Abstract
Adverse birth outcomes are a common cause of health problems in developing nations and have a significant negative impact on infant health as well as financial costs to families, communities, and the world. Mothers with HIV may be at increased risk of adverse birth outcomes. However, there is a limited study about adverse birth outcomes among mothers with HIV around the world including in Ethiopia. Therefore this study aimed to assess adverse birth outcomes and associated factors among mothers with HIV Facility based cross-sectional study was conducted among mothers with HIV who gave birth in northwest Amhara region referral hospitals from September 2016 to September 2019. Simple random sampling was used to select 590 mothers. Bivariable and multivariable logistic regressions were carried out to identify factors. Statistical significance was declared by using a p-value < 0.05. An adjusted odds ratio was used to show the magnitude of the association. Out of a total of 590 mothers, the prevalence of adverse birth outcomes among HIV-positive mothers was 21% (95% CI 17.8–24.6%). History of spontaneous abortion [AOR = 1.9, 95% CI (1.19, 3.70)], PROM [AOR = 3.55, 95% CI (1.72, 7.30)], opportunistic infection [AOR = 3.38, 95% CI (1.50, 8.22)], pre-pregnancy BMI of < 18.5 [AOR = 5.61, 95% CI (1.97, 15.91)], MUAC < 23 cm [AOR = 2.56, 95% CI (1.10, 5.97)], and ANC visit of < 4 times [AOR = 3.85, 95% CI (2.34, 6.55)] were significantly associated with Adverse birth outcome. The prevalence of adverse birth outcomes was high. Abortion history, MUAC, BMI, Opportunistic infection, PROM, and a number of ANC visits were associated with adverse birth outcomes. This study suggests to increase number of antenatal care follow-ups, prevent and treat opportunistic infections, and focus on early detection and treatment of pregnancy-related complication
Similar content being viewed by others
Introduction
HIV continues to be a burden on women and children worldwide1. In 2019, 37.9 million people were living with HIV2. The sub-Saharan region is the most affected place in the world with 25.6 million people living with HIV3. In Ethiopia by 2018, nearly 690,000 people were living with HIV/AIDS and 11,000 people have died from AIDS4. Although HIV infection has been reported to have little effect on pregnancy outcomes in the developed world, early studies from sub-Saharan Africa suggest that infants of mothers with HIV may be at increased risk of adverse pregnancy outcomes such as lower birth weight, prematurity, and perinatal and neonatal death5,6.
Each year, 15 million babies are preterm birth around the world7 and preterm birth is the leading cause of neonatal deaths which is contributing to 35% of the world’s neonatal mortality8. Globally 20.5 million live births is suffered from LBW in 2015 almost half of them in Southern Asia which is 9.8 million and about one-quarter of all LBW newborns are in sub-Saharan Africa9. Worldwide, over 2.6 million deliveries are stillbirths 98% of which occur in low and middle-income countries; 77% in South Asia and sub-Saharan Africa10.
Adverse birth outcomes are a common cause of health problems in developing nations and have a significant negative impact on infant health as well as emotional and financial costs to families, communities, and the world, especially in resource-constrained settings with underdeveloped health systems and weak access to and use of health services11. Children born with low birth weight and preterm are more likely to die prematurely compared to infants of normal birth weight and gestational age12. Likewise, these children experience more morbidity, both in the short and long term. Among these respiratory distress, heart problems, chronic lung disorders, growth impairment, blindness or low vision, deafness, cognitive impairment, and cerebral palsy are the problems associated with low birth weight and preterm babies13,14. There is also a greater vulnerability to infectious diseases due to a poorer immune response15.
Studies conducted in different areas reported risk factors for Adverse birth outcomes: low socio-economic status, MUAC < 23 cm, pregnancy-related complications and history of preterm birth, age less than 20, PROM, UTI, multiple pregnancies, preeclampsia, fetal malformation, polyhydramnios, antepartum hemorrhage, previous abortion, residence, lack of antenatal care, maternal disease, null parity, The presence of chronic illness, the absence of antenatal follow-up, HIV status of the mother, CD4 count, Viral load, WHO clinical stage, and anemia were found to be significantly associated with Adverse birth outcomes16,17,18,19,20,21.
In Ethiopia, globally recommended effective strategies have been implemented for a newborn with an adverse birth outcome with given emphasis on the packages of care provided at the prenatal, ante-natal, intrapartum, and postnatal periods. However, the outcome during pregnancy and delivery periods is a major challenge in realizing the seated goal of Sustainable Development Goals. While the effect of HIV infection on maternal morbidity, mortality, and vertical transmission to her offspring is well established. But there is a limited study about adverse birth outcomes among mothers with HIV in Ethiopia. Therefore, this study aims to assess adverse birth outcomes and associated factors among HIV-positive mothers.
Methodology
Study design and period
An institutional-based cross-sectional study was conducted among mothers delivered from September 2016 to September 2019 in northwest Amhara region referral hospitals and the data was extracted from March 3 to May 18/2020.
Study area
Amhara national region is one of the ten national states in Ethiopia which is found in the Northern part of Ethiopia. The region has 80 hospitals, 847 health centers, and 3342 health posts. there are 6 referral hospitals—namely Gondar University Comprehensive Specialized Hospital (GUCSH), Felegehiwot Comprehensive Specialized Hospital (FCSH), Dessie Referral Hospital (DRH), Debre-Markos Referral Hospital (DMRH), Debre-Birhan Referral Hospital (DBRH) and Debre tabor referral hospitals. Three out of six referral hospitals were found in the Northwest part of the Amhara region. These include: —the University of Gondar comprehensive and specialized Hospital (UoGCSH), Felege Hiwot comprehensive, and specialized hospital (FHCS), and Debre Markos referral hospital. Each referral hospital’s catchment population is estimated to be 5–7 million people. The annual average number of births in each hospital is 6000 per year. according to the hospital report. All three hospitals are providing full ANC/PMTCT, ART, delivery services, and ultrasound-guided obstetric care.
Eligibility criteria
All mothers with HIV delivered from September 2016–September 2019 in northwest Amhara region referral hospitals with a gestational age of 28 weeks and above were included in the study. However, mothers who had unknown or unreliable last normal menstrual period (LNMP) with the absence of ultrasound evidence and a mother with unrecorded birth outcome were excluded from the study.
Variables of the study
The dependent variable in this study was the adverse birth outcome. Whereas Socio-demographic, obstetric, medical, nutritional, and HIV-related variables were the independent variables. This includes age, residence, educational status, marital status history of substance use, including alcohol drinking and smoking, nutritional counseling during ANC, iron and folic acid supplementation during pregnancy, pre-pregnancy BMI, MUAC, CD4 count, viral load, WHO clinical stage of the disease, initiation of ART, time of initiation of ART, time of diagnosis with HIV, types of ARV, anemia, chronic medical disease, Urinary tract infection (UTI), pregnancy-induced hypertension (PIH), Antepartum hemorrhage (APH), the premature rapture of the membrane (PROM), previous history of abortion, previous history of stillbirth, parity, and gravidity.
Operational definition
Adverse birth outcomes: A woman who had at least one of the following stillbirth, low birth weight, preterm birth22.
Preterm birth: Preterm is defined as babies born alive before 37 weeks of gestation but after viability (28 weeks of gestation) and gestational age was calculated based on LNMP or first-trimester ultrasound result23.
Low birth weight: a birth weight < 2500 g irrespective of gestational age24.
Stillbirth: dead birth after the 28th week of gestation and before the expulsion from the uterus25.
APH: defined as any vaginal bleeding in the mother after 28 weeks of gestation as documented in the records by the attending clinician26.
PIH: defined clinically as a blood pressure of > 140/90 mmHg after 20 weeks of gestation with or without proteinuria and/or edema as diagnosed and documented by the attending clinician26.
Anemia: documented Hgb level below 11gm/dl laboratory diagnosis26.
UTI: Defined as a documented clinical/laboratory diagnosis of UTI at any time during the pregnancy26.
Sample size determination and sampling procedure
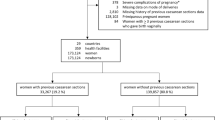
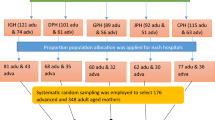
The required sample size was determined by using the single population proportion formula n = za2/2p(1 − p)/d2 by considering the prevalence PTB among mothers with HIV was 16.6%16, 95% confidence interval (CI), 3% margin of error to yield a total of 590 study participants. The total sample size was proportionally allocated for the three Hospitals depending on their load of delivery. A simple random sampling technique was employed to select the study participant’s medical records. The delivery registration logbooks were used as a sampling frame and selected each record for our study used a computer-generated random number. Whenever the selected chart did not fulfill the inclusion criteria, the next medical record was considered (Fig. 1.).
Data collection tool
The patient's medical records were used as a source of data. The data, consisting of socio-demographic variables, clinical and obstetric history as well as birth outcome, were collected using a data extraction tool. Maternal BMI was determined by using the mother’s pre-pregnancy, initial weight, and height from their ART and PMTCT follow-up. Newborn weight was measured using standard beam balance within the first hour of birth Six Bachelor of science (BSc) Midwives collected the data, while 3 midwives who have a second degree in clinical midwifery supervised the data collection process. Data quality was maintained by the following data quality control mechanisms; A 5% preliminary chart review was conducted in the Gondar university comprehensive and specialized hospital before the actual data collection and amendments were considered based on the result of a preliminary chart review. One day of training was given to data collectors and supervisors. Strict supervision of the data collection was carried out throughout the data collection period. The collected data was checked for its consistency and completeness before any attempt to enter, code, and analyze it.
Data processing and analysis
Data were coded and then entered using EPI data version 4.6 and exported to SPSS. The final statistical analysis was done by SPSS version 25. Before analysis, data were cleaned using frequency; listing, and sorting to identify any missed values, and then corrections were made by revising the original questionnaire. There are different techniques of missing data management. Deletion, replacement using the mean or mode of the data (mean substitution/replacement) or predicted values from a regression to substitute the missing values. So for this study, we had used replacement by mean for continuous and Mode for categorical variable if less than 20% of values are missed in one variable, but if more than 20% of values are missed in one variable, we discard the variables. Descriptive statistics were made for categorical variables using frequencies. The result was presented using texts and tables. a multivariable binary logistic regression model was used to assess the association between dependent and independent variables. P-value < 0.05 and Adjusted Odds Ratio (AOR) with 95% CI was used to declare statistically significant predictors in multivariable analysis.
Ethical approval and informed consent of participants
Ethical approval was obtained and the need for informed consent was waived by the ethical review committee of the Institute of public health on behalf of the Institutional Review Board (IRB) of the University of Gondar. Permission was obtained from the clinical director of each hospital. Since this study uses secondary data to ensure confidentiality Personal Identifiers Were not used on the data collection form, and all data were kept strictly confidential and used only for the study purposes. The research was conducted according to the Helsinki declarations.
Result
Socio-demographic and HIV-related characteristics of mothers
Regarding sociodemographic variable such as: educational status and occupational status had missing values of 30 and 43 respectively. These missing values replaced by their Modal value. The study result showed that the majority 564 (95.6%) of respondents were from an urban area and the rest were from a rural area. Regarding the religion of respondents; the majority 553 (93.7%) were orthodox followers and the rest were Muslim and protestant followers. Almost all 584 (99%) mothers with HIV received ARV intervention. Most (84.4%) mothers started their HAART before pregnancy. Regarding their adherence, almost all 578 (98%) have good adherence (Table 1).
Nutrition and medical-related characteristics of mothers
Regarding nutrition variable such as: pre pregnancy BMI and MUAC had missing values of 25 and 14 respectively. These missing values replaced by the mean value. Almost all 583 (98.81%) respondents had taken iron/folate during pregnancy Among those who took iron/folate during pregnancy, 359 (61.58%) of mothers taken with a duration of fewer than 3 months. Almost all 583 (98.81%) respondents received nutritional counseling during their ANC visit. A majority, 524 (88.81%) and 547 (92.71%), of mothers, had MUAC ≥ 23 cm and pre-pregnancy BMI of ≥ 18.5 respectively. A few proportions 36 (6.10%) of mothers are anemic and the rest/majority 554 (93.90%) of them had no anemia. Regarding medical conditions, about 31 (5.25%) had STI and 43 (7.29%) had UTI.
Pregnancy and labor-related complications of the mothers
Almost all 585 (99.15) mothers with HIV have ANC follow-ups. Only 27 (4.58%) of mothers had prolonged labor the rest/majority of them don’t have prolonged labor (Table 2).
Prevalence of adverse birth outcome
This study's finding showed that the prevalence of adverse birth outcomes among HIV-positive mothers was 21.4% (95% CI 18–25%). Out of 590 births 10 (1.7%) were stillbirth, 98 (16.6%) were LBW, 74 (12.5%) were preterm, 5 (0.8%) were both stillbirth and LBW, 50 (8.5%) LBW and preterm, 4 (0.68%) Still birth and preterm, and 4 (0.68%) were Still birth, LBW and preterm.
Determinants of adverse birth outcome
In multivariable analysis; history of spontaneous abortion, PROM, presence of opportunistic infection, BMI, MUAC, and ANC visit was significantly associated with adverse birth outcome. This study result showed that having a history of spontaneous abortion increases the risk of adverse birth outcomes by 1.9 times [AOR = 1.9, 95% CI (1.19, 3.70)]. The odds of adverse birth outcomes among mothers who had PROM during current pregnancy were 3.55 times [AOR = 3.55, 95% CI (1.72, 7.30)] higher as compared with their counterparts and other variables kept constant. Regarding opportunistic infection; HIV positive mothers with opportunistic infection were 3.38 times [AOR = 3.38, 95% CI (1.50, 8.22)] more likely to develop adverse birth outcomes as compared to those who don’t have an opportunistic infection and the effect of other variables remained constant. Those HIV-positive mothers with pre-pregnancy BMI of < 18.5 were 5.61 times [AOR = 5.61, 95% CI (1.97, 15.99)] more likely to have an adverse birth outcome as compared with their counterparts.
The study result showed that a mother with MUAC < 23 cm increases the risk of adverse birth outcome by 2.56 times [AOR = 2.56, 95% CI (1.10, 5.97)] as compared to those with MUAC ≥ 23 cm and other variables remained constant. Regarding ANC visits; mothers with ANC visits of < 4 times were 3.85 times [AOR = 3.85, 95% CI (2.34, 6.55)] more likely to have adverse birth outcomes as compared to mothers with ≥ 4 ANC visits (Table 3).
Discussion
The finding of the study showed that the prevalence of adverse birth outcomes was 126 (21.4% 95% CI 18–25%) among which 10 (1.7%) were stillbirth, 74 (12.5%) were preterm and 98(16.6%) were low birth weight. These figures were comparable with findings from studies conducted in Hosanna (24.5%)13, Hawassa (18.3%), Tanzania (18%), and Ghana (19%) of mothers who experienced adverse birth outcomes27,28.
The overall prevalence of adverse birth outcomes in this study was slightly lower than in studies conducted in Ethiopia, Dessie, 32.5%24 The discrepancy might be due to a difference in the study area and study participant's residents and age group. the study conducted in Dessie used 30–40% of rural resident participants and rural resident mothers are highly prone to adverse birth outcome than those living in urban29 and 15% of study participants in Dessie was Age group < 20 years and this age group is highly prone adverse birth outcome13,30.
The overall prevalence of adverse birth outcomes in this study is slightly higher than in a study done in Kembata (13.9%)25 this might be due to the difference in the study area, this study is done in referral hospitals whereas a study done in Kembata were in a health center and primary hospital. This may be because most normal deliveries take place in health centers while more complicated ones are referred to the tertiary hospital contributing to higher rates of adverse birth outcomes at referral hospitals20 and study participants in this study were HIV positive and HIV increases the risk of having adverse birth outcome23,31 or it might be due to compromised immune system of HIV positive mothers increase the risk of opportunistic infection, which contributes to the occurrence of adverse birth outcome.
Mothers who had opportunistic infections during pregnancy were found to be more than 3 times more likely to have Adverse birth outcomes than mothers who did not have Opportunistic infections. this finding is consistent with studies done in Nigeria32. This might be due to opportunistic infections compromising the nutritional status of the mother and fetal growth, for instance, infants from mothers with syphilis are often premature33.
In HIV-positive women the risk of having adverse birth outcomes were more than fourfold higher in a mother who had pre-pregnancy BMI less than 18.5 when compared with mothers having pre-pregnancy BMI ≥ 18.5. This result was similar to a study done in northwest Ethiopia public hospitals16. Moreover, In these findings mothers with MUAC, less than 23 cm were also found to experience adverse birth outcomes when compared with those with MUAC greater than 23 cm this result is in agreement with the study done in Dessie referral hospital20 This might be due to intergenerational effect of malnutrition that leads to LBW29 or poor nutritional status of the mother compromised the immune system and increase the risk of opportunistic infections that leads to preterm birth.
In this study, mothers with less than four times ANC visits were 3.5 times at high risk to have Adverse birth outcomes than those with four and more visits. This result was similar with study done in Mekell Hospital30 Debre tabor23, Jima34, Dodola town35, and Metu36. This might be due to the lack of adequate ANC visits decreases the chance of identifying risks factors of Adverse birth outcome early and providing appropriate interventions23.
Pregnancy-related complication during the current pregnancy was significantly associated with Adverse birth outcome, according to the finding of this research the risk of having adverse birth outcome among mothers who had PROM during the current pregnancy were more than 3 times higher than those mothers who had no PROM. This finding is consistent with a study done Debre tabor23, East Africa37, Ghana and Kenyatta national hospital38,39, Axum and Adwa public hospitals40, and Hosanna13. This might be due to that labor will spontaneously initiate within a week after preterm PROM23, or this might be due to -provider-initiated early termination of pregnancy to manage pregnancy-related complications20.
Limitation of study
Since this study is hospital-based, it doesn’t include mothers who gave birth at home, which makes it difficult to conclude the general population. In addition, the data used were secondary there may be bias and incomplete information or missing variables.
Data availability
Data will be available upon request from the corresponding author.
Abbreviations
- AIDS:
-
Acquire immune deficiency syndrome
- ANC:
-
Antenatal care
- AOR:
-
Adjusted odd ratio
- APH:
-
Anti partum hemorrhage
- ART:
-
Anti-retroviral treatment
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- COR:
-
Crude odds ratio
- DM:
-
Diabetes mellitus
- HAART:
-
Highly active anti-retroviral therapy
- HIV:
-
Human immune virus
- HTN:
-
Hypertension
- LBW:
-
Low birth weight
- LNMP:
-
Last normal menstrual period
- MUAC:
-
Mid upper arm circumference
- PIH:
-
Pregnancy induced hypertension
- PMTCT:
-
Prevention of mother to child transmission
- PROM:
-
Premature rupture of membrane
- PTB:
-
Pre term birth
- SD:
-
Standard deviation
- SPSS:
-
Statistical package for social science
- UOG:
-
University of Gondar
- UTI:
-
Urinary tract infection
- WHO:
-
World Health Organization
References
Organization WH. AIDS Epidemic Update: December 2009 (WHO Regional Office Europe, 2010).
UNAIDS. Global Statistics of HIV/AIDS (UNAIDS, 2019).
WHO. HIV/AIDS Fact Sheet (World Health Organization, 2018).
CIA. Ethiopia HIV_AIDS-adult prevalence rate-Demographics (2018).
van Benthem, B. H. et al. Pregnancies before and after HIV diagnosis in a European cohort of HIV-infected women. AIDS 14(14), 2171–2178 (2000).
Leroy, V. et al. Effect of HIV-1 infection on pregnancy outcome in women in Kigali, Rwanda, 1992–1994. AIDS 12(6), 643–650 (1998).
Soon, B. T. The Global Action Report on Preterm Birth (World Health Organization, 2012).
Gladstone, M., Oliver, C. & Van den Broek, N. Survival, morbidity, growth and developmental delay for babies born preterm in low and middle income countries—A systematic review of outcomes measured. PLoS ONE 10(3), e0120566 (2015).
Blencowe, H. et al. National, regional, and worldwide estimates of low birthweight in 2015, with trends from 2000: A systematic analysis. Lancet Glob. Health 7(7), e849–e860 (2019).
Lawn, J. E. et al. Stillbirths: Rates, risk factors, and acceleration towards 2030. Lancet 387(10018), 587–603 (2016).
Lee, A. C. et al. National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle-income countries in 2010. Lancet Glob. Health 1(1), e26–e36 (2013).
Liu, L. et al. Global, regional, and national causes of child mortality: An updated systematic analysis for 2010 with time trends since 2000. Lancet 379(9832), 2151–2161 (2012).
Abdo, R., Endalemaw, T. & Tesso, F. Prevalence and associated factors of adverse birth outcomes among women attended maternity ward at Negest Elene Mohammed Memorial General Hospital in Hosanna Town, SNNPR, Ethiopia. J. Women’s Health Care. 5(4), 324 (2016).
Martin, J. A. Born a bit too early: recent trends in late preterm births. (2009).
Tripathy, P. Clinical characteristics & morbidity pattern among low birth weight babies. Age 20, 20–30 (2014).
Kebede, B., Andargie, G. & Gebeyehu, A. Birth outcome and correlates of low birth weight and preterm delivery among infants born to HIV-infected women in public hospitals of Northwest Ethiopia. health 5(07), 25 (2013).
Adane, A. A., Ayele, T. A., Ararsa, L. G., Bitew, B. D. & Zeleke, B. M. Adverse birth outcomes among deliveries at Gondar University hospital, Northwest Ethiopia. BMC Pregnancy Childbirth. 14(1), 1–8 (2014).
Zack, R. M. et al. Risk factors for preterm birth among HIV-infected Tanzanian women: A prospective study. Obstet. Gynecol. Int. 2014 (2014).
Yu, L. et al. Pregnancy outcomes and risk factors for low birth weight and preterm delivery among HIV-infected pregnant women in Guangxi, China. Chin. Med. J. 125(03), 403–409 (2012).
Cherie, N. & Mebratu, A. Adverse birth out comes and associated factors among delivered mothers in dessie referral hospital. North East Ethiopia 1–6 (2018).
Fentie, E. A., Yeshita, H. Y. & Bokie, M. M. Low birth weight and associated factors among HIV positive and negative mothers delivered in northwest Amhara region referral hospitals, Ethiopia, 2020 a comparative crossectional study. PLoS ONE 17(2), e0263812 (2022).
Adane, A. A., Ayele, T. A., Ararsa, L. G., Bitew, B. D. & Zeleke, B. M. Adverse birth outcomes among deliveries at Gondar University hospital, Northwest Ethiopia. BMC Pregnancy Childbirth 14(1), 90 (2014).
Mekonen, D. G., Yismaw, A. E., Nigussie, T. S. & Ambaw, W. M. Proportion of Preterm birth and associated factors among mothers who gave birth in Debretabor town health institutions northwest Ethiopia. BMC Res. Notes. 12(1), 2 (2019).
Cherie, N. & Mebratu, A. Adverse birth out comes and associated factors among delivered mothers in Dessie Referral Hospital. North East Ethiopia. 1–6 (2018).
Lolaso, T., Oljira, L., Dessie, Y., Gebremedhin, M. & Wakgari, N. Adverse birth outcome and associated factors among newborns delivered in public health institutions Southern Ethiopia. East Afr. J. Health Biomed. Sci. 3(2), 35–44 (2019).
Wagura, P., Wasunna, A., Laving, A., Wamalwa, D. & Ng’ang’a, P. Prevalence and factors associated with preterm birth at Kenyatta National Hospital. BMC Pregnancy Childbirth. 18(1), 107 (2018).
Watson-Jones, D. et al. Adverse birth outcomes in United Republic of Tanzania: Impact and prevention of maternal risk factors. Bull. World Health Organ. 85, 9–18 (2007).
Asundep, N. N. et al. Determinants of access to antenatal care and birth outcomes in Kumasi, Ghana. J. Epidemiol. Glob. Health. 3(4), 279–288 (2013).
Gebremedhin, M., Ambaw, F., Admassu, E. & Berhane, H. Maternal associated factors of low birth weight: A hospital based cross-sectional mixed study in Tigray, Northern Ethiopia. BMC Pregnancy Childbirth. 15(1), 222 (2015).
Bugssa, G., Dimtsu, B. & Alemayehu, M. Socio demographic and maternal determinants of low birth weight at Mekelle Hospital, Northern Ethiopia: A cross sectional study. Am. J. Adv. Drug Deliv. 2(5), 609–618 (2014).
Xiao, P.-L. et al. Association between maternal HIV infection and low birth weight and prematurity: A meta-analysis of cohort studies. BMC Pregnancy Childbirth 15(1), 246 (2015).
Ezechi, O. et al. Pregnancy, obstetric and neonatal outcomes in HIV positive Nigerian women. Afr. J. Reprod. Health 17(3), 160–168 (2013).
Dreyfuss, M. L. et al. Determinants of low birth weight among HIV-infected pregnant women in Tanzania. Am. J. Clin. Nutr. 74(6), 814–826 (2001).
Abaraya, M., Seid, S. S. & Ibro, S. A. Determinants of preterm birth at Jimma University Medical Center, southwest Ethiopia. Pediatr. Health Med. Ther. 9, 101 (2018).
Woldeyohannes, D., Kene, C., Gomora, D., Seyoum, K. & Assefa, T. Factors associated with preterm birth among mothers who gave birth in Dodola Town Hospitals, Southeast Ethiopia: Institutional based cross sectional study. Clin. Mother Child Health. 16(317), 2 (2019).
Nekatibeb, G. Analysis of birth weight in Metu Karl Hospital South West Ethiopia. Ethiop. Med. J. 45, 195–202 (2007).
Laelago, T. et al. Determinants of preterm birth among mothers who gave birth in East Africa: Systematic review and meta-analysis. Ital. J. Pediatr. 46, 10 (2020).
Adu-Bonsaffoh, K., Gyamfi-Bannerman, C., Oppong, S. A. & Seffah, J. D. Determinants and outcomes of preterm births at a Tertiary Hospital in Ghana. Placenta 79, 62–67 (2019).
Wagura, P., Wasunna, A., Laving, A., Wamalwa, D. & Ng’ang’a, P. Prevalence and factors associated with preterm birth at Kenyatta National Hospital. BMC Pregnancy Childbirth 18(1), 107 (2018).
Aregawi, G. et al. Preterm births and associated factors among mothers who gave birth in Axum and Adwa Town public hospitals, Northern Ethiopia, 2018. BMC Res. Notes. 12, 1–6 (2019).
Acknowledgements
The authors acknowledge the University of Gondar for securing ethical clearance for this study. We would like to extend our gratitude to Specialized and referral Hospitals found in the northwest Amhara regional state, and data collector.
Author information
Authors and Affiliations
Contributions
E.A.F.: conceive the idea, develop a proposal, participated in designing, data collection, data management, analyses, interpretation, and manuscript a write-up. Both M.M.B. and H.Y.Y.: participated equally in developing a proposal, data management, and analyses. T.G.A., E.S.S., and A.A. participated in data management and analyses, interpretation, and manuscript write-up. All authors read and approved the final manuscript, agreed to submit it to the current journal, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fentie, E.A., Yeshita, H.Y., Shewarega, E.S. et al. Adverse birth outcome and associated factors among mothers with HIV who gave birth in northwest Amhara region referral hospitals, northwest Ethiopia, 2020. Sci Rep 12, 22514 (2022). https://doi.org/10.1038/s41598-022-27073-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-27073-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.