Abstract
In meta-analyses, it has been reported that myopia is a risk factor for glaucoma and there is increasing evidence that autonomic dysfunction causing vascular dysregulation or perfusion dysfunction is considered an important factor in the progression of glaucoma. There have been experimental studies to find out the association between autonomic nervous system and ocular growth, but no clinical study yet has evaluated the relationship between them. Therefore, we enrolled 208 open angle glaucoma patients and measured heart-rate-variability(HRV). We used the standard deviation value of the qualified normal to normal intervals (SDNN) parameter of HRV, which is considered an autonomic influence index and characterized the total effect of the regulation of autonomic blood circulation. Patients were classified into the two groups according to SDNN: those with low possibility of autonomic dysfunction (LoAD group) and those with high possibility of autonomic dysfunction (HiAD group). We evaluated myopic features employing a ‘posterior scleral profile’ identified by the disc tilt ratio, disc torsion, fovea-BMO center (FoBMO) angle and peripapapillary area(PPA) to disc ratio. HiAD group showed higher values than LoAD group in posterior scleral deformation profile such like axial length, disc tilt, torsion degree. We suggest the possibility of association between myopic deformation and autonomic dysfunction.
Similar content being viewed by others
Introduction
Glaucoma is a progressive optic neuropathy characterized by the optic nerve damage and loss of retinal ganglion cells1. While elevated intraocular pressure and age are considered main risk factors for the development and progression of the disease, the pathogenesis of glaucoma is still unclear. There is increasing evidence that vascular dysfunction and perfusion insufficiency need to be considered as important factors in the progression of glaucoma2,3,4. Autonomic dysfunction may contribute to unstable or fluctuating blood pressure which can cause dysfunction of autoregulation and lead to glaucoma progression5. A previous study revealed that there is the sympathovagal inbalance of autonomic nervous system(ANS) in patients with NTG6,7,8. Sympathovagal inbalance may be responsible for the faster rate of central visual field(VF) progression in NTG9.
Meanwhile, myopia has been reported as a risk factor for glaucoma in meta-analyses of epidemiological studies10. The Tajimi Study reported that age, intraocular pressure (IOP) and myopia were significant risk factors for primary open-angle glaucoma (POAG) and normal-tension glaucoma (NTG)11. In parallel with the increased prevalence of myopia, glaucoma also increases. Posterior pole profile variables like disc tilt, FoBMO angle, disc torsion, PPA to disc ratio are related to myopic optic nerve change12,13. These structural changes in the ONH may affect the higher susceptibility to glaucomatous optic disc damage14,15. Brazitikos et al.16 reported that tilted disc may cause visual field defects. Park et al.17 reported that optic disc torsion was related to the location of the visual field defect.
Several experimental studies have documented that there is relationship between the autonomic nervous system and ocular growth18,19,20. They reported that dysfunction or abnormality of autonomic nervous system result in ultradian rhythms in axial length and choroidal thickness that are associated with an increased rate of ocular growth underlying myopia development18. But no study yet has evaluated the linkage of myopic ocular change and autonomic inbalance in glaucoma patients, which are known to be associated with glaucomatous optic nerve damage.
The purpose of the present investigation was to evaluate whether the various indices including the posterior scleral profile have differences in according to presence of autonomic dysfunction.
Results
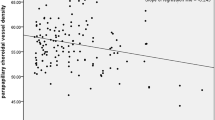
The mean value of the SDNN in 208 NTG patients was 33.71 and the standard deviation was 18.16. So LoAD group had a SDNN values between 15.55(33.71 –(minus) 18.16) and 51.87(33.71 + (plus)18.16) and HiAD group had a SDNN value less than 15.55 or greater than 51.87. Among 208 NTG patients, 164(78.8%) were LoAD group (15.55–51.87) and 44(21.2%) were HiAD group (<15.55 or >51.87). Analysis of several factors, including the posterior scleral pole profile for both groups is shown in Table 1. There were no significant differences between LoAD group and HiAD group with respect to age, sex, CCT, spherical equivalent, MD of VF, PSD of VF, average RNFL thickness. Axial length was significantly longer in HiAD group than LoAD group (p = 0.022). Torsion degree was significantly higher in HiAD group than LoAD group (p < 0.001), and the only factor related to heart rate variability in both simple (p < 0.001) and multiple (p = 0.008, p = 0.040 after bonferroni correction) logistic regression analysis (Table 2).
Discussion
To the best of our knowledge, this is the first study that has revealed a relation with myopic ocular change and autonomic nervous system in patients with glaucoma. The association of these two factors with glaucoma has already been well investigated, respectively.
An association between open-angle glaucoma and myopia has been reported for decades21. There have been many studies to explain the correlation between glaucoma and myopia22. In myopia, structures of optic nerve, including lamina, may be more vulnerable to glaucomatous damage. The shearing force caused by scleral deformation of myopia affects the lamina cribrosa23,24,25,26,27. This may be the main mechanism of glaucomatous damage in myopia23,24,25,26,27. There are also studies about myopia-related optic disc and retinal change such like the axis of tilt and tilt ratio and PPA28. Chameen et al.29 reported that beta-PPA was predominantly located in the temporal direction in eyes with disc tilt as myopic patients are predominantly temporally tilted. Tilted disc may exacerbate visual field defects16. Park et al.17 reported that the torsion direction of the optic disc may predict the location of VF damage. So, the indicators of myopic optic disc change are associated with glaucomatous damage.
There are many studies that hemodynamic instability can contribute to the onset and exacerbation of glaucoma30,31,32. Glaucoma patients with vascular dysregulation have impaired autoregulatory function, so they cannot respond appropriately to low perfusion pressure33,34. The pathogenesis of vascular dysregulation is not clearly known, but it is assumed to be due to dysfunction of ANS and endothelial vascular layer35. Systemic sympathetic or parasympathetic neuropathy has been reported in patients with POAG and NTG patients36,37,38. In particular, NTG patients have been reported to have abnormal autonomic nervous system, it would have affected ocular blood flow and structural damage8.
In our study, we described the correlation between myopic change parameter, namely the posterior scleral profile, and an autonomic dysfunction parameter, namely HRV. Nickla et al.18,39 tried to explain the relationship between myopia and autonomic nervous system by several experiments in chicks. They found abnormal ocular rhythms in chick having procedures like parasympathetic resection, which causes autonomic dysfunction18. They also reported that abnormal ocular rhythm results in abnormal ocular growth stimulation18.
We used Heart rate variability (HRV) to evaluate autonomic dysfunction. HRV is a non-invasive tool, which is widely used to evaluate the autonomic nervous system (ANS). HRV provides information about the functions of the sympathetic and parasympathetic nervous system40. HRV is defined as ‘the amount of fluctuations from the mean heart rate’41. It is mainly controlled by the continuous interaction of the ANS41. The HRV test has many indicators. Among them, the SDNN is considered the best indicator of the ANS42. It reflects all the cyclic components that affect variability, therefore it represents total variability and balance of SNS and PNS43. Autonomic nervous system dysfunction which can cause blood pressure problems may relate to hypertension, orthostatic intolerance, cardiac disease, and other disease states44. So it can cause fluctuation of blood pressure. When blood pressure is decreased and renal blood flow is decreased, juxtaglomerular cells convert the precursor prorenin into renin in the kidneys45. Renin breaks down angiotensinogen synthesized in the liver to make angiotensin I46. Angiotension I is converted to angiotensin II46. This angiotensin II has multiple effects in various organs including constricting blood vessels and producing aldosterone in the adrenal cortex45,46.
Meanwhile, it has been reported that ECM synthesis is regulated by sympathetic nervous system or angiotensin II47. So activated renin-angiotension system(RAS) affects the ECMs in many organs, then what about eyeballs? Sclera is composed of approximately 50% collagens and ECM such as proteoglygan, glycoproteins and matrix metalloproteinase. Therefore, We hypothesize that the renin angiotension system may have a effect on sclera. Especially events that occur in scleral extracellular matrix during childhood and young adulthood may be very important because it is the time when the eyeball is growing. The composition of extracellular matrix plays a very important role in determining the properties of the sclera, which affects the eyeball elongation48. Deformity of scleral canal (disc tilt, torsion, PPA) and thinning of sclera, especially posterior pole, is usually happens with elongation of the eyeball during childhood and young adulthood. We carefully suggest that people who have abnormality of HRV are more affected by activated renin-angiotensin system than normal people during childhood and young adulthood. So that may explain our result that posterior scleral deformity such as tilt ratio, FoBMO angle, axial length is associated with abnormality of HRV.
In our results, there was no statistical difference in refraction (spherical equivalent) between the two groups. The amount of refraction is determined by axial length, curvature and refractive index. Curvature myopia refers to a type of refractive error that develops when the cornea is curved too much. By contrast, index myopia is caused by change in the refractive index of the media such as cataracts or hydration of lens (diabetes, drugs)49. The pathophysiology of myopia that we are interested in is not just myopia (myopic refraction), but axial myopia. Because only axial myopia is associated with posterior scleral deformity and glaucomatous optic nerve damage.
We found a difference for axial length, tilt ratio and torsion degree of the optic disc in Chi-Square, independent t-test and logistical regression analysis, with only torsion degree being statistically significant for a multivariate(multiple) logistic regression analysis. It does not mean that the axial length, tilt ratio are not associated with HRV. Since all three factors: axial length, tilt and torsion, have similar mechanism in development, the association wound have been reduced in multivariate analysis, which adjust for confounding.
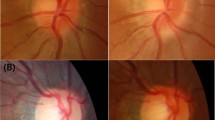
Figure 1 shows representative case. The patient of HiAD group shows a higher tilt ratio, torsion degree and PPA to disc ratio than patient of LoAD group.
A representative case. A1. A 46-year-old woman. Her SDNN of HRV was 34.87. She was classified as LoAD group. Her axial length was 28.31 mm. B1. A 32-year-old man. His SDNN of HRV was 14.71. He was classified as HiAD group. His axial length was 27.93 mm. A2. Tilt ratio was defined as the ratio between the longest diameter (LD) and the shortest diameter (SD) of the optic disc. Tilt ratio of LoAD group patient was 1.10. B2. Tilt ratio of HiAD group patient was 1.92. A3. Torsion degree was measured between the LD and the horizontal line connecting the fovea and the center of the optic disc. Torsion degree of LoAD group patients was 6.5 \(^\circ \). B3. Torsion degree of HiAD group patients was 17.5 \(^\circ \). A4. PPA/disc ratio was defined as the ratio between area of D and area of P. PPA/disc ratio of LoAD group patients was 0.51. B4. PPA/disc ratio of HiAD group patients was 0.96.
In summary, We found that patients with abnormality of HRV had more association with posterior scleral deformity such as disc tilt, FoBMO angle, axial length. And further studies are needed to explore this finding and mechanism.
Material and Methods
Patients
This study included 208 OAG patients who visited the Seoul St. Mary’s Hospital between September 2018 and October 2018. It was approved by Institutional review and Ethics Board of Seoul St. Mary’s Hospital and performed according to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all the subjects.
All patients enrolled underwent comprehensive ophthalmologic examination consisting of best-corrected visual acuity, intraocular pressure by Goldmann applanation tonometry. Anterior chamber angle evaluated by gonioscopy. Central corneal thickness were measured using ultrasound pachymetry (Tomey Corp, Nagoya, Japan), and axial length was measured by biometry (IOLMaster, Carl Zeiss Meditec, Dublin, CA, USA). Optic disc was examined with red-free fundus photography (Kowa nonmyd WX; Kowa Company Ltd., Tokyo,Japan). RNFL thickness was measured using the Cirrus OCT(Cirrus, version 6.0; Carl Zeiss Meditec). Global RNFL thickness was automatically calculated. VF was examined using the Swedish Interactive Threshold Algorithm standard 24-2 perimetry (Carl Zeiss Meditec, Dublin, CA, USA). History of disc hemorrhage (DH) was investigated through medical records. NTG was defined as the presence of an open anterior chamber angle, glaucomatous optic disc cupping by funduscopic examination and compatible repeatable VF damage, and IOP never exceeded 21 mmHg by a Goldmann applanation tonometer in repeated measurement on different days. Glaucomatous optic disc is increased cupping or loss(focal/diffuse) of neuroretinal rim. Glaucomatous VF was defined as a cluster of 3 or more non-edge points on pattern deviation map with a probability <5% of the healthy population, including at least one of these points with the probability of <1% of the healthy population; or VF is outside the normal limits on the glaucoma hemifield test for a pattern standard deviation (PSD) outside 95% normal limits, reliable test (<15% false negatives, <15% false positives and ≤33% fixation losses). Refractive errors (myopia, hyperopia, presbyopia) were usually corrected with a trial lens when performing VF tests. Mild myopia not exceeding −3 diopters was not corrected, astigmatism less than 1 diopter was corrected with spherical equivalent and astigmatism over −1.25 diopters was corrected with the corrective lens. And in myopia over −6 diopters, contact lenses were used when VF examination was performed50. Exclusion criteria included any other neurologic disorder and the taking of any drugs known to affect ANS or the cardiovascular system.
HRV assessment
The participants were asked to avoid activities that could affect blood pressure at least 2 hours before the test. The testing was performed over 5 minutes in controlled conditions. The echocardiography was monitored for 5 minutes by an experienced technician. The echocardiography signal was transferred to a Medicore Heart rate Analyzer, Model SA-3000P (Medicore, Seoul, Korea). The SDNN index is the mean of the standard of all the normal RR ECG wav intervals of the standard deviations of all the normal RR intervals. The parameter is primarily a measure of the autonomic effect on heart rate variability and characterize the total effect of autonomic blood circulation regulation43. A reduction of SDNN is correlated with left ventricular dysfunction indicating a high tone of heart sympathetic activity and has been found to be predictive of increased risk of sudden cardiac death51,52,53,54,55. Reduced SDNN mainly reflects sympathetic overactivity, and increased SDNN reflect parasympathetic overactivity56.
Patients were divided into 2 groups, according to their SDNN. LoAD group consisted of patients within the one standard deviation from the average of the SDNN measurements. And HiAD group consisted of patients outside one standard deviation from the average of the SDNN measurements, indicating that they had too higher or too lower SDNN of HRV. So HiAD group having deviated value was thought to have abnormality in HRV. it can cause fluctuation of blood pressure.
Posterior scleral profile (optic disc tilt, torsion, PPA to disc ratio, FoBMO angle)
Optic disc tilt, torsion, and PPA to disc ratio were measured from photographs by a two independent examiners(DYS and H-YLP) using the National Institutes of Health image-analysis software (ImageJ version 1.40; available at http://rsb.info.nih.gov/ij/index.html; developed by Wayne Rasband, National Institutes of Health, Bethesda, MD).
Optic disc tilt was defined as the ratio between the longest and shortest diameters of the optic disc (Figure 1A2,B2)13,17,57,58. The torsion of optic disc was identified and defined as the deviation of the long axis of the optic disc from the vertical meridian (Figure 1A3,B3)12,17,28. The technique of assessing the disc tilt and torsion has already been described and applied in previous investigations12,13,17,28,57,58.
The pixel areas of the PPA were calculated using the imageJ software, and the pixel area of the disc were also calculated. And PPA to disc ratio defined as the ratio between the PPA area and disc area(PPA/disc ratio = PPA area/disc area)(Figure 1A4,B4).
FoBMO angle determined as the angle between and the line connecting the fovea and BMO center and the horizontal meridian passing through the Bruch’s membrane opening (BMO) center. It was measured by spectral domain-OCT scans performed with the Heidelberg spectralis OCT(spectralis software v. 5.1.1.0, Eye Explorer Software 1.6.1.0; Heidelberg Engineering).
Statistical analysis
Sample size calculations were performed using the G*Power 3.1. The sample size calculation showed a power of 80 and alpha error of 0.05, for sample size of 160 in the LoAD group versus 40 in the HiAD group. The independent t-test and chi-square test for independent samples were used to assess the differences between groups. Binary logistic regression analyses were used to identify posterior scleral factors associated with autonomic dysfunction. A value of P < 0.2 in the simple binary logistic regression model was included in multiple model. A value of P < 0.05 indicated statistical significance. The independent variables were age, axial length, MD of the VF, PSD of the VF, PPA to disc ratio, FoBMO angle from spectral domain-OCT, tilt ratio, torsion degree. All statistical analysis were performed with SPSS for windows statistical software(ver.24.0; SPSS Inc, Chicago, Illinois, USA).
References
Weinreb, R. N., Aung, T. & Medeiros, F. A. The pathophysiology and treatment of glaucoma: a review. Jama 311, 1901–1911 (2014).
Haas, J. S. Low tension glaucoma. Transactions of the Pacific Coast Oto-Ophthalmological Society annual meeting 43, 153–160 (1962).
Chung, H. S., Harris, A., Kagemann, L. & Martin, B. Peripapillary retinal blood flow in normal tension glaucoma. The British journal of ophthalmology 83, 466–469 (1999).
Flammer, J. et al. The impact of ocular blood flow in glaucoma. Progress in retinal and eye research 21, 359–393 (2002).
Flammer, J., Konieczka, K. & Flammer, A. J. The primary vascular dysregulation syndrome: implications for eye diseases. The EPMA journal 4, 14 (2013).
Wierzbowska, J., Wierzbowski, R., Stankiewicz, A., Siesky, B. & Harris, A. Cardiac autonomic dysfunction in patients with normal tension glaucoma: 24-h heart rate and blood pressure variability analysis. The British journal of ophthalmology 96, 624–628 (2012).
Na, K. S., Lee, N. Y., Park, S. H. & Park, C. K. Autonomic dysfunction in normal tension glaucoma: the short-term heart rate variability analysis. Journal of glaucoma 19, 377–381 (2010).
Kurysheva, N. I., Shlapak, V. N. & Ryabova, T. Y. Heart rate variability in normal tension glaucoma: A case-control study. Medicine 97, e9744 (2018).
Park, H. Y., Park, S. H. & Park, C. K. Central visual field progression in normal-tension glaucoma patients with autonomic dysfunction. Investigative ophthalmology & visual science 55, 2557–2563 (2014).
Nitta, K., Sugiyama, K., Wajima, R. & Tachibana, G. Is high myopia a risk factor for visual field progression or disk hemorrhage in primary open-angle glaucoma. Clinical ophthalmology (Auckland, N.Z.) 11, 599–604 (2017).
Suzuki, Y. et al. Risk factors for open-angle glaucoma in a Japanese population: the Tajimi Study. Ophthalmology 113, 1613–1617 (2006).
How, A. C. et al. Population prevalence of tilted and torted optic discs among an adult Chinese population in Singapore: the Tanjong Pagar Study. Archives of ophthalmology (Chicago, Ill. : 1960) 127, 894–899 (2009).
Vongphanit, J., Mitchell, P. & Wang, J. J. Population prevalence of tilted optic disks and the relationship of this sign to refractive error. American journal of ophthalmology 133, 679–685 (2002).
Scott, R. & Grosvenor, T. Structural model for emmetropic and myopic eyes. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists) 13, 41–47 (1993).
Avetisov, E. S. & Savitskaya, N. F. Some features of ocular microcirculation in myopia. Annals of ophthalmology 9, 1261–1264 (1977).
Brazitikos, P. D., Safran, A. B., Simona, F. & Zulauf, M. Threshold perimetry in tilted disc syndrome. Archives of ophthalmology (Chicago, Ill. : 1960) 108, 1698–1700 (1990).
Park, H. Y., Lee, K. & Park, C. K. Optic disc torsion direction predicts the location of glaucomatous damage in normal-tension glaucoma patients with myopia. Ophthalmology 119, 1844–1851 (2012).
Nickla, D. L. & Schroedl, F. Effects of autonomic denervations on the rhythms in axial length and choroidal thickness in chicks. Journal of comparative physiology. A, Neuroethology, sensory, neural, and behavioral physiology, (2019).
Lauber, J. K., Boyd, J. E. & Boyd, T. A. Sympathetic denervation effects of avian eye development and aqueous fluid dynamics. Proceedings of the Society for Experimental Biology and Medicine. Society for Experimental Biology and Medicine (New York, N.Y.) 140, 351–356 (1972).
Schmid, G. F. et al. Autonomic denervations influence ocular dimensions and intraocular pressure in chicks. Experimental eye research 68, 573–581 (1999).
Mitchell, P., Hourihan, F., Sandbach, J. & Wang, J. J. The relationship between glaucoma and myopia: the Blue Mountains Eye Study. Ophthalmology 106, 2010–2015 (1999).
Fong, D. S., Epstein, D. L. & Allingham, R. R. Glaucoma and myopia: are they related? International ophthalmology clinics 30, 215–218 (1990).
Perkins, E. S. & Phelps, C. D. Open angle glaucoma, ocular hypertension, low-tension glaucoma, and refraction. Archives of ophthalmology (Chicago, Ill. : 1960) 100, 1464–1467 (1982).
Lotufo, D., Ritch, R., Szmyd, L. Jr. & Burris, J. E. Juvenile glaucoma, race, and refraction. Jama 261, 249–252 (1989).
Chihara, E. et al. Severe myopia as a risk factor for progressive visual field loss in primary open-angle glaucoma. Ophthalmologica. Journal international d’ophtalmologie. International journal of ophthalmology. Zeitschrift fur Augenheilkunde 211, 66–71 (1997).
Quigley, H. A. Reappraisal of the mechanisms of glaucomatous optic nerve damage. Eye (London, England) 1(Pt 2), 318–322 (1987).
Jonas, J. B., Gusek, G. C. & Naumann, G. O. Optic disk morphometry in high myopia. Graefe’s archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie 226, 587–590 (1988).
Samarawickrama, C. et al. Myopia-related optic disc and retinal changes in adolescent children from singapore. Ophthalmology 118, 2050–2057 (2011).
You, Q. S., Xu, L. & Jonas, J. B. Tilted optic discs: The Beijing Eye Study. Eye (London, England) 22, 728–729 (2008).
Choi, J., Jeong, J., Cho, H. S. & Kook, M. S. Effect of nocturnal blood pressure reduction on circadian fluctuation of mean ocular perfusion pressure: a risk factor for normal tension glaucoma. Investigative ophthalmology & visual science 47, 831–836 (2006).
Bonomi, L. et al. Vascular risk factors for primary open angle glaucoma: the Egna-Neumarkt Study. Ophthalmology 107, 1287–1293 (2000).
Tokunaga, T., Kashiwagi, K., Tsumura, T., Taguchi, K. & Tsukahara, S. Association between nocturnal blood pressure reduction and progression of visual field defect in patients with primary open-angle glaucoma or normal-tension glaucoma. Japanese journal of ophthalmology 48, 380–385 (2004).
Kashiwagi, K. et al. Circadian rhythm of autonomic nervous function in patients with normal-tension glaucoma compared with normal subjects using ambulatory electrocardiography. Journal of glaucoma 9, 239–246 (2000).
Drance, S. M., Douglas, G. R., Wijsman, K., Schulzer, M. & Britton, R. J. Response of blood flow to warm and cold in normal and low-tension glaucoma patients. American journal of ophthalmology 105, 35–39 (1988).
Sossi, N. & Anderson, D. R. Blockage of axonal transport in optic nerve induced by elevation of intraocular pressure. Effect of arterial hypertension induced by angiotensin I. Archives of ophthalmology (Chicago, Ill. : 1960) 101, 94–97 (1983).
Clark, C. V. & Mapstone, R. Systemic autonomic neuropathy in open-angle glaucoma. Documenta ophthalmologica. Advances in ophthalmology 64, 179–185 (1986).
Kumar, R. & Ahuja, V. M. A study of changes in the status of autonomic nervous system in primary open angle glaucoma cases. Indian journal of medical sciences 53, 529–534 (1999).
Brown, C. M., Dutsch, M., Michelson, G., Neundorfer, B. & Hilz, M. J. Impaired cardiovascular responses to baroreflex stimulation in open-angle and normal-pressure glaucoma. Clinical science (London, England : 1979) 102, 623–630 (2002).
Nickla, D. L., Rada, J. A. & Wallman, J. Isolated chick sclera shows a circadian rhythm in proteoglycan synthesis perhaps associated with the rhythm in ocular elongation. Journal of comparative physiology. A, Sensory, neural, and behavioral physiology 185, 81–90 (1999).
Friedman, B. H. & Thayer, J. F. Anxiety and autonomic flexibility: a cardiovascular approach. Biological psychology 47, 243–263 (1998).
Kim, G. M. & Woo, J. M. Determinants for heart rate variability in a normal Korean population. Journal of Korean medical science 26, 1293–1298 (2011).
Shaffer, F., McCraty, R. & Zerr, C. L. A healthy heart is not a metronome: an integrative review of the heart’s anatomy and heart rate variability. Frontiers in psychology 5, 1040 (2014).
Shaffer, F. & Ginsberg, J. P. An Overview of Heart Rate Variability Metrics and Norms. Frontiers in public health 5, 258 (2017).
Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 93, 1043-1065, (1996).
Galen, F. X. et al. Renin biosynthesis by human tumoral juxtaglomerular cells. Evidences for a renin precursor. The Journal of clinical investigation 73, 1144–1155 (1984).
Jakschik, B. A., Marshall, G. R., Kourik, J. L. & Needleman, P. Profile of circulating vasoactive substances in hemorrhagic shock and their pharmacologic manipulation. The Journal of clinical investigation 54, 842–852 (1974).
Dab, H. et al. Regulation of aortic extracellular matrix synthesis via noradrenergic system and angiotensin II in juvenile rats. Pharmaceutical biology 50, 1219–1225 (2012).
Harper, A. R. & Summers, J. A. The dynamic sclera: extracellular matrix remodeling in normal ocular growth and myopia development. Experimental eye research 133, 100–111 (2015).
Dubbelman, M. & Van der Heijde, G. L. The shape of the aging human lens: curvature, equivalent refractive index and the lens paradox. Vision Res 41, 1867–1877 (2001).
Aung, T. et al. Automated static perimetry: the influence of myopia and its method of correction. Ophthalmology 108, 290–295 (2001).
Bigger, J. T., Fleiss, J. L., Rolnitzky, L. M. & Steinman, R. C. The ability of several short-term measures of RR variability to predict mortality after myocardial infarction. Circulation 88, 927–934 (1993).
Dekker, J. M. et al. Low heart rate variability in a 2-minute rhythm strip predicts risk of coronary heart disease and mortality from several causes: the ARIC Study. Atherosclerosis Risk In Communities. Circulation 102, 1239–1244 (2000).
Malik, M. & Camm, A. J. Heart rate variability. Clinical cardiology 13, 570–576 (1990).
Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. European heart journal 17, 354–381 (1996).
Kleiger, R. E., Miller, J. P., Bigger, J. T. Jr. & Moss, A. J. Decreased heart rate variability and its association with increased mortality after acute myocardial infarction. The American journal of cardiology 59, 256–262 (1987).
Salles, G. F., Ribeiro, F. M., Guimaraes, G. M., Muxfeldt, E. S. & Cardoso, C. R. A reduced heart rate variability is independently associated with a blunted nocturnal blood pressure fall in patients with resistant hypertension. Journal of hypertension 32, 644–651 (2014).
Tay, E. et al. Optic disk ovality as an index of tilt and its relationship to myopia and perimetry. American journal of ophthalmology 139, 247–252 (2005).
Giuffre, G. Chorioretinal degenerative changes in the tilted disc syndrome. International ophthalmology 15, 1–7 (1991).
Author information
Authors and Affiliations
Contributions
Da Young Shin and Chan Kee Park wrote main manuscript text Soo Ji Jeon and Hae Young Lopilly Park prepared Figure 1. All authors reviewed the revised text and figure.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shin, D.Y., Jeon, S.J., Park, H.Y.L. et al. Posterior scleral deformation and autonomic dysfunction in normal tension glaucoma. Sci Rep 10, 8203 (2020). https://doi.org/10.1038/s41598-020-65037-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-65037-6
This article is cited by
-
Regional differences of the sclera in the ocular hypertensive rat model induced by circumlimbal suture
Eye and Vision (2023)
-
Association of choroidal blood flow with autonomic dysfunction in patients with normal tension glaucoma
Scientific Reports (2022)
-
The effect of anxiety and depression on progression of glaucoma
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.