Abstract
The uterus plays an important and unique role during pregnancy and is a dynamic organ subjected to mechanical stimuli. It has been reported that infertility occurs when the peristalsis is prevented, although its mechanisms remain unknown. In this study, we found that mechanical strain mimicking the peristaltic motion of the uterine smooth muscle layer enabled the endometrial stromal cells to acquire contractility. In order to mimic the peristalsis induced by uterine smooth muscle cells, cyclic tensile stretch was applied to human endometrial stromal cells. The results showed that the strained cells exerted greater contractility in three-dimensional collagen gels in the presence of oxytocin, due to up-regulated alpha-smooth muscle actin expression via the cAMP signaling pathway. These in vitro findings underscore the plasticity of the endometrial stromal cell phenotype and suggest the possibility of acquired contractility by these cells in vivo and its potential contribution to uterine contractile activity. This phenomenon may be a typical example of how a tissue passively acquires new contractile functions under mechanical stimulation from a neighboring tissue, enabling it to support the adjacent tissue’s functions.
Similar content being viewed by others
Introduction
It is now widely known that mechanical stimuli applied to various cell types can trigger intracellular signaling events leading to physiological and pathological changes1,2,3,4,5. The uterus allows implantation of the embryo and regulates its growth by supplying nutrients from the mother’s body6. It is also known as a dynamic organ that is modulated by menstrual hormone changes during the menstrual cycle and pregnancy. The uterine wall consists of three layers, namely the endometrium, the myometrium, and the perimetrium7,8. While the inner layer of the endometrium is composed of epithelial cells and stromal cells, the thickest middle myometrial layer mainly consists of smooth muscle cells. The perimetrium is the thin outermost layer of connective tissue. The myometrium is known to show spontaneous contractile activity9, and undergoes remodeling by hyperplasia and hypertrophy during pregnancy10.
The non-pregnant uterus also shows a distinct activity called “endometrium movement” throughout the menstrual cycle, which is regulated by ovarian steroid hormones11. Furthermore, the endometrium wave is known to play a significant role during pregnancy in order to transport the fertilized egg/zygote through the utero-tubal cavities prior to implantation12. It has also been reported that infertility occurs when the mechanical stress induced by the endometrium wave is prevented13. Therefore, we believe that this mechanical stimulus from the myometrium has a crucial role in physiological functions of the endometrium, such as menstruation and pregnancy.
In this study, we hypothesized that the uterine peristalsis induced by uterine smooth muscle cells might affect the contractile ability of endometrial stromal cells, an important function of the uterus for pregnancy. The endometrial stromal cells have been thought to passively undergo strain stimulation under the contractile movement of uterine smooth muscle cells. However, we propose that stromal cells actually actively support the peristaltic movement of the uterus. It is possible that the existence of these mechanisms helps to make the uterine peristaltic movement, which plays an important role for implantation of fertilized eggs and pregnancy, more steady and reliable.
Results
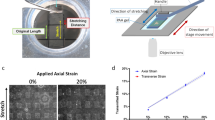
Reorientation of hESCs after applying 7 days of uniaxial cyclic strain
In this study, we loaded 15% of uniaxial cyclic strain at 0.1 Hz to hESCs for 7 days, as shown in Fig. 1(A). In order to quantify the reorientation of hESCs after applying uniaxial cyclic strain for 7 days, we evaluated the changes in the cells’ angle from normal microscope images of control and strained cells as shown in Fig. 1(B),(C). In Fig. 1(D),(E), mean angles of cells (or mean direction of elongation) in control and strained hESCs were 108° (SD 69.1°) and 91.3° (SD 33.6°), respectively. The mean angle of strained hESCs compared to that of control cells was significantly different (p < 0.005). Moreover, the standard deviation of the angle in the strained cells was much smaller than that of the control sample. This indicates the angle of the cells in the strained hESCs was much more uniform compared to the more random orientation of the control hESCs. Hence, after 7 days, the strained cells reoriented perpendicularly to the direction of strain and became elongated while the control cells were randomly oriented.
(A) Schematic view of the experimental setup showing the side view of the Flexcell tension system and the top view of the Flexcell plate. Microscope images of (B) control and (C) strained cells after applying 7 days of cyclic strain. The white bar indicates 300 μm. (D) Quantification of orientation changes in the strained cells. Graphs show the angle of cells (300 cells from 6 independent experiments). The bars represent the mean ± standard error deviation (p-value was obtained from F-test; *p < 0.05, **p < 0.005). (E) Schematic plot of the cell distribution. The red and black arrows represent the strained and control group, respectively.
Uniaxial cyclic strain up-regulated α-SMA expression in hESCs
As shown in Fig. 2(A), we analyzed by real-time PCR several stromal cell markers including CD10 and CD90 and uterine smooth muscle cell (SMC) markers such as ACTA2 and TAGLN. Particularly, ACTA2 plays a key role in the production of alpha-smooth muscle actin (α-SMA), which belongs to the actin protein family and is involved in cell contraction. Cyclic strain slightly decreased endometrial stromal cell marker expression (0.90-fold change for CD10 and 0.86-fold change for CD90), but the changes were not significant. With regards to ACTA2 and TAGLN, they were significantly up-regulated by cyclic strain (1.32-fold change for ACTA2, p < 0.005; and 1.59-fold change for TAGLN, p < 0.05). In the same manner as ACTA2 and TAGLN, 7 days of cyclic strain significantly raised mRNA expression of the oxytocin receptor (OXTR), which is highly expressed in the myometrium to regulate uterine contraction (2.13-fold change for OXTR, p < 0.05).
Promoted expressions of smooth muscle cell markers in hESCs after applying cyclic strain for 7 days, measured by real-time PCR and immunostaining. (A) mRNA expressions of endometrial stromal cell markers and smooth muscle cell markers in hESCs after applying cyclic strain for 7 days measured by real-time PCR. (CD10, CD90, ACATA2, TAGLN, OXTR, DES, IL6, ANGPT1, and RAMP1). Graphs show the fold change of mRNA expressions relative to RPL32 mRNA normalized to the control mean (n = 6). The bars represent the mean ± standard error (p-value was obtained from Student’s t-test; *p < 0.05, **p < 0.005). (B) Immunostaining of Vimentin (Vim) and smooth muscle actin (α-SMA) in hESCs after loading cyclic strain for 7 days; Vim and α-SMA expression in control samples (left). Vim and α-SMA expression in strained samples (right). The arrows indicate the direction of cyclic strain. Scale bar = 100 μm.
In order to distinguish uterine SMCs and myofibroblasts, we also examined desmin (DES) and Interleukin 6 (IL6) expression, which are associated with myofibroblasts. Real-time PCR results also showed an up-regulation of DES mRNA expression (1.63-fold change, p < 0.05) and a decrease in IL6 (0.68-fold change; p < 0.05) after application of cyclic strain. On the other hand, mRNA expressions of Angiopoietin 1 (ANGPT1) (0.73-fold change; p = 0.12) and Receptor activity modifying protein (RAMP1) (0.50-fold change, p < 0.005) were measured to distinguish uterine SMCs and vascular smooth muscle cells.
After applying cyclic strain for 7 days, immunostaining for vimentin (Vim) and α-SMA was carried out to check for changes in stromal cell and smooth muscle cell marker expression as shown in Fig. 2(B). As a result, there was an increase in the staining intensity of α-SMA in the strained cells while no significant change in the expression of the stromal cell marker was observed after applying cyclic strain.
Cyclic strain increases cAMP production in hESC
In order to understand the effect of uniaxial cyclic strain on hESCs, we measured the level of cAMP in hESCs after applying strain. Firstly, cAMP concentrations after 15 mins of cyclic strain were measured. Figure 3(A) shows a transient and significant up-regulation in cAMP production (1.75-fold change; p < 0.005) in as little as 15 mins. In addition, Fig. 3(B) shows the levels of cAMP after 7 days of cyclic strain. There was a non-significant increase in cAMP production immediately after 7 days of strain (1.62-fold change; p = 0.07). We then performed 7 days of strain, followed by a 2-hour break for cAMP levels to stabilize, followed by an extra 15 mins of cyclic strain. After such a strain regimen, cAMP concentration was significantly up-regulated (2.35-fold change; p < 0.05).
Relative cAMP production levels measured by the cyclic AMP EIA kit. (A) Applying cyclic strain for 15 mins significantly up-regulated cAMP production in hESCs. (B) cAMP levels were measured after 7 days of strain, followed by a 2-hour break for cAMP levels to stabilize, followed by an extra 15 mins of cyclic strain. 7 days of strain induced a non-significant increase in cAMP production, but adding a 2-hour break followed by an extra 15 mins significantly up-regulated cAMP levels. Graphs show the fold change of cAMP production levels relative to the amounts of DNA and normalized to the control mean. The bars represent the mean ± standard error (n = 4) (p-value was obtained from Student’s t-test; *p < 0.05, **p < 0.005).
SQ22536 and H-89 inhibit the up-regulation of α-SMA expression by cyclic strain in hESCs
To determine whether the cAMP pathway is involved in the up-regulation of α-SMA expression under strain, we stretched hESCs in the presence or absence of the adenylyl cyclase inhibitor SQ22536 or the PKA inhibitor H-89. Figure 4(A)–(F) represent the fold changes in mRNA expression measured by real-time PCR in the presence or absence of inhibitors. As in the previous experiment, the cyclic strain did not significantly affect CD10 or CD90 expression in hESCs but significantly up-regulated ACTA2 (1.37-fold change) and TAGLN (1.68-fold change) expression. By adding SQ22536, the up-regulation of ACTA2, TAGLN, and OXTR by cyclic strain was inhibited, with a respectively 1.01-, 0.91-, and 1.00-fold change in ACTA2, TAGLN, and OXTR expression. Moreover, the use of H-89 also showed an inhibiting effect on ACTA2 (0.47-fold change), TAGLN (0.55-fold change), and OXTR (0.73-fold change) expression. Moreover, the SQ22536 and H-89 non-significantly suppressed the increase in DES (0.81- and 1.12-fold change, respectively) expression.
mRNA expressions measured by real-time PCR of (A) CD10, (B) CD90, (C) ACTA2, (D) TAGLN, (E) OXTR, and (F) DES in hESCs after applying cyclic strain in the presence or absence of the inhibitors SQ22536 and H-89. All the mRNA expressions were normalized to RPL32 expression and further normalized to control values. Applying cyclic strain for 7 days non-significantly down-regulated both endometrial stromal cell markers and up-regulated the smooth muscle cell markers. While the non-significant down-regulation of CD10 and CD90 were unchanged by addition of SQ22536 and H-89, both inhibitors significantly inhibited the up-regulation of ACTA2 and OXTR. The bars represent the mean fold change ± standard error between strained and control samples (n = 4) (p-values were obtained from ANOVA followed by Fisher’s LSD test; *p < 0.05). (G) Schematic diagram of the signaling pathway activated in hESCs in response to cyclic strain. Adenylyl cyclase located on the inner side of the plasma membrane converts ATP to intracellular cAMP. cAMP induced by cyclic strain then promoted SMa marker α-SMA expression, via adenylyl cyclase and PKA.
Effect of oxytocin on the hESC-mediated collagen I gel contraction
After applying uniaxial cyclic strain to hESCs for 7 days, the strained cells were collected for a cell contraction assay to check the contractile ability of the cells seeded in a three-dimensional collagen gel. Before the stress in the gel was released by detaching the gels from the culture dish, the cells in the collagen I gel were treated with oxytocin (10 nM) to examine if in the presence of oxytocin, the strained cells exerted greater contractility, behaving like uterine SMC. Figure 5(A)–(D) show the samples 7 days after releasing the gels from the culture dish in the presence or absence of oxytocin. The surface areas of the samples were measured and quantified as shown in Fig. 5(E). The surface areas of the control samples with and without oxytocin shrank to 71.6% (1.36 cm2) and 55.9% (1.06 cm2), respectively. On the other hand, the strained cells showed a significant elevation in their contractile ability both in the absence and in the presence of oxytocin, as gels shrank to 48.9% (0.93 cm2) and 36.7% (0.70 cm2), respectively, of their initial surface area. In particular, while the strained cells showed greater contractility than the control cells (p < 0.005), the addition of oxytocin in the strained cells further enhanced their contractility (p < 0.05).
hESCs-mediated collagen I gel contraction after 7 days in response to oxytocin (10 nM). (A) control sample without oxytocin (B) control sample with oxytocin, (C) gel containing strained cells without oxytocin, and (D) gel containing strained cells with oxytocin. (E) The graph represents the gel area 7 days after release normalized to the initial area. The bars represent the mean ± standard error of gel area (n = 4) (p-value was obtained from ANOVA followed by Fisher’s LSD; *p < 0.05, **p < 0.005; the statistical analysis was performed using the original area measurement data).
Discussion
Mechanical stimulation is crucial to the proper function of many different organs like cartilage, blood vessels or the uterus14,15. For the uterus, which plays an important role during pregnancy and childbirth, the mechanical stress caused by the peristaltic movement of the fallopian tube due to the contraction of uterine smooth muscle cells promotes the migration of fertilized eggs16. In addition, infertility can also be caused by uterine fibroids that perturb the periodic uterine peristaltic movement induced by hormones17. Therefore, although the number of studies regarding mechanical stress responses in the uterus is still limited, the mechanical stress may play a role in homeostasis and pathogenesis of the uterus.
In this study, we proposed a new hypothesis regarding the response to mechanical stress in the uterine tissues with a hierarchical structure. The uterus has a three-layer structure consisting of, starting from the inside, epithelial cells, stromal cells, and smooth muscle cells. From our in vitro results, it is reasonable to imagine a similar mechanism in vivo, by which the peristaltic movement of the uterus caused by contraction of the outermost smooth muscle layer enhances the contractility of the inner stromal cells. We believe that such a mechanism might make the three-dimensional peristaltic movements of the uterus during pregnancy and childbirth more consistent and reliable.
In two-dimensional culture, the tensile stress that mimics the peristaltic movement of the myometrium is reported to regulate the biochemical function of stromal cells to support a the differentiation process of endometrium, decidualization18, but it is dubious whether the tensile stress is well loaded three-dimensionally on the stromal cells in the body. As shown in this study, acquisition of contractility by the stromal cells under strain may be an effective mechanism to transmit the tensile stress from the smooth muscle layer in the body. In other words, it is suspected that contraction by uterine smooth muscle cells is transmitted to the inner stromal cells, whereby each individual stromal cell can contract steadily thanks to the increased expression of proteins such as α-SMA and oxytocin. Considering the fact that, in vivo, infertility can occur when the uterus is unable to contract properly, these findings may represent a new mechanotransduction mechanism, by which contractility is transmitted from the outside to the adjacent inner cell layer.
It is possible that such a phenomenon occurs not only in the uterus, but also in blood vessels as reported in the literature. When the tensile stress is applied to vascular endothelial cells such as human umbilical cord endothelial cells (HUVEC), smooth muscle actin expression is dramatically increased19,20,21. It might imply that the vascular endothelial cells loaded with tensile stimulation may not differentiate into vascular smooth muscle cells, and individual vascular endothelial cells might have instead acquired the contractility under the tensile stimulation induced by mechanical activation of intracellular signaling pathways, thus potentially enhancing the efficiency of blood vessel contraction. Our experiments in hESCs have shown that the strain slightly increases the gene expression levels of SMC markers, ACTA222 and TAGLN23. On the other hand, the immuno-staining data still showed strong staining levels of vimentin, a marker for stromal cells24, even with or without strain. Although Additionally, the α-SMA staining levels in ESC were extremely low compared to those in the SMC in vivo24. However, the strain did not apparently increase those of α-SMA in ESC even after stretching. Taking into consideration those results, it is reasonable to conclude that strain did not differentiate ESC into SMC, but made ESC acquire the ability to contract. This phenomenon might be similar to the response of HUVEC under strain.
In the field of cell and tissue engineering, mechanical stimuli have been identified as a significant factor to induce physiological changes by activating intracellular signaling pathways. While many researchers have reported on the effects and roles of mechanical stimuli in various cell models, studies of the uterus in response to mechanical stimuli are limited. There have been only a few studies reporting the effect of mechanical stretch on hESCs, particularly focusing on the expression of specific genes such as IGFBP1 or interleukin-8 (IL-8), which are associated with decidualization or inflammatio18,25. In this study, we aimed to understand the effects of mechanical stimuli on the hESCs, particularly on their contractility.
We applied 15% of uniaxial cyclic strain to hESCs at 0.1 Hz for up to 7 days. First, application of uniaxial cyclic strain to hESCs induced rearrangement in the direction perpendicular to the strain axis while control cells were randomly distributed. Moreover, both real-time PCR and immunostaining showed that the cyclic strain induced an increase in the expression of α-SMA. As well as the up-regulation of α-SMA, real-time PCR results showed a significant up-regulation in the mRNA expression of oxytocin receptor (OXTR) after loading cyclic strain for 7 days, a gene which is highly expressed in the myometrium26,27,28. The oxytocin receptor, however, is also expressed in the endometrium and its expression varies during the non-pregnant cycle, depending on ovarian steroid hormones, such as progesterone and estrogen29,30. Kunz’s group showed that oxytocin increases the frequency of the endometrial wave31. Moreover, it is known that up-regulation of the oxytocin receptor before the onset of labor during pregnancy induces the production of prostaglandin F2α, which results in an increase in endometrial contraction. This study is the first to suggest that mechanical stimuli play a role in endometrial stromal cells in the acquisition of contractility, by up-regulating α-SMA and oxytocin receptor expression.
In addition, we showed the strained cells to be different from myofibroblasts. While there is a lack of desmin accumulated in myofibroblasts, the expression of DES is known to be relatively abundant in the myometrium32,33. Moreover, IL6 production level is known to be elevated in myofibroblasts34,35,36. Application of cyclic strain for 7 days significantly induced the expression of DES and also down-regulated the expression of IL6, which indicates the strained hESCs were distinct from myofibroblasts. On the other hand, an essential marker abundantly expressed in vascular smooth muscle cells, ANGPT1, was non-significantly but slightly reduced by cyclic strain37,38,39,40. RAMP1 mRNA expression, which is specific to vascular smooth muscle cells in uterine arteries, was significantly down-regulated by cyclic strain, indicating that the strained cells were distinct from vascular smooth muscle cells41,42,43.
In this study, a cAMP production assay was performed after loading strain on hESCs. cAMP is a secondary messenger produced from adenosine triphosphate (ATP) and is known to regulate endometrial stromal cells for decidualization during the menstrual cycle44. There is a report that addition of estradiol in uterine cells evoked an increase in cAMP levels, and the cAMP pathway via adenylyl cyclase is involved in this mechanism45. Moreover, the phenotype induced in bone marrow-derived MSCs by cAMP treatment suggests those cells could serve as a source of endometrial stem/progenitor cells46. Thus, cAMP has a significant regulatory role in the uterus just like hormones such as estrogen and progesterone. In this study, we therefore focused on the involvement of cAMP in response to cyclic strain.
Here we also report that cyclic strain up-regulated cAMP production in hESCs, implying that the cAMP signaling pathway may be involved in the up-regulation of α-SMA expression under stretch. Applying cyclic strain for as little as 15 mins induced the up-regulation of cAMP production in hESCs. After up-regulating α-SMA expression in hESCs under cyclic strain for 7 days, we also examined whether cAMP production was responsive to strain. Since cAMP production is usually transiently induced, cells strained for 7 days were subjected to a 2-hour break (static condition) to stabilize the level of cAMP, followed by 15 mins of cyclic strain. This resulted in a significant up-regulation of cAMP production, showing that stretch was able to induce cAMP production both before and after applying cyclic strain for 7 days.
In order to determine the importance of cAMP in the stretch-induced up-regulation of α-SMA expression, we carried out inhibitor tests using the adenylyl cyclase inhibitor SQ22536 and the PKA inhibitor H-89, since adenylyl cyclase regulates cAMP production while PKA is a well-known cAMP-dependent protein kinase47,48. Figure 4(G) schematically illustrates the signaling pathway activated in the hESCs under cyclic strain, as discussed in this study. Adenylyl cyclase is an enzyme located on the inner side of the plasma membrane and usually activated by G proteins. Activation of adenylyl cyclase under cyclic strain converts adenosine triphosphate (ATP) to cAMP, an intracellular second messenger. We showed that cyclic strain increased the cAMP production level in hESCs. This transient up-regulation of cAMP in hESCs by cyclic strain was consistent with previous studies using other cell models under mechanical stimuli such as cyclic strain or static compressive strain49,50. As suggested by the inhibitor tests, the increase in intracellular cAMP levels is essential for the up-regulation of α-SMA expression in hESCs by cyclic strain. Interestingly, the addition of H-89 led to a decrease in the mRNA expression of SMC markers and OXTR under cyclic strain. The result may imply that H-89 did not only specifically inhibit the cAMP signaling pathway, but also activated other signaling pathways which inhibit SMC markers and OXTR expression under strain. Further studies will be required to address this point.
The cell contraction assay using collagen gels was then carried out to measure the cells’ contractile ability. As a result, the samples strained for 7 days showed an increased contractile ability compared to control samples. Moreover, the contractility in the strained samples was significantly enhanced in the presence of oxytocin, indicating that the strained hESCs behaved like uterine smooth muscle cells. It has been reported that the enhanced contractile ability of ESC may help to minimize defects in an endometrial wound model and promote endometrial tissue repair in vivo51. In ruminants, the level of oxytocin receptor is known to increase during the diestrus phase, reach its maximum value during the proestrus phase, and then decline during the estrus phase52,53. Peristaltic patterns such as intrauterine pressure and strain have also been reported to change during the estrous cycle54. Up-regulation of OXTR mRNA expression induced by mechanical stimulation might contribute to stopping the bleeding during the menstrual cycle by strengthening the contractility of the endometrium in response to oxytocin. Although the endometrium is exposed to a dynamic environment induced by the myometrium, the effect of mechanical stimuli on the ESCs with regard to their contractility remained unknown. In this study, we suggested that the enhanced contractility in the strained cells was due to the up-regulation of α-SMA expression and the oxytocin receptor. While several studies have shown that biochemical stimulation using cytokines or platelet-derived growth factor (PDGF) increased the contractility in hESCs in vitro51,55, we are the first to report that mechanical stimuli also allowed endometrial stromal cells to acquire greater contractility while keeping their original cell phenotype. In other words, mechanical stimulation might help to control the dynamic and active functions of endometrial stromal cells. It has been reported that OXTR is not expressed in stromal cells in vivo by immuno-staining27 or in situ hybridization56. However, in this paper, we reported that strain up-regulated OXTR mRNA expression in stromal cells by real-time PCR, which enables more sensitive signal detection than immune-staining and in situ hybridization. However, our current studies have only been performed in vitro, and the relevance of our findings will be examined during further studies. Although there are limitations to direct extrapolation of in vitro result to the in vivo context, passive strain stimulation of stromal cells caused by uterus SMCs might trigger active stromal cell contraction.
In summary, we report that applying uniaxial cyclic strain significantly up-regulates the expression of α-SMA as well as cAMP production. Together, the results show that strained hESCs acquire greater contractility, thus behaving more like uterine smooth muscle cells. Furthermore, these findings may imply that contractile movements by the myometrium have a significant role in inducing endometrial stromal cells to acquire the ability to contract in vivo for physiological functions of the endometrium. This newly reported phenomenon might be a typical example of how a tissue passively acquires new contractile functions under mechanical stimulation from a neighboring tissue, enabling it to support the adjacent tissue’s functions.
Methods
Isolation and culture of hESCs
Endometrial biopsies were obtained from 38~48-year-old female patients who had regular menstrual cycles. Fresh human endometrial stromal cells were isolated and cultured as previously reported57,58,59. The purity of the cell source was greater than 98%59. This study was approved by the Institutional Review Board of the University of Tokyo in accordance with the Declaration of Helsinki, and each patient gave informed consent for sample collection. We cultured hESCs in DMEM/Ham’s F12 (Sigma) supplemented with 2.5% charcoal-stripped FBS (Funakoshi) and 1% of Antibiotic-Antimycotic (GIBCO) in a humidified incubator at 37 °C with 5% CO2. The culture medium was changed every 3 or 4 days. For inhibitor tests, we used the adenylyl cyclase inhibitor SQ22536 and the protein kinase A (PKA) inhibitor H-89 (both from Cayman Chemical). SQ22536 (100 μM) and H-89 (10 μM) were added to the cells’ culture medium just before loading cyclic strain.
Uniaxial cyclic strain loading
In this study, we loaded cyclic strain using the Flexcell tension system (FX-4000; Flexcell International Corporation) placed in a humidified incubator at 37 °C with 5% CO2. The Flexcell is computer-operated and applies its strain by vacuum. In this study, 15% uniaxial strain was applied at 0.1 Hz as illustrated in Fig. 1. During application of the uniaxial cyclic strain, the culture medium was changed every 2 or 3 days. For control samples, hESCs were cultured in identical Flexcell plates but without strain.
Measurement of cell reorientation under cyclic strain
In order to measure the cells’ orientation angles, we used normal microscope images (×5) taken from the center of Flexwell plate to cover a wide range of the sample, that is further to avoid sample vialing. By using ImageJ, a line was drawn from the bottom of the cell to the top of the cell along the cell’s major axis. After drawing the line, the angle between this line and the horizontal axis was measured using ImageJ. We selected 50 cells per each sample from 6 different experiments so as to select entirely in terms of area distribution.
Real Time-PCR
To measure mRNA expression in the different samples from the Flexcell system, we carried out real-time PCR. After finishing loading cyclic strain, the cells were rinsed with PBS and immediately lysed with Trizol reagent (Invitrogen) before RNA extraction and cDNA synthesis using the ReverTra Ace qPCR RT Master Mix with gDNA Remover (Toyobo). CD10 and CD90 were used as endometrial stromal cell markers while ACTA2 and transgelin (TAGLN) are highly expressed in SMC. Oxytocin receptor (OXTR) was also examined as a uterine smooth muscle cell marker while desmin (DES) and interleukin 6 (IL6) were utilized to distinguish uterine SMCs from myofibroblasts. Similarly, the expression of the vascular smooth muscle cell markers angiopoietin 1 (ANGPT1) and receptor activity modifying protein 1 (RAMP1) were also measured. All genes were normalized to RPL32 expression and further normalized to the control samples. Primer sequences and amplicon sizes are listed in Table 1.
Immunostaining
After 7 days of cyclic strain, hESCs were immediately fixed with 4% paraformaldehyde. The fixed samples were permeabilized with 0.2% Triton-X 100 in PBS for 3 min and washed with PBS 3 times. Then non-specific binding was blocked with PBS containing 1% BSA before covering the cells with anti-α-SMA antibody (Abcam) at a 1/500 dilution for 1 hour at room temperature or overnight at 4°C. After revealing the antibody using the DAB peroxidase substrate kit (Vector Laboratories), the samples were mounted on glass slides for visualization and storage.
Cyclic adenosine monophosphate (cAMP) measurement
The samples were collected and lysed with 0.1 M HCl. After centrifugation at 1,000 g the supernatant was decanted and stored at −80 °C until assay. Cyclic AMP concentrations were measured using the cyclic AMP EIA kit (Cayman Chemical) according to the manufacturer’s instructions. The absorbance at 412 nm was measured with an EnSpire Multimode Plate Reader (PerkinElmer). The cAMP concentrations were normalized to the DNA amounts quantified using the Quant-iT PicoGreen dsDNA Reagent and Kit (Invitrogen).
Cell contraction assay
After the samples were subjected to cyclic strain for 7 days, they were trypsinized and resuspended in medium at a density of 2.0 × 106 cells/ml. By using the collagen-based Cell Contraction Assay kit (Cell Biolabs, Inc.), we prepared a collagen lattice with bovine type I collagen at a concentration of 3.0 mg/ml. As indicated in the protocol of the kit, the collagen gel was polymerized in the presence of cells and incubated for two days to allow stresses to develop within the gel. Before the stress was released by detaching the gel from the culture dish, oxytocin (10 nM) was added to promote contraction as in SMC. Seven days after releasing the gels from the culture dish, pictures were taken and the surface area of the sample was measured using ImageJ.
Statistical analysis
The statistical significance was assessed using Student’s t-test, F-test, or ANOVA followed by Fisher’s least significant difference (LSD). P-values below 0.05 were regarded as significant.
References
Kim, J., Montagne, K., Ushida, T. & Furukawa, K. Enhanced chondrogenesis with upregulation of PKR using a novel hydrostatic pressure bioreactor. Bioscience, Biotechnology, and Biochemistry 79, 239–241 (2014).
Kim, J., Montagne, K., Nemoto, H., Ushida, T. & Furukawa, K. S. Hypergravity down-regulates c-fos gene expression via ROCK/Rho-GTP and the PI3K signaling pathway in murine ATDC5 chondroprogenitor cells. PLoS ONE 12, e0185394 (2017).
Ting, S. Y. W., Montagne, K., Nishimura, Y., Ushida, T. & Furukawa, K. S. Modulation of the Effect of Transforming Growth Factor-β3 by Low-Intensity Pulsed Ultrasound on Scaffold-Free Dedifferentiated Articular Bovine Chondrocyte Tissues. Tissue Eng Part C Methods 21, 1005–1014 (2015).
Furukawa, K. S., Imura, K., Tateishi, T. & Ushida, T. Scaffold-free cartilage by rotational culture for tissue engineering. J. Biotechnol. 133, 134–145 (2008).
Kim, J. & Adachi, T. Cell Condensation Triggers the Differentiation of Osteoblast Precursor Cells to Osteocyte-Like Cells. Front. Bioeng. Biotechnol. 7, (2019).
Levasseur, M. C. Utero-ovarian relationships in placental mammals: role of uterus and embryo in the regulation of progesterone secretion by the corpus luteum. A review. Reprod Nutr Dev 23, 793–816 (1983).
Padykula, H. A. Regeneration in the primate uterus: the role of stem cells. Ann. N. Y. Acad. Sci. 622, 47–56 (1991).
Chan, R. W. S., Schwab, K. E. & Gargett, C. E. Clonogenicity of human endometrial epithelial and stromal cells. Biol. Reprod. 70, 1738–1750 (2004).
Bulletti, C. et al. Abnormal uterine contractility in nonpregnant women. Ann. N. Y. Acad. Sci. 828, 223–229 (1997).
Shynlova, O., Mitchell, J. A., Tsampalieros, A., Langille, B. L. & Lye, S. J. Progesterone and gravidity differentially regulate expression of extracellular matrix components in the pregnant rat myometrium. Biol. Reprod. 70, 986–992 (2004).
van Gestel, I., IJland, M. M., Hoogland, H. J. & Evers, J. L. H. Endometrial wave-like activity in the non-pregnant uterus. Hum. Reprod. Update 9, 131–138 (2003).
Bulletti, C. & de Ziegler, D. Uterine contractility and embryo implantation. Curr. Opin. Obstet. Gynecol. 18, 473–484 (2006).
IJland, M. M., Evers, J. L., Dunselman, G. A., Volovics, L. & Hoogland, H. J. Relation between endometrial wavelike activity and fecundability in spontaneous cycles. Fertil. Steril. 67, 492–496 (1997).
Montagne, K. et al. High hydrostatic pressure induces pro-osteoarthritic changes in cartilage precursor cells: A transcriptome analysis. PLoS ONE 12, e0183226 (2017).
Slager, C. J. et al. The role of shear stress in the generation of rupture-prone vulnerable plaques. Nat Rev Cardiol 2, 401–407 (2005).
Matsuura, K. et al. Improved development of mouse and human embryos using a tilting embryo culture system. Reproductive BioMedicine Online 20, 358–364 (2010).
Yoshino, O. et al. Decreased pregnancy rate is linked to abnormal uterine peristalsis caused by intramural fibroids. Hum Reprod 10, 2475–2479 (2010).
Harada, M. et al. Mechanical stretch upregulates IGFBP-1 secretion from decidualized endometrial stromal cells. American Journal of Physiology - Endocrinology and Metabolism 290, E268–E272 (2006).
Ishisaki, A., Hayashi, H., Li, A.-J. & Imamura, T. Human Umbilical Vein Endothelium-derived Cells Retain Potential to Differentiate into Smooth Muscle-like Cells. J. Biol. Chem. 278, 1303–1309 (2003).
Cevallos, M. et al. Cyclic strain induces expression of specific smooth muscle cell markers in human endothelial cells. Differentiation 74, 552–561 (2006).
Shoajei, S., Shahdpour, M. T., Shokrgozar, M. A. & Haghighipour, N. Alteration of human umbilical vein endothelial cell gene expression in different biomechanical environments. Cell Biology International 38, 577–581 (2014).
Konrad, L. et al. Composition of the stroma in the human endometrium and endometriosis. Reproductive Science 25(7), 1106–1115 (2018).
Tawfik, O. et al. Transgelin, a novel marker of smooth muscle cell differentiation, effectively distinguishes endometrial stromal tumors from uterine smooth muscle tumors. Int. J. Gynecol. Obstet. Reprod. Med. Res. 1(1), 26–31 (2014).
Santoso, E. G. et al. Application of detergents or high hydrostatic pressure as decellularization processes in uterine tissues and their subsequent effects on in vivo uterine regeneration in murine models. PLoS One 24;9(7), e103201 (2014).
Harada, M. et al. Mechanical Stretch Stimulates Interleukin-8 Production in Endometrial Stromal Cells: Possible Implications in Endometrium-Related Events. The Journal of Clinical Endocrinology & Metabolism 90, 1144–1148 (2005).
Havelock, J. C. et al. Human myometrial gene expression before and during parturition. Biol. Reprod. 72, 707–719 (2005).
Loddenkemper, C. et al. Use of oxytocin receptor expression in distinguishing between uterine smooth muscle tumors and endometrial stromal sarcoma. Am. J. Surg. Pathol. 27, 1458–1462 (2003).
Blanks, A. M., Shmygol, A. & Thornton, S. Preterm labour. Myometrial function in prematurity. Best Pract Res Clin Obstet Gynaecol 21, 807–819 (2007).
Kimura, T., Tanizawa, O., Mori, K., Brownstein, M. J. & Okayama, H. Structure and expression of a human oxytocin receptor. Nature 1992 356:6369 356, 526–529 (1992).
Robinson, R. S., Mann, G. E., Lamming, G. E. & Wathes, D. C. The effect of pregnancy on the expression of uterine oxytocin, oestrogen and progesterone receptors during early pregnancy in the cow. J Endocrinol 160, 21–33 (1999).
Kunz, G., Noe, M., Herbertz, M. & Leyendecker, G. Uterine peristalsis during the follicular phase of the menstrual cycle: effects of oestrogen, antioestrogen and oxytocin. Hum. Reprod. Update 4, 647–654 (1998).
Schürch, W., Seemayer, T. A., Lagacé, R. & Gabbiani, G. The intermediate filament cytoskeleton of myofibroblasts: an immunofluorescence and ultrastructural study. Virchows Arch A Pathol Anat Histopathol 403, 323–336 (1984).
Eyden, B. P., Hale, R. J., Richmond, I. & Buckley, C. H. Cytoskeletal filaments in the smooth muscle cells of uterine leiomyomata and myometrium: an ultrastructural and immunohistochemical analysis. Virchows Arch A Pathol Anat Histopathol 420, 51–58 (1992).
Yu, J. et al. IL-6 downregulates transcription of NTPDase2 via specific promoter elements. Am. J. Physiol. Gastrointest. Liver Physiol. 294, G748–56 (2008).
Shimada, M. et al. IL-6 secretion by human pancreatic periacinar myofibroblasts in response to inflammatory mediators. J. Immunol. 168, 861–868 (2002).
Catarzi, S. et al. Oxidative state and IL-6 production in intestinal myofibroblasts of Crohn’s disease patients. Inflamm. Bowel Dis. 17, 1674–1684 (2011).
Iivanainen, E. et al. Angiopoietin-regulated recruitment of vascular smooth muscle cells by endothelial-derived heparin binding EGF-like growth factor. FASEB J 17, 1609–1621 (2003).
Jeansson, M. et al. Angiopoietin-1 is essential in mouse vasculature during development and in response to injury. The Journal of Clinical Investigation 121, 2278–2289 (2011).
Hellström, M., Kalén, M., Lindahl, P., Abramsson, A. & Betsholtz, C. Role of PDGF-B and PDGFR-beta in recruitment of vascular smooth muscle cells and pericytes during embryonic blood vessel formation in the mouse. Development 126, 3047–3055 (1999).
Rensen, S. S. M., Doevendans, P. A. F. M. & van Eys, G. J. J. M. Regulation and characteristics of vascular smooth muscle cell phenotypic diversity. Neth Heart J 15, 100–108 (2007).
Frayon, S., Cueille, C., Gnidéhou, S., de Vernejoul, M. C. & Garel, J. M. Dexamethasone increases RAMP1 and CRLR mRNA expressions in human vascular smooth muscle cells. Biochemical and Biophysical Research Communications 270, 1063–1067 (2000).
Zhang, Z., Dickerson, I. M. & Russo, A. F. Calcitonin gene-related peptide receptor activation by receptor activity-modifying protein-1 gene transfer to vascular smooth muscle cells. Endocrinology 147, 1932–1940 (2006).
Nikitenko, L. L. et al. Differential and cell-specific expression of calcitonin receptor-like receptor and receptor activity modifying proteins in the human uterus. Mol. Hum. Reprod. 7, 655–664 (2001).
Logan, P. C., Ponnampalam, A. P., Steiner, M. & Mitchell, M. D. Effect of cyclic AMP and estrogen/progesterone on the transcription of DNA methyltransferases during the decidualization of human endometrial stromal cells. Mol. Hum. Reprod. 19, 302–312 (2013).
Aronica, S. M., Kraus, W. L. & Katzenellenbogen, B. S. Estrogen action via the cAMP signaling pathway: stimulation of adenylate cyclase and cAMP-regulated gene transcription. Proc. Natl. Acad. Sci. USA 91, 8517–8521 (1994).
Aghajanova, L., Horcajadas, J. A., Esteban, F. J. & Giudice, L. C. The bone marrow-derived human mesenchymal stem cell: potential progenitor of the endometrial stromal fibroblast. Biol. Reprod. 82, 1076–1087 (2010).
Walsh, D. A. & Van Patten, S. M. Multiple pathway signal transduction by the cAMP-dependent protein kinase. FASEB J 8, 1227–1236 (1994).
Goel, M., Zuo, C.-D. & Schilling, W. P. Role of cAMP/PKA signaling cascade in vasopressin-induced trafficking of TRPC3 channels in principal cells of the collecting duct. Am. J. Physiol. Renal Physiol. 298, F988–96 (2010).
Ngan, P. et al. The interactive effects of mechanical stress and interleukin-1 beta on prostaglandin E and cyclic AMP production in human periodontal ligament fibroblasts in vitro: comparison with cloned osteoblastic cells of mouse (MC3T3-E1). Arch. Oral Biol. 35, 717–725 (1990).
Fitzgerald, J. B. et al. Mechanical compression of cartilage explants induces multiple time-dependent gene expression patterns and involves intracellular calcium and cyclic AMP. J. Biol. Chem. 279, 19502–19511 (2004).
Matsumoto, H. et al. Regulation of proliferation, motility, and contractility of human endometrial stromal cells by platelet-derived growth factor. The Journal of Clinical Endocrinology & Metabolism 90, 3560–3567 (2005).
Murata, T., Narita, K., Honda, K. & Higuchi, T. Changes of receptor mRNAs for oxytocin and estrogen during the estrous cycle in rat uterus. J. Vet. Med. Sci. 65, 707–712 (2003).
Fuchs, A. R. et al. Oxytocin and vasopressin receptors in bovine endometrium and myometrium during the estrous cycle and early pregnancy. Endocrinology 127, 629–636 (1990).
Bulletti, C. et al. Uterine contractility during the menstrual cycle. Human Reproduction 15, 81–89 (2000).
Kimatrai, M., Oliver, C., Abadía-Molina, A. C., García-Pacheco, J. M. & Olivares, E. G. Contractile activity of human decidual stromal cells. The Journal of Clinical Endocrinology & Metabolism 88, 844–849 (2003).
Takemura, M. et al. Expression and localization of oxytocin receptor gene in human uterine endometrium in relation to the menstrual cycle. Endocrinology 132, 1830–1835 (1993).
Koga, K. et al. Demonstration of angiogenin in human endometrium and its enhanced expression in endometrial tissues in the secretory phase and the decidua. The Journal of Clinical Endocrinology & Metabolism 86, 5609–5614 (2001).
Taguchi, A. et al. Resveratrol Enhances Apoptosis in Endometriotic Stromal Cells. Am. J. Reprod. Immunol. 75, 486–492 (2016).
Hirota, Y. et al. Possible implication of midkine in the development of endometriosis. Hum. Reprod. 20, 1084–1089 (2005).
Acknowledgements
The authors thank Dr. Katie Ryan for helpful advice on cell reorientation under cyclic strain. This work was supported by Research Fellowships from the Japan Society for the Promotion of Science for Young Scientists (Grant Numbers JP17J07735), Grants-in-aid for Scientific Research from the Japanese Ministry of Education, Culture, Sports, Science and Technology, and grants from the Translational Systems Biology and Medicine Initiative from the Ministry of Education, Culture, Sports, Science and Technology of Japan, and from the Japan Agency for Medical Research and Development (AMED; Development of Manufacturing System for Regenerative Medicinal Cells from Human Mesenchymal Stem Cells).
Author information
Authors and Affiliations
Contributions
F.S.K., U.T., H.T., H.Y., Y.O., and O.Y. conceived and supervised the study; K.J., F.S.K. and U.T. designed experiments; K.J., and H.T. performed experiments; K.J. and M.K. analyzed data; K.J. wrote the manuscript; M.K., F.S.K. and U.T. made manuscript revisions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, J., Ushida, T., Montagne, K. et al. Acquired contractile ability in human endometrial stromal cells by passive loading of cyclic tensile stretch. Sci Rep 10, 9014 (2020). https://doi.org/10.1038/s41598-020-65884-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-65884-3
This article is cited by
-
Revolutionizing the female reproductive system research using microfluidic chip platform
Journal of Nanobiotechnology (2023)
-
Strategies for modelling endometrial diseases
Nature Reviews Endocrinology (2022)
-
Estrogen- and Progesterone (P4)-Mediated Epigenetic Modifications of Endometrial Stromal Cells (EnSCs) and/or Mesenchymal Stem/Stromal Cells (MSCs) in the Etiopathogenesis of Endometriosis
Stem Cell Reviews and Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.