Abstract
Matrix metalloproteinases (MMPs) are proteolytic zinc-endopeptidases regulated by tissue Inhibitors of matrix metalloproteinases (TIMPs). We evaluated the potential of MMPs and TIMPs as clinical tools for Intracranial Haemorrhage (ICH). Spontaneous non‐traumatic ICH patients were recruited from two hospitals: Complejo Hospitalario de Navarra (CHN = 29) and Vall d´Hebron (VdH = 76). Plasmatic levels of MMP-1, −2, −7, −9, −10 and TIMP-1 and their relationship with clinical, radiological and functional variables were evaluated. We further studied the effect of TIMP-1 (0.05–0.2 mg/Kg) in an experimental tail-bleeding model. In CHN, TIMP-1 was associated with admission-hematoma volume and MMP-7 was elevated in patients with deep when compared to lobar hematoma. In VdH, admission-hematoma volume was associated with TIMP-1 and MMP-7. When data from both hospitals were combined, we observed that an increase in 1 ng/ml in TIMP-1 was associated with an increase of 0.14 ml in haemorrhage (combined β = 0.14, 95% CI = 0.08–0.21). Likewise, mice receiving TIMP-1 (0.2 mg/Kg) showed a shorter bleeding time (p < 0.01). Therefore, the association of TIMP-1 with hematoma volume in two independent ICH cohorts suggests its potential as ICH biomarker. Moreover, increased TIMP-1 might not be sufficient to counterbalance MMPs upregulation indicating that TIMP-1 administration might be a beneficial strategy for ICH.
Similar content being viewed by others
Introduction
Stroke is the second leading cause of death and disability worldwide1. Intracranial hemorrhage (ICH), accounting for 10–15% of all strokes, is the most devastating subtype2. However, unlike ischemic stroke, the incidence of ICH has not declined over the last decades3 and no specific treatments have been developed4. Almost 40% of ICH patients will die within the first 30 days and only 20% of survivors will achieve independent functionality5.
ICH is a complex disease characterized by blood vessel rupture and extravasation into brain parenchyma, leading to hematoma expansion, ischemia and neuronal loss6. The most common ICH are either lobar or deep in location and differ in admission hematoma volume, hematoma growth and outcome7. Several factors are involved in the ICH pathophysiology including: (a) the remodeling of the extracellular matrix (ECM) which in physiological conditions maintains the integrity, elasticity and strength of the arterial wall, (b) the breakdown of the blood-brain barrier (BBB) which contributes to edema formation and neuronal degeneration and (c) the inflammatory responses involved in secondary brain injury8,9.
Matrix metalloproteinases (MMPs) are zinc-dependent endopeptidases with proteolytic activity that contribute to ECM degradation, tissue remodeling and regeneration10. The catalytic activity of MMPs is regulated by tissue inhibitors of matrix metalloproteinases (TIMPs)11. The four members of the TIMP family (TIMP 1–4) are broad spectrum inhibitors that directly bind to the catalytic domain of MMPs12.
After brain injury, the role of MMPs and their inhibitors may be critical, since both participate in early acute injury along with tissue recovering during later stages13. Clinical studies have observed increased MMP-2, −3, −9 and TIMP-1 levels in blood and cerebrospinal fluid of ICH patients when compared to normal population14,15, suggesting that MMPs/TIMPs are likely to be involved in brain injury after spontaneous ICH and may be associated with patients’ outcome16. In the last years our group has studied the role of MMPs in different neurovascular diseases. We showed that TIMP-1 levels were associated with mortality in patients with traumatic brain injury and malignant middle cerebral artery occlusion17,18,19, while MMP-2 expression might be implicated in the development of amyloid angiopathy in ICH patients20. Moreover, MMPs have been related to hematoma expansion, edema growth and neuronal loss in extensive pre-clinical studies16. However, their potential as therapeutic or diagnostic clinical tools has not yet been fully identified.
In this study, we explored the plasmatic levels of several MMPs and TIMP-1 and their relationship with hematoma volume and location as well as with other clinical, radiological and functional variables in two independent cohorts of ICH patients. In addition, we further studied the effect of TIMP-1 in an experimental tail-bleeding model.
Results
Clinical and demographic characteristics according to hematoma location
Clinical and demographic characteristics of both cohorts according to hematoma location at admission and follow-up data are shown in Tables 1 and 2.
In the CHN cohort (Table 1), the median [interquartile range, IQR] age was 76 [66–85] years, almost 40% were female, 52% had hypertension and the severity of the stroke was moderate (median [IQR], NIHSS = 8 [4–17]). Ninety days after ICH, the mortality rate reached 33% (n = 9) and survivors were moderate to severely disabled (mRS = 4 [2–6]). Patients with lobar ICH (n = 16, 55%) had larger hematoma volumes at admission when compared to deep location (38 [19–69] mL lobar vs. 8 [4–17] mL deep, p < 0.001), and 24–48 hours after ICH onset (42 [23–58] mL lobar vs. 9.4 [3.6–18] mL deep, p = 0.004). There was a tendency to a higher prevalence of hypertension (dichotomized) in patients with deep hematoma (p = 0.089). Only MMP-7 levels were higher in patients with deep hematoma when compared to lobar (median [IQR], 21.1 [15.5–24.3] ng/mL deep vs. 15.3 [13.0–19.0] ng/mL lobar, p = 0.048). We did not find differences on functional outcomes, mortality or the rest of MMPs and TIMP-1 between these two ICH locations (Table 1).
In the VdH cohort (Table 2), the median [IQR] age of ICH patients was 72 [66–80] years, nearly 44% were female, almost 90% presented hypertension and stroke severity ranged from moderate to severe (median [IQR], NIHSS = 12 [6.7–19.2]). Ninety days after ICH, mortality rate was 31% (n = 21) and survivors presented moderate to severe disability (mRS = 4 [2–6]). ICH location was lobar in 28 patients (37%) and deep in 48 (63%). As reported for the CHN cohort, hemorrhage volumes were also larger in patients with lobar hematoma when compared to deep location at admission (43.7 [15.55–77] mL lobar vs.5.8 [3.25–19.27] mL deep, p = 0.0001) and 24–48 hours after ICH (39 [20.2–48.11] mL lobar vs. 5.7 [3.3–14.8] mL deep, p = 0.0015). Furthermore, the prevalence of hypertension was higher in patients with deep hematoma when compared to lobar (94% deep vs. 75% lobar, p = 0.047), while glucose levels were lower (124 [108–147.75] deep vs. 141.5 [116.75–216.5] mg/mL lobar, p = 0.036). No significant association of hematoma location was observed with any of the functional outcomes, mortality, MMPs or TIMP-1 (Table 2).
Association of MMPs and TIMP-1 with clinical and radiological variables
We performed a univariate analysis to assess the relationship between plasma MMPs and TIMP-1 and clinical and radiological variables (Tables 3 and 4).
First in the CHN cohort, the MMPs studied were not associated with either cardiovascular risk factors, functional outcomes or mortality (Supplemental Table 1). However, TIMP-1 levels were positively associated with admission hematoma volume (0.19; 95% CI 0.09 to 0.28 p = 0.001, Table 3). We also assessed the association between admission hematoma volume and different clinical and radiological parameters. Admission NIHSS (2.8; 95% CI 1.1 to 4.4, p = 0.002), 90-days mortality (46; 95% CI 12.5 to 79.5, p = 0.009) and ventricle’s blood (44.2; 95% CI 12.2 to 76.2, p = 0.008) were positively associated with admission hematoma volume. Moreover, patients with a lobar location had a significantly higher hemorrhage volume than patients with a deep location (43.7; 95% CI 14.5 to 72.8, p = 0.005). Hypertensive patients showed lower hematoma volume (−32.2; 95% CI -63.4 to −0.94, p = 0.044, Table 3).
In the VdH cohort, MMP-2 levels were associated with age (0.95; 95% CI 0.27 to 1.63, p = 0.007), mRS 90 days (3.8; 95% CI 0.48 to7.07, p = 0.025), hypertension and 90-days mortality (OR = 1.032, 95% CI 1.002 to 1.064, p = 0.039 and OR = 1.025, 95% CI 1.003 to 1.048, p = 0.027, respectively). MMP-10 levels were associated with age (11.7; 95% CI 1.4 to 21.9, p = 0.025) and diabetes (OR = 1.001, 95% CI 1.000 to 1.003, p = 0.021), and MMP-9 levels were lower in female patients (−59.9; 95% CI −98.1 to −7.7, p = 0.022, Supplemental Table 2). Moreover, we again observed that admission hematoma volume was positively associated with TIMP-1 levels (0.17; 95% CI 0.03 to 0.32, p = 0.022, Table 4) but also with MMP-7 levels (0.83; 95% CI 0.32 to 1.34, p = 0.002, Table 4). Regarding the association between admission hematoma volume and other clinical and radiological parameters, we found a positive association of this variable, with glucose levels (0.25; 95% CI 0.1 to 0.41 p = 0.0021), age (1.3; 95% CI 0.4 to 2.3, p = 0.007), mortality (48.7; 95% CI 29.4 to 68.0, p < 0.001) and with admission NIHSS (2.05; 95% CI 0.99 to 3.11, p < 0.001). Again, patients, with lobar location had a significantly higher hemorrhage volume than patients with a deep location (46.2; 95% CI 29.9 to 62.6, p < 0.001). Hypertensive patients showed lower hematoma volume (−28.94; 95% CI −55.1 to −2.78, p = 0.033, Table 4).
TIMP-1 as a potential biomarker for hematoma volume
We aimed to further analyze the association of plasmatic TIMP-1 with the volume of hemorrhage at admission observed in both cohorts by multivariate regression analysis.
First, in the CHN cohort, the multivariate analysis showed a significant association of TIMP-1 and hemorrhage volume after adjusting for confounding factors in all tested models (models 1 to 3, Table 5). This association was further confirmed in the VdH cohort in both, the univariate and the multivariate analysis (Table 6).
When we combined the results from the two cohorts, we observed a statistically significant association between TIMP-1 and hematoma volume (Overall β = 0.14, 95% CI = 0.08–0.21, Fig. 1). These results suggest that TIMP-1 might be a potential biomarker for ICH.
TIMP-1 effects in experimental haemorrhage
After finding an association between hematoma volume and TIMP-1, we further explored the effects of TIMP-1 in an experimental model of tPA-induced haemorrhage. Our results showed that an experimental dose of TIMP-1 (0.05 mg/Kg) did not decrease the maximum bleeding time allowed (30 minutes). However, mice injected with the highest dose of TIMP-1 (0.2 mg/Kg), showed a much shorter bleeding time (1.8 ± 0.7 vs. 28.3 ± 3.3 min, p < 0.01, Fig. 2a) and blood lost (15.3 ± 4.7 vs. 42.8 ± 14.9 μL, p < 0.05, Fig. 2b). These results suggest that TIMP-1 might be able to control experimental haemorrhage.
Discussion
The main objective of this study was to explore the relationship of MMPs and TIMP-1 with clinical, radiological and functional variables in two independent cohorts of ICH patients. Hematoma volume and expansion have been associated with poor prognosis, neurological detriment and disability after ICH21. We reported for the first time that circulating levels of TIMP-1 at admission are associated with hematoma volume independently of hypertension, NIHSS and hematoma location in two independent cohorts of ICH patients.
TIMP-1 is an endogenous inhibitor of MMPs present under normal conditions in tissues to regulate MMPs activity22. Studies addressing the role of TIMP1 in ICH are scarce. In this study, we report that TIMP-1 is significantly associated with hematoma volume in two independent cohorts, and after a combined meta-analysis, suggesting that TIMP-1 might be potential critical biomarker in ICH. These results are in agreement with other studies showing increased concentrations of TIMP-1 during the acute phase of ICH, that remained highly sustained during the first week after stroke onset23, and showing TIMP-1 association with early mortality rates24, supporting a potential role of TIMP-1 as severity biomarker in ICH. The elevated secretion of TIMP-1 might be induced to lessen MMPs activity and thus, to prevent further brain damage25. However, it might not be enough to counterbalance the concomitant upregulation of MMPs. Likewise, it has been reported a relative increase in MMP-9/TIMP-1 ratio associated with symptomatic ICH26 and Subarachnoid Haemorrhage (SAH)27 supporting the hypothesis that perturbations in MMPs/TIMPs levels may contribute to the matrix disruption associated with cerebral aneurysms28.
Additionally, we found that administration of TIMP-1 (approximately 10-fold circulating levels) is able to control experimental acute bleeding in mice. These findings are consistent with the overall idea that in conditions of brain haemorrhage, damage, and inflammation, there may be an imbalance in the dynamic equilibrium between MMPs and TIMPs, so that any way of enhancing the inhibitor side of the equation might be beneficial29,30. Supporting this hypothesis, previous data in TIMP-1 knockout mice showed exacerbated BBB disruption and brain injury31, while adenoviral TIMP-1 overexpression in mice, reduced brain lesion volume, neuronal damage and BBB leakage after ischemia32. Moreover, MMP inhibitors significantly decreased bleeding and brain damage in experimental models of haemorrhage, including ICH33,34.
One of the main factors that influences ICH outcome is the hematoma location; deep and lobar predominantly35 that usually results in different hematoma volumes. Despite the relevance of this parameter for ICH outcome, there are few clinical data regarding the association of MMPs with hematoma location. Abilleira et al. reported higher MMP-9 plasmatic levels in patients with deep-associated ICH36. Moreover, in cerebral amyloid ICH, typically located in lobar regions, MMP-2 and -9 were up-regulated in perihematomal area of the brains20,37. In our study, CHN patients with deep hematoma location showed elevated plasmatic MMP-7 levels compared to patients with lobar hematoma. MMP-7/matrilysin is a small, secreted metalloproteinase capable of digesting a large series of proteins of the extracellular matrix38. A recent population-based cohort study followed for more than 10 years, reported that high serum levels of MMP-7 were independently associated with increased risk of incident spontaneous SAH suggesting its possible use as a predictive marker for SAH39. Likewise, several studies with MMP-7 null mice indicated that the robust expression of MMP-7 during severe inflammation lead to irreparable tissue damage40. Furthermore, we observed an association of this metalloprotease with hematoma volume in the VdH cohort. Therefore, our results suggest that MMP-7 might be involved in the pathophysiology of deep-ICH although it may be partly dependent on risk factors, therefore, further studies must be performed to confirm these data.
Other associations found in this study, such as MMP-10 with age and diabetes and MMP-2 with age, hypertension and 90-days mortality, were only significant in VdH possibly explained by larger sample size and statistical power of this cohort. However, these associations were lost after adjusting for risk factors of ICH. Previous data about the association of high MMP-10 levels with microvascular complications in diabetes type 1 in clinical and experimental studies41,42 could explain the association found in ICH patients. Regarding MMP-2, several studies support the association of MMP-2 with hypertension and mortality in diabetic patients and in patients with heart failure43,44. However, concerning spontaneous ICH patients, elevated levels of MMP-2 were only found at admission decreasing during the first 24 hours of hospitalization23 and, specifically at tissue level in β-amyloid-damaged vessels located far from the acute ICH20. Therefore, future studies with larger sample size might confirm these data.
Our work has several limitations: first the small sample sizes of our series make our results to be interpreted carefully. Therefore, data from this study should be confirmed in larger cohorts before definitive clinical conclusions can be drawn. The observational study design did not allow us to establish a cause-effect relationship between TIMP-1 and hematoma volume, although the effect of TIMP-1 reducing bleeding time in an experimental model of tail bleeding supports the hypothesis that TIMP-1 could be a promising strategy to control hematoma volume in ICH. However, further experimental models of ICH using deficient mice might be performed.
Conclusion
We report for the first time that circulating TIMP-1 is associated with hematoma volume in two independent ICH cohorts and when we combined the results from both cohorts suggesting the potential of TIMP-1 as biomarker for ICH. Additionally, TIMP-1 administration significantly reduces experimental bleeding. Therefore, it could be considered that after ICH increased TIMP-1 levels might not be sufficient to counterbalance the upregulation of MMPs, and that its exogenous administration could be a beneficial strategy for ICH in order to reduce MMPs activity and restore the MMPs/TIMPs balance.
Materials and methods
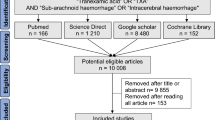
Study populations
Spontaneous non‐traumatic ICH patients were recruited from two different Spanish tertiary hospitals (Tables 1 and 2): a cohort from Complejo Hospitalario de Navarra (CHN, n = 29), collected between February 2016 and June 2017; and a larger cohort of patients (n = 76) from Hospital Universitario Vall d’Hebron (VdH) collected between August 2012 and December 2013. These prospective studies were approved by the ethics committee of the Navarra Government (63/2015) and the Catalonia Government [PR(AG)157–2011] respectively. All patients or their “legally authorised representative” provided written informed consent according to Helsinki declaration. The study included only patients with spontaneous nontraumatic supratentorial intracerebral hemorrhage (ICH), diagnosed by experienced neurologists of the Stroke Unit by initial cranial non-contrast computed tomography (CT) at admission in the emergency department. Patients with brainstem/infratentorial ICH and/or secondary ICH (vascular malformation, aneurysm, tumors, ischemic stroke with haemorrhagic transformation) were excluded. We excluded other causes of intracranial haemorrhages, as subdural hematoma, epidural bleeds, and subarachnoid hemorrhage. However, we included patients who had suffered subarachnoid and intraventricular haemorrhage (IVH), although always associated with concurrent parenchymal hematoma. Systemic cancer and inflammatory systemic condition patients were also excluded from the study. ICH was classified by its location by experienced neurologist as previously reported by Aguilar I et al.45. Demographics and previous antiplatelet and/or anticoagulation therapy were registered. Reversal of anticoagulation was indicated in some patients according to current guidelines.
Radiologic measurements
The primary radiologic outcomes were hemorrhage volume (admission volume and after the following 24–48 hours), hematoma location, hematoma expansion (more than 6 mL or 33% growth during the first 24 hours) and IVH. Hematoma volume was quantified by using the ABC/2 method46,47. This well-validated method, consist on measuring the greatest axial dimension of the hematoma (A), a perpendicular diameter on the same slice (B), and the cranio-caudal dimension (C) estimated by counting the number of slices where the hematoma is present and multiplying that number by the slice thickness. The hematoma volume is estimated by multiplying these three dimensions together and dividing by 2, which estimates the simplified volume of an ellipse.
Neurological and functional outcomes
Clinical severity was assessed at admission using the National Institute of Health Stroke Scale (NIHSS)48 and initial prognosis was evaluated by ICH score49. Functional outcome was defined by modified Rankin Scale (mRS)50 and mortality rates at 90 days after onset to evaluate the mid-term outcome of patients. Previous functional situation evaluated by mRS was registered at admission.
Sample collection
Citrated plasma samples of venous blood were obtained from both study cohorts at the moment of hospitalization (admission). All samples were processed within 4 hours of collection and stored at −80 °C. Samples were thawed on ice and thoroughly vortexed prior to beginning any experiment. Plasma MMP-1, −2, −7, −9, −10 were measured with MAP Human MMP panel 2 (Milliplex, Millipore, Darmstadt, Germany) in a Luminex 200 platform (Luminex technology, Comercial Rafer S.L., Spain) and TIMP-1 was measured with ELISA kit for TIMP-1 (R&D Systems, Minneapolis, US) in an automated ELISA system (Triturus, Movaco, Spain). All experiments were performed according to manufacturer´s instructions by blinded investigators.
Bleeding assay
Bleeding assay was performed in 5-week-old male C57/BL6J mice (n = 12, Envigo, Spain). All experiments in this study were conducted according to the European Community guidelines for the ethical animal care and use of laboratory animals (2010/63/EU) and approved by the University of Navarra Animal Research Review Committee (ref. 46,12). The experimental protocol is shown in Supplemental Fig. 1. Briefly, animals were anesthetized with 2.5% isoflurane, placed in prone position and tPA (0.05 mg/Kg) was injected through the ocular plexus. Five minutes later, TIMP-1 (0.05 and 0.2 mg/Kg) or saline were injected through the femoral vein catheter (10% bolus and 90% perfusion during 40 minutes). A distal 5 mm segment of the tail was transected with a scalpel blade 5 minutes after starting the treatments. The tail was immediately immersed in a tube containing pre-warmed saline (37 °C in a water bath). Bleeding time was defined as the time elapsed until bleeding stops for a maximum of 30 min. Blood lost was defined as the amount of blood collected during 30 min and absorbance was measured in a spectrophotometer (Tecan Sunrise, Switzerland) and quantified against a standard curve generated with known quantities of blood33.
Statistical analysis
Descriptive statistics (median, interquartile range, frequency and percentage) were defined for all clinical, radiological and functional variables. Normality was assessed using the Shapiro-Wilk test. Bivariate comparisons of characteristics at admission between ICH location (deep and lobar index ICH) were performed using Student t test or Mann-Whitney U test for continuous variables, and χ2 test or Fisher exact test for categorical variables. All covariates associated with the end point in the univariate analysis, considering a threshold of p < 0.1 in both cohorts, were included in the multivariate linear regression analyses for the target molecules of the study (MMPs and TIMP-1). Due to the small sample size in one of the cohorts, the following baseline models were considered for adjustment: model 1, TIMP-1, location, and hypertension (yes/no); and model 2, TIMP-1, location and NIHSS. Finally, we conducted a fixed effect meta-analysis to combine the data from our two cohorts in a meta-analysis. Statistical analysis of the data from experimental model was done using Mann-Whitney U two-tailed test.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Dichgans, M., Pulit, S. L. & Rosand, J. Stroke genetics: discovery, biology, and clinical applications. The Lancet Neurology. https://doi.org/10.1016/S1474-4422(19)30043-2 (2019).
Al-Shahi Salman, R. et al. Absolute risk and predictors of the growth of acute spontaneous intracerebral haemorrhage: a systematic review and meta-analysis of individual patient data. Lancet Neurol. https://doi.org/10.1016/S1474-4422(18)30253-9 (2018).
Selim, M. Unmet needs and challenges in clinical research of intracerebral hemorrhage. Stroke. https://doi.org/10.1161/STROKEAHA.117.019541 (2018).
Hanley, D. F. et al. Efficacy and safety of minimally invasive surgery with thrombolysis in intracerebral haemorrhage evacuation (MISTIE III): a randomised, controlled, open-label, blinded endpoint phase 3 trial. Lancet. https://doi.org/10.1016/S0140-6736(19)30195-3 (2019).
Ziai, W. C. et al. A randomized 500-subject open-label phase 3 clinical trial of minimally invasive surgery plus alteplase in intracerebral hemorrhage evacuation (MISTIE III). Int. J. Stroke. https://doi.org/10.1177/1747493019839280 (2019).
Urday, S. et al. Targeting secondary injury in intracerebral haemorrhage-perihaematomal oedema. Nature Reviews Neurology. https://doi.org/10.1038/nrneurol.2014.264 (2015).
Biffi, A. et al. Association between blood pressure control and risk of recurrent intracerebral hemorrhage. JAMA - J. Am. Med. Assoc. https://doi.org/10.1001/jama.2015.10082 (2015).
Alg, V. S. et al. Association of functional MMP-2 gene variant with intracranial aneurysms: case-control genetic association study and meta-analysis. Br. J. Neurosurg. https://doi.org/10.1080/02688697.2018.1427213 (2018).
Zhang, X. et al. Matrix metalloproteases-mediated cleavage on β-dystroglycan may play a key role in the blood–brain barrier after intracerebral hemorrhage in rats. Med. Sci. Monit. https://doi.org/10.12659/MSM.908500 (2019).
Purroy, A. et al. Matrix metalloproteinase-10 deficiency delays atherosclerosis progression and plaque calcification. Atherosclerosis. https://doi.org/10.1016/j.atherosclerosis.2018.09.022 (2018).
Duits, F. H. et al. Matrix Metalloproteinases in Alzheimer’s Disease and Concurrent Cerebral Microbleeds. J. Alzheimer’s Dis. https://doi.org/10.3233/JAD-143186 (2015).
Brew, K. & Nagase, H. The tissue inhibitors of metalloproteinases (TIMPs): An ancient family with structural and functional diversity. Biochimica et Biophysica Acta - Molecular Cell Research. https://doi.org/10.1016/j.bbamcr.2010.01.003 (2010).
Yang, Y. & Rosenberg, G. A. Matrix metalloproteinases as therapeutic targets for stroke. Brain Research. https://doi.org/10.1016/j.brainres.2015.04.024 (2015).
Howe, M. D. et al. Serum markers of blood-brain barrier remodeling and fibrosis as predictors of etiology and clinicoradiologic outcome in intracerebral hemorrhage. Front. Neurol. https://doi.org/10.3389/fneur.2018.00746 (2018).
Li, N. et al. Association of molecular markers with perihematomal edema and clinical outcome in intracerebral hemorrhage. Stroke. https://doi.org/10.1161/STROKEAHA.112.673590 (2013).
Florczak-Rzepka, M., Grond-Ginsbach, C., Montaner, J. & Steiner, T. Matrix metalloproteinases in human spontaneous intracerebral hemorrhage: An update. Cerebrovascular Diseases. https://doi.org/10.1159/000341686 (2012).
Lorente, L. et al. Association between serum tissue inhibitor of matrix metalloproteinase-1 levels and mortality in patients with severe brain trauma injury. PLoS One. https://doi.org/10.1371/journal.pone.0094370 (2014).
Lorente, L. et al. Persistently high circulating tissue inhibitor of matrix metalloproteinase-1 levels in non-survivor brain trauma injury patients. J. Crit. Care. https://doi.org/10.1016/j.jcrc.2019.02.014 (2019).
Lorente, L. et al. Serum tissue inhibitor of matrix metalloproteinase-1 levels are associated with mortality in patients with malignant middle cerebral artery infarction. BMC Neurol. https://doi.org/10.1186/s12883-015-0364-7 (2015).
Hernandez-Guillamon, M. et al. MMP-2/MMP-9 plasma level and brain expression in cerebral amyloid angiopathy-associated hemorrhagic stroke. Brain Pathol. https://doi.org/10.1111/j.1750-3639.2011.00512.x (2012).
Haller, J. T., Wiss, A. L., May, C. C., Jones, G. M. & Smetana, K. S. Acute Management of Hypertension Following Intracerebral Hemorrhage. Critical Care Nursing Quarterly. https://doi.org/10.1097/CNQ.0000000000000247 (2019).
Cunningham, L. A., Wetzel, M. & Rosenberg, G. A. Multiple roles for MMPs and TIMPs in cerebral ischemia. GLIA. https://doi.org/10.1002/glia.20169 (2005).
Alvarez-Sabín, J. et al. Temporal profile of matrix metalloproteinases and their inhibitors after spontaneous intracerebral hemorrhage: Relationship to clinical and radiological outcome. Stroke. https://doi.org/10.1161/01.STR.0000126827.69286.90 (2004).
Lorente, L. et al. High Serum Tissue Inhibitor of Matrix Metalloproteinase-1 Levels and Mortality in Patients with Spontaneous Intracerebral Hemorrhage. World Neurosurg. https://doi.org/10.1016/j.wneu.2019.10.106 (2020).
Zhang, J. X., Zhang, Z. Y. & Cheng, Y. Elevated MMP-1 and TIMP-1 are related with acute cerebral infarction patients with diabetes mellitus. Int. J. Clin. Exp. Med. 10(12) 16555–16561 (2017).
Piccardi, B. et al. Unbalanced metalloproteinase-9 and tissue inhibitors of metalloproteinases ratios predict hemorrhagic transformation of lesion in ischemic stroke patients treated with thrombolysis: Results from the MAGIC study. Front. Neurol. https://doi.org/10.3389/fneur.2015.00121 (2015).
Fischer, M. et al. Differential Regulation of Matrix-Metalloproteinases and Their Tissue Inhibitors in Patients with Aneurysmal Subarachnoid Hemorrhage. PLoS One. https://doi.org/10.1371/journal.pone.0059952 (2013).
Kim, S. C. et al. Matrix metalloproteinase-9 in cerebral aneurysms. Neurosurgery. https://doi.org/10.1097/00006123-199709000-00027 (1997).
Sellner, J. & Leib, S. L. In bacterial meningitis cortical brain damage is associated with changes in parenchymal MMP-9/TIMP-1 ratio and increased collagen type IV degradation. Neurobiol. Dis. https://doi.org/10.1016/j.nbd.2005.09.007 (2006).
Waubant, E. et al. IFNβ lowers MMP-9/TIMP-1 ratio, which predicts new enhancing lesions in patients with SPMS. Neurology. https://doi.org/10.1212/WNL.60.1.52 (2003).
Fujimoto, M. et al. Tissue inhibitor of metalloproteinases protect blood-brain barrier disruption in focal cerebral ischemia. J. Cereb. Blood Flow Metab. https://doi.org/10.1038/jcbfm.2008.59 (2008).
Magnoni, S. et al. Neuroprotective effect of adenoviral-mediated gene transfer of TIMP-1 and -2 in ischemic brain injury. Gene Ther. https://doi.org/10.1038/sj.gt.3302894 (2007).
Orbe, J. et al. Design, synthesis, and biological evaluation of novel matrix metalloproteinase inhibitors as potent antihemorrhagic agents: From hit identification to an optimized lead. J. Med. Chem. https://doi.org/10.1021/jm501940y (2015).
Rodríguez, J. A. et al. CM352 reduces brain damage and improves functional recovery in a rat model of intracerebral hemorrhage. J. Am. Heart Assoc. https://doi.org/10.1161/JAHA.117.006042 (2017).
Ironside, N. et al. Location-specific differences in hematoma volume predict outcomes in patients with spontaneous intracerebral hemorrhage. Int. J. Stroke. https://doi.org/10.1177/1747493019830589 (2020).
Abilleira, S. et al. Matrix metalloproteinase-9 concentration after spontaneous intracerebral hemorrhage. J. Neurosurg. https://doi.org/10.3171/jns.2003.99.1.0065 (2003).
Zhao, L. et al. Matrix metalloproteinase 9-mediated intracerebral hemorrhage induced by cerebral amyloid angiopathy. Neurobiol. Aging. https://doi.org/10.1016/j.neurobiolaging.2015.07.016 (2015).
Barrett, A. J., Rawlings, N. D. & Woessner, J. F. Handbook of Proteolytic Enzymes: Second Edition. Handbook of Proteolytic Enzymes: Second Edition. https://doi.org/10.1016/C2009-0-03628-9 (2004).
Söderholm, M., Nordin Fredrikson, G., Nilsson, J. & Engström, G. High Serum Level of Matrix Metalloproteinase-7 Is Associated with Increased Risk of Spontaneous Subarachnoid Hemorrhage. Stroke. https://doi.org/10.1161/STROKEAHA.118.020660 (2018).
Li, Q., Park, P. W., Wilson, C. L. & Parks, W. C. Matrilysin shedding of syndecan-1 regulates chemokine mobilization and transepithelial efflux of neutrophils in acute lung injury. Cell. https://doi.org/10.1016/S0092-8674(02)01079-6 (2002).
Toni, M. et al. Matrix metalloproteinase-10 plays an active role in microvascular complications in type 1 diabetic patients. Diabetologia. https://doi.org/10.1007/s00125-013-3052-4 (2013).
Peeters, S. A. et al. Plasma levels of matrix metalloproteinase-2, -3, -10, and tissue inhibitor of metalloproteinase-1 are associated with vascular complications in patients with type 1 diabetes: The EURODIAB Prospective Complications Study. Cardiovasc. Diabetol. https://doi.org/10.1186/s12933-015-0195-2 (2015).
Peeters, S. A. et al. Plasma matrix metalloproteinases are associated with incident cardiovascular disease and all-cause mortality in patients with type 1 diabetes: A 12-year follow-up study. Cardiovasc. Diabetol. https://doi.org/10.1186/s12933-017-0539-1 (2017).
George, J. et al. Circulating matrix metalloproteinase-2 but not matrix metalloproteinase-3, matrix metalloproteinase-9, or tissue inhibitor of metalloproteinase-1 predicts outcome in patients with congestive heart failure. Am. Heart J. https://doi.org/10.1016/j.ahj.2004.11.016 (2005).
Aguilar, M. I. & Brott, T. G. Update in Intracerebral Hemorrhage. The Neurohospitalist. https://doi.org/10.1177/1941875211409050 (2011).
Huttner, H. B. et al. Comparison of ABC/2 estimation technique to computer-assisted planimetric analysis in warfarin-related intracerebral parenchymal hemorrhage. Stroke. https://doi.org/10.1161/01.STR.0000198806.67472.5c (2006).
Kranz, P. G., Malinzak, M. D. & Amrhein, T. J. Approach to Imaging in Patients with Spontaneous Intracranial Hemorrhage. Neuroimaging Clinics of North America. https://doi.org/10.1016/j.nic.2018.03.003 (2018).
Kwah, L. K. & Diong, J. National Institutes of Health Stroke Scale (NIHSS). Journal of Physiotherapy. https://doi.org/10.1016/j.jphys.2013.12.012 (2014).
Schmidt, F. A., Liotta, E. M., Prabhakaran, S., Naidech, A. M. & Maas, M. B. Assessment and comparison of the max-ICH score and ICH score by external validation. Neurology. https://doi.org/10.1212/WNL.0000000000006117 (2018).
Broderick, J. P., Adeoye, O. & Elm, J. Evolution of the Modified Rankin Scale and Its Use in Future Stroke Trials. Stroke. https://doi.org/10.1161/STROKEAHA.117.017866 (2017).
Acknowledgements
We would like to thank all patients that kindly participated in this study, the nurses from the Stroke Unit of the Complejo Hospitalario de Navarra and the Hospital Universitario Vall d’Hebron for the collection of the samples and Lara Montori and Miriam Belzunce for their help with the experimental work. This work was supported by the Ministerio de Economía y Competitividad, Instituto de Salud Carlos III [PI15/01807, PI19/00065] and Federal Ministry of Education and Research (FEDER) funds; grants from the Spanish Society of Thrombosis and Haemostasis (SETH), Navarra Government (02/2015), Patrimonio Praga (Mexico) and Virto Group (Navarra, Spain); and a PhD scholarship from the Asociación de Amigos de la Universidad de Navarra (ADA).
Author information
Authors and Affiliations
Contributions
M.N.O. participated in the design of the project, experimental work, statistical analysis, and wrote, reviewed and edited the manuscript; R.M. participated in the design of the project and edited and reviewed the manuscript; B.Z. participated in the design of the project and reviewed the manuscript; J.M.E. participated in the design of the project and reviewed the manuscript; A.B.P. participated in the design of the project and reviewed the manuscript; J.A.R. participated in the design of the project and reviewed the manuscript; C.R. participated in the design of the project and reviewed the manuscript; J.A.P. participated in the design of the project, supervised the work and edited and reviewed the manuscript; E.T. participated in the statistical analysis and reviewed the manuscript; J.M. participated in the design of the project and reviewed the manuscript; M.H.G. participated in the design of the project and edited and reviewed the manuscript; J.O. was in charge of the whole project design, supervised the work and wrote, edited and reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Navarro-Oviedo, M., Muñoz-Arrondo, R., Zandio, B. et al. Circulating TIMP-1 is associated with hematoma volume in patients with spontaneous intracranial hemorrhage. Sci Rep 10, 10329 (2020). https://doi.org/10.1038/s41598-020-67250-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-67250-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.