Abstract
Pre-exposure prophylaxis (PrEP) with tenofovir (TFV) disoproxil fumarate and emtricitabine administered orally daily is effective in preventing human immunodeficiency virus (HIV) acquisition in both men and women with sufficient adherence; however, the adherence–efficacy relationship in cisgender women has not been well established. We calculated the adherence–efficacy curve for cisgender women by using HIV incidence and plasma TFV concentration data from three trials (FEM-PrEP, VOICE and Partners PrEP). We imputed TFV diphosphate (TFV-DP) concentrations, a measure of long-term adherence, from TFV quantification by using data from the HIV Prevention Trials Network 082 study, which measured both TFV-DP and TFV concentrations. Two, four and seven pills per week reduced HIV incidence by 59.3% (95% credible interval (CrI) 29.9–95.8%), 83.8% (95% CI 51.7–99.8%) and 95.9% (95% CI 72.6–100%), respectively. Our adherence–efficacy curve can be validated and updated by HIV prevention studies that directly measure TFV-DP concentrations. The curve suggests that high adherence confers high protection in cisgender women. However, the lower efficacy with partial adherence highlights the need for new PrEP products and interventions to increase adherence.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data used in this study are available on GitHub (https://github.com/FredHutch/PrEPCiswomen).
Code availability
Model and calibration code is available on GitHub (https://github.com/FredHutch/PrEPCiswomen).
References
Grant, R. M. et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N. Engl. J. Med. 363, 2587–2599 (2010).
Choopanya, K. et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet 381, 2083–2090 (2013).
Baeten, J. M. et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N. Engl. J. Med. 367, 399–410 (2012).
Thigpen, M. C. et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N. Engl. J. Med. 367, 423–434 (2012).
Van Damme, L. et al. Preexposure prophylaxis for HIV infection among African women. N. Engl. J. Med. 367, 411–422 (2012).
Marrazzo, J. M. et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. N. Engl. J. Med. 372, 509–518 (2015).
Grant, R. M. et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect. Dis. 14, 820–829 (2014).
Anderson, P. L. et al. Intracellular tenofovir-diphosphate and emtricitabine-triphosphate in dried blood spots following directly observed therapy. Antimicrob. Agents Chemother. 62, e01710–e01717 (2017).
Anderson, P. L. et al. Emtricitabine–tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci. Transl. Med. 4, 151ra125 (2012).
Delany-Moretlwe, S. et al. Cabotegravir for the prevention of HIV-1 in women: results from HPTN 084, a phase 3, randomised clinical trial. Lancet 399, 1779–1789 (2022).
Anderson, P. L., Marzinke, M. A. & Glidden, D. V. Updating the adherence–response for oral emtricitabine/tenofovir disoproxil fumarate for human immunodeficiency virus pre-exposure prophylaxis among cisgender women. Clin. Infect. Dis. 76, 1850–1853 (2023).
Donnell, D. et al. HIV protective efficacy and correlates of tenofovir blood concentrations in a clinical trial of PrEP for HIV prevention. J. Acquir. Immune Defic. Syndr. 66, 340–348 (2014).
Mitchell, K. M. et al. Modelling the impact and cost-effectiveness of combination prevention amongst HIV serodiscordant couples in Nigeria. AIDS 29, 2035–2044 (2015).
Mukandavire, Z., Mitchell, K. M. & Vickerman, P. Comparing the impact of increasing condom use or HIV pre-exposure prophylaxis (PrEP) use among female sex workers. Epidemics 14, 62–70 (2016).
Mudimu, E. et al. Individual and community-level benefits of PrEP in Western Kenya and South Africa: implications for population prioritization of PrEP provision. PLoS ONE 15, e0244761 (2020).
Kripke, K. et al. The case for prevention—primary HIV prevention in the era of universal test and treat: a mathematical modeling study. EClinicalMedicine 46, 101347 (2022).
Hoffman, R. M. et al. Benefits of PrEP as an adjunctive method of HIV prevention during attempted conception between HIV-uninfected women and HIV-infected male partners. J. Infect. Dis. 212, 1534–1543 (2015).
Mitchell, K. M. et al. Potential impact of pre-exposure prophylaxis for female sex workers and men who have sex with men in Bangalore, India: a mathematical modelling study. J. Int. AIDS Soc. 19, 20942 (2016).
Smith, J. A., Garnett, G. P. & Hallett, T. B. The potential impact of long-acting cabotegravir for HIV prevention in South Africa: a mathematical modeling study. J. Infect. Dis. 224, 1179–1186 (2021).
Phillips, A. N. et al. Cost-effectiveness of easy-access, risk-informed oral pre-exposure prophylaxis in HIV epidemics in sub-Saharan Africa: a modelling study. Lancet HIV 9, e353–e362 (2022).
Phillips, A. N. et al. Potential impact and cost-effectiveness of condomless-sex-concentrated PrEP in KwaZulu-Natal accounting for drug resistance. J. Infect. Dis. 223, 1345–1355 (2021).
Geidelberg, L. et al. Mathematical model impact analysis of a real-life pre-exposure prophylaxis and treatment-as-prevention study among female sex workers in Cotonou, Benin. J. Acquir. Immune Defic. Syndr. 86, e28–e42 (2021).
Celum, C. et al. PrEP uptake, persistence, adherence, and effect of retrospective drug level feedback on PrEP adherence among young women in Southern Africa: results from HPTN 082, a randomized controlled trial. PLoS Med. 18, e1003670 (2021).
Marrazzo, J. et al. 8+ years pooled analysis: adherence and HIV incidence in 6000 women on F/TDF for PrEP [CROI Abstract 163]. In Special Issue: Abstracts from CROI 2023 Conference on Retroviruses and Opportunistic Infections. Top. Antivir. Med. 31, 67 (2023).
Patterson, K. B. et al. Penetration of tenofovir and emtricitabine in mucosal tissues: implications for prevention of HIV-1 transmission. Sci. Transl. Med. 3, 112re4 (2011).
Hendrix, C. W. et al. Dose frequency ranging pharmacokinetic study of tenofovir–emtricitabine after directly observed dosing in healthy volunteers to establish adherence benchmarks (HPTN 066). AIDS Res. Hum. Retroviruses 32, 32–43 (2016).
Cottrell, M. L. et al. A translational pharmacology approach to predicting outcomes of preexposure prophylaxis against HIV in men and women using tenofovir disoproxil fumarate with or without emtricitabine. J. Infect. Dis. 214, 55–64 (2016).
Garrett, K. L. et al. A pharmacokinetic/pharmacodynamic model to predict effective HIV prophylaxis dosing strategies for people who inject drugs. J. Pharmacol. Exp. Ther. 367, 245–251 (2018).
On-demand PrEP. Centers for Disease Control and Prevention https://www.cdc.gov/hiv/basics/prep/on-demand-prep.html (2022).
Glidden, D. V., Stirrup, O. T. & Dunn, D. T. A Bayesian averted infection framework for PrEP trials with low numbers of HIV infections: application to the results of the DISCOVER trial. Lancet HIV 7, e791–e796 (2020).
Gao, F., Glidden, D. V., Hughes, J. P. & Donnell, D. J. Sample size calculation for active-arm trial with counterfactual incidence based on recency assay. Stat. Commun. Infect. Dis. 13, 20200009 (2021).
Zhu, Y., Gao, F., Glidden, D., Donnell, D. & Janes, H. Estimating counterfactual placebo HIV incidence in HIV prevention trials without placebo arms based on markers of HIV exposure. Preprint at medRxiv https://doi.org/10.1101/2022.05.06.22274780 (2022).
Abaasa, A. et al. Use of propensity score matching to create counterfactual group to assess potential HIV prevention interventions. Sci. Rep. 11, 7017 (2021).
Glidden, D. V. et al. Using the adherence–efficacy relationship of emtricitabine and tenofovir disoproxil fumarate to calculate background HIV incidence: a secondary analysis of a randomized, controlled trial. J. Int. AIDS Soc. 24, e25744 (2021).
Velloza, J. et al. Alignment of PrEP adherence with periods of HIV risk among adolescent girls and young women in South Africa and Zimbabwe: a secondary analysis of the HPTN 082 randomised controlled trial. Lancet HIV 9, e680–e689 (2022).
Corneli, A. et al. Episodic use of pre-exposure prophylaxis among young cisgender women in Siaya County, Kenya. AIDS Patient Care STDS 36, 379–388 (2022).
Celum, C. & Baeten, J. PrEP for HIV prevention: evidence, global scale-up, and emerging options. Cell Host Microbe 27, 502–506 (2020).
Acknowledgements
We are grateful to H. Angier, a scientific writer at the Vaccine and Infectious Disease Division of the Fred Hutchinson Cancer Center, for editing the manuscript. This paper was reviewed and approved by the HIV Prevention Trials Network manuscript review committee. This work was funded by the US National Institutes of Health through the following grants from the National Institute of Allergy and Infectious Diseases and the National Institute on Drug Abuse: UM1AI068613, UM1AI068617 and UM1AI068619. The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the preparation of the manuscript. S.D.-M., L.-G.B., N.M.M. and C.L.C. led the HIV Prevention Trials Network 082 trial. Laboratory testing of tenofovir diphosphate concentrations in dried blood spot samples was supervised by P.L.A. M.M. wrote the R code, ran the calibration and wrote the initial draft of the manuscript. D.J.D. and D.D. supervised the analysis of the project. D.J.D., D.D., M.-C.B., K.M.M. and S.S. provided feedback on methodology.
Corresponding author
Ethics declarations
Competing interests
P.L.A. has received personal fees from Gilead, ViiV and Merck, as well as research support from Gilead, paid to his institution. L.-G.B. has received honoraria for advisories to Gilead Sciences, Merck (Pty) Ltd, ViiV Healthcare and Janssen; these are not ongoing. K.M.M. has received teaching payments from Pfizer, outside the submitted work. All other authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Jeremie Guedj, Robin Schaefer and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Alison Farrell, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Efficacy of TDF/FTC by TFV-DP measurement in model h2.
Reduction in incidence in HIV as a function of tenofovir diphosphate (TFV-DP) levels in dried blood spots measurement according to model h_2. Grey ribbon = IQR, Dashed line = 95% Credible Interval. Colored rectangles represent the IQR of TFV-DP measurements associated with two pills per week (red), four pills per week (blue) and seven pills per week (green) derived from directly observed dosing8.
Extended Data Fig. 2 Efficacy of TDF/FTC by TFV-DP measurement in model h3.
Reduction in incidence in HIV as a function of tenofovir diphosphate (TFV-DP) levels in dried blood spots measurement according to model h3. Grey ribbon = IQR, Dashed line = 95% Credible Interval. Colored rectangles represent the IQR of TFV-DP measurements associated with two pills per week (red), four pills per week (blue) and seven pills per week (green) derived from directly observed dosing8.
Extended Data Fig. 3 Adherence-efficacy model curves.
Assumed functional forms for PrEP efficacy as a function of intraerythrocytic tenofovir diphosphate, testing assumptions that individuals with no quantifiable TFV-DP have the same HIV incidence as individuals concurrently randomized to placebo and that HIV incidence approaches zero with increasing TFV-DP. f1 includes both assumptions. f2 challenges the first assumption by allowing individuals with low PrEP adherence to have lower (or higher) efficacy k2 than those on placebo. f3 challenges the second assumption as efficacy approaches k3.
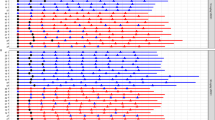
Extended Data Fig. 4 Imputation of TFV-DP concentration from plasma TFV quantifiability.
Measurements of intraerythrocytic TFV-DP among HPTN 082 participants with quantifiable or unquantifiable plasma TFV using the quantification threshold of each trial (see Extended Data Table 2). Plots are based on a total of N = 1083 samples, which are divided into positive and negative depending on the quantification threshold. For FEMPrEP and partners PrEP, the total is only 1081 because for two samples the quantification threshold could not be evaluated due to missing data. Width = frequency, white dot = median, black rectangle = interquartile range, black line = upper and lower adjacent values.
Supplementary information
Supplementary Information
Supplementary Fig. 1 and Table 1.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Moore, M., Stansfield, S., Donnell, D.J. et al. Efficacy estimates of oral pre-exposure prophylaxis for HIV prevention in cisgender women with partial adherence. Nat Med 29, 2748–2752 (2023). https://doi.org/10.1038/s41591-023-02564-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-023-02564-5
This article is cited by
-
Person-centered HIV PrEP for cisgender women
Nature Medicine (2023)