the predicted means follows a Poisson or negative binomial distribution well enough. However, there are many cases when a Poisson or negative binomial regression does not fit data with excess zeroes well. So, we need to consider models that are specifically designed for count data with excess zeroes. Two types of models are often used for this purpose: zero-inflated models and hurdle models11.
Models for outcomes with excess zeroes
Modelling an outcome with excess zeroes is a little more complicated than an ordinary count model. Such models consist of two parts:
-
One part predicts structural zeroes.
-
The other part predicts the remaining counts.
This section will introduce zero-inflated and hurdle models for both Poisson and negative binomial count distributions. As we will see, in both zero-inflated and hurdle models, we use logistic regression to predict structural zeroes. But the zero-inflated and hurdle models differ in how we model the counts:
-
In a zero-inflated model, the counts are modelled with a Poisson or negative binomial distribution, and predicted counts have a theoretical minimum of zero (because there can be sampling zeroes as well as structural zeroes).
-
In a hurdle model, the counts are modelled with a zero-truncated Poisson or zero-truncated negative binomial distribution, and predicted counts have a theoretical minimum of 1 (because there can be no sampling zeroes). Mathematically, a zero-inflated Poisson model can be expressed as follows:
$$\begin{aligned} & {\text{P}}\left( {{\text{Yi}} = 0} \right) = \pi {\text{i}} + \left( {1 - \pi {\text{i}}} \right){\text{e}} - \mu {\text{i}} \\ & {\text{P}}\left( {{\text{Yi}} = {\text{k}}} \right) = \left( {1 - \pi {\text{i}}} \right)\mu {\text{ike}} - \mu {\text{i}}/{\text{k}}!,{\text{k}} \ge 1 \\ \end{aligned}$$
The first equation describes the probability of observing zero events. This probability is the sum of the probability of a structural zero (πi) and the probability of a sampling zero [(1 − πi) e − μi]. The second equation describes the probability of observing 1, 2, 3,… or more events11,13.
Generalized Poisson distribution (GPD)
Generalized Poisson distribution (GPD) was introduced by Consul and Jain as a limiting form of the generalized negative binomial (GNB) distribution. The GNB parameters are defined such that a Poisson distribution with two parameters is produced, in which one of them is as a dispersion parameter. With the additional of dispersion parameters, the GPD can accommodate overdispersion or under dispersion in the Poisson distribution14. Means and variance of Generalized Poisson distribution are E(Y) = µ and var(Y) = µ (1 + ά µ)2. If the value of ά is zero then the model formed is Poisson regression. If the value of ά greater than zero then it called over dispersion, while the value of ά less than zero then it called under dispersion. The method that used for estimate parameter of GPR model is Maximum Likelihood Estimation (MLE) with the combination of Newton–Raphson iteration15.
Investigating over dispersion and model comparison
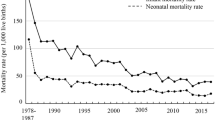
In Fig. 1, it is observed that the sample mean of the response variable, which represents the number of very early newborn infant deaths, is 0.05, while the sample variance is 0.1225 (standard deviation squared = 0.35). The fact that the mean is less extreme than the variance indicates an over dispersion situation. Furthermore, due to the presence of extra zeros in the data and the skewed nature of the data, it is expected that the Poisson model would not be suitable for accurately predicting the number of deaths.
To compare different models, the log likelihood, Akaike’s Information Criterion (AIC), and Bayesian Information Criterion (BIC) were utilized (reference 11). Based on the findings, the generalized Poisson regression model was determined to be the most appropriate count data model for this dataset (Table 2).
Ethical approval
Ethical approval for this study was waived by ethical review board of Institute of Public Health, College of Medicine and Health Sciences, Wollo University and DHS International Program because all of the secondary data used in this study were collected from publicly available sources and lacked any personal information that might be used to identify specific people, groups, or study participants. Anonymity was used to ensure data confidentiality.
Results
Descriptive statistics
Among the 5527 weighted live births included in the study, 3.1% (n = 174) of newborns died within the first 72 h of life (Table 3). This represents over half (52.3%) of all neonatal deaths occurring within the five-year period covered by the survey. The proportion of very early neonatal mortality was slightly higher among males (2.4%) compared to females (2.2%). Additionally, nearly half (49.4%) of uneducated mothers experienced at least one very early neonatal death, and participants with risky fertility behaviors during pregnancy were more likely to have multiple deaths within the first 72 h of delivery (62.1%) (Table 3).
Results of the generalized poisson regression analysis
Results in Table 4 provide estimates of the effect of some selected variables for very early mortality of newly born babies. Accordingly, among the predictors in the final model number of household member, multiple birth, taking additional feeding and higher birth order were the major predictors for mortality among newly born babies within the first seventy-two hours of their postnatal age per mother in Ethiopia. The expected number of very early neonatal deaths increased by a factor of 2.23 (IRR = 2.23; CI = 1.008, 4.916) for those birth order six and above compared to second to fifth birth order after controlling for other variables in the model. Similarly, expected number of mortalities in women who gave twin birth increased by a factor of 3.48 times compared to those gave single birth controlling for other variables in the model (IRR = 3.48; CI = 1.76, 6.887). These finding indicate that the risk of very early neonatal mortality decreases with each additional household member increment lived at the time of giving birth (IRR = 0.72; CI = 0.586, 0.885). Moreover, risk of early neonatal mortality for those babies got an additional feeding after birth was 77% less likely to die before seventy-two hours of age as compared to counterparts keeping other variables held constant in the model (IRR = 0.33; CI = 0.188, 0.579).
Discussion
We conducted an investigation into the factors that contribute to the high mortality rate among newborn infants in Ethiopia within the first few days of life. Our findings revealed that several factors, including the number of household members, multiple births, additional feeding, and birth order, were associated with an increased risk of death. This study is the first of its kind to examine the determinants of mortality within the first three days of life in Ethiopia, providing valuable insights for policymakers to identify areas of improvement and track progress towards achieving the Millennium Development Goals (MDGs).
Our research confirmed that the risk of mortality within the first 72 h of life is higher for twins or multiple births compared to single births, which is consistent with previous studies7,16,17,18. Multiple births are often linked to premature birth, low birth weight, and biological immaturity, which increase the likelihood of adverse outcomes, including early newborn mortality19.
Additionally, birth order was found to be a significant predictor of infant death within the first 72 h of life, similar to findings from other studies7,18,20,21. The biological depletion hypothesis suggests that children born later may be less healthy than their older siblings due to being born to older mothers who have already given birth to multiple children and may be less physiologically capable of producing healthier offspring. However, there is evidence to suggest that first-born babies are also vulnerable to illness and death, as they are typically born to younger and less experienced mothers who may lack the necessary resources for adequate care22,23.
Furthermore, our study revealed that an increase in the size of the household was associated with a higher risk of very early neonatal mortality, consistent with previous findings21,24,25. This could be attributed to a reduction in parent–child emotional and physical attachments, which are crucial for promoting survival23. Additionally, larger family sizes may lead to food insecurity, resulting in poor maternal nutrition and adverse birth outcomes, including neonatal mortalities26.
Another significant factor associated with very early newborn mortality was the initiation of additional feeding. Our findings indicated that newborns who received additional feeding were less likely to die within the first three days of life compared to those who did not receive it. While breastfeeding is known to offer protection against mortality and disease, additional feeding may be beneficial in reducing very early neonatal deaths, particularly by preventing complications associated with hypoglycemia and hypothermia caused by delayed breastfeeding initiation and inadequate breast milk production in the initial days27,28.
In general, developing countries like Ethiopia tend to experience higher mortality rates among newborns within the first 72 h of life due to challenges in adapting to extra uterine life. Based on the 2019 mini-Ethiopian Demographic and Health Survey data, our study identified an increased number of household members, multiple births, additional feeding, and birth order six and above as significant predictors of mortality among newborns within the first 72 h of life per mother.
In conclusion, this study aimed to identify the key predictors of very early neonatal mortality using count regression models in Ethiopia. It utilized recent nationally representative data from the 2019 mini-Ethiopian Demographic and Health Survey. Out of 5527 weighted live births that occurred within five years preceding the survey, 174 (3.1%) experienced at least one very early neonatal mortality. These deaths accounted for 52.3% of all deaths among children under five. To reduce this high mortality rate, further efforts should focus on addressing the factors identified in this study, including the number of household members, multiple births, additional feeding, and higher birth order. Additionally, future studies should consider more detailed recommendations for practical interventions and strategies that can be implemented to reduce very early neonatal mortality in Ethiopia. Policymakers should carefully consider the policy implications of these findings and develop targeted approaches that address the specific needs of the population, taking into account socio-demographic characteristics, women’s empowerment, and partner education.
The strengths of this study lie in its use of a recent nationally representative dataset (2019 mini-EDHS) and the application of sampled weights and a well-fitted model (Generalized Poisson regression) to identify determinants of very early neonatal death in Ethiopia. However, it is important to note that this study relied on secondary data, and some variables were not included due to high rates of missing values, such as the number of antenatal visits, preceding birth interval, and breastfeeding initiation. As a cross-sectional survey, causality cannot be established, and there may be uncertainty regarding temporal associations.
Data availability
This study used 2019 mini EDHS child data set and extracted the outcome and explanatory variables. The datasets generated and analyzed in this study is not publicly available but can be obtained upon justifiable request from the corresponding author.
Abbreviations
- ANC:
-
Antenatal care
- C/S:
-
Cesarian section delivery
- CI:
-
Confidence interval
- EDHS:
-
Ethiopia Demographic and Health Survey
- EMDHS:
-
Ethiopia Mini Demographic and Health Survey
- ICF:
-
International classification of functioning, disability, and health
- MDGs:
-
Millennium development goals
- Sd:
-
Standard deviation
- SNNPR:
-
Southern nation nationalities and peoples region
References
Tessema, G. A., Berheto, T. M., Pereira, G., Misganaw, A. & Kinfu, Y. National and subnational burden of under-5, infant, and neonatal mortality in Ethiopia, 1990–2019: Findings from the global burden of disease study 2019. PLOS Glob. Public Health 3(6), e0001471 (2023).
David, S., Lucia, H., Sinae Lee, Y.L., & D.Y. Levels & Trends in Child mortality (UNICEF and UN IGME) (2021).
United Nations Children’s Fund. Health results 2021 maternal, newborn and adolescent health (2021).
Nations, U., Affairs, S. & Division, P. World Mortality (2017).
Ethiopian Public Health Institute E. Ethiopia mini demography and health survey (2021).
Yohannis, H. K., Fetene, M. Z. & Gebresilassie, H. G. Identifying the determinants and associated factors of mortality under age five in Ethiopia. BMC Public Health 21(1), 1–11 (2021).
Muhammed, G. et al. Determinants of early neonatal mortality in Afghanistan: An analysis of the Demographic and Health Survey 2015. Glob. Health 14, 1–12 (2018).
Shayo, A. et al. Early neonatal mortality is modulated by gestational age, birthweight and fetal heart rate abnormalities in the low resource setting in Tanzania–a five year review 2015–2019. BMC Pediatr. 22(1), 313 (2022).
Aragaw, A. M., Azene, A. G. & Workie, M. S. Poisson logit hurdle model with associated factors of perinatal mortality in Ethiopia. J. Big Data 9(1), 1–11 (2022).
Lawn, J. E., Cousens, S. & Zupan, J. Neonatal survival 1 4 million neonatal deaths: When? Where? Why?. Lancet 365(9462), 891–900 (2005).
Martin, P. Regression Models for Categorical and Count Data 215–217 (SAGE Publications Ltd, 2021).
Hilbe, J. M. Negative Binomial Regression 68–72 (Cambridge University Press, 2011).
Vieu, W. H. & Mori, Y. Statistical Methods for Biostatistics and Related Fields (Springer, 2006).
Berliana, S. M. & Rahayu, S.P. Multivariate generalized Poisson regression model with exposure and correlation as a function of covariates: Parameter estimation and hypothesis testing multivariate generalized Poisson regression model with exposure and correlation as a function of Cova. in AIP Conference Proceedings (2021).
Prahutama, A., Ispriyanti, D., Warsito, B. Modelling generalized Poisson regression in the number of dengue hemorrhagic fever (DHF) in East Nusa Tenggara. in E3S Web of Conferences (2020).
Mulugeta, S. S., Muluneh, M. W., Belay, A. T. & Moyehodie, Y. A. Multilevel log linear model to estimate the risk factors associated with infant mortality in Ethiopia: Further analysis of 2016 EDHS. BMC Pregnancy Childbirth 22, 597 (2022).
Basha, G. W., Woya, A. A. & Tekile, A. K. Determinants of neonatal mortality in Ethiopia: An analysis of the 2016 Ethiopia Demographic and Health Survey. Afr. Health Sci. 20(2), 715–723 (2020).
Alamirew, W. G., Belay, D. B. & Zeru, M. A. Prevalence and associated factors of neonatal mortality in Ethiopia. Sci. Rep. 12(1), 12124 (2022).
Martin, R. J., Fanaroff, A. A. & Walsh, M. C. (2016) Fanaroff And Martin’s neonatal-Perinatal Medicine 10th edition Diseases of the Fetus and Infant. 1074–1086.
Mulugeta, S. S. & Wassihun, S. G. Determinant of infant mortality in Ethiopia: Demographic, socio economic, maternal and environmental factors. MOJ Women’s Health 11(2), 49–57 (2022).
Ali, E. A. & Tilahun, T. Count models for identifying factors associated with child mortality in Ethiopia. Res. Sq. https://doi.org/10.21203/rs.3.rs-222761/v1 (2021).
Lundberg, E., Svaleryd, H. Birth Order and Child Health (2016).
Julihn, A., Soares, F. C., Hammarfjord, U., Hjern, A. & Dahllöf, G. Birth order is associated with caries development in young children: A register-based cohort study. BMC Public Health 20(1), 1–8 (2020).
Li, Z., Kapoor, M., Kim, R. & Subramanian, S. V. Association of maternal history of neonatal death with subsequent neonatal death across 56 low-and middle-income countries. Sci. Rep. 11(1), 19919 (2021).
Ekholuenetale, M., Wegbom, A. I., Tudeme, G. & Onikan, A. Household factors associated with infant and under–five mortality in sub–Saharan Africa countries. Int. J. Child Care Educ. Policy 14, 1–15 (2020).
Campbell, A. A. et al. Relationship of household food insecurity to neonatal, infant, and under-five child mortality among families in rural Indonesia. Food Nutr. Bull. 30(2), 112–119 (2009).
Derebe, K., Id, F., Muche, S., Id, F. & Biresaw, H. B. Factors associated with post-neonatal mortality in Ethiopia: Using the 2019 Ethiopia mini demographic and health survey. Plos one 17(7), e0272016 (2022).
Kliegman, R. et al. (eds). Nelson textbook of Pediatrics. 21th Ed, 3944–60 (2020).
Acknowledgements
We thank the Central Statistical Agency (Ethiopia) for granting us permission to utilize the results of the 2019 Ethiopia Demographic and Health Survey.
Funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
F.B.G. and A.G. conceived and design the idea, participated in the data collection process, analyze data, and wrote the paper. A.A., T.A., and A.M. participated in data analysis and wrote the paper. L.D. extensively reviewed the manuscript and incorporated intellectual input. All authors approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Getaneh, F.B., Belete, A.G., Ayres, A. et al. A generalized Poisson regression analysis of determinants of early neonatal mortality in Ethiopia using 2019 Ethiopian mini demographic health survey. Sci Rep 14, 2784 (2024). https://doi.org/10.1038/s41598-024-53332-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-53332-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.