Abstract
Currently, most men with infertility cannot be given an aetiology, which reflects a lack of knowledge around gamete production and how it is affected by genetics and the environment. A failure to recognize the burden of male infertility and its potential as a biomarker for systemic illness exists. The absence of such knowledge results in patients generally being treated as a uniform group, for whom the strategy is to bypass the causality using medically assisted reproduction (MAR) techniques. In doing so, opportunities to prevent co-morbidity are missed and the burden of MAR is shifted to the woman. To advance understanding of men’s reproductive health, longitudinal and multi-national centres for data and sample collection are essential. Such programmes must enable an integrated view of the consequences of genetics, epigenetics and environmental factors on fertility and offspring health. Definition and possible amelioration of the consequences of MAR for conceived children are needed. Inherent in this statement is the necessity to promote fertility restoration and/or use the least invasive MAR strategy available. To achieve this aim, protocols must be rigorously tested and the move towards personalized medicine encouraged. Equally, education of the public, governments and clinicians on the frequency and consequences of infertility is needed. Health options, including male contraceptives, must be expanded, and the opportunities encompassed in such investment understood. The pressing questions related to male reproductive health, spanning the spectrum of andrology are identified in the Expert Recommendation.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
WHO. Infecundity, infertility, and childlessness in Developing Countries - DHS Comparative reports no. 9. WHO https://www.who.int/publications/m/item/infecundity-infertility-and-childlessness-in-developing-countries---dhs-comparative-reports-no.-9 (2004).
Forti, G. & Krausz, C. Clinical review 100: evaluation and treatment of the infertile couple. J. Clin. Endocrinol. Metab. 83, 4177–4188 (1998).
De Jonge, C. & Barratt, C. L. R. The present crisis in male reproductive health: an urgent need for a political, social, and research roadmap. Andrology 7, 762–768 (2019).
Esteves, S. C. Evolution of the World Health Organization semen analysis manual: where are we? Nat. Rev. Urol. 19, 439–446 (2022).
Boitrelle, F. et al. The sixth edition of the WHO manual for human semen analysis: a critical review and SWOT analysis. Life 11, 1368 (2021).
Eisenberg, M. L., Li, S., Behr, B., Pera, R. R. & Cullen, M. R. Relationship between semen production and medical comorbidity. Fertil. Steril. 103, 66–71 (2015).
Lismer, A. & Kimmins, S. Emerging evidence that the mammalian sperm epigenome serves as a template for embryo development. Nat. Commun. 14, 2142 (2023).
Houston, B. J. et al. A systematic review of the validated monogenic causes of human male infertility: 2020 update and a discussion of emerging gene-disease relationships. Hum. Reprod. Update 28, 15–29 (2021).
Skakkebaek, N. E. et al. Environmental factors in declining human fertility. Nat. Rev. Endocrinol. 18, 139–157 (2022).
Datta, J. et al. Prevalence of infertility and help seeking among 15 000 women and men. Hum. Reprod. 31, 2108–2118 (2016).
Barratt, C. L. R. et al. The diagnosis of male infertility: an analysis of the evidence to support the development of global WHO guidance-challenges and future research opportunities. Hum. Reprod. Update 23, 660–680 (2017).
Baker, H. W. G. in Endocrinology (eds Jameson J. L. & DeGroot, L. J.) Ch. 141, 2556–2579 (Saunders Elsevier, 2010).
Bonde, J. P. et al. Relation between semen quality and fertility: a population-based study of 430 first-pregnancy planners. Lancet 352, 1172–1177 (1998).
Schlegel, P. N. et al. Diagnosis and treatment of infertility in Men: AUA/ASRM guideline part I. J. Urol. 205, 36–43 (2021).
Schlegel, P. N. et al. Diagnosis and treatment of infertility in Men: AUA/ASRM guideline part II. J. Urol. 205, 44–51 (2021).
Minhas, S. et al. European Association of Urology guidelines on male sexual and reproductive health: 2021 update on male infertility. Eur. Urol. 80, 603–620 (2021).
Practice Committee of the American Society for Reproductive Medicine. Diagnostic evaluation of the infertile male: a committee opinion. Fertil. Steril. 103, e18–e25 (2015).
Samplaski, M. K. et al. Reproductive endocrinologists are the gatekeepers for male infertility care in North America: results of a North American survey on the referral patterns and characteristics of men presenting to male infertility specialists for infertility investigations. Fertil. Steril. 112, 657–662 (2019).
Punab, M. et al. Causes of male infertility: a 9-year prospective monocentre study on 1737 patients with reduced total sperm counts. Hum. Reprod. 32, 18–31 (2017).
Campbell, M. J. et al. Distribution of semen examination results 2020 — A follow up of data collated for the WHO semen analysis manual 2010. Andrology 9, 817–822 (2021).
Bohring, C. & Krause, W. Serum levels of inhibin B in men with different causes of spermatogenic failure. Andrologia 31, 137–141 (1999).
Sikaris, K. et al. Reproductive hormone reference intervals for healthy fertile young men: evaluation of automated platform assays. J. Clin. Endocrinol. Metab. 90, 5928–5936 (2005).
Waller, E.-J., Conceicao, J., Matson, P. & Yovich, J. Proposed age-stratified reference intervals of FSH derived from normozoospermic men. Asian Pac. J. Reprod. 10, 162–167 (2021).
Nahoul, K. & Roger, M. Age-related decline of plasma bioavailable testosterone in adult men. J. Steroid Biochem. 35, 293–299 (1990).
Neaves, W. B., Johnson, L., Porter, J. C., Parker, C. R. Jr. & Petty, C. S. Leydig cell numbers, daily sperm production, and serum gonadotropin levels in aging men. J. Clin. Endocrinol. Metab. 59, 756–763 (1984).
Bjørnerem, A. et al. Endogenous sex hormones in relation to age, sex, lifestyle factors, and chronic diseases in a general population: the Tromsø Study. J. Clin. Endocrinol. Metab. 89, 6039–6047 (2004).
Gray, A., Feldman, H. A., McKinlay, J. B. & Longcope, C. Age, disease, and changing sex hormone levels in middle-aged men: results of the Massachusetts Male Aging Study. J. Clin. Endocrinol. Metab. 73, 1016–1025 (1991).
Andersson, A. M., Jorgensen, N., Frydelund-Larsen, L., Rajpert-De Meyts, E. & Skakkebaek, N. E. Impaired Leydig cell function in infertile men: a study of 357 idiopathic infertile men and 318 proven fertile controls. J. Clin. Endocrinol. Metab. 89, 3161–3167 (2004).
Schlegel, P. N. et al. Diagnosis and treatment of infertility in men: AUA/ASRM guideline part II. Fertil. Steril. 115, 62–69 (2021).
Schlegel, P. N. et al. Diagnosis and treatment of infertility in men: AUA/ASRM guideline part I. Fertil. Steril. 115, 54–61 (2021).
Jungwirth, A et al. EAU Guidelines on Male Infertility https://d56bochluxqnz.cloudfront.net/media/EAU-Guidelines-on-Male-Infertility-2019.pdf (EAU, 2019).
Australia and New Zealand Assisted Reproduction Database ANZARD https://www.fertilitysociety.com.au/anzard/#anzard (2019).
Nixon, B. et al. New horizons in human sperm selection for assisted reproduction. Front. Endocrinol. 14, 1145533 (2023).
You, J. B. et al. Machine learning for sperm selection. Nat. Rev. Urol. 18, 387–403 (2021).
Khandwala, Y. S., Zhang, C. A., Lu, Y. & Eisenberg, M. L. The age of fathers in the USA is rising: an analysis of 168 867 480 births from 1972 to 2015. Hum. Reprod. 32, 2110–2116 (2017).
Hviid Malling, G. M. et al. ‘Doing it in the right order’: childless men’s intentions regarding family formation. Hum. Fertil. 25, 188–196 (2020).
Priskorn, L. et al. RUBIC (ReproUnion Biobank and Infertility Cohort): a binational clinical foundation to study risk factors, life course, and treatment of infertility and infertility-related morbidity. Andrology 9, 1828–1842 (2021).
Mazzilli, R. et al. Severe male factor in in vitro fertilization: definition, prevalence, and treatment. An update. Asian J. Androl. 24, 125–134 (2022).
Tournaye, H., Krausz, C. & Oates, R. D. Concepts in diagnosis and therapy for male reproductive impairment. Lancet Diabetes Endocrinol. 5, 554–564 (2017).
Young, J. et al. Clinical management of congenital hypogonadotropic hypogonadism. Endocr. Rev. 40, 669–710 (2019).
Butz, H., Nyiro, G., Kurucz, P. A., Liko, I. & Patocs, A. Molecular genetic diagnostics of hypogonadotropic hypogonadism: from panel design towards result interpretation in clinical practice. Hum. Genet. 140, 113–134 (2021).
Chudnovsky, A. & Niederberger, C. S. Gonadotropin therapy for infertile men with hypogonadotropic hypogonadism. J. Androl. 28, 644–646 (2007).
Avellino, G. J., Lipshultz, L. I., Sigman, M. & Hwang, K. Transurethral resection of the ejaculatory ducts: etiology of obstruction and surgical treatment options. Fertil. Steril. 111, 427–443 (2019).
Heidenreich, A., Altmann, P. & Engelmann, U. H. Microsurgical vasovasostomy versus microsurgical epididymal sperm aspiration/testicular extraction of sperm combined with intracytoplasmic sperm injection. A cost-benefit analysis. Eur. Urol. 37, 609–614 (2000).
Aggour, A., Mostafa, H. & Maged, W. Endoscopic management of ejaculatory duct obstruction. Int. Urol. Nephrol. 30, 481–485 (1998).
Modgil, V., Rai, S., Ralph, D. J. & Muneer, A. An update on the diagnosis and management of ejaculatory duct obstruction. Nat. Rev. Urol. 13, 13–20 (2016).
Wosnitzer, M., Goldstein, M. & Hardy, M. P. Review of azoospermia. Spermatogenesis 4, e28218 (2014).
Practice Committee of the American Society for Reproductive Medicine in collaboration with the Society for Male Reproduction and Urology. The management of obstructive azoospermia: a committee opinion. Fertil. Steril. 111, 873–880 (2019).
Colpi, G. M. et al. European Academy of Andrology guideline management of oligo-astheno-teratozoospermia. Andrology 6, 513–524 (2018).
Nicopoullos, J. D. et al. Use of surgical sperm retrieval in azoospermic men: a meta-analysis. Fertil. Steril. 82, 691–701 (2004).
Punjani, N., Kang, C. & Schlegel, P. N. Two decades from the introduction of microdissection testicular sperm extraction: how this surgical technique has improved the management of NOA. J. Clin. Med. 10, 1374 (2021).
Krausz, C. et al. Genetic dissection of spermatogenic arrest through exome analysis: clinical implications for the management of azoospermic men. Genet. Med. 22, 1956–1966 (2020).
Ji, C. et al. Potential of testis-derived circular RNAs in seminal plasma to predict the outcome of microdissection testicular sperm extraction in patients with idiopathic non-obstructive azoospermia. Hum. Reprod. 36, 2649–2660 (2021).
Rastrelli, G., Corona, G., Mannucci, E. & Maggi, M. Factors affecting spermatogenesis upon gonadotropin-replacement therapy: a meta-analytic study. Andrology 2, 794–808 (2014).
Boeri, L., Capogrosso, P. & Salonia, A. Gonadotropin treatment for the male hypogonadotropic hypogonadism. Curr. Pharm. Des. 27, 2775–2783 (2020).
Ferlin, A. et al. Management of male factor infertility: position statement from the Italian Society of Andrology and Sexual Medicine (SIAMS): endorsing organization: Italian Society of Embryology, Reproduction, and Research (SIERR). J. Endocrinol. Invest. 45, 1085–1113 (2022).
Lee, J. A. & Ramasamy, R. Indications for the use of human chorionic gonadotropic hormone for the management of infertility in hypogonadal men. Transl. Androl. Urol. 7, S348–S352 (2018).
Prior, M., Stewart, J., McEleny, K., Dwyer, A. A. & Quinton, R. Fertility induction in hypogonadotropic hypogonadal men. Clin. Endocrinol. 89, 712–718 (2018).
Ramasamy, R., Stahl, P. J. & Schlegel, P. N. Medical therapy for spermatogenic failure. Asian J. Androl. 14, 57–60 (2012).
Omar, M. I. et al. Benefits of empiric nutritional and medical therapy for semen parameters and pregnancy and live birth rates in couples with idiopathic infertility: a systematic review and meta-analysis. Eur. Urol. 75, 615–625 (2019).
Behre, H. M. Clinical use of FSH in male infertility. Front. Endocrinol. 10, 322 (2019).
Caroppo, E. & Colpi, G. M. Hormonal treatment of men with nonobstructive azoospermia: what does the evidence suggest? J. Clin. Med. 10, 387 (2021).
Barbonetti, A. et al. The use of follicle stimulating hormone (FSH) for the treatment of the infertile man: position statement from the Italian Society of Andrology and Sexual Medicine (SIAMS). J. Endocrinol. Invest. 41, 1107–1122 (2018).
Del Giudice, F. et al. A systematic review and meta-analysis of clinical trials implementing aromatase inhibitors to treat male infertility. Asian J. Androl. 22, 360–367 (2020).
Ko, E. Y., Siddiqi, K., Brannigan, R. E. & Sabanegh, E. S. Jr. Empirical medical therapy for idiopathic male infertility: a survey of the American Urological Association. J. Urol. 187, 973–978 (2012).
Thaker, H. et al. Empirical medical therapy for idiopathic male infertility. F. S Rep. 1, 15–20 (2020).
Ferlin, A. et al. Toward a pharmacogenetic approach to male infertility: polymorphism of follicle-stimulating hormone beta-subunit promoter. Fertil. Steril. 96, 1344–1349.e2 (2011).
Simoni, M. et al. Treatment with human, recombinant FSH improves sperm DNA fragmentation in idiopathic infertile men depending on the FSH receptor polymorphism p.N680S: a pharmacogenetic study. Hum. Reprod. 31, 1960–1969 (2016).
Casamonti, E. et al. Short-term FSH treatment and sperm maturation: a prospective study in idiopathic infertile men. Andrology 5, 414–422 (2017).
de Ligny, W. et al. Antioxidants for male subfertility. Cochrane Database Syst. Rev. 5, CD007411 (2022).
Agarwal, A. et al. A global survey of reproductive specialists to determine the clinical utility of oxidative stress testing and antioxidant use in male infertility. World J. Mens. Health 39, 470–488 (2021).
Barati, E., Nikzad, H. & Karimian, M. Oxidative stress and male infertility: current knowledge of pathophysiology and role of antioxidant therapy in disease management. Cell Mol. Life Sci. 77, 93–113 (2020).
Aitken, R. J. Antioxidant trials — the need to test for stress. Hum. Reprod. Open. 2021, hoab007 (2021).
Schisterman, E. F. et al. Effect of folic acid and zinc supplementation in men on semen quality and live birth among couples undergoing infertility treatment: a randomized clinical trial. JAMA 323, 35–48 (2020).
Zini, A., San Gabriel, M. & Baazeem, A. Antioxidants and sperm DNA damage: a clinical perspective. J. Assist. Reprod. Genet. 26, 427–432 (2009).
Aitken, R. J. Reactive oxygen species as mediators of sperm capacitation and pathological damage. Mol. Reprod. Dev. 84, 1039–1052 (2017).
Houston, B., Curry, B. & Aitken, R. J. Human spermatozoa possess an IL4I1 l-amino acid oxidase with a potential role in sperm function. Reproduction 149, 587–596 (2015).
Lee, D., Moawad, A. R., Morielli, T., Fernandez, M. C. & O’Flaherty, C. Peroxiredoxins prevent oxidative stress during human sperm capacitation. Mol. Hum. Reprod. 23, 106–115 (2017).
Aitken, R. J. & Baker, M. A. Oxidative stress, sperm survival and fertility control. Mol. Cell Endocrinol. 250, 66–69 (2006).
Aitken, R. J. & Roman, S. D. Antioxidant systems and oxidative stress in the testes. Oxid. Med. Cell Longev. 1, 15–24 (2008).
Gharagozloo, P. & Aitken, R. J. The role of sperm oxidative stress in male infertility and the significance of oral antioxidant therapy. Hum. Reprod. 26, 1628–1640 (2011).
Kowalczyk, A. The role of the natural antioxidant mechanism in sperm cells. Reprod. Sci. 29, 1387–1394 (2022).
O’Flaherty, C. Orchestrating the antioxidant defenses in the epididymis. Andrology 7, 662–668 (2019).
Aitken, R. J. & Bakos, H. W. Should we be measuring DNA damage in human spermatozoa? New light on an old question. Hum. Reprod. 36, 1175–1185 (2021).
Smits, R. M. et al. Antioxidants for male subfertility. Cochrane Database Syst. Rev. 3, CD007411 (2019).
Steiner, A. Z. et al. The effect of antioxidants on male factor infertility: the Males, Antioxidants, and Infertility (MOXI) randomized clinical trial. Fertil. Steril. 113, 552–560.e3 (2020).
Tuttelmann, F., Ruckert, C. & Ropke, A. Disorders of spermatogenesis: perspectives for novel genetic diagnostics after 20 years of unchanged routine. Med. Genet. 30, 12–20 (2018).
Tuttelmann, F. et al. Clinical experience with azoospermia: aetiology and chances for spermatozoa detection upon biopsy. Int. J. Androl. 34, 291–298 (2011).
Krausz, C. & Riera-Escamilla, A. Genetics of male infertility. Nat. Rev. Urol. 15, 369–384 (2018).
Wyrwoll, M. J. et al. Genetic architecture of azoospermia-time to advance the standard of care. Eur. Urol. 83, 452–462 (2022).
Toure, A. et al. The genetic architecture of morphological abnormalities of the sperm tail. Hum. Genet. 140, 21–42 (2021).
Salas-Huetos, A. et al. Disruption of human meiotic telomere complex genes TERB1, TERB2 and MAJIN in men with non-obstructive azoospermia. Hum. Genet. 140, 217–227 (2021).
Wyrwoll, M. J. et al. Bi-allelic mutations in M1AP are a frequent cause of meiotic arrest and severely impaired spermatogenesis leading to male infertility. Am. J. Hum. Genet. 107, 342–351 (2020).
Kasak, L. et al. Bi-allelic recessive loss-of-function variants in FANCM cause non-obstructive azoospermia. Am. J. Hum. Genet. 103, 200–212 (2018).
Hardy, J. J. et al. Variants in GCNA, X-linked germ-cell genome integrity gene, identified in men with primary spermatogenic failure. Hum. Genet. 140, 1169–1182 (2021).
Liu, C. et al. Deleterious variants in X-linked CFAP47 induce asthenoteratozoospermia and primary male infertility. Am. J. Hum. Genet. 108, 309–323 (2021).
Zhu, F. et al. Biallelic SUN5 mutations cause autosomal-recessive acephalic spermatozoa syndrome. Am. J. Hum. Genet. 99, 942–949 (2016).
Coutton, C. et al. Bi-allelic mutations in ARMC2 lead to severe astheno-teratozoospermia due to sperm flagellum malformations in humans and mice. Am. J. Hum. Genet. 104, 331–340 (2019).
Tang, S. et al. Biallelic mutations in CFAP43 and CFAP44 cause male infertility with multiple morphological abnormalities of the sperm flagella. Am. J. Hum. Genet. 100, 854–864 (2017).
Veltman, J. A. & Brunner, H. G. De novo mutations in human genetic disease. Nat. Rev. Genet. 13, 565–575 (2012).
Hodzic, A. et al. De novo mutations in idiopathic male infertility — a pilot study. Andrology 9, 212–220 (2021).
Oud, M. S. et al. Exome sequencing reveals variants in known and novel candidate genes for severe sperm motility disorders. Hum. Reprod. 36, 2597–2611 (2021).
Oud, M. S. et al. A de novo paradigm for male infertility. Nat. Commun. 13, 154 (2022).
Xavier, M. J., Salas-Huetos, A., Oud, M. S., Aston, K. I. & Veltman, J. A. Disease gene discovery in male infertility: past, present and future. Hum. Genet. 140, 7–19 (2021).
Krausz, C. et al. Phenotypic variation within European carriers of the Y-chromosomal gr/gr deletion is independent of Y-chromosomal background. J. Med. Genet. 46, 21–31 (2009).
Romerius, P. et al. Estrogen receptor alpha single nucleotide polymorphism modifies the risk of azoospermia in childhood cancer survivors. Pharmacogenet Genomics 21, 263–269 (2011).
Visscher, P. M., Yengo, L., Cox, N. J. & Wray, N. R. Discovery and implications of polygenicity of common diseases. Science 373, 1468–1473 (2021).
Townsley, K. G., Brennand, K. J. & Huckins, L. M. Massively parallel techniques for cataloguing the regulome of the human brain. Nat. Neurosci. 23, 1509–1521 (2020).
Groopman, E. E., Povysil, G., Goldstein, D. B. & Gharavi, A. G. Rare genetic causes of complex kidney and urological diseases. Nat. Rev. Nephrol. 16, 641–656 (2020).
Zhu, X. B. et al. Vertical transmission of the Yq AZFc microdeletion from father to son over two or three generations in infertile Han Chinese families. Asian J. Androl. 12, 240–246 (2010).
Smits, R. M. et al. De novo mutations in children born after medical assisted reproduction. Hum. Reprod. 37, 1360–1369 (2022).
Yu, X. W., Wei, Z. T., Jiang, Y. T. & Zhang, S. L. Y chromosome azoospermia factor region microdeletions and transmission characteristics in azoospermic and severe oligozoospermic patients. Int. J. Clin. Exp. Med. 8, 14634–14646 (2015).
Beaud, H., Tremblay, A. R., Chan, P. T. K. & Delbes, G. Sperm DNA damage in cancer patients. Adv. Exp. Med. Biol. 1166, 189–203 (2019).
Payne, K. S., Mazur, D. J., Hotaling, J. M. & Pastuszak, A. W. Cannabis and male fertility: a systematic review. J. Urol. 202, 674–681 (2019).
Diamanti-Kandarakis, E. et al. Endocrine-disrupting chemicals: an Endocrine Society scientific statement. Endocr. Rev. 30, 293–342 (2009).
Salas-Huetos, A., James, E. R., Aston, K. I., Jenkins, T. G. & Carrell, D. T. Diet and sperm quality: nutrients, foods and dietary patterns. Reprod. Biol. 19, 219–224 (2019).
Wu, H. et al. Preconception urinary phthalate concentrations and sperm DNA methylation profiles among men undergoing IVF treatment: a cross-sectional study. Hum. Reprod. 32, 2159–2169 (2017).
Skakkebæk, N. E. et al. Environmental factors in declining human fertility. Nat. Rev. Endocrinol. 18, 139–157 (2021).
Sharpe, R. M. Environmental/lifestyle effects on spermatogenesis. Philos. Trans. R. Soc. Lond. B Biol. Sci. 365, 1697–1712 (2010).
Bergman, A. et al. State of the science of endocrine disrupting chemicals 2012 (eds Bergman, Å et al.) (World Health Organization, 2012).
Gore, A. C. et al. EDC-2: the Endocrine Society’s second scientific statement on endocrine-disrupting chemicals. Endocr. Rev. 36, E1–E150 (2015).
Istvan, M. et al. Maternal occupational exposure to endocrine-disrupting chemicals during pregnancy and semen parameters in adulthood: results of a nationwide cross-sectional study among Swiss conscripts. Hum. Reprod. 36, 1948–1958 (2021).
Bonde, J. P. et al. The epidemiologic evidence linking prenatal and postnatal exposure to endocrine disrupting chemicals with male reproductive disorders: a systematic review and meta-analysis. Hum. Reprod. Update 23, 104–125 (2016).
Aneck-Hahn, N. H., Schulenburg, G. W., Bornman, M. S., Farias, P. & de Jager, C. Impaired semen quality associated with environmental DDT exposure in young men living in a malaria area in the Limpopo Province, South Africa. J. Androl. 28, 423–434 (2007).
Krewski, D. et al. Toxicity testing in the 21st century: progress in the past decade and future perspectives. Arch. Toxicol. 94, 1–58 (2020).
Barrow, P. & Schmitt, G. Regulatory approaches to nonclinical reproductive toxicity testing of anti-cancer drugs. Anticancer. Agents Med. Chem. 17, 1171–1183 (2017).
Kortenkamp, A. et al. Combined exposures to bisphenols, polychlorinated dioxins, paracetamol, and phthalates as drivers of deteriorating semen quality. Env. Int. 165, 107322 (2022).
Marcho, C., Oluwayiose, O. A. & Pilsner, J. R. The preconception environment and sperm epigenetics. Andrology 8, 924–942 (2020).
Short, A. K. et al. Elevated paternal glucocorticoid exposure alters the small noncoding RNA profile in sperm and modifies anxiety and depressive phenotypes in the offspring. Transl. Psychiatry 6, e837 (2016).
Komninos, D. et al. High fat diet-induced obesity prolongs critical stages of the spermatogenic cycle in a Ldlr−/−.Leiden mouse model. Sci. Rep. 12, 430 (2022).
Nassan, F. L. et al. Association between intake of soft drinks and testicular function in young men. Hum. Reprod. 36, 3036–3048 (2021).
Samplaski, M. K. & Nangia, A. K. Adverse effects of common medications on male fertility. Nat. Rev. Urol. 12, 401–413 (2015).
Sominsky, L. et al. Linking stress and infertility: a novel role for ghrelin. Endocr. Rev. 38, 432–467 (2017).
Abu-Musa, A. A., Nassar, A. H., Hannoun, A. B. & Usta, I. M. Effect of the Lebanese civil war on sperm parameters. Fertil. Steril. 88, 1579–1582 (2007).
Fenster, L. et al. Effects of psychological stress on human semen quality. J. Androl. 18, 194–202 (1997).
Leisegang, K., Henkel, R. & Agarwal, A. Obesity and metabolic syndrome associated with systemic inflammation and the impact on the male reproductive system. Am. J. Reprod. Immunol. 82, e13178 (2019).
Leisegang, K., Sengupta, P., Agarwal, A. & Henkel, R. Obesity and male infertility: mechanisms and management. Andrologia 53, e13617 (2021).
Kleeman, E. A., Gubert, C. & Hannan, A. J. Transgenerational epigenetic impacts of parental infection on offspring health and disease susceptibility. Trends Genet. 38, 662–675 (2022).
Gapp, K. et al. Alterations in sperm long RNA contribute to the epigenetic inheritance of the effects of postnatal trauma. Mol. Psychiatry 25, 2162–2174 (2020).
Maciejewski, R., Radzikowska-Büchner, E., Flieger, W., Kulczycka, K., Baj, J., Forma, A. & Flieger, J. An overview of essential microelements and common metallic nanoparticles and their effects on male fertility. Int. J. Env. Res. Public. Health 19, 11066 (2022). Sep 4.
Andersen, E. et al. Sperm count is increased by diet-induced weight loss and maintained by exercise or GLP-1 analogue treatment: a randomized controlled trial. Hum. Reprod. 37, 1414–1422 (2022).
Schjenken, J. E. et al. High fat diet alters male seminal plasma composition to impair female immune adaptation for pregnancy in mice. Endocrinology 162, bqab123 (2021).
Maleki-Saghooni, N., Amirian, M., Sadeghi, R. & Latifnejad Roudsari, R. Effectiveness of infertility counseling on pregnancy rate in infertile patients undergoing assisted reproductive technologies: a systematic review and meta-analysis. Int. J. Reprod. Biomed. 15, 391–402 (2017).
Rimmer, M. P. et al. Outcome reporting across randomized controlled trials evaluating potential treatments for male infertility: a systematic review. Hum. Reprod. Open. 2022, hoac010 (2022).
World Drug Report 2021. United Nations Office on Drugs and Crime https://www.unodc.org/unodc/en/data-and-analysis/wdr2021.html (2021).
Fronczak, C. M., Kim, E. D. & Barqawi, A. B. The insults of illicit drug use on male fertility. J. Androl. 33, 515–528 (2012).
Sakib, S., Voigt, A., Goldsmith, T. & Dobrinski, I. Three-dimensional testicular organoids as novel in vitro models of testicular biology and toxicology. Env. Epigenet 5, dvz011 (2019).
Martus, H. J. et al. Summary of major conclusions from the 7th International Workshop on Genotoxicity Testing (IWGT), Tokyo, Japan. Mutat. Res. 852, 503134 (2020).
Greally, J. M. Endocrine disruptors and the epigenome (OECD review) (Organisation for Economic Co-operation and Development, 2011).
Skakkebaek, N. E. et al. Male reproductive disorders and fertility trends: influences of environment and genetic susceptibility. Physiol. Rev. 96, 55–97 (2016).
Priskorn, L. et al. Increasing trends in childlessness in recent birth cohorts — a registry-based study of the total Danish male population born from 1945 to 1980. Int. J. Androl. 35, 449–455 (2012).
Boulicault, M. et al. The future of sperm: a biovariability framework for understanding global sperm count trends. Hum. Fertil. 25, 888–902 (2021). 1-15.
Guzick, D. S. et al. Sperm morphology, motility, and concentration in fertile and infertile men. N. Engl. J. Med. 345, 1388–1393 (2001).
Slama, R. et al. Time to pregnancy and semen parameters: a cross-sectional study among fertile couples from four European cities. Hum. Reprod. 17, 503–515 (2002).
Nelson, C. M. & Bunge, R. G. Semen analysis: evidence for changing parameters of male fertility potential. Fertil. Steril. 25, 503–507 (1974).
MacLeod, J. & Wang, Y. Male fertility potential in terms of semen quality: a review of the past, a study of the present. Fertil. Steril. 31, 103–116 (1979).
Carlsen, E., Giwercman, A., Keiding, N. & Skakkebaek, N. E. Evidence for decreasing quality of semen during past 50 years. BMJ 305, 609–613 (1992).
Levine, H. et al. Temporal trends in sperm count: a systematic review and meta-regression analysis. Hum. Reprod. Update 23, 646–659 (2017).
Lv, M. Q. et al. Temporal trends in semen concentration and count among 327 373 Chinese healthy men from 1981 to 2019: a systematic review. Hum. Reprod. 36, 1751–1775 (2021).
Vahidi, S., Moein, M. R., Yazdinejad, F., Ghasemi-Esmailabad, S. & Narimani, N. Iranian temporal changes in semen quality during the past 22 years: a report from an infertility center. Int. J. Reprod. Biomed. 18, 1059–1064 (2020).
Rosa-Villagrán, L., Barrera, N., Montes, J., Riso, C. & Sapiro, R. Decline of semen quality over the last 30 years in Uruguay. Basic. Clin. Androl. 31, 8 (2021).
Sengupta, P., Nwagha, U., Dutta, S., Krajewska-Kulak, E. & Izuka, E. Evidence for decreasing sperm count in African population from 1965 to 2015. Afr. Health Sci. 17, 418–427 (2017).
Mishra, P., Negi, M. P. S., Srivastava, M., Singh, K. & Rajender, S. Decline in seminal quality in Indian men over the last 37 years. Reprod. Biol. Endocrinol. 16, 103 (2018).
Levine, H. et al. Temporal trends in sperm count: a systematic review and meta-regression analysis of samples collected globally in the 20th and 21st centuries. Hum. Reprod. Update 29, 157–176 (2023).
Jorgensen, N. et al. Are worldwide sperm counts declining? Fertil. Steril. 116, 1457–1463 (2021).
Tiegs, A. W., Landis, J., Garrido, N., Scott, R. T. Jr. & Hotaling, J. M. Total motile sperm count trend over time: evaluation of semen analyses from 119,972 men from subfertile couples. Urology 132, 109–116 (2019).
Jorgensen, N. et al. East-West gradient in semen quality in the Nordic-Baltic area: a study of men from the general population in Denmark, Norway, Estonia and Finland. Hum. Reprod. 17, 2199–2208 (2002).
Paasch, U. et al. Semen quality in sub-fertile range for a significant proportion of young men from the general German population: a co-ordinated, controlled study of 791 men from Hamburg and Leipzig. Int. J. Androl. 31, 93–102 (2008).
Mendiola, J., Stahlhut, R. W., Jorgensen, N., Liu, F. & Swan, S. H. Shorter anogenital distance predicts poorer semen quality in young men in Rochester, New York. Env. Health Perspect. 119, 958–963 (2011).
Fernandez, M. F. et al. Semen quality and reproductive hormone levels in men from Southern Spain. Int. J. Androl. 35, 1–10 (2012).
Iwamoto, T. et al. Semen quality of 1559 young men from four cities in Japan: a cross-sectional population-based study. BMJ Open 3, e002222 (2013).
Jorgensen, N., Asklund, C., Carlsen, E. & Skakkebaek, N. E. Coordinated European investigations of semen quality: results from studies of Scandinavian young men is a matter of concern. Int. J. Androl. 29, 54–61 (2006). discussion 105–108.
Smarr, M. M. et al. Is human fecundity changing? A discussion of research and data gaps precluding us from having an answer. Hum. Reprod. 32, 499–504 (2017).
Belladelli, F., Muncey, W. & Eisenberg, M. L. Reproduction as a window for health in men. Fertil. Steril. 120, 429–437 (2023).
Economist Intelligence Unit. Fertile ground. How can Japan raise its fertility rate? Economist Intelligence Unit https://www.eiu.com/graphics/marketing/pdf/Fertility-in-Japan-EIU.pdf (2018).
Hauser, R. et al. Male reproductive disorders, diseases, and costs of exposure to endocrine-disrupting chemicals in the European Union. J. Clin. Endocrinol. Metab. 100, 1267–1277 (2015).
Attina, T. M. et al. Exposure to endocrine-disrupting chemicals in the USA: a population-based disease burden and cost analysis. Lancet Diabetes Endocrinol. 4, 996–1003 (2016).
Institute for Health Metrics and Evaluation. Global Burden of Disease. IHME https://www.healthdata.org/research-analysis/gbd (2023).
Arya, S. T. & Dibb, B. The experience of infertility treatment: the male perspective. Hum. Fertil. 19, 242–248 (2016).
Koert, E., Takefman, J. & Boivin, J. Fertility quality of life tool: update on research and practice considerations. Hum. Fertil. 24, 236–248 (2019).
Salonia, A. et al. Are infertile men less healthy than fertile men? Results of a prospective case-control survey. Eur. Urol. 56, 1025–1031 (2009).
Ventimiglia, E. et al. Infertility as a proxy of general male health: results of a cross-sectional survey. Fertil. Steril. 104, 48–55 (2015).
Eisenberg, M. L. et al. The relationship between male BMI and waist circumference on semen quality: data from the LIFE study. Hum. Reprod. 29, 193–200 (2014).
Jacobsen, R. et al. Risk of testicular cancer in men with abnormal semen characteristics: cohort study. BMJ 321, 789–792 (2000).
Walsh, T. J., Croughan, M. S., Schembri, M., Chan, J. M. & Turek, P. J. Increased risk of testicular germ cell cancer among infertile men. Arch. Intern. Med. 169, 351–356 (2009).
Del Giudice, F. et al. Association between male infertility and male-specific malignancies: systematic review and meta-analysis of population-based retrospective cohort studies. Fertil. Steril. 114, 984–996 (2020).
Al-Jebari, Y. et al. Risk of prostate cancer for men fathering through assisted reproduction: nationwide population based register study. BMJ 366, l5214 (2019).
Walsh, T. J. et al. Increased risk of high-grade prostate cancer among infertile men. Cancer 116, 2140–2147 (2010).
Hanson, H. A. et al. Subfertility increases risk of testicular cancer: evidence from population-based semen samples. Fertil. Steril. 105, 322–328.e1 (2016).
Eisenberg, M. L., Li, S., Brooks, J. D., Cullen, M. R. & Baker, L. C. Increased risk of cancer in infertile men: analysis of U.S. claims data. J. Urol. 193, 1596–1601 (2015).
Eisenberg, M. L., Betts, P., Herder, D., Lamb, D. J. & Lipshultz, L. I. Increased cancer risk and azoospermia. Fertil. Steril. 100, 681–685 (2013).
Swerdlow, A. J., Bruce, C., Cooke, R., Coulson, P. & Jones, M. E. Infertility and risk of breast cancer in men: a national case-control study in England and Wales. Breast Cancer Res. 24, 29 (2022).
Man, Y. et al. Whole-exome sequencing identifies the VHL mutation (c.262T > C, p.Try88Arg) in non-obstructive azoospermia-associated cystic renal cell carcinoma. Curr. Oncol. 29, 2376–2384 (2022).
Chen, P. C. et al. Male infertility increases the risk of cardiovascular diseases: a nationwide population-based cohort study in Taiwan. World J. Mens. Health 40, 490–500 (2022).
Elenkov, A., Melander, O., Nilsson, P. M., Zhang, H. & Giwercman, A. Impact of genetic risk score on the association between male childlessness and cardiovascular disease and mortality. Sci. Rep. 11, 18526 (2021).
Brubaker, W. D., Li, S., Baker, L. C. & Eisenberg, M. L. Increased risk of autoimmune disorders in infertile men: analysis of US claims data. Andrology 6, 94–98 (2018).
Eisenberg, M. L., Li, S., Cullen, M. R. & Baker, L. C. Increased risk of incident chronic medical conditions in infertile men: analysis of United States claims data. Fertil. Steril. 105, 629–636 (2015).
Glazer, C. H. et al. Male factor infertility and risk of multiple sclerosis: a register-based cohort study. Mult. Scler. 24, 1835–1842 (2017).
Glazer, C. H. et al. Risk of diabetes according to male factor infertility: a register-based cohort study. Hum. Reprod. 32, 1474–1481 (2017).
Latif, T. et al. Semen quality as a predictor of subsequent morbidity: a Danish cohort study of 4,712 men with long-term follow-up. Am. J. Epidemiol. 186, 910–917 (2017).
Latif, T. et al. Semen quality associated with subsequent hospitalizations — can the effect be explained by socio-economic status and lifestyle factors? Andrology 6, 428–435 (2018).
Jensen, T. K., Jacobsen, R., Christensen, K., Nielsen, N. C. & Bostofte, E. Good semen quality and life expectancy: a cohort study of 43,277 men. Am. J. Epidemiol. 170, 559–565 (2009).
Glazer, C. H. et al. Male factor infertility and risk of death: a nationwide record-linkage study. Hum. Reprod. 34, 2266–2273 (2019).
Eisenberg, M. L. et al. Semen quality, infertility and mortality in the USA. Hum. Reprod. 29, 1567–1574 (2014).
Del Giudice, F. et al. The association between mortality and male infertility: systematic review and meta-analysis. Urology 154, 148–157 (2021).
Del Giudice, F. et al. Increased mortality among men diagnosed with impaired fertility: analysis of US claims data. Urology 147, 143–149 (2021).
Choy, J. T. & Eisenberg, M. L. Male infertility as a window to health. Fertil. Steril. 110, 810–814 (2018).
Uhlen, M. et al. Proteomics. Tissue-based map of the human proteome. Science 347, 1260419 (2015).
Fagerberg, L. et al. Analysis of the human tissue-specific expression by genome-wide integration of transcriptomics and antibody-based proteomics. Mol. Cell Proteom. 13, 397–406 (2014).
Djureinovic, D. et al. The human testis-specific proteome defined by transcriptomics and antibody-based profiling. Mol. Hum. Reprod. 20, 476–488 (2014).
Bonadona, V. et al. Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome. JAMA 305, 2304–2310 (2011).
Ji, G. et al. Common variants in mismatch repair genes associated with increased risk of sperm DNA damage and male infertility. BMC Med. 10, 49 (2012).
Mak, V. et al. Proportion of cystic fibrosis gene mutations not detected by routine testing in men with obstructive azoospermia. JAMA 281, 2217–2224 (1999).
Gunes, S. et al. Microtubular dysfunction and male infertility. World J. Mens. Health 38, 9–23 (2020).
Day, F. R. et al. Large-scale genomic analyses link reproductive aging to hypothalamic signaling, breast cancer susceptibility and BRCA1-mediated DNA repair. Nat. Genet. 47, 1294–1303 (2015).
O’Bryan, M. K. & Hedger, M. P. Inflammatory networks in the control of spermatogenesis : chronic inflammation in an immunologically privileged tissue? Adv. Exp. Med. Biol. 636, 92–114 (2008).
Meinhardt, A. & Hedger, M. P. Immunological, paracrine and endocrine aspects of testicular immune privilege. Mol. Cell Endocrinol. 335, 60–68 (2011).
Meseguer, M. et al. Sperm cryopreservation in oncological patients: a 14-year follow-up study. Fertil. Steril. 85, 640–645 (2006).
Liu, W., Schulster, M. L., Alukal, J. P. & Najari, B. B. Fertility preservation in male to female transgender patients. Urol. Clin. North. Am. 46, 487–493 (2019).
Cooper, H. C., Long, J. & Aye, T. Fertility preservation in transgender and non-binary adolescents and young adults. PLoS ONE 17, e0265043 (2022).
Lambertini, M. et al. Fertility preservation and post-treatment pregnancies in post-pubertal cancer patients: ESMO clinical practice guidelines(dagger). Ann. Oncol. 31, 1664–1678 (2020).
Lee, S. J. et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J. Clin. Oncol. 24, 2917–2931 (2006).
Kuczynski, W. et al. The outcome of intracytoplasmic injection of fresh and cryopreserved ejaculated spermatozoa-a prospective randomized study. Hum. Reprod. 16, 2109–2113 (2001).
Hervas, I. et al. TESE-ICSI outcomes per couple in vasectomized males are negatively affected by time since the intervention, but not other comorbidities. Reprod. Biomed. Online 43, 708–717 (2021).
Newton, H. L. et al. Inconsistencies in fertility preservation for young people with cancer in the UK. Arch. Dis. Child. 107, 265–270 (2022).
Anazodo, A. et al. The development of an international oncofertility competency framework: a model to increase oncofertility implementation. Oncologist 24, e1450–e1459 (2019).
Anazodo, A. et al. How can we improve oncofertility care for patients? A systematic scoping review of current international practice and models of care. Hum. Reprod. Update 25, 159–179 (2019).
Delgouffe, E., Braye, A. & Goossens, E. Testicular tissue banking for fertility preservation in young boys: which patients should be included? Front. Endocrinol. 13, 854186 (2022).
Martinez, F. & International Society for Fertility Preservation. Update on fertility preservation from the Barcelona International Society for Fertility Preservation-ESHRE-ASRM 2015 expert meeting: indications, results and future perspectives. Fertil. Steril. 108, 407–415.e11 (2017).
Mulder, R. L. et al. Fertility preservation for male patients with childhood, adolescent, and young adult cancer: recommendations from the PanCareLIFE Consortium and the International Late Effects of Childhood Cancer Guideline Harmonization Group. Lancet Oncol. 22, e57–e67 (2021).
Ghidei, L. et al. Current gaps in fertility preservation for men: how can we do better? J. Clin. Oncol. 40, 2524–2529 (2022).
Goossens, E. et al. Fertility preservation in boys: recent developments and new insights. Hum. Reprod. Open. 2020, hoaa016 (2020).
Sharma, S., Wistuba, J., Pock, T., Schlatt, S. & Neuhaus, N. Spermatogonial stem cells: updates from specification to clinical relevance. Hum. Reprod. Update 25, 275–297 (2019).
Wyns, C., Curaba, M., Vanabelle, B., Van Langendonckt, A. & Donnez, J. Options for fertility preservation in prepubertal boys. Hum. Reprod. Update 16, 312–328 (2010).
Kliesch, S. [Androprotect and prospects for fertility treatment]. Urol. A 55, 898–903 (2016).
Kanbar, M., Delwiche, G. & Wyns, C. Fertility preservation for prepubertal boys: are we ready for autologous grafting of cryopreserved immature testicular tissue? Ann. Endocrinol. 83, 210–217 (2022).
Abdelaal, O., Barber, H., Atala, A. & Sadri-Ardekani, H. Purging of malignant cell contamination prior to spermatogonia stem cell autotransplantation to preserve fertility: progress & prospects. Curr. Opin. Endocrinol. Diabetes Obes. 26, 166–174 (2019).
Shetty, G. et al. Postpubertal spermatogonial stem cell transplantation restores functional sperm production in rhesus monkeys irradiated before and after puberty. Andrology 9, 1603–1616 (2021).
Fayomi, A. P. et al. Autologous grafting of cryopreserved prepubertal rhesus testis produces sperm and offspring. Science 363, 1314–1319 (2019).
Alves-Lopes, J. P., Soder, O. & Stukenborg, J. B. Use of a three-layer gradient system of cells for rat testicular organoid generation. Nat. Protoc. 13, 248–259 (2018).
Mincheva, M. et al. Reassembly of adult human testicular cells: can testis cord-like structures be created in vitro. Mol. Hum. Reprod. 24, 55–63 (2018).
Oliver, E. et al. Self-organising human gonads generated by a Matrigel-based gradient system. BMC Biol. 19, 212 (2021).
Ishikura, Y. et al. In vitro reconstitution of the whole male germ-cell development from mouse pluripotent stem cells. Cell Stem Cell 28, 2167–2179.e9 (2021).
Saitou, M. & Hayashi, K. Mammalian in vitro gametogenesis. Science 374, eaaz6830 (2021).
Pennings, G., Couture, V. & Ombelet, W. Social sperm freezing. Hum. Reprod. 36, 833–839 (2021).
Degraeve, A. et al. European countries have different rates of sperm cryopreservation before vasectomy and at the time of reversal. Andrology 10, 1286–1291 (2022).
Marinaro, J., Hayden, R. P., Shin, P. & Tanrikut, C. The utility of sperm cryopreservation at the time of vasectomy reversal. J. Urol. 205, 236–240 (2021).
Ravitsky, V. & Kimmins, S. The forgotten men: rising rates of male infertility urgently require new approaches for its prevention, diagnosis and treatment. Biol. Reprod. 101, 872–874 (2019).
Kong, A. et al. Rate of de novo mutations and the importance of father’s age to disease risk. Nature 488, 471–475 (2012).
Taylor, J. L. et al. Paternal-age-related de novo mutations and risk for five disorders. Nat. Commun. 10, 3043 (2019).
Sartorius, G. A. & Nieschlag, E. Paternal age and reproduction. Hum. Reprod. Update 16, 65–79 (2010).
Couture, V., Delisle, S., Mercier, A. & Pennings, G. The other face of advanced paternal age: a scoping review of its terminological, social, public health, psychological, ethical and regulatory aspects. Hum. Reprod. Update 27, 305–323 (2021).
Urhoj, S. K. et al. Advanced paternal age and childhood cancer in offspring: a nationwide register-based cohort study. Int. J. Cancer 140, 2461–2472 (2017).
Cao, M. et al. High-resolution analyses of human sperm dynamic methylome reveal thousands of novel age-related epigenetic alterations. Clin. Epigenetics 12, 192 (2020).
Salas-Huetos, A. et al. The combined effect of obesity and aging on human sperm DNA methylation signatures: inclusion of BMI in the paternal germ line age prediction model. Sci. Rep. 10, 15409 (2020).
Laurentino, S. et al. A germ cell-specific ageing pattern in otherwise healthy men. Aging Cell 19, e13242 (2020).
Berntsen, S. et al. The health of children conceived by ART: ‘the chicken or the egg?’. Hum. Reprod. Update 25, 137–158 (2019).
Horne, G. et al. Live birth with sperm cryopreserved for 21 years prior to cancer treatment: case report. Hum. Reprod. 19, 1448–1449 (2004).
Rotondo, J. C., Lanzillotti, C., Mazziotta, C., Tognon, M. & Martini, F. Epigenetics of male infertility: the role of DNA methylation. Front. Cell Dev. Biol. 9, 689624 (2021).
Erkek, S. et al. Molecular determinants of nucleosome retention at CpG-rich sequences in mouse spermatozoa. Nat. Struct. Mol. Biol. 20, 868–875 (2013).
Siklenka, K. et al. Disruption of histone methylation in developing sperm impairs offspring health transgenerationally. Science 350, aab2006 (2015).
Sendler, E. et al. Stability, delivery and functions of human sperm RNAs at fertilization. Nucleic Acids Res. 41, 4104–4117 (2013).
Cavalli, G. & Heard, E. Advances in epigenetics link genetics to the environment and disease. Nature 571, 489–499 (2019).
Janssen, S. M. & Lorincz, M. C. Interplay between chromatin marks in development and disease. Nat. Rev. Genet. 23, 137–153 (2021).
Lin, H. piRNAs in the germ line. Science 316, 397 (2007).
Trasler, J. M. Epigenetics in spermatogenesis. Mol. Cell Endocrinol. 306, 33–36 (2009).
Glaser, S. et al. The histone 3 lysine 4 methyltransferase, Mll2, is only required briefly in development and spermatogenesis. Epigenetics Chromatin 2, 5 (2009).
Kimmins, S. et al. Differential functions of the Aurora-B and Aurora-C kinases in mammalian spermatogenesis. Mol. Endocrinol. 21, 726–739 (2007).
Peters, A. H. et al. Loss of the Suv39h histone methyltransferases impairs mammalian heterochromatin and genome stability. Cell 107, 323–337 (2001).
Nagirnaja, L. et al. Variant PNLDC1, defective piRNA processing, and azoospermia. N. Engl. J. Med. 385, 707–719 (2021).
Fellmeth, J. E., Ghanaim, E. M. & Schindler, K. Characterization of macrozoospermia-associated AURKC mutations in a mammalian meiotic system. Hum. Mol. Genet. 25, 2698–2711 (2016).
Dieterich, K. et al. Homozygous mutation of AURKC yields large-headed polyploid spermatozoa and causes male infertility. Nat. Genet. 39, 661–665 (2007).
Eloualid, A. et al. Prevalence of the Aurora kinase C c.144delC mutation in infertile Moroccan men. Fertil. Steril. 101, 1086–1090 (2014).
Ben Khelifa, M. et al. Identification of a new recurrent aurora kinase C mutation in both European and African men with macrozoospermia. Hum. Reprod. 27, 3337–3346 (2012).
Tremblay, A., Beaud, H. & Delbes, G. Transgenerational impact of chemotherapy: would the father exposure impact the health of future progeny [French]? Gynecol. Obstet. Fertil. Senol. 45, 609–618 (2017).
Carrell, D. T. Epigenetics of the male gamete. Fertil. Steril. 97, 267–274 (2012).
Santiago, J., Silva, J. V., Howl, J., Santos, M. A. S. & Fardilha, M. All you need to know about sperm RNAs. Hum. Reprod. Update 28, 67–91 (2021).
Kobayashi, H. et al. Aberrant DNA methylation of imprinted loci in sperm from oligospermic patients. Hum. Mol. Genet. 16, 2542–2551 (2007).
Marques, C. J. et al. Abnormal methylation of imprinted genes in human sperm is associated with oligozoospermia. Mol. Hum. Reprod. 14, 67–74 (2008).
Minor, A., Chow, V. & Ma, S. Aberrant DNA methylation at imprinted genes in testicular sperm retrieved from men with obstructive azoospermia and undergoing vasectomy reversal. Reproduction 141, 749–757 (2011).
Donkin, I. et al. Obesity and bariatric surgery drive epigenetic variation of spermatozoa in humans. Cell Metab. 23, 369–378 (2016).
Velotti, N. et al. Effect of bariatric surgery on in vitro fertilization in infertile men with obesity. Surg. Obes. Relat. Dis. 17, 1752–1759 (2021).
Keyhan, S. et al. Male obesity impacts DNA methylation reprogramming in sperm. Clin. Epigenetics 13, 17 (2021).
Stokes, V. J., Anderson, R. A. & George, J. T. How does obesity affect fertility in men – and what are the treatment options? Clin. Endocrinol. 82, 633–638 (2015).
Chan, D. et al. Customized methylC-capture sequencing to evaluate variation in the human sperm DNA methylome representative of altered folate metabolism. Env. Health Perspect. 127, 87002 (2019).
Pembrey, M., Saffery, R. & Bygren, L. O. Human transgenerational responses to early-life experience: potential impact on development, health and biomedical research. J. Med. Genet. 51, 563–572 (2014).
Radford, E. J. et al. In utero effects. In utero undernourishment perturbs the adult sperm methylome and intergenerational metabolism. Science 345, 1255903 (2014).
Chen, Q. et al. Sperm tsRNAs contribute to intergenerational inheritance of an acquired metabolic disorder. Science 351, 397–400 (2016).
Lismer, A. et al. Histone H3 lysine 4 trimethylation in sperm is transmitted to the embryo and associated with diet-induced phenotypes in the offspring. Dev. Cell 56, 1–16 (2021).
Hammoud, S. S. et al. Distinctive chromatin in human sperm packages genes for embryo development. Nature 460, 473–478 (2009).
Brykczynska, U. et al. Repressive and active histone methylation mark distinct promoters in human and mouse spermatozoa. Nat. Struct. Mol. Biol. 17, 679–687 (2010).
Lambrot, R. et al. Whole-genome sequencing of H3K4me3 and DNA methylation in human sperm reveals regions of overlap linked to fertility and development. Cell Rep. 36, 109418 (2021).
Ly, L. et al. Intergenerational impact of paternal lifetime exposures to both folic acid deficiency and supplementation on reproductive outcomes and imprinted gene methylation. Mol. Hum. Reprod. 23, 461–477 (2017).
Lambrot, R. et al. Low paternal dietary folate alters the mouse sperm epigenome and is associated with negative pregnancy outcomes. Nat. Commun. 4, 2889 (2013).
Sharma, U. et al. Biogenesis and function of tRNA fragments during sperm maturation and fertilization in mammals. Science 351, 391–396 (2016).
Yoshida, K. et al. ATF7-dependent epigenetic changes are required for the intergenerational effect of a paternal low-protein diet. Mol. Cell 78, 445–458 e446 (2020).
Watkins, A. J. et al. Paternal diet programs offspring health through sperm- and seminal plasma-specific pathways in mice. Proc. Natl Acad. Sci. USA 115, 10064–10069 (2018).
Terashima, M. et al. Effect of high fat diet on paternal sperm histone distribution and male offspring liver gene expression. Epigenetics 10, 861–871 (2015).
de Castro Barbosa, T. et al. High-fat diet reprograms the epigenome of rat spermatozoa and transgenerationally affects metabolism of the offspring. Mol. Metab. 5, 184–197 (2016).
Pepin, A. S., Lafleur, C., Lambrot, R., Dumeaux, V. & Kimmins, S. Sperm histone H3 lysine 4 tri-methylation serves as a metabolic sensor of paternal obesity and is associated with the inheritance of metabolic dysfunction. Mol. Metab. 59, 101463 (2022).
Rodgers, A. B., Morgan, C. P., Leu, N. A. & Bale, T. L. Transgenerational epigenetic programming via sperm microRNA recapitulates effects of paternal stress. Proc. Natl Acad. Sci. USA 112, 13699 (2015).
Beck, D., Ben Maamar, M. & Skinner, M. K. Integration of sperm ncRNA-directed DNA methylation and DNA methylation-directed histone retention in epigenetic transgenerational inheritance. Epigenetics Chromatin 14, 6 (2021).
Lismer, A., et al. Exposure of Greenlandic Inuit and South African VhaVenda men to the persistent DDT metabolite is associated with an altered sperm epigenome at regions implicated in paternal epigenetic transmission and developmental disease — a cross-sectional study. Preprint at bioRxiv https://doi.org/10.1101/2022.08.15.504029 (2022).
Amor, D. J. & Halliday, J. A review of known imprinting syndromes and their association with assisted reproduction technologies. Hum. Reprod. 23, 2826–2834 (2008).
Lazaraviciute, G., Kauser, M., Bhattacharya, S., Haggarty, P. & Bhattacharya, S. A systematic review and meta-analysis of DNA methylation levels and imprinting disorders in children conceived by IVF/ICSI compared with children conceived spontaneously. Hum. Reprod. Update 20, 840–852 (2014).
Novakovic, B. et al. Assisted reproductive technologies are associated with limited epigenetic variation at birth that largely resolves by adulthood. Nat. Commun. 10, 3922 (2019).
Chen, W. et al. Integrated multi-omics reveal epigenomic disturbance of assisted reproductive technologies in human offspring. EBioMedicine 61, 103076 (2020).
Katari, S. et al. DNA methylation and gene expression differences in children conceived in vitro or in vivo. Hum. Mol. Genet. 18, 3769–3778 (2009).
Katagiri, Y. et al. Effects of assisted reproduction technology on placental imprinted gene expression. Obstet Gynecol. Int. 2010, 437525, (2010).
Lou, H. et al. Assisted reproductive technologies impair the expression and methylation of insulin-induced gene 1 and sterol regulatory element-binding factor 1 in the fetus and placenta. Fertil. Steril. 101, 974–980.e972 (2014).
Loke, Y. J., Galati, J. C., Saffery, R. & Craig, J. M. Association of in vitro fertilization with global and IGF2/H19 methylation variation in newborn twins. J. Dev. Orig. Health Dis. 6, 115–124 (2015).
Sakian, S. et al. Altered gene expression of H19 and IGF2 in placentas from ART pregnancies. Placenta 36, 1100–1105 (2015).
Choux, C. et al. The epigenetic control of transposable elements and imprinted genes in newborns is affected by the mode of conception: ART versus spontaneous conception without underlying infertility. Hum. Reprod. 33, 331–340 (2018).
Tierling, S. et al. Assisted reproductive technologies do not enhance the variability of DNA methylation imprints in human. J. Med. Genet. 47, 371–376 (2010).
Zechner, U. et al. Quantitative methylation analysis of developmentally important genes in human pregnancy losses after ART and spontaneous conception. Mol. Hum. Reprod. 16, 704–713 (2010).
Li, L. et al. Evaluation of DNA methylation status at differentially methylated regions in IVF-conceived newborn twins. Fertil. Steril. 95, 1975–1979 (2011).
Feng, C. et al. General imprinting status is stable in assisted reproduction-conceived offspring. Fertil. Steril. 96, 1417–1423.e1419 (2011).
Oliver, V. F. et al. Defects in imprinting and genome-wide DNA methylation are not common in the in vitro fertilization population. Fertil. Steril. 97, 147–153.e147 (2012).
Rancourt, R. C., Harris, H. R. & Michels, K. B. Methylation levels at imprinting control regions are not altered with ovulation induction or in vitro fertilization in a birth cohort. Hum. Reprod. 27, 2208–2216 (2012).
Penova-Veselinovic, B. et al. DNA methylation patterns within whole blood of adolescents born from assisted reproductive technology are not different from adolescents born from natural conception. Hum. Reprod. 36, 2035–2049 (2021).
Litzky, J. F. et al. Placental imprinting variation associated with assisted reproductive technologies and subfertility. Epigenetics 12, 653–661 (2017).
Song, S. et al. DNA methylation differences between in vitro- and in vivo-conceived children are associated with ART procedures rather than infertility. Clin. Epigenetics 7, 41 (2015).
Hansen, M., Bower, C., Milne, E., de Klerk, N. & Kurinczuk, J. J. Assisted reproductive technologies and the risk of birth defects — a systematic review. Hum. Reprod. 20, 328–338 (2005).
Albertini, D. F. et al. Birth defects and congenital health risks in children conceived through assisted reproduction technology (ART): a meeting report. J. Assist. Reprod. Genet. 31, 947–958 (2014).
Hansen, M. & Bower, C. The impact of assisted reproductive technologies on intra-uterine growth and birth defects in singletons. Semin. Fetal Neonatal Med. 19, 228–233 (2014).
Qin, J. et al. Assisted reproductive technology and risk of congenital malformations: a meta-analysis based on cohort studies. Arch. Gynecol. Obstet. 292, 777–798 (2015).
Boulet, S. L. et al. Assisted reproductive technology and birth defects among liveborn infants in Florida, Massachusetts, and Michigan, 2000–2010. JAMA Pediatr. 170, e154934 (2016).
Palomba, S., Homburg, R., Santagni, S., La Sala, G. B. & Orvieto, R. Risk of adverse pregnancy and perinatal outcomes after high technology infertility treatment: a comprehensive systematic review. Reprod. Biol. Endocrinol. 14, 76 (2016).
Luke, B. et al. The risk of birth defects with conception by ART. Hum. Reprod. 36, 116–129 (2021).
Catford, S. R., McLachlan, R. I., O’Bryan, M. K. & Halliday, J. L. Long-term follow-up of ICSI-conceived offspring compared with spontaneously conceived offspring: a systematic review of health outcomes beyond the neonatal period. Andrology 6, 635–653 (2018).
Belva, F. et al. Semen quality of young adult ICSI offspring: the first results. Hum. Reprod. 31, 2811–2820 (2016).
Belva, F. et al. Reproductive hormones of ICSI-conceived young adult men: the first results. Hum. Reprod. 32, 439–446 (2017).
Catford, S. R. et al. Reproductive function in men conceived with in vitro fertilization and intracytoplasmic sperm injection. Fertil. Steril. 117, 727–737 (2022).
Belva, F. et al. Serum reproductive hormone levels and ultrasound findings in female offspring after intracytoplasmic sperm injection: first results. Fertil. Steril. 107, 934–939 (2017).
Guo, X. Y. et al. Cardiovascular and metabolic profiles of offspring conceived by assisted reproductive technologies: a systematic review and meta-analysis. Fertil. Steril. 107, 622–631.e5 (2017).
Belva, F. et al. Body fat content, fat distribution and adipocytokine production and their correlation with fertility markers in young adult men and women conceived by intracytoplasmic sperm injection (ICSI). Clin. Endocrinol. 88, 985–992 (2018)
Belva, F. et al. Metabolic syndrome and its components in young adults conceived by ICSI. Int. J. Endocrinol. 2018, 8170518 (2018).
Zhu, J. L., Basso, O., Obel, C., Hvidtjorn, D. & Olsen, J. Infertility, infertility treatment and psychomotor development: the Danish National Birth Cohort. Paediatr. Perinat. Epidemiol. 23, 98–106 (2009).
Diop, H. et al. Early autism spectrum disorders in children born to fertile, subfertile, and ART-treated women. Matern. Child. Health J. 23, 1489–1499 (2019).
Hargreave, M. et al. Association between fertility treatment and cancer risk in children. JAMA 322, 2203–2210 (2019).
Schendelaar, P. et al. Increased time to pregnancy is associated with less optimal neurological condition in 4-year-old singletons, in vitro fertilization itself is not. Hum. Reprod. 29, 2773–2786 (2014).
Jenkins, T. G., Liu, L., Aston, K. I. & Carrell, D. T. Pre-screening method for somatic cell contamination in human sperm epigenetic studies. Syst. Biol. Reprod. Med. 64, 146–155 (2018).
Leitao, E. et al. The sperm epigenome does not display recurrent epimutations in patients with severely impaired spermatogenesis. Clin. Epigenetics 12, 61 (2020).
Asenius, F., Danson, A. F. & Marzi, S. J. DNA methylation in human sperm: a systematic review. Hum. Reprod. Update 26, 841–873 (2020).
Economidis, M. A. & Mishell, D. R. Jr. Pharmacological female contraception: an overview of past and future use. Expert. Opin. Investig. Drugs 14, 449–456 (2005).
Thirumalai, A. & Amory, J. K. Emerging approaches to male contraception. Fertil. Steril. 115, 1369–1376 (2021).
Reynolds-Wright, J. J., Cameron, N. J. & Anderson, R. A. Will men use novel male contraceptive methods and will women trust them? A systematic review. Ann. Rev. Sex. Res. 58, 838–849 (2021).
World Health Organisation Task Force on Methods for the Regulation of Male Fertility. Contraceptive efficacy of testosterone-induced azoospermia and oligozoospermia in normal men. Fertil. Steril. 65, 821–829 (1996).
Behre, H. M. et al. Efficacy and safety of an injectable combination hormonal contraceptive for men. J. Clin. Endocrinol. Metab. 101, 4779–4788 (2016).
Long, J. E., Lee, M. S. & Blithe, D. L. Update on novel hormonal and nonhormonal male contraceptive development. J. Clin. Endocrinol. Metab. 106, e2381–e2392 (2021).
Mommers, E. et al. Male hormonal contraception: a double-blind, placebo-controlled study. J. Clin. Endocrinol. Metab. 93, 2572–2580 (2008).
North, B. B. et al. Evaluation of the novel vaginal contraceptive agent PPCM in preclinical studies using sperm hyaluronan binding and acrosome status assays. Andrology 10, 367–376 (2021).
Noman, M. A. A., Kyzer, J. L., Chung, S. S. W., Wolgemuth, D. J. & Georg, G. I. Retinoic acid receptor antagonists for male contraception: current status. Biol. Reprod. 103, 390–399 (2020).
Male Contraceptive Initiative. The Drug Development Pipeline. MCI https://www.malecontraceptive.org/the-drug-development-pipeline.html (2023).
Gruber, F. S., Johnston, Z. C., Barratt, C. L. & Andrews, P. D. A phenotypic screening platform utilising human spermatozoa identifies compounds with contraceptive activity. Elife 9, e51739 (2020).
Chamberlain, S. G. et al. Reboot contraceptives research — it has been stuck for decades. Nature 587, 543–545 (2020).
Hinton, L. & Miller, T. Mapping men’s anticipations and experiences in the reproductive realm: (in)fertility journeys. Reprod. Biomed. Online 27, 244–252 (2013).
Mossman, J. A. & Pacey, A. A. The fertility fitness paradox of anabolic-androgenic steroid abuse in men. J. Intern. Med. 286, 231–232 (2019).
Practice Committee of the American Society for Reproductive Medicine. Smoking and infertility: a committee opinion. Fertil. Steril. 110, 611–618 (2018).
Healthy Male. Engaging Men in Primary Health Care. Healthy Male https://www.healthymale.org.au/health-professionals/engaging-men-primary-health-care (2023).
Smith, J. A., Braunack-Mayer, A., Wittert, G. & Warin, M. “It’s sort of like being a detective”: understanding how Australian men self-monitor their health prior to seeking help. BMC Health Serv. Res. 8, 56 (2008).
Pearson, L., Holton, S., McLachlan, R. & Hammarberg, K. Australian men’s fertility information seeking attitudes and behaviour: a qualitative investigation. Sex. Reprod. Healthc. 29, 100621 (2021).
Stevenson, E. L. & McEleny, K. R. Male subfertility as a chronic illness: the role of adaptive challenges. Hum. Fertil. 20, 148–154 (2017).
Hadley, R. & Hanley, T. Involuntarily childless men and the desire for fatherhood. J. Reprod. Infant. Psychol. 29, 56–68 (2011).
Hammarberg, K., Collins, V., Holden, C., Young, K. & McLachlan, R. Men’s knowledge, attitudes and behaviours relating to fertility. Hum. Reprod. Update 23, 458–480 (2017).
Sørensen, N. O. et al. Fertility awareness and attitudes towards parenthood among Danish university college students. Reprod. Health 13, 146 (2016).
Prior, E., Lew, R., Hammarberg, K. & Johnson, L. Fertility facts, figures and future plans: an online survey of university students. Hum. Fertil. 22, 283–290 (2019).
De Jonge, C. J., Gellatly, S. A., Vazquez-Levin, M. H., Barratt, C. L. R. & Rautakallio-Hokkanen, S. Male attitudes towards infertility: results from a global questionnaire. World J. Mens. Health 41, 204–214 (2022).
Pedro, J., Brandão, T., Schmidt, L., Costa, M. E. & Martins, M. V. What do people know about fertility? A systematic review on fertility awareness and its associated factors. Ups. J. Med. Sci. 123, 71–81 (2018).
Daumler, D., Chan, P., Lo, K. C., Takefman, J. & Zelkowitz, P. Men’s knowledge of their own fertility: a population-based survey examining the awareness of factors that are associated with male infertility. Hum. Reprod. 31, 2781–2790 (2016).
Victoria State Government Department of Health. Infertility in women. Victoria State Government https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/infertility-in-women (2021).
Daniluk, J. C. & Koert, E. Fertility awareness online: the efficacy of a fertility education website in increasing knowledge and changing fertility beliefs. Hum. Reprod. 30, 353–363 (2015).
Goodyear, V. & Quennerstedt, M. #Gymlad — young boys learning processes and health-related social media. Qual. Res. Sport. Exerc. Health 12, 18–33 (2020).
Sangster, S. L. & Lawson, K. L. Is any press good press? the impact of media portrayals of infertility on young adults’ perceptions of infertility. J. Obstet. Gynaecol. Can. 37, 1072–1078 (2015).
Berthelsen, A. S. N., Gamby, A. L. N., Christensen, U., Schmidt, L. & Koert, E. How do young men want to receive information about fertility? Young men’s attitudes towards a fertility campaign targeting men in Copenhagen, Denmark. Hum. Reprod. Open. 2021, hoab027 (2021).
Goldfarb, E. S. & Lieberman, L. D. Three decades of research: the case for comprehensive sex education. J. Adolesc. Health 68, 13–27 (2021).
Warner, J. N. & Frey, K. A. The well-man visit: addressing a man’s health to optimize pregnancy outcomes. J. Am. Board. Fam. Med. 26, 196–202 (2013).
Choiriyyah, I. et al. Men aged 15–44 in need of preconception care. Matern. Child. Health J. 19, 2358–2365 (2015).
Bodin, M., Tydén, T., Käll, L. & Larsson, M. Can reproductive life plan-based counselling increase men’s fertility awareness? Ups. J. Med. Sci. 123, 255–263 (2018).
Grau Grau, M. & Riley Bowles, H. in Engaged Fatherhood for Men, Families and Gender Equality: Healthcare, Social Policy, and Work Perspectives (eds Grau Grau, M, las Heras Maestro, M. & Bowles, H. R.) 1–12 (Springer International Publishing, 2022).
Hogg, K., Rizio, T., Manocha, R., McLachlan, R. I. & Hammarberg, K. Men’s preconception health care in Australian general practice: GPs’ knowledge, attitudes and behaviours. Aust. J. Prim. Health 25, 353–358 (2019).
Barnes, L. W. Conceiving Masculinity. Male Infertility, Medicine, and Identity (Temple University Press, 2014).
WHO. Laboratory Manual for the examination of human semen and sperm-cervical mucus interaction (Cambridge University Press, 1999).
WHO. WHO laboratory manual for the examination and processing of human semen 5th edn (World Health Organization, 2010).
Rodprasert, W. et al. An update on semen quality among young Finnish men and comparison with Danish data. Andrology 7, 15–23 (2019).
Jorgensen, N. et al. Recent adverse trends in semen quality and testis cancer incidence among Finnish men. Int. J. Androl. 34, e37–e48 (2011).
Jorgensen, N. et al. Human semen quality in the new millennium: a prospective cross-sectional population-based study of 4867 men. BMJ Open 2, e000990 (2012).
Gyllenborg, J. et al. Secular and seasonal changes in semen quality among young Danish men: a statistical analysis of semen samples from 1927 donor candidates during 1977-1995. Int. J. Androl. 22, 28–36 (1999).
Huang, C. et al. Decline in semen quality among 30,636 young Chinese men from 2001 to 2015. Fertil. Steril. 107, 83–88.e2 (2017).
Rao, M. et al. Evaluation of semen quality in 1808 university students, from Wuhan, Central China. Asian J. Androl. 17, 111–116 (2015).
Zou, Z. et al. Semen quality analysis of military personnel from six geographical areas of the People’s Republic of China. Fertil. Steril. 95, 2018–2023.e3 (2011).
Li, Y. et al. Semen quality of 1346 healthy men, results from the Chongqing area of southwest China. Hum. Reprod. 24, 459–69 (2009).
Junqing, W. et al. Reference value of semen quality in Chinese young men. Contraception 65, 365–368 (2002).
Gao, J. et al. Semen quality in a residential, geographic and age representative sample of healthy Chinese men. Hum. Reprod. 22, 477–484 (2007).
Wang, C. et al. Cross-sectional study of semen parameters in a large group of normal Chinese men. Int. J. Androl. 8, 257–274 (1985).
Itoh, N. et al. Have sperm counts deteriorated over the past 20 years in healthy, young Japanese men? Results from the Sapporo area. J. Androl. 22, 40–44 (2001).
Medras, M. et al. The quality of semen among a sample of young, healthy men from Lower Silesia (AndroLS). Endokrynol. Pol. 68, 668–675 (2017).
Rahban, R. et al. Semen quality of young men in Switzerland: a nationwide cross-sectional population-based study. Andrology 7, 818–826 (2019).
Lopez-Teijon, M., Elbaile, M. & Alvarez, J. G. Geographical differences in semen quality in a population of young healthy volunteers from the different regions of Spain. Andrologia 40, 318–328 (2008).
Mendiola, J. et al. Reproductive parameters in young men living in Rochester, New York. Fertil. Steril. 101, 1064–1071 (2014).
Levine, R. J. et al. Air-conditioned environments do not prevent deterioration of human semen quality during the summer. Fertil. Steril. 57, 1075–1083 (1992).
Uhler, M. L. et al. Relationship between sperm characteristics and hormonal parameters in normal couples. Fertil. Steril. 79 (Suppl. 3), 1535–1542 (2003).
Selevan, S. G. et al. Semen quality and reproductive health of young Czech men exposed to seasonal air pollution. Environ. Health Perspect. 108, 887–894 (2000).
Sheriff, D. S. & Legnain, M. Evaluation of semen quality in a local Libyan population. Indian J. Physiol. Pharmacol. 36, 83–87 (1992).
Shine, R., Peek, J. & Birdsall, M. Declining sperm quality in New Zealand over 20 years. N. Z. Med. J. 121, 50–56 (2008).
Hadjkacem Loukil, L. et al. Relation between male obesity and male infertility in a Tunisian population. Andrologia 47, 282–285 (2015).
Acknowledgements
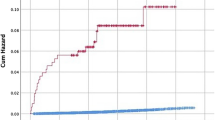
Thanks goes to R. Agnew, E. Heighton and A. Mergo from The University of Dundee for their assistance with data collection for Fig. 1. Thanks also goes to A. O’Connor from the University of Melbourne for assistance with referencing. This research was supported in part by funding by the National Health and Medical Research Council of Australia to M.K.O., R.I.M. and J.A.V. (APP1120356); S.K. is a Canada Research Chair in Epigenomics, Reproduction and Development and funding for this study is provided by the Canada Research Chairs program, and the Canadian Institutes of Health Research grants (DOHaD Team grant 358654 and Operating grant 350129). The authors thank ESHRE for financial and logistical support of the MRHI.
Author information
Authors and Affiliations
Contributions
All authors researched data for the article. S.K., R.A.A., C.L.R.B., C.J.D.J. and M.K.O. contributed substantially to discussion of the content. All authors wrote the article. S.K., R.A.A., C.L.R.B., H.M.B., S.R.C., C.J.D.J., G.D., M.L.E., N.G., N.J., C.K., A.L., R.I.M., S.M., T.M., A.P., L.P., S.S., J.T., L.T., F.T., M.H.V.-L., J.A.V., F.Z. and M.K.O. reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
C.L.R.B. is supported in part by the Bill and Melinda Gates Foundation in the area of contraceptive development, Chief Scientist Office (Scotland), NHS and Genus Healthcare. C.L.R.B. has received fees from Cooper Surgical for lectures on scientific research methods outside the submitted work and Ferring for a lecture on the future of male reproductive health. M.L.E. is an adviser to Ro, Doveras, VSeat, and Next. R.A.A. reports grants and personal fees from Roche Diagnostics, personal fees from Ferring Pharmaceuticals, IBSA, Merck Serono, outside the submitted work. S.K. is an inventor on a Provisional patent 14647-P68337CA00 10 June 2022: Methods for identifying epigenetic modifications in sperm, diagnosing infertility, and identifying treatment strategies. A.P. has undertaken paid consultancy for Cryos International, Cytoswim Ltd, Exceed Health, Meals Group, and Merck Serono in the last 2 years, but all monies have been paid to the University of Sheffield (former employer). M.K.O. is supported in part by the Bill and Melinda Gates Foundation in the area of contraceptive development. All other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Urology thanks Marco Alves and Gerhard Haidl for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Australian Male Infertility Exposure Study: http://www.mcri.edu.au/research/projects/australian-male-infertility-exposure-amie-study
European Society of Human Reproduction and Embryology: http://www.eshre.eu/Specialty-groups/Special-Interest-Groups/Andrology/MRHI
Family Planning 2030: https://fp2030.org/
Male Contraceptive Initiative: http://www.malecontraceptive.org
NordFertil: https://nordfertil.org
United Nations Sustainable Development Goals 3 and 5: https://sdgs.un.org/goals
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kimmins, S., Anderson, R.A., Barratt, C.L.R. et al. Frequency, morbidity and equity — the case for increased research on male fertility. Nat Rev Urol 21, 102–124 (2024). https://doi.org/10.1038/s41585-023-00820-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41585-023-00820-4
This article is cited by
-
Focusing on male infertility
Nature Reviews Urology (2024)