Abstract
The psychiatric classification of “normal” versus disordered sexual behavior has been a subject of some dispute. Although atypical sexual interests have been viewed traditionally as typically male, epidemiological data indicate its presence in both genders. We examined how gender and sexual orientation influence whether or not atypical sexual behavior is classified as a mental disorder. Mental health professionals (N = 546) were presented with five case vignettes where subjects exhibit paraphilic behaviors; one case with psychotic symptoms served as the control condition. For each vignette we randomly changed the described subject’s gender (male/female), sexual orientation (homosexual/heterosexual), and presented diagnostic criteria (fulfilled/ambiguous). Female subjects were significantly less pathologized and overall less stigmatized in terms of exhibitionistic, frotteuristic, sexual sadistic and pedophilic behavior. On the other hand, female sexual behavior that fulfilled diagnostic criteria for masochistic disorder was more pathologized. Our results demonstrate that nosologically irrelevant factors, which may be related to different sexual norms for men and women, affect clinicians’ decisions regarding atypical sexuality.
Similar content being viewed by others
Introduction
Historically, the distinction between “normal” and atypical sexual behaviors has undergone profound changes, because it is based on a socially-constructed sexual morality that is ever changing1. Since Krafft-Ebing’s Psychopathia sexualis2 in 1886, it has increasingly become the task of psychiatry to define pathological forms of sexual behavior. Since that time, historical changes in social norms have found their expression in new terminologies and diagnostic criteria for sexual behaviors across time3,4. Sexual practices such as masturbation were once considered as diseases5,6 and, up until 1973, the Diagnostic Manual of Mental Disorders (DSM)-II pathologized homosexuality as a sexual deviation7. Psychiatric nosology has also shaped such female sexual pathologies as frigidity, hysteria and nymphomania8,9. Additionally, the influence of psychiatric diagnoses on criminal law highlights its impact on society10.
Current research indicates that atypical sexual fantasies are much more common in the general population than the terms “deviant” or “atypical” might suggest11,12,13,14,15,16. Importantly, most people with atypical sexual fantasies or behaviors do not fulfill the criteria for a mental disorder17. Recently, this has been underlined by the latest update of the DSM. The DSM-5 makes a distinction between atypical sexual behaviors - paraphilias - and paraphilic disorders. Only if a paraphilia causes distress or harm to oneself or to others, such as acting a behavior upon a person without consent, can a paraphilic disorder be diagnosed. Thus, atypical sexual behaviors are not ipso facto mental disorders. With a different terminology, this has also been true for the fourth edition of the DSM18.
Even though the DSM-5 update was applauded by some researchers and clinicians, others have criticized the concept of paraphilias and paraphilic disorders in general. Most predominantly discussed are the vague and problematic boundaries between normal and pathological behaviors, the lack of scientific evidence for this distinction, and the possible legal consequences in criminal trials19,20,21,22. Lately, some researchers have therefore argued for the deletion of paraphilias from the DSM, especially those behaviors that are performed solitarily or consensually19. Most authors nowadays agree with the removal of legal and consenting paraphilias, as proposed for the forthcoming eleventh revision of the International Classification of Diseases and Related Health Problems (ICD-11)23. In line, paraphilias were among the most frequently-recommended diagnoses for removal from mental disorders classification by mental health professionals (MHP)24 and some Scandinavian countries have already removed certain paraphilias from their national psychiatric manuals25. In contrast, in other countries, practitioners are still in danger of prosecution26 and recently a U.S. Court decided that engaging in consensual BDSM sexual activity is not a constitutional right27.
In general, men seem to be more likely to report greater interest in paraphilic interests and behaviors than women17, even if recent evidence challenges this assumption11,12. However, paraphilias are perceived as typical male mental disorders, and are highly stigmatizing compared to other mental disorders28. Various editions of the DSM and ICD illustrate that “…kinky behaviors are perceived as an attribute or tendency of men”4. The DSM-IV concluded that paraphilias “…are almost never diagnosed in females”. The question as to whether this conclusion is an expression of a male construction of paraphilias, or simply represents the clinical reality, remains yet unclear. Male gender is, however, not a diagnostic criterion for paraphilic disorders, and although the prevalence for paraphilic disorders seems to be higher in men, robust epidemiological data is sparse17,29.
The diagnostic criteria for paraphilias in DSM and ICD are nowadays designed for use as an objective tool to differentiate between non-disordered and mentally-disordered sexuality. Such criteria are intended to help reduce the influence of a psychiatrist’s cultural attitudes and her or his own socialization when making a diagnosis. Consequently, the same behaviors in different people should be diagnosed comparably. Non-decisive factors such as the gender or sexual orientation of the patient should not affect the likelihood of diagnosing a mental disorder, especially because biased clinical decisions might have harmful consequences associated with negative healthcare outcomes30.
The aim of our present study was to investigate for the first time how gender and sexual orientation affect the diagnosis and stigmatization of atypical sexual behaviors among MHP. To account for the multifaceted nature of stigma31, different stigma dimensions (desire for social distance, blame, and perceived dangerousness) were assessed. Based on empirical evidence suggesting that atypical sexual behaviors are predominantly perceived as masculine, we hypothesized that men and women with atypical sexuality would be evaluated differently.
Results
We provided mental health professionals (N = 546, Table 1) with case vignettes of different paraphilic behaviors and a control vignette, and randomly changed the gender and sexual orientation of the described subject. We also randomly changed the severity of the described symptoms to include a condition that should affect the evaluation based on the diagnostic criteria. Thus, MHP were randomly assigned to one cell of a 2 “gender” (male/female) × 2 “sexual orientation” (homosexual/heterosexual) × 2 “diagnostic criteria” (fulfilled/ambiguous) factorial design. They were asked to evaluate the cases, and to estimate whether or not a mental disorder is present, indicate its biological or psychological underpinnings, and provide various measures of stigma. Sixty-four % women and 35% men participated in the present study. Most participants were psychologists (59%) or psychiatrists (36%) who had, on average, 11 years of clinical experience (further details see Table 1).
The first vignette described an individual with psychotic symptoms followed by five vignettes describing subjects with paraphilic sexual interests or behaviors (exhibitionistic, frotteuristic, sexual sadistic, pedophilic, sexual masochistic) (for detailed descriptions of the vignettes see Supplementary File 1).
Estimation of psychopathology was lower (p < 0.001) in all of the paraphilic vignettes compared to the psychosis vignette (Fig. 1) with regard to the question as to whether or not the subject is mentally disordered (F5,3222 = 162.95, p < 0.001) and fulfills the criteria for a mental disorder (F5,3182 = 93.21, p < 0.001). On average, the mean scores of all the vignettes were >3.5 (on a rating between strongly disagree “1” and strongly agree “6”) and thus leaning toward the pathological end of the scale. The pedophilic vignette was significantly more pathologized compared to the other paraphilic vignettes (p < 0.001). When participants had to indicate “the cause” of the symptoms, it was also found that a significant difference existed between vignettes (F5,3270 = 61.91, p < 0.001). While psychotic symptoms were comparably attributed to both biological and psychological factors (49.5% vs. 50.5%), the paraphilic vignettes were significantly more often ascribed to psychological factors (~70%, p < 0.001). The pedophilic vignette (62 ± 1% psychological factors) was again somewhat between the psychotic vignette and the other paraphilias. Pedophilia was thus estimated of being remarkably more “biological” and “mentally disordered” than the other paraphilias (p < 0.001), especially in terms of the full criteria condition (Suppl. Figure 1). Overall, the behaviors presented also differed in the degree to which they were stigmatized (F5,3183 = 202.09, p < 0.001). A Bonferroni post-hoc analysis indicated that the overall stigmatization scores were lowest in the psychosis condition, followed by masochism, exhibitionism, and frotteurism, and highest in the pedophilia and sexual sadism condition (Fig. 1C).
Mental health professionals responded differently to the six vignettes. While psychotic behavior were rated highest regarding psychopathology (A) they were also the least stigmatized (C) and the presumed psychological component was lowest (B). Pedophilic behavior were rated to be significantly more biologically-based and mentally-disordered compared to all other paraphilic behavior. Pedophilic and sexual sadistic behavior had the highest stigma index. Sexual masochism was significantly less stigmatized compared to all other paraphilias. ***Indicates a significant difference in post-hoc analysis compared to all other vignettes.
Both questions addressing how participants evaluate the mental health of the subject correlated highly (Fig. 1; for example, R = 0.77, p < 0.001 for the psychosis vignette and R = 0.81, p < 0.001 for the exhibitionism vignette). We calculated a “psychopathology factor” as the mean of both values for further analysis in order to include both a subjective and an objective estimation of mental disorder. This psychopathology factor was included in a 2 × 2 × 2 ANOVA. In this 3-factorial ANOVA, the ambiguous condition was estimated as less pathological in all of the vignettes (psychosis: F1,513 = 9.78, p = 0.002, exhibitionism: F1,510 = 56.14, p < 0.001, frotteurism: F1,516 = 20.85, p < 0.001, sexual sadism: F1,513 = 14.79, p < 0.001, pedophilia: F1,538 = 105.53, p < 0.001, and sexual masochism: F1,519 = 8.85, p = 0.003). Thus, we confirmed that the manipulation of the vignettes affected the participants’ estimation of psychopathology.
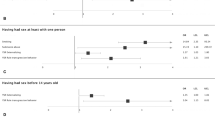
Interestingly, MHP also gave lower psychopathology factors to female subjects in most of the paraphilic vignettes (exhibitionism: F1,510 = 35.95, p < 0.001, frotteurism: F1,516 = 7.34, p = 0.007, sexual sadism: F1,513 = 17.46, p < 0.001, and pedophilia: F1,523 = 26.50, p < 0.001, Fig. 2A). In contrast, with regard to the control and sexual masochism vignettes, gender did not influence the participants’ estimation of psychopathology (psychosis: F1,513 = 0.01, p = 0.917, sexual masochism: F1,519 = 0.02, p = 0.964). The percentage of MHP who rated the symptoms described as a mental disorder (psychopathology factor >3.5) also differed profoundly from vignette to vignette (Fig. 2B). Almost 100% of the participants judged the psychotic symptoms as indicating a mental disorder, independent of gender or criteria (χ²(3) = 3.43, p = 0.329, Fig. 2B). In contrast, in the exhibitionistic (χ²(3) = 62.20, p < 0.001), frotteuristic (χ²(3) = 34.14, p < 0.001), sexual sadistic (χ²(3) = 21.03, p < 0.001) and pedophilic (χ²(3) = 47.12, p < 0.001) vignettes, female subjects were less likely to be diagnosed as mentally disordered. This gender bias was particularly pronounced in the ambiguous condition (Fig. 2B). For example, while 65% of MHP pathologized an exhibitionistic man, only 36% pathologized the female subject in the ambiguous condition. Interestingly, we also found a gender effect for the sexual masochism vignette (χ²(3) = 10.23, p < 0.017). In the ambiguous condition, females were less likely to be pathologized. In contrast, when full diagnostic criteria were present, the percentage of MHP who diagnosed a mental disorder was almost 10% higher in the female condition.
Female subjects were less pathologized in the exhibitionistic, frotteuristic, sexual sadistic and pedophilic vignette (A). In line with this, the percentage of mental health professionals who rated the symptoms as a mental disorder (=psychopathology factor >3.5) was lower in the female condition in these vignettes (B). In contrast, the psychopathology factor was comparable between males and females in the masochistic vignette (A). Interestingly, while females were also less pathologized in the ambiguous condition with the number of females who received a mental disorder diagnosis increased in the full criteria condition (B). Neither the psychopathology factor, nor the percentage of mental health professionals that gave a diagnosis was affected by gender in the psychosis control condition. *,**,***Indicate a significant difference in post-hoc analysis compared to all other vignettes with p < 0.05, 0.01, 0.001, respectively.
In terms of different stigma dimensions, a gender difference occurred for all paraphilias – with the exception of masochism – on the dimensions desire for social distance and perceived dangerousness. Male subjects were perceived as being more dangerous and provoked more desire for social distance compared to female subjects. In addition, MHP blamed male subjects more than female subjects for frotteuristic behaviors (see Table 2).
Roughly 20–25% of all participants provided explanations concerning their diagnoses in the open-ended text boxes. These qualitative data were rated by two independent raters and sorted into different coding categories (displayed in Supplemental Table 1). In line with the quantitative results, under ambiguous conditions, MHP listed on average less pro and more contra arguments compared to the full criteria condition (Fig. 3A). In the female compared to the male condition, the percentage of MHP who listed at least one pro argument was lower in the exhibitionism, frotteurism, sexual sadism and pedophilia vignettes. This was more pronounced under ambiguous conditions (Fig. 3A). In contrast, in terms of sexual masochism in the full criteria condition, the percentage who listed at least one pro argument was 25% higher in the female condition (χ²(3) = 8.99, p = 0.029, Fig. 3B). Intriguingly, personality disorders were only listed as a reason for pathologizing atypical sexual behavior in the female/full criteria condition by 21% of the participants (χ²(3) = 17.98, p < 0.001, Fig. 3B). Moreover, less contra arguments (21%) were to be found in the female/full criteria condition, in contrast to 45–58% in the other three conditions (χ²(3) = 7.19, p = 0.066, Fig. 3B).
Percentage of mental health professionals listing at least one pro argument for a mental disorder in their opinions in the open text box (A). Especially in the ambiguous condition, the percentage of mental health professionals in the female condition was lower. Again, sexual masochism was differently evaluated in the ambiguous and full criteria condition (B). The percentage of mental health professionals listing at least one pro argument was increased in the full criteria condition and reduced in the ambiguous condition. Moreover, more than 20% of mental health professionals diagnosed a personality disorder for the female subject in the full criteria condition. *,***Indicate a significant difference in post-hoc analysis compared to all other vignettes with p < 0.05, 0.001, respectively. #Indicates a difference on trend level p < 0.1.
In all cases, the sexual orientation of the subject did not affect the psychopathology factor in the present study. Moreover, the gender of the participating MHP had no effect on the results – pathologization of male paraphilic behaviors was more pronounced in both male and female MHP. Additionally, mental health professionals tended to pathologize male paraphilic behaviors to a higher extent, independently of their therapeutic background. Only for the sadism vignette did we find an effect of the therapeutic background (F2,391 = 5.32, p = 0.005). MHP trained in psychoanalysis pathologized subjects expressing sexual sadistic behaviors to a greater extent than MHP trained in cognitive-behavioral therapy (p = 0.01).
Discussion
The present study demonstrates for the first time how a person’s gender can influence their likelihood of being pathologized with a paraphilic disorder. One possible reason may be that MHP tend to ignore or downplay paraphilic interests in women. Indeed, paraphilias seem to be particularly perceived (and possibly overestimated) as masculine mental disorders28. In contrast, seen from a historical perspective, women’s sexuality was more socially sanctioned than male sexuality, and indeed women’s sexual desire was once deemed as socially disruptive8,32. Before Krafft-Ebing’s Psychopathia sexualis, sexual deviancy was even considered a sign of feminization in men33. Our data indicate different contemporary sexual norms for women and men, which impact the evaluation of atypical sexual behavior within the mental health system. Future research should address to what extent this result is associated with sociocultural norms, and the social construction of female sexuality as being passive and submissive, and male sexuality as being dominant and aggressive34. However, the result that female subjects were more likely to be pathologized in the full criteria masochism condition points to activated gender stereotypes in the clinical decision process. To date, masochism seems to be the most common paraphilic interest among women11,35,36,37, which may have also affected the views of MHP. Of note is the fact that sexual masochism was also the only paraphilic behavior in the present study that did not involve a possibly non-consenting person, as is the case in exhibitionism, frotteurism, sexual sadism and pedophilia. Thus, even if paraphilias are considered to be typically male mental disorders, and male mental disorders seem to be characterized by externalizing symptoms, sexual masochism can be seen as the paraphilia with the most internalizing symptoms28. Interestingly, sexual sadism was the only paraphilia that was more pathologized by MHP with a psychoanalytic background compared to MHP with a cognitive-behavioral background. This is worth noting, as it may indicate that psychoanalytic MHP still assume more (presumably unconsciously) pathology in people with sadistic sexual behavior.
Paraphilias (particularly in women), apart from in forensic settings, have been neglected in terms of research. To date, neither has research on the actual prevalence rates been conducted, nor has the utility of the diagnostic criteria of paraphilic disorders been tested in DSM field trials29. This is striking, given the legal and social consequences of paraphilic disorders. Indeed, the few existing studies indicate that atypical interests and behaviors are common in both genders and challenge “…the idea that women’s sexual interests are necessarily centered on normophilic behaviors”11,14,38.
Overall, paraphilias were more stigmatized and less pathologized compared to the psychosis vignette. This result is not surprising because paraphilias are among the most stigmatized mental disorders39. Interestingly, the order of overall stigmatization in the present study can be understood as an expression of the forensic psychiatric relevance of disorders. Behaviors involving no bodily contact (hands-off behavior) seem to be less stigmatized then such potential hands-on behaviors as sadism or pedophilia. This was particularly true for the stigma-dimension “blame” (Table 2).
A limitation of the present study is that we did not assess all of the atypical sexual behaviors that are listed in DSM and ICD (e.g. fetishism or voyeurism). We cannot rule out that our stigma results are thus confounded by the fact that the atypical sexual behaviors surveyed either potentially include non-consenting individuals (sadism, pedophilia, exhibitionism, and frotteurism) and thus constitute crimes, or were arguably self-harming (masochism). Thus even if no stigma against atypical sexual behaviors existed, these behaviors might still be stigmatized for being crimes. Nevertheless, we were particularly interested in those behaviors that might be of legal importance, for example in criminal trials. In addition, always presenting the psychosis vignette first may have led to an order effect in the rating of subsequent disorders, an aspect which needs to be considered as a further limitation. The fact that 47% of the approached participants did not finish the study is a further methodological limitation. The present study included MHP from Germany, Austria and the German-speaking part of Switzerland, and we cannot rule out a selection bias. For example, those MHP who are less busy and are particularly interested in scientific experiments, and show more openness to sexuality, may have been more likely to complete the online questionnaire. While the present results may be representative of the Western world, given the important cultural impact on sexual norms, they cannot be generalized to other countries. In order to examine different cultural influences on the pathologization of atypical sexual behaviors, it may be fruitful in the future to compare MHP from culturally-diverse countries.
In conclusion, we have demonstrated for the first time a gender-bias in the perception and diagnosis of paraphilic disorders by male and female MHP. MHP are the most crucial group when it comes to differentiating between non-disordered and mentally disordered sexuality nowadays. Our data indicate that most atypical sexual behaviors are less pathologized in women. The underlying mechanisms and sociosexual norms leading to this bias should be addressed in future research because it has been shown that gender bias may have a serious impact on clinical and legal decisions40. Consequently, most ethical guidelines for MHP postulate a restriction of bias in clinical practice41,42. In future, it would also be interesting to explore whether or not gender influences other stigma facets, such as prognostic pessimism, which may influence therapeutic decisions.
Thus, although diagnostic criteria for paraphilic disorders exist, our study reveals that the pathologization of atypical sexual behavior still seems to be profoundly affected by nosologically irrelevant sexual norms. When confronted with atypical sexual expressions, MHP are therefore at risk of promoting gender stereotypes and sexual morality.
Methods
Recruitment procedure
MHP were recruited by means of an email invitation to complete an anonymous online survey concerning ‘diagnostic evaluation of sexual behavior’. Email invitations were sent to the chief physicians of psychiatric and psychosomatic hospitals in Germany, Austria and the German-speaking part of Switzerland. They were asked to distribute an invitation and a link to the study amongst their psychiatrists and clinical psychologists. At the beginning of the anonymous survey we fully explained the procedure, and participants had to give informed consent before starting the study. The local ethics committee (Psychotherapeutic Chamber Hamburg) approved the study protocol and all experiments were performed in accordance with relevant guidelines and regulations. In total, 971 individuals clicked on the survey link and 546 MHP (53%) completed it. The greatest number of drop-outs (81%) occurred before any question had been presented.
Study design
Participants were randomly assigned to six case vignettes. The first vignette described an individual with psychotic symptoms followed by five vignettes describing subjects with atypical sexual interests or behaviors (exhibitionistic, frotteuristic, sexual sadistic, pedophilic, and sexual masochistic) and one vignette with non-paraphilic compulsive sexual behaviour, which will be reported elsewhere) (for detailed descriptions of the vignettes see Supplementary File 1). The vignettes gave detailed information about the person’s atypical sexual arousal pattern, which was manifested by sexual thoughts, fantasies, urges or behaviors. Moreover, vignettes in the fulfilled criteria condition included information about the duration criterion (over a period of at least 6 months) and acting out of the arousal pattern with individuals unwilling or unable to consent, or associated with impairments in functioning, according to DSM-5 criteria17. In contrast, in the ambiguous condition, no information about duration and consent or impairment in functioning was given. For each vignette, MHP were randomly assigned to one cell of a 2 “gender” (male/female) × 2 “sexual orientation” (homosexual/heterosexual) × 2 “diagnostic criteria” (fulfilled/ambiguous) factorial design. Participants were instructed to read the vignettes carefully and, after each vignette, were asked to rate their subjective estimation of the person’s mental health on a 6-point scale, and to indicate whether or not the person fulfilled the diagnostic criteria of a mental disorder according to DSM or ICD (Fig. 1). Qualitative data were collected in an open-ended text box asking participants to explain their answer. In addition, we adapted items used by Boysen and colleagues28 to measure the degree of stigma directed toward persons expressing paraphilic preferences. For each vignette, participants provided a stigma rating on a six-point Likert scale (strongly disagree - strongly agree) that included the following stigma dimensions: desire for social distance (“I feel irritation towards Mr./Mrs. X.”;, “If I were a landlord, I probably would rent an apartment to Mr./Mrs. X.”); perceived dangerousness (“I would feel threatened by Mr./Mrs. X.”; “Mr./Mrs. X is dangerous.”); blame (“I think it is the fault of Mr./Mrs. X that he/she is in that condition.”; “Mr./Mrs. X should be punished.”; “Mr./Mrs. X. could control his/her behavior if she/he wanted to”). In addition, the seven stigma items were combined to form a single stigmatization index. Moreover, all participants provided an opinion if the symptom was predominantly caused by biological or psychological factors by moving a slider between biological (0) and psychological (100) etiology (“Please indicate if the fantasies/behavior of the person is “caused” by biological or psychological factors?”). Additionally, in order to control for potential confounding variables, four items measuring the MHP attitudes were assessed on a six-point Likert scale (“I am religious”, “I perceive myself as a member of a minority group.”, “Sexual behavior of men and women strongly differ.” and “I am politically…”(1 = liberal to 6 = conservative).
Statistical analyses
Statistical analyses were carried out using IBM SPSS Statistics 22.0 (IBM Corp., Armonk, NY). Data are reported as means ± S.E.M. A three-factorial analysis of variance (ANOVA), followed by Bonferroni’s post-hoc analysis, were carried out to study the effect of vignette version, gender and sexual orientation on the estimation of psychopathology and stigmatization. A chi-square test was performed to compare the percentage of MHP diagnosing a mental disorder, and for the quantification of qualitative data. Qualitative data were analyzed using content analysis43,44. They were first rated by a coder in order to determine categories. All data were subsequently coded by two independent raters, who were trained by two of the authors (VK & JF). Cohen’s kappa was calculated to compare the inter-rater reliability, and is reported in Supplemental Table 1. The kappa value can be interpreted according to Altman (1991). It was very good for 52 categories (0.81–1) and good for 47 categories (0.61–0.80). Only 4 categories had a moderate (<0.61) inter-rater reliability. Significance was evaluated at a probability of 5% or less (<0.05).
Data availability statement
We confirm that all relevant data are available from the authors.
Change history
16 April 2018
A correction to this article has been published and is linked from the HTML and PDF versions of this paper. The error has been fixed in the paper.
References
Foucault, M. & Hurley, R. The history of sexuality. Vol. 1: An introduction. (Vintage Books, 1990).
Krafft-Ebing, R. Psychopathia sexualis. (Enke, 1886).
De Block, A. & Adriaens, P. R. Pathologizing sexual deviance: A history. J. Sex Res. 50, 276–298 (2013).
Giami, A. Between DSM and ICD: Paraphilias and the transformation of sexual norms. Arch. Sex. Behav. 44, 1127–1138 (2015).
Laqueur, T. W. Making sex: body and gender from the Greeks to Freud. (Harvard University Press, 1990).
Engelhardt, H. T. The disease of masturbation: values and the concept of disease. Bull. Hist. Med. 48, 234 (1974).
Drescher, J. Out of DSM: Depathologizing homosexuality. Behav. Sci. (Basel) 5, 565–575 (2015).
Groneman, C. Nymphomania: a history. (W.W. Norton, 2001).
Eriksen, K. & Kress, V. E. Gender and diagnosis: Struggles and suggestions for counselors. J. Couns. Dev. 86, 152–162 (2008).
Lave, T. Only yesterday: The rise and fall of twentieth century sexual psychopath laws. LA. Law Rev. 69 (2009).
Joyal, C. C. & Carpentier, J. The prevalence of paraphilic interests and behaviors in the general population: A Provincial Survey. J. Sex Res. 54, 161–171 (2017).
Joyal, C. C., Cossette, A. & Lapierre, V. What exactly is an unusual sexual fantasy? J. Sex. Med. 12, 328–340 (2015).
Richters, J., De Visser, R. O., Rissel, C. E., Grulich, A. E. & Smith, A. M. A. Demographic and psychosocial features of participants in bondage and discipline, ‘sadomasochism’ or dominance and submission (BDSM): Data from a national survey. J. Sex. Med. 5, 1660–1668 (2008).
Långström, N. & Seto, M. C. Exhibitionistic and voyeuristic behavior in a swedish national population survey. Arch. Sex. Behav. 35, 427–435 (2006).
Ahlers, C. J. et al. How unusual are the contents of paraphilias? Paraphilia-associated sexual arousal patterns in a community-based sample of men. J. Sex. Med. 8, 1362–1370 (2011).
Långström, N. The DSM Diagnostic criteria for exhibitionism, voyeurism, and frotteurism. Arch. Sex. Behav. 39, 317–324 (2010).
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. (American Psychiatric Association, 2013).
Moser, C. DSM-5 and the paraphilic disorders: Conceptual issues. Arch. Sex. Behav. 45 (2016).
Moser, C. & Kleinplatz, P. J. DSM-IV-TR and the paraphilias. J. Psychol. Human Sex. 17, 91–109 (2006).
Moser, C. When is an unusual sexual interest a mental disorder? Arch. Sex. Behav. 38, 323–325 (2009).
Shindel, A. W. & Moser, C. A. Why are the paraphilias mental disorders? J. Sex. Med. 8, 927–9 (2011).
Zonana, H. Sexual disorders: new and expanded proposals for the DSM-5–do we need them? J. Am. Acad. Psychiatry Law 39, 245–9 (2011).
Reed, G. M. et al. Disorders related to sexuality and gender identity in the ICD-11: revising the ICD-10 classification based on current scientific evidence, best clinical practices, and human rights considerations. World Psychiatry 15, 205–221 (2016).
Robles, R. et al. Categories that should be removed from mental disorders classifications: Perspectives and rationales of clinicians from eight countries. J. Clin. Psychol. 71, 267–281 (2015).
Finish-National-Institute-for-Health-and-Welfare-(THL). ICD-10-tautiluokitusta päivitetään 2011 (2011).
Glyde, T. BDSM: psychotherapy’s grey area. The Lancet Psychiatry 2, 211–213 (2015).
Court for the eastern district of Virginia. Doe-v.-Rector&Visitors-of-George-Mason-Univ.le, Case No. 1:15-cv-209 (2016).
Boysen, G., Ebersole, A., Casner, R. & Coston, N. Gendered mental disorders: Masculine and feminine stereotypes about mental disorders and their relation to stigma. J. Soc. Psychol. 154, 546–565 (2014).
Beech, A. R., Miner, M. H. & Thornton, D. Paraphilias in the DSM-5. Annu. Rev. Clin. Psychol. 12, 383–406 (2016).
Boysen, G. A. A review of experimental studies of explicit and implicit bias among counselors. J. Multicult. Couns. Devel. 37, 240–249 (2009).
Haslam, N. & Kvaale, E. P. Biogenetic explanations of mental disorder. Curr. Dir. Psychol. Sci. 24, 399–404 (2015).
Tolman, D. L., & Diamond, L. M. Desegregating sexuality research: Cultural and biological perspectives on gender and desire. Annu. Rev. Sex Res. 12, 33–74
Peter Cryle, P. & Lisa Downing, L. Feminine sexual pathologies. J. Hist. Sex. 18, 1–7 (2008).
Sanchez, D. T., Fetterolf, J. C. & Rudman, L. A. Eroticizing inequality in the united states: The consequences and determinants of traditional gender role adherence in intimate relationships. J. Sex Res. 49, 168–183 (2012).
Breslow, N., Evans, L. & Langley, J. On the prevalence and roles of females in the sadomasochistic subculture: Report of an empirical study. Arch. Sex. Behav. 14, 303–317 (1985).
Levitt, E. E., Moser, C. & Jamison, K. V. The prevalence and some attributes of females in the sadomasochistic subculture: a second report. Arch. Sex. Behav. 23, 465–73 (1994).
Wilson, G. D. & Lang, R. J. Sex differences in sexual fantasy patterns. Pers. Individ. Dif. 2, 343–346 (1981).
Seto, M. C. Pedophilia: Psychopathology and theory. In Sexual deviance: Theory, assessment, and treatment (ed. O’Donohue, D. R. L. & W. T.) 164–182 (Guilford Press, 2008).
Feldman, D. B. & Crandall, C. S. Dimensions of mental illness stigma: what about mental illness causes social rejection? J. Soc. Clin. Psychol. 26, 137–154 (2007).
Ruiz, M. T. & Verbrugge, L. M. A two way view of gender bias in medicine. J. Epidemiol. Community Health 51, 106–9 (1997).
American Psychiatric Association. The principles of medical ethics: with annotations especially applicable to psychiatry. (American Psychiatric Association, 2001).
American Psychological Association. Ethical principles of psychologists and code of conduct. Am. Psychol. 57, 1060–1073 (2002).
Fuss, J., Dressing, H. & Briken, P. Neurogenetic evidence in the courtroom: a randomised controlled trial with German judges. J Med Genet 52, 730–737 (2015).
Mayring, P. Qualitative Inhaltsanalyse in Handbuch qualitative Forschung in der Psychologie. (Springer, 2010).
Acknowledgements
The authors have no conflict of interest to declare. We are grateful to Dr. K.M. Reininger for critical comments on the study design, A. Masemann and F. Loss for coding qualitative data and Dr. P. Vermehren for translating the vignettes. Finally, we thank the participating mental health professionals for their time.
Author information
Authors and Affiliations
Contributions
J.F. and V.K. designed the experiment with input from P.B., J.F. and V.K. collected data and wrote the manuscript. P.B. revised the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fuss, J., Briken, P. & Klein, V. Gender bias in clinicians’ pathologization of atypical sexuality: a randomized controlled trial with mental health professionals. Sci Rep 8, 3715 (2018). https://doi.org/10.1038/s41598-018-22108-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-22108-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.