Abstract
Women who have previously had an induced abortion (IA) before their first birth have been associated with preterm birth (PTB). However, previous studies on the PTB are inconsistent. Therefore, the aim of this study was to clarify the association between IA and PTB and low birth weight (LBW) for first-time mothers. A total of 3,684 Southern Chinese women who gave birth for the first time to a live singleton infants were recruited between January 2015 and December 2015 in the province of Guangdong, China. Univariable and multivariable analyses were conducted to determine whether IA was associated with PTB and LBW. Previous IA was not associated with increased risks of PTB or LBW, adjusted odds ratios were 0.80 (95% CI = 0.53 to 1.20) and 0.86 (95% CI = 0.57 to 1.31), respectively. Additionally, no significant associations were observed for infants born at before 37, before 32, and before 28 gestational weeks. And no significant associations were also observed for LBW measuring lower than 2500 grams and also measuring lower than 1500 grams. Our study suggested that a previous IA, as compared with women who reported no previous IA, does not increase the risk of PTB or LBW in subsequent pregnancy for the first-time mothers among Southern Chinese women.
Similar content being viewed by others
Introduction
Preterm birth (PTB), an important adverse pregnancy outcome, is one of the most important contributing factors to neonatal morbidity and mortality1. It affects approximately 14.9 million infants worldwide in 20102. Despite recent advances in medical care, its relative importance is still increasing. At least 70% of perinatal mortality are attributable to newborns weighing less than 2500 grams3,4, of whom the majority are born preterm. It is well established that the occurrence and progression of PTB is a complicated process, which multiple genetic and environmental factors are involved in5,6,7,8,9. Thus, elucidation of the etiological factors for the development of preterm would be of great help to develop the effectively preventative and therapeutic approaches for neonatal morbidity and mortality.
Induced abortion (IA) is something many women undergo at some point in their lives. According to World Health Organization’s (WHO) statistics, 30% of pregnancies in Europe end in abortion, with the highest and lowest sub-regional termination rates world-wide being in Eastern and Western Europe at 43 and 12, respectively, per 1,000 fertile women10. In China, IA is widely practiced, about 8 million legally IAs are performed annually11. The average annual rate of IA was 28.95% among Chinese married women 20–49 years old, according to the data from 1979 to 201012. IA not only does harm to the women13, particularly in adolescents and young women14, but also to the future child, e.g. PTB15 and low birth weight (LBW)16 children.
Previous studies have examined the relationship between IA (medical and surgical) and PTB, but an induced termination of pregnancy prior to the first birth adversely affecting the outcome of that birth has been previously debated17,18,19,20,21. There are evidences of an increased risk of PTB with many IAs prior to the first birth17,18,19,20. Nevertheless, some studies did not find an association between previous IA and PTB or LBW21,22,23,24. However, few studies have assessed the effect that IA have on the risk of PTB or LBW in a subsequent pregnancies for the first-time mothers among Southern Chinese women.
In view of the above controversies, we carried out a retrospective cohort study of 809 exposures with IA and 2875 non-exposures among Southern Chinese women to evaluate whether IA is associated with an increased risk of PTB or LBW in the subsequent pregnancy.
Results
Characteristics of the study subjects
The baseline maternal characteristics are shown in Table 1. IA was reported by 809 women, 588 of these reported one prior induced abortion, and the remaining 221 reported two or more prior IAs. There were 2,875 women who reported no prior IA. As expected, women who reported prior IA were slightly older compared with those with no prior IA (29.38 and 28.61 years old, respectively). Significant associations were also seen between health insurance, occupation, gravidity and education (all P < 0.01). However, no significant differences were observed for both groups with regard to BMI, gestational hypertension and caesarean section (all P > 0.05).
Association analysis between IA and PTB or LBW incidence risk
The associations between IA and the risk of PTB or LBW were presented in Table 2. Previous IA was not associated with increased risks of PTB or LBW, adjusted odds ratios (AOR) were 0.80 (95% CI = 0.53 to 1.20) and 0.86 (95% CI = 0.57 to 1.31), respectively. Moreover, we also categorized PTB separately for infants born at before 37, before 32 and before 28 gestational weeks, and no difference emerged (AOR = 0.83, 95% CI = 0.53 to 1.30; AOR = 0.64, 95% CI = 0.23 to 1.78; and AOR = 0.83, 95% CI = 0.09 to 7.55, respectively). Separately, no association was seen for infants with LBW less than 2500 grams and less than 1500 grams (AOR = 0.89, 95% CI = 0.56 to 1.43 and AOR = 0.77, 95% CI = 0.33 to 1.80, respectively).
Additionally, women with two or more prior IA’s had a weakness significantly higher risk of delivering preterm in a subsequent pregnancy before adjusted confound factors (OR = 1.61, 95% CI = 1.07 to 2.43), but this difference disappeared after adjusting for confounding factors (AOR = 1.09, 95% CI = 0.53 to 2.22). Meanwhile, the AOR for LBW was 0.83 (95% CI = 0.54 to 1.27) for women with 1 IA and 1.73 (95% CI = 0.77 to 3.86) for women with 2 or more IAs (Table 3).
Discussion
In the present study, we conducted a retrospective cohort study in a Southern Chinese women to explore the association between IA, PTB, and LBW risk. Our results demonstrated that women with a previous IA were not associated with the risk of PTB or LBW incidence in a subsequent pregnancy for the first-time mothers.
The effect of an induced abortion causing preterm birth in a subsequent pregnancy is very controversial. In a review of risk factors for PTB, Hogue et al.25 included studies published concerning PTB subsequent to IA from the early 1960s to the early 1980s. Most these studies suggested that the relationship between IA and PTB failed to reach conventional levels of statistical significance. Conversely, in the review by Thorp et al.26, it was suggested that IA increased risk for PTB in subsequent pregnancy.
In recent years, various studies have addressed this association, but with inconsistent findings. There are evidences of an increased risk of PTB with an IA prior to the first birth15,18,27,28,29,30. However, some studies did not find an association between previous IA and PTB24,31,32,33,34,35,36. Furthermore, the relationship between IA and LBW is also debated, a cohort study by Denmark30 showed that IA was associated with the risk of LBW incidence in subsequent live births. Conversely, another study18 contradicted this result suggesting that IA did not elevated the risk for LBW.
However, the association of IA with PTB or LBW showed by our study was consistent with the previous publication by Chen et al.31, Chen compared pregnancy outcomes in women with one previous mifepristone IA with pregnancy outcomes in women with no previous IA and in women with one previous surgical IA. The study demonstrated that a previous medical IA was not associated with increased the risk of PTB or LBW incidence, as compared with no previous IA or a previous surgical IA. Moreover, Raatikainen and colleagues24 suggested that PTB was higher among women with one or more IA. Nevertheless, no such association emerged between IA and PTB after the adjustments for potential confounding factors. Additionally, a review study from Atrash et al.22. explored the risk in PTB and LBW after early surgical IA and reported no association between IA and a higher risk of PTB and LBW in the subsequent birth. Various studies performed since then are in line with such results16,23,31,37.
Although we controlled for several confounding factors known to be associated with adverse pregnancy outcomes, we did not adjust for variables such as alcohol consumption and maternal smoking since only one woman reported tobacco use in our data. Thus, we regarded these two variables not as confounders in our analysis.
However, the findings have been inconsistent. The inconsistency that emerged among the studies can at least partially be explained by differences in study design or power, by multiple comparisons, by recall bias and by differences in the methods used to perform IA at different times and in different countries. Additionally, epidemiological studies have been showed that revision of the uterine cavity might be responsible for endometritis, which is more likely to be the result of traumatic procedures25,38. This could also contribute to the differences in several studies. In spite of the research of PTB, the underlying etiology contributing to PTB needs to be further elucidated.
There are several advantages in our study as compared to Chen’s study31. First, the time of collecting the data was 17 years later than the time of the previous study, during which time the abortion laws and health and socioeconomic status of women had been changed significantly. These changes may have impacted the rate of IA and the recovery after performing an IA, which has a direct impact on the outcome of subsequent pregnancy. Second, in the present study, we not only controlled the possible influence of confounding variables by applying multivariate logistic regression analysis on a variety of risk factors that were found to be associated with PTB or LBW in previous studies, but also included other variables in our analysis, such as ‘health insurance’ and ‘gravidity’, which were not included in Chen’s study. Finally, the population we collected was from Southern China, whereas the population in Chen's study was from Northern China, which is also an innovation in our research. However, potential limitations of this study should be considered. One of the limitations of this study is lack of detailed information on types of PTB (i.e., spontaneous or iatrogenic PTB). We could not estimate the association between IAs and special types of PTB. Besides, some women might deliberately make inaccurate statements regarding previous IA, perhaps out of a perceived stigma associated with having had IA.
In summary, our study suggested that a previous IA, as compared with women who reported no previous IA, does not increase the risk of PTB or LBW in subsequent pregnancy for the first-time mothers among Southern Chinese women.
Methods
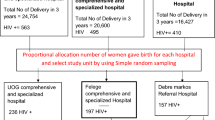
Study subjects
This retrospective cohort study was approved by the Medical Ethics Committee of the Third Affiliated Hospital of Guangzhou Medical University, Guangdong, China. All the methods in the present study were carried out in accordance with the approved guidelines. Between January 2015 and December 2015, a total of 3,684 women who had their first live birth at the Obstetric Department of The Third Affiliated Hospital of Guangzhou Medical University in Guangdong Province, China were included in the study.
The IA group (N = 809) consisted of women becoming mothers for the first time with a history of IA. Women pregnant with their first child and with no prior IA history were chosen for the non-IA group (N = 2,875). Women with prior deliveries, multifetal pregnancies, stillbirth, in vitro fertilization and embryo transfer were excluded from the study. For all subjects, the data were collected by interviewing women during their stay in the maternity unit, including maternal age, occupation, height and weight before of pregnancy, health insurance, education, gravidity and obstetric history. We derived the data on outcome measures, gestational week at birth (based on last menstruation and ultrasonography in early pregnancy), caesarean section and birth weight at delivery, from the hospital records. Gestational hypertension referred to diastolic pressure above 90 mmHg or systolic pressure above 140 mmHg on at least two occasions 24 hours apart, without proteinuria. Pre-pregnancy BMI, defined as the body weight in kilograms divided by the square of the height in metres (kg/m2), was obtained from the pre-pregnancy examinations at the first prenatal clinic visit, and all participants provided written informed consent.
Exposure was defined as the occurrence of a prior IA, including no previous IA (non-IA group), one previous IA or two or more previous IAs (IA group). For our analysis, we also categorized women who reported a prior IA as having had either one abortion or two or more abortions. Our primary outcome was PTB as birth before a 37-week gestation, we also categorized it as having occurred before 28 weeks, before 32 weeks and before 37 weeks. The secondary outcome was LBW that was defined as a birth weight less than 2500 grams at delivery, and very LBW was defined as infants weighing below 1500 grams.
Statistical analysis
Differences in the distribution of demographic characteristics between the IA group and non-IA group were evaluated by using the t test (for continuous variables) or χ2 test (for categorical variables). The associations between IA and development of PTB or LBW were estimated using the adjusted odds ratio (OR) and their 95% confidence intervals (CI), as estimators of the relative risks of PTB or LBW, which were calculated in logistic regression models with adjustment for age, health insurance, occupation, gravidity and education. We also conducted an unconditional logistic regression to estimate the odds ratio of having a PTB or LBW with one previous IA and two or more prior IAs as compare to those who reported no previous IA. A P value of less than 0.05 was considered as statistically significant. All statistical analyses were conducted in the SAS 9.4 software (SAS Institute, Inc.,Cary, NC, USA).
References
Boghossian, N. S. et al. Association of Antenatal Corticosteroids With Mortality, Morbidity, and Neurodevelopmental Outcomes in Extremely Preterm Multiple Gestation Infants. JAMA pediatrics 170, 593–601, https://doi.org/10.1001/jamapediatrics.2016.0104 (2016).
Blencowe, H. et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet 379, 2162–2172, https://doi.org/10.1016/S0140-6736(12)60820-4 (2012).
Hack, M. et al. School-age outcomes in children with birth weights under 750 g. The New England journal of medicine 331, 753–759, https://doi.org/10.1056/NEJM199409223311201 (1994).
Rutter, N. The extremely preterm infant. British journal of obstetrics and gynaecology 102, 682–687 (1995).
He, J. R. et al. Maternal IGF1 and IGF1R polymorphisms and the risk of spontaneous preterm birth. Journal of clinical laboratory analysis 31, https://doi.org/10.1002/jcla.22125 (2017).
Xiao, Q., Cui, Y. Y., Lu, J., Zhang, G. Z. & Zeng, F. L. Risk for Gestational Diabetes Mellitus and Adverse Birth Outcomes in Chinese Women with Polycystic Ovary Syndrome. International journal of endocrinology 2016, 5787104, https://doi.org/10.1155/2016/5787104 (2016).
Qiu, X. et al. Association of maternal serum homocysteine concentration levels in late stage of pregnancy with preterm births: a nested case-control study. The journal of maternal-fetal & neonatal medicine: the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstet, 1–5, https://doi.org/10.1080/14767058.2017.1351534 (2017).
Liu, G. J. et al. Associations of maternal PLA2G4C and PLA2G4D polymorphisms with the risk of spontaneous preterm birth in a Chinese population. Molecular medicine reports 15, 3607–3614, https://doi.org/10.3892/mmr.2017.6475 (2017).
Zhong, X. et al. Toll-like 4 receptor/NFkappaB inflammatory/miR-146a pathway contributes to the ART-correlated preterm birth outcome. Oncotarget 7, 72475–72485, https://doi.org/10.18632/oncotarget.11987 (2016).
World Health Organization. Facts on termination of pregnancy worldwide http://www.who.int/reproductivehealth/publications/unsafe_abortion/induced_abortion_2012.pdf?ua=1 (2012).
Ministry of Public Health of China: Health Yearbook of China. Beijing, Health Publishing Company of China (2008).
Wang, C. Induced abortion patterns and determinants among married women in China: 1979 to 2010. Reproductive health matters 22, 159–168, https://doi.org/10.1016/S0968-8080(14)43753-4 (2014).
Huang, Y. et al. A meta-analysis of the association between induced abortion and breast cancer risk among Chinese females. Cancer causes & control: CCC 25, 227–236, https://doi.org/10.1007/s10552-013-0325-7 (2014).
Thorp, J. M. Jr., Hartmann, K. E. & Shadigian, E. Long-term physical and psychological health consequences of induced abortion: review of the evidence. Obstetrical & gynecological survey 58, 67–79, https://doi.org/10.1097/01.OGX.0000045217.37578.0B (2003).
Hardy, G., Benjamin, A. & Abenhaim, H. A. Effect of induced abortions on early preterm births and adverse perinatal outcomes. Journal of obstetrics and gynaecology Canada: JOGC = Journal d’obstetrique et gynecologie du Canada: JOGC 35, 138–143, https://doi.org/10.1016/S1701-2163(15)31018-5 (2013).
Che, Y., Zhou, W., Gao, E. & Olsen, J. Induced abortion and prematurity in a subsequent pregnancy: a study from Shanghai. Journal of obstetrics and gynaecology: the journal of the Institute of Obstetrics and Gynaecology 21, 270–273, https://doi.org/10.1080/01443610120046396 (2001).
Ancel, P. Y. et al. History of induced abortion as a risk factor for preterm birth in European countries: results of the EUROPOP survey. Human reproduction 19, 734–740, https://doi.org/10.1093/humrep/deh107 (2004).
Henriet, L. & Kaminski, M. Impact of induced abortions on subsequent pregnancy outcome: the 1995 French national perinatal survey. BJOG: an international journal of obstetrics and gynaecology 108, 1036–1042 (2001).
Klemetti, R., Gissler, M., Niinimaki, M. & Hemminki, E. Birth outcomes after induced abortion: a nationwide register-based study of first births in Finland. Human reproduction 27, 3315–3320, https://doi.org/10.1093/humrep/des294 (2012).
Shah, P. S. & Zao, J. Knowledge Synthesis Group of Determinants of preterm, L. B. W. b. Induced termination of pregnancy and low birthweight and preterm birth: a systematic review and meta-analyses. BJOG: an international journal of obstetrics and gynaecology 116, 1425–1442, https://doi.org/10.1111/j.1471-0528.2009.02278.x (2009).
Zhou, W., Sorensen, H. T. & Olsen, J. Induced abortion and low birthweight in the following pregnancy. International journal of epidemiology 29, 100–106 (2000).
Atrash, H. K. & Hogue, C. J. The effect of pregnancy termination on future reproduction. Bailliere’s clinical obstetrics and gynaecology 4, 391–405 (1990).
Frank, P. I., McNamee, R., Hannaford, P. C., Kay, C. R. & Hirsch, S. The effect of induced abortion on subsequent pregnancy outcome. British journal of obstetrics and gynaecology 98, 1015–1024 (1991).
Raatikainen, K., Heiskanen, N. & Heinonen, S. Induced abortion: not an independent risk factor for pregnancy outcome, but a challenge for health counseling. Annals of epidemiology 16, 587–592, https://doi.org/10.1016/j.annepidem.2006.01.007 (2006).
Hogue, C. J., Cates, W. Jr. & Tietze, C. The effects of induced abortion on subsequent reproduction. Epidemiologic reviews 4, 66–94 (1982).
Thorp, J. M., Hartmann, K. E. & Shadigan, E. Long-term physical and psychological health consequences of induced abortion: a review of the evidence. The Linacre quarterly 72, 44–69 (2005).
de Haas, I., Harlow, B. L., Cramer, D. W. & Frigoletto, F. D. Jr. Spontaneous preterm birth: a case-control study. American journal of obstetrics and gynecology 165, 1290–1296 (1991).
Lang, J. M., Lieberman, E. & Cohen, A. A comparison of risk factors for preterm labor and term small-for-gestational-age birth. Epidemiology 7, 369–376 (1996).
Pickering, R. M. & Forbes, J. F. Risks of preterm delivery and small-for-gestational age infants following abortion: a population study. British journal of obstetrics and gynaecology 92, 1106–1112 (1985).
Zhou, W., Sorensen, H. T. & Olsen, J. Induced abortion and subsequent pregnancy duration. Obstetrics and gynecology 94, 948–953 (1999).
Chen, A. et al. Mifepristone-induced early abortion and outcome of subsequent wanted pregnancy. American journal of epidemiology 160, 110–117, https://doi.org/10.1093/aje/kwh182 (2004).
Frank, P. I., Kay, C. R., Lewis, T. L. & Parish, S. Outcome of pregnancy following induced abortion. Report from the joint study of the Royal College of General Practitioners and the Royal College of Obstetricians and Gynaecologists. British journal of obstetrics and gynaecology 92, 308–316 (1985).
Lao, T. T. & Ho, L. F. Induced abortion is not a cause of subsequent preterm delivery in teenage pregnancies. Human reproduction 13, 758–761 (1998).
Park, T. K., Strauss, L. T., Hogue, C. J. & Kim, I. S. Previous experience of induced abortion as a risk factor for fetal death and preterm delivery. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics 22, 195–202 (1984).
Virk, J., Zhang, J. & Olsen, J. Medical abortion and the risk of subsequent adverse pregnancy outcomes. The New England journal of medicine 357, 648–653, https://doi.org/10.1056/NEJMoa070445 (2007).
Parazzini, F. et al. Does induced abortion increase the risk of preterm birth? Results from a case-control study. Gynecologic and obstetric investigation 69, 40–45, https://doi.org/10.1159/000253848 (2010).
Mandelson, M. T., Maden, C. B. & Daling, J. R. Low birth weight in relation to multiple induced abortions. American journal of public health 82, 391–394 (1992).
Holmlund, S. et al. Induced abortion - impact on a subsequent pregnancy in first-time mothers: a registry-based study. BMC pregnancy and childbirth 16, 325, https://doi.org/10.1186/s12884-016-1109-3 (2016).
Acknowledgements
We would like to express our gratitude to all subjects who participated in this current study.
Author information
Authors and Affiliations
Contributions
L.K. contributed to analysis and interpretation of data, and drafted the article. W.L. contributed to conception and design. Y.L. assisted in the analysis and interpretation of the data. W.O. contributed to acquisition of data. Z.L. contributed to conception and design, interpretation of the results and critical revision of the manuscript for important intellectual content. All authors aided in the design of the study, in the interpretation of the data and critical revision of the manuscript for important intellectual content, and all authors approved the final version.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ke, L., Lin, W., Liu, Y. et al. Association of induced abortion with preterm birth risk in first-time mothers. Sci Rep 8, 5353 (2018). https://doi.org/10.1038/s41598-018-23695-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-23695-7
This article is cited by
-
Cultural considerations and beliefs surrounding preterm birth in Kenya and South Africa
Reproductive Health (2023)
-
The effect of previous induced abortion history on the assisted reproduction outcomes
Archives of Gynecology and Obstetrics (2023)
-
Association of induced abortion with hypertensive disorders of pregnancy risk among nulliparous women in China: a prospective cohort study
Scientific Reports (2020)
-
Determinants and adverse perinatal outcomes of low birth weight newborns delivered in Hawassa University Comprehensive Specialized Hospital, Ethiopia: a cohort study
BMC Research Notes (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.