Abstract
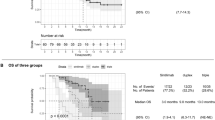
Hepatocellular carcinoma (HCC), particularly when accompanied by microvascular invasion (MVI), has a markedly high risk of recurrence after liver resection. Adjuvant immunotherapy is considered a promising avenue. This multicenter, open-label, randomized, controlled, phase 2 trial was conducted at six hospitals in China to assess the efficacy and safety of adjuvant sintilimab, a programmed cell death protein 1 inhibitor, in these patients. Eligible patients with HCC with MVI were randomized (1:1) into the sintilimab or active surveillance group. The sintilimab group received intravenous injections every 3 weeks for a total of eight cycles. The primary endpoint was recurrence-free survival (RFS) in the intention-to-treat population. Key secondary endpoints included overall survival (OS) and safety. From September 1, 2020, to April 23, 2022, a total of 198 eligible patients were randomly allocated to receive adjuvant sintilimab (n = 99) or undergo active surveillance (n = 99). After a median follow-up of 23.3 months, the trial met the prespecified endpoints. Sintilimab significantly prolonged RFS compared to active surveillance (median RFS, 27.7 versus 15.5 months; hazard ratio 0.534, 95% confidence interval 0.360–0.792; P = 0.002). Further follow-up is needed to confirm the difference in OS. In the sintilimab group, 12.4% of patients experienced grade 3 or 4 treatment-related adverse events, the most common of which were elevated alanine aminotransferase levels (5.2%) and anemia (4.1%). These findings support the potential of immune checkpoint inhibitors as effective adjuvant therapy for these high-risk patients. Chinese Clinical Trial Registry identifier: ChiCTR2000037655.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The study protocol is available in the Supplementary Information. The datasets of the clinical trial may be requested 12 months after the publication of this article. Researchers who wish to request access to raw and analyzed data should send an email to the corresponding authors (S.-Q.C. and Y.-F.L.), with a clear indication of the research purpose. Requests will be reviewed by the institutional review board, considering the risk of patient reidentification, and a response can be expected within 14 days. Individual deidentified data of the participants are available for approved eligible applications and investigators after signing a data access agreement. Source data are provided with this paper.
Code availability
R software was used for data analysis (‘survminer’ package, ‘tableone’ package, http://www.r-project.org/).
References
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
European Association for the Study of the Liver. EASL Clinical Practice Guidelines: management of hepatocellular carcinoma. J. Hepatol. 69, 182–236 (2018).
Singal, A. G. et al. AASLD Practice Guidance on prevention, diagnosis, and treatment of hepatocellular carcinoma. Hepatology 78, 1922–1965 (2023).
Lim, K.-C. et al. Systematic review of outcomes of liver resection for early hepatocellular carcinoma within the Milan criteria. Br. J. Surg. 99, 1622–1629 (2012).
Zhang, X., Li, J., Shen, F. & Lau, W. Y. Significance of presence of microvascular invasion in specimens obtained after surgical treatment of hepatocellular carcinoma. J. Gastroenterol. Hepatol. 33, 347–354 (2018).
Xiang, Y.-J. et al. Prognostic value of microvascular invasion in eight existing staging systems for hepatocellular carcinoma: a bi-centeric retrospective cohort study. Front. Oncol. 11, 726569 (2021).
Chamseddine, S., LaPelusa, M. & Kaseb, A. O. Systemic neoadjuvant and adjuvant therapies in the management of hepatocellular carcinoma—a narrative review. Cancers (Basel) 15, 3508 (2023).
Nevola, R. et al. Neoadjuvant and adjuvant systemic therapies in loco-regional treatments for hepatocellular carcinoma: are we at the dawn of a new era? Cancers (Basel) 15, 2950 (2023).
Cheng, A.-L. et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 10, 25–34 (2009).
Zhang, X.-P. et al. Postoperative adjuvant sorafenib improves survival outcomes in hepatocellular carcinoma patients with microvascular invasion after R0 liver resection: a propensity score matching analysis. HPB (Oxford) 21, 1687–1696 (2019).
Huang, Y. et al. Should we apply sorafenib in hepatocellular carcinoma patients with microvascular invasion after curative hepatectomy? OncoTargets Ther. 12, 541–548 (2019).
Wang, D. et al. Retrospective analysis of sorafenib efficacy and safety in Chinese patients with high recurrence rate of post-hepatic carcinectomy. OncoTargets Ther. 12, 5779–5791 (2019).
Bruix, J. et al. Adjuvant sorafenib for hepatocellular carcinoma after resection or ablation (STORM): a phase 3, randomised, double-blind, placebo-controlled trial. Lancet Oncol. 16, 1344–1354 (2015).
Pinyol, R. et al. Molecular predictors of prevention of recurrence in HCC with sorafenib as adjuvant treatment and prognostic factors in the phase 3 STORM trial. Gut 68, 1065–1075 (2019).
Zhang, W. Sorafenib in adjuvant setting: call for precise and personalized therapy. Transl. Gastroenterol. Hepatol. 1, 13 (2016).
Dikilitas, M. Why adjuvant and neoadjuvant therapy failed in HCC. Can the new immunotherapy be expected to be better? J. Gastrointest. Cancer 51, 1193–1196 (2020).
Pinato, D. J., Fessas, P., Sapisochin, G. & Marron, T. U. Perspectives on the neoadjuvant use of immunotherapy in hepatocellular carcinoma. Hepatology 74, 483–490 (2021).
Chow, P. et al. Abstract CT003: IMbrave050: phase 3 study of adjuvant atezolizumab + bevacizumab versus active surveillance in patients with hepatocellular carcinoma (HCC) at high risk of disease recurrence following resection or ablation. Cancer Res. 83, CT003 (2023).
Gao, S. et al. Neoadjuvant PD-1 inhibitor (sintilimab) in NSCLC. J. Thorac. Oncol. 15, 816–826 (2020).
Pinter, M., Scheiner, B. & Pinato, D. J. Immune checkpoint inhibitors in hepatocellular carcinoma: emerging challenges in clinical practice. Lancet Gastroenterol. Hepatol. 8, 760–770 (2023).
Yu, S. J. Immunotherapy for hepatocellular carcinoma: recent advances and future targets. Pharmacol. Ther. 244, 108387 (2023).
Ren, Z. et al. Sintilimab plus a bevacizumab biosimilar (IBI305) versus sorafenib in unresectable hepatocellular carcinoma (ORIENT-32): a randomised, open-label, phase 2–3 study. Lancet Oncol. 22, 977–990 (2021).
Finn, R. S. et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N. Engl. J. Med. 382, 1894–1905 (2020).
Qin, S. et al. Camrelizumab plus rivoceranib versus sorafenib as first-line therapy for unresectable hepatocellular carcinoma (CARES-310): a randomised, open-label, international phase 3 study. Lancet 402, 1133–1146 (2023).
Yau, T. et al. Efficacy and safety of nivolumab plus ipilimumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib: the CheckMate 040 randomized clinical trial. JAMA Oncol. 6, e204564 (2020).
Yau, T. et al. Nivolumab versus sorafenib in advanced hepatocellular carcinoma (CheckMate 459): a randomised, multicentre, open-label, phase 3 trial. Lancet Oncol. 23, 77–90 (2022).
Kudo, M. et al. Final results of adjuvant nivolumab for hepatocellular carcinoma (HCC) after surgical resection (SR) or radiofrequency ablation (RFA) (NIVOLVE): a phase 2 prospective multicenter single-arm trial and exploratory biomarker analysis. J. Clin. Oncol. 40, 416 (2022).
Finn, R. S. et al. Pembrolizumab as second-line therapy in patients with advanced hepatocellular carcinoma in KEYNOTE-240: a randomized, double-blind, phase III trial. J. Clin. Oncol. 38, 193–202 (2020).
He, H. et al. Multi-dimensional single-cell characterization revealed suppressive immune microenvironment in AFP-positive hepatocellular carcinoma. Cell Discov. 9, 60 (2023).
Chen, W. et al. Adjuvant anti-PD-1 antibody for hepatocellular carcinoma with high recurrence risks after hepatectomy. Hepatol. Int. 17, 406–416 (2023).
Li, J. et al. Postoperative adjuvant tyrosine kinase inhibitors combined with anti-PD-1 antibodies improves surgical outcomes for hepatocellular carcinoma with high-risk recurrent factors. Front. Immunol. 14, 1202039 (2023).
Li, L. et al. Adjuvant immune checkpoint inhibitors associated with higher recurrence-free survival in postoperative hepatocellular carcinoma (PREVENT): a prospective, multicentric cohort study. J. Gastroenterol. 58, 1043–1054 (2023).
Qin, S. et al. Atezolizumab plus bevacizumab versus active surveillance in patients with resected or ablated high-risk hepatocellular carcinoma (IMbrave050): a randomised, open-label, multicentre, phase 3 trial. Lancet 402, 1835–1847 (2023).
Hack, S. P. et al. IMbrave 050: a phase III trial of atezolizumab plus bevacizumab in high-risk hepatocellular carcinoma after curative resection or ablation. Future Oncol. 16, 975–989 (2020).
Galle, P. R. et al. Patient-reported outcomes with atezolizumab plus bevacizumab versus sorafenib in patients with unresectable hepatocellular carcinoma (IMbrave150): an open-label, randomised, phase 3 trial. Lancet Oncol. 22, 991–1001 (2021).
Zhao, M., Huang, H., He, F. & Fu, X. Current insights into the hepatic microenvironment and advances in immunotherapy for hepatocellular carcinoma. Front. Immunol. 14, 1188277 (2023).
Waterhouse, D. M. et al. Continuous versus 1-year fixed-duration nivolumab in previously treated advanced non-small-cell lung cancer: CheckMate 153. J. Clin. Oncol. 38, 3863–3873 (2020).
Zalcman, G. et al. 972O nivolumab (Nivo) plus ipilimumab (Ipi) 6-months treatment versus continuation in patients with advanced non-small cell lung cancer (aNSCLC): results of the randomized IFCT-1701 phase III trial. Ann. Oncol. 33, S992 (2022).
Su, D., Wu, B. & Shi, L. Cost-effectiveness of atezolizumab plus bevacizumab vs sorafenib as first-line treatment of unresectable hepatocellular carcinoma. JAMA Netw. Open 4, e210037 (2021).
Zhang, X. et al. Cost-effectiveness of atezolizumab plus bevacizumab vs sorafenib for patients with unresectable or metastatic hepatocellular carcinoma. JAMA Netw. Open 4, e214846 (2021).
McDonnell, P. J. & Jacobs, M. R. Hospital admissions resulting from preventable adverse drug reactions. Ann. Pharmacother. 36, 1331–1336 (2002).
Hess, L. M. et al. Factors associated with adherence to and treatment duration of erlotinib among patients with non-small cell lung cancer. J. Manag. Care Spec. Pharm. 23, 643–652 (2017).
Kelley, R. K. Adjuvant sorafenib for liver cancer: wrong stage, wrong dose. Lancet Oncol. 16, 1279–1281 (2015).
Cong, W.-M. et al. Practice guidelines for the pathological diagnosis of primary liver cancer: 2015 update. World J. Gastroenterol. 22, 9279–9287 (2016).
Edmondson, H. A. & Steiner, P. E. Primary carcinoma of the liver: a study of 100 cases among 48,900 necropsies. Cancer 7, 462–503 (1954).
Zhang, X. P. et al. An Eastern Hepatobiliary Surgery Hospital microvascular invasion scoring system in predicting prognosis of patients with hepatocellular carcinoma and microvascular invasion after R0 liver resection: a large-scale, multicenter study. Oncologist 24, e1476–e1488 (2019).
Sun, J. J. et al. Postoperative adjuvant transcatheter arterial chemoembolization after R0 hepatectomy improves outcomes of patients who have hepatocellular carcinoma with microvascular invasion. Ann. Surg. Oncol. 23, 1344–1351 (2016).
Shi, M. et al. Partial hepatectomy with wide versus narrow resection margin for solitary hepatocellular carcinoma: a prospective randomized trial. Ann. Surg. 245, 36–43 (2007).
Zhang, Y.-F. et al. Intermediate-stage hepatocellular carcinoma treated with hepatic resection: the NSP score as an aid to decision-making. Br. J. Cancer 115, 1039–1047 (2016).
Marrero, J. A. et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Hepatology 68, 723–750 (2018).
Eisenhauer, E. A. et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur. J. Cancer 45, 228–247 (2009).
El-Khoueiry, A. B. et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet 389, 2492–2502 (2017).
Acknowledgements
This work was supported by the National Key Research and Development Program of China (2022YFC2503705 to S.-Q.C.), Shanghai Municipal Health Commission (2023ZZ02005 to S.-Q.C.) and the National Natural Science Foundation of China (82072618 to S.-Q.C.). The funders had no role in the study design, data collection, data analysis, data interpretation or writing of the report.
Author information
Authors and Affiliations
Contributions
S.-Q.C., Y.-F.L. and K.W. were responsible for study conception and design, project supervision, quality assessment, review, and approval of the article. Y.-J.X., H.-M.Y., Y.-Q.C. and Z.-H.L. contributed to the design of the clinical trial, writing of the protocol, recruitment and treatment of the patients, management of the trial and data, analysis and interpretation of data, and writing and final approval of the paper. J.S., W.-X.G., C.-D.L., Y.-X.Z., F.-G.Z. and J.-J.L. accessed and verified the data. M.-L.Y., H.-K.Z., C.L., F.Z. and W.-J.W. were involved in the design of the clinical trial, recruitment and treatment of the patients, management of the trial and data, and review of the paper. W.Y.L. accessed and verified the data and reviewed the paper. Y.-Y.Q. was responsible for statistical analysis and interpretation and the data review. All authors read and approved the final draft of the paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Fei Liang, David Pinato and Arndt Vogel for their contribution to the peer review of this work. Primary Handling Editor: Ulrike Harjes, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Adjusted Kaplan-Meier curves of RFS for patients in the sintilimab and active surveillance groups.
HR, two-sided 95%CI and P value were estimated using the Cox proportional hazards method. Cox proportional hazards regression model adjustment for cirrhosis and microvascular invasion stage. Abbreviations: RFS, recurrence-free survival; HR, hazard ratio; CI, confidence interval.
Extended Data Fig. 2 HRs (center square) with 95% CIs (error bars) for OS in different patient subgroups.
HRs with two-sided 95%CIs were calculated using the Cox proportional hazards method. Abbreviations: RFS, recurrence-free survival; HR, hazard ratio; CI, confidence interval; AFP, alpha-fetoprotein; DCP, des gamma-carboxy prothrombin.
Supplementary information
Supplementary Information
Supplementary Table 1, protocol and CONSORT 2010 checklist.
Source data
Source Data Fig. 2
Statistical source data.
Source Data Fig. 3
Statistical source data.
Source Data Extended Data Fig. 1
Statistical source data.
Source Data Extended Data Fig. 2
Statistical source data.
Source Data Extended Data Table 3
Statistical source data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, K., Xiang, YJ., Yu, HM. et al. Adjuvant sintilimab in resected high-risk hepatocellular carcinoma: a randomized, controlled, phase 2 trial. Nat Med 30, 708–715 (2024). https://doi.org/10.1038/s41591-023-02786-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-023-02786-7
This article is cited by
-
Adjuvant sintilimab effective in high-risk HCC
Nature Reviews Clinical Oncology (2024)
-
Sintilimab as adjuvant therapy for patients with resected HCC at high risk of recurrence
Nature Reviews Gastroenterology & Hepatology (2024)
-
Immunotherapy at all stages of hepatocellular carcinoma
Nature Medicine (2024)