Abstract
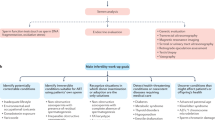
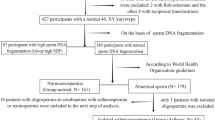
Clinical infertility is the inability of a couple to conceive after 12 months of trying. Male factors are estimated to contribute to 30–50% of cases of infertility. Infertility or reduced fertility can result from testicular dysfunction, endocrinopathies, lifestyle factors (such as tobacco and obesity), congenital anatomical factors, gonadotoxic exposures and ageing, among others. The evaluation of male infertility includes detailed history taking, focused physical examination and selective laboratory testing, including semen analysis. Treatments include lifestyle optimization, empirical or targeted medical therapy as well as surgical therapies that lead to measurable improvement in fertility. Although male infertility is recognized as a disease with effects on quality of life for both members of the infertile couple, fewer data exist on specific quantification and impact compared with other health-related conditions.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$99.00 per year
only $99.00 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
WHO TEAM: Sexual and Reproductive Health and Research. Infertility Prevalence Estimates, 1990–2021 (WHO, 2023).
Practice Committee of the American Society for Reproductive Medicine. Fertility evaluation of infertile women: a committee opinion. Fertil. Steril. 116, 1255–1265 (2021).
Schlegel, P. N. et al. Diagnosis and treatment of infertility in men: AUA/ASRM guideline part I. Fertil. Steril. 115, 54–61 (2021).
Thonneau, P. et al. Incidence and main causes of infertility in a resident population (1,850,000) of three French regions (1988–1989). Hum. Reprod. 6, 811–816 (1991).
Agarwal, A., Mulgund, A., Hamada, A. & Chyatte, M. R. A unique view on male infertility around the globe. Reprod. Biol. Endocrinol. 13, 37 (2015).
Samplaski, M. K. et al. Reproductive endocrinologists are the gatekeepers for male infertility care in North America: results of a North American survey on the referral patterns and characteristics of men presenting to male infertility specialists for infertility investigations. Fertil. Steril. 112, 657–662 (2019).
Eisenberg, M. L., Lathi, R. B., Baker, V. L., Westphal, L. M., Milki, A. A. & Nangia, A. K. Frequency of the male infertility evaluation: data from the national survey of family growth. J. Urol. 189, 1030–1034 (2013).
Bonde, J. P. et al. Relation between semen quality and fertility: a population-based study of 430 first-pregnancy planners. Lancet 352, 1172–1177 (1998).
Zinaman, M. J., Brown, C. C., Selevan, S. G. & Clegg, E. D. Semen quality and human fertility: a prospective study with healthy couples. J. Androl. 21, 145–153 (2000).
Guzick, D. S. et al. Sperm morphology, motility, and concentration in fertile and infertile men. N. Engl. J. Med. 345, 1388–1393 (2001).
Buck Louis, G. M. et al. Semen quality and time to pregnancy: the Longitudinal Investigation of Fertility and the Environment Study. Fertil. Steril. 101, 453–462 (2014).
Jedrzejczak, P., Taszarek-Hauke, G., Hauke, J., Pawelczyk, L. & Duleba, A. J. Prediction of spontaneous conception based on semen parameters. Int. J. Androl. 31, 499–507 (2008).
Minhas, S. et al. European Association of Urology Guidelines on Male Sexual and Reproductive Health: 2021 Update on Male Infertility. Eur. Urol. 80, 603–620 (2021).
World Health Organization. WHO Laboratory Manual for the Examination and Processing of Human Semen 6th edn (WHO, 2021).
Wang, C. et al. Evolution of the WHO “Semen” processing manual from the first (1980) to the sixth edition (2021). Fertil. Steril. 117, 237–245 (2022).
Bjorndahl, L. et al. The sixth edition of the WHO Laboratory Manual for the Examination and Processing of Human Semen: ensuring quality and standardization in basic examination of human ejaculates. Fertil. Steril. 117, 246–251 (2022).
Bjorndahl, L. et al. Standards in semen examination: publishing reproducible and reliable data based on high-quality methodology. Hum. Reprod. 37, 2497–2502 (2022).
Barratt, C. L. R. et al. What advances may the future bring to the diagnosis, treatment, and care of male sexual and reproductive health? Fertil. Steril. 117, 258–267 (2022).
Vasconcelos, A., Henedi, Z. & Barratt, C. L. R. WHO 2021 and 2030 reference values for semen assessment: three challenges for andrology in the journey ahead. Reprod. Biomed. Online 45, 187–190 (2022).
Vasconcelos, A. L., Campbell, M. J., Barratt, C. L. R. & Gellatly, S. A. Do studies published in two leading reproduction journals between 2011 and 2020 demonstrate that they followed WHO5 recommendations for basic semen analysis? Hum. Reprod. 37, 2255–2263 (2022).
Kruger, T. F., Acosta, A. A., Simmons, K. F., Swanson, R. J., Matta, J. F. & Oehninger, S. Predictive value of abnormal sperm morphology in in vitro fertilization. Fertil. Steril. 49, 112–117 (1988).
Lamb, D. J. Semen analysis in 21st century medicine: the need for sperm function testing. Asian J. Androl. 12, 64–70 (2010).
Silber, S. J. The relationship of abnormal semen parameters to male fertility. Hum. Reprod. 4, 947–953 (1989).
Sokol, R. Z. & Sparkes, R. Demonstrated paternity in spite of severe idiopathic oligospermia. Fertil. Steril. 47, 356–358 (1987).
Burris, A. S., Clark, R. V., Vantman, D. J. & Sherins, R. J. A low sperm concentration does not preclude fertility in men with isolated hypogonadotropic hypogonadism after gonadotropin therapy. Fertil. Steril. 50, 343–347 (1988).
Kruger, T. F. et al. Sperm morphologic features as a prognostic factor in in vitro fertilization. Fertil. Steril. 46, 1118–1123 (1986).
Katz, D. F., Overstreet, J. W., Samuels, S. J., Niswander, P. W., Bloom, T. D. & Lewis, E. L. Morphometric analysis of spermatozoa in the assessment of human male fertility. J. Androl. 7, 203–210 (1986).
Bostofte, E., Serup, J. & Rebbe, H. Relation between morphologically abnormal spermatozoa and pregnancies obtained during a twenty-year follow-up period. Int. J. Androl. 5, 379–386 (1982).
Aitken, R. J., Best, F. S., Warner, P. & Templeton, A. A prospective study of the relationship between semen quality and fertility in cases of unexplained infertility. J. Androl. 5, 297–303 (1984).
Bartoov, B., Eltes, F., Pansky, M., Lederman, H., Caspi, E. & Soffer, Y. Estimating fertility potential via semen analysis data. Hum. Reprod. 8, 65–70 (1993).
Stahl, P. J., Stember, D. S. & Schlegel, P. N. Interpretation of the semen analysis and initial male factor management. Clin. Obstet. Gynecol. 54, 656–665 (2011).
Mascarenhas, M. N., Flaxman, S. R., Boerma, T., Vanderpoel, S. & Stevens, G. A. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. 9, e1001356 (2012).
Andrade, D. L., Viana, M. C. & Esteves, S. C. Differential diagnosis of azoospermia in men with infertility. J. Clin. Med. 10, 3144 (2021).
Esteves, S. C. Who cares about oligozoospermia when we have ICSI. Reprod. Biomed. Online 44, 769–775 (2022).
Esteves, S. C., Miyaoka, R. & Agarwal, A. An update on the clinical assessment of the infertile male [corrected]. Clinics 66, 691–700 (2011).
Esteves, S. C., Santi, D. & Simoni, M. An update on clinical and surgical interventions to reduce sperm DNA fragmentation in infertile men. Andrology 8, 53–81 (2020).
Fraietta, R., Zylberstejn, D. S. & Esteves, S. C. Hypogonadotropic hypogonadism revisited. Clinics 68, 81–88 (2013).
Gunes, S. & Esteves, S. C. Role of genetics and epigenetics in male infertility. Andrologia 53, e13586 (2021).
Hamada, A. J., Esteves, S. C. & Agarwal, A. A comprehensive review of genetics and genetic testing in azoospermia. Clinics 68, 39–60 (2013).
Jensen, C. F. S., Østergren, P., Dupree, J. M., Ohl, D. A., Sønksen, J. & Fode, M. Varicocele and male infertility. Nat. Rev. Urol. 14, 523–533 (2017).
Teixeira, T. A. et al. Viral infections and implications for male reproductive health. Asian J. Androl. 23, 335–347 (2021).
World Health Organization. Infections, pregnancies, and infertility: perspectives on prevention. Fertil. Steril. 47, 964–968 (1987).
Polis, C. B., Cox, C. M., Tunçalp, Ö., McLain, A. C. & Thoma, M. E. Estimating infertility prevalence in low-to-middle-income countries: an application of a current duration approach to demographic and health survey data. Hum. Reprod. 32, 1064–1074 (2017).
Khandwala, Y. S., Zhang, C. A., Lu, Y. & Eisenberg, M. L. The age of fathers in the USA is rising: an analysis of 168 867 480 births from 1972 to 2015. Hum. Reprod. 32, 2110–2116 (2017).
Bertoncelli Tanaka, M., Agarwal, A. & Esteves, S. C. Paternal age and assisted reproductive technology: problem solver or trouble maker? Panminerva Med. 61, 138–151 (2019).
Esteves, S. C., Carvalho, J. F., Bento, F. C. & Santos, J. A novel predictive model to estimate the number of mature oocytes required for obtaining at least one euploid blastocyst for transfer in couples undergoing in vitro fertilization/intracytoplasmic sperm injection: the ART calculator. Front. Endocrinol. 10, 99 (2019).
Esteves, S. C. et al. Cumulative delivery rate per aspiration IVF/ICSI cycle in POSEIDON patients: a real-world evidence study of 9073 patients. Hum. Reprod. 36, 2157–2169 (2021).
Fauser, B. C. Towards the global coverage of a unified registry of IVF outcomes. Reprod. Biomed. Online 38, 133–137 (2019).
Chambers, G. M. et al. International Committee for Monitoring Assisted Reproductive Technologies World Report: Assisted Reproductive Technology, 2014. Hum. Reprod. 36, 2921–2934 (2021).
Sunderam, S. et al. Assisted Reproductive Technology Surveillance – United States, 2018. MMWR Surveill. Summ. 71, 1–19 (2022).
Dyer, S. et al. International Committee for Monitoring Assisted Reproductive Technologies World Report: Assisted Reproductive Technology 2008, 2009 and 2010. Hum. Reprod. 31, 1588–1609 (2016).
Boulet, S. L., Mehta, A., Kissin, D. M., Warner, L., Kawwass, J. F. & Jamieson, D. J. Trends in use of and reproductive outcomes associated with intracytoplasmic sperm injection. JAMA 313, 255–263 (2015).
Wyn, C. et al. ART in Europe, 2018: results generated from European registries by ESHRE. Hum. Reprod. Open 2022, hoac022 (2022).
Esteves, S. C., Roque, M., Bedoschi, G., Haahr, T. & Humaidan, P. Intracytoplasmic sperm injection for male infertility and consequences for offspring. Nat. Rev. Urol. 15, 535–562 (2018).
Jewett, A. et al. Assisted reproductive technology cycles involving male factor infertility in the United States, 2017-2018: data from the National Assisted Reproductive Technology Surveillance System. FS Rep. 3, 124–130 (2022).
Buttorff, C., Ruder, T. & Bauman, M. Multiple Chronic Conditions in the United States (Rand, 2017).
Chen, T., Belladelli, F., Del Giudice, F. & Eisenberg, M. L. Male fertility as a marker for health. Reprod. Biomed. Online 44, 131–144 (2022).
Eisenberg, M. L., Li, S., Brooks, J. D., Cullen, M. R. & Baker, L. C. Increased risk of cancer in infertile men: analysis of U.S. claims data. J. Urol. 193, 1596–1601 (2015).
Faja, F. et al. Environmental disruptors and testicular cancer. Endocrine 78, 429–435 (2022).
Brubaker, W. D., Li, S., Baker, L. C. & Eisenberg, M. L. Increased risk of autoimmune disorders in infertile men: analysis of US claims data. Andrology 6, 94–98 (2018).
Del Giudice, F. et al. The association between mortality and male infertility: systematic review and meta-analysis. Urology 154, 148–157 (2021).
Del Giudice, F. et al. Increased mortality among men diagnosed with impaired fertility: analysis of US claims data. Urology 147, 143–149 (2021).
Dohle, G. R. Male infertility in cancer patients: review of the literature. Int. J. Urol. 17, 327–331 (2010).
Glazer, C. H. et al. Male factor infertility and risk of multiple sclerosis: a register-based cohort study. Mult. Scler. 24, 1835–1842 (2018).
Gunnes, M. W. et al. Reproduction and marriage among male survivors of cancer in childhood, adolescence and young adulthood: a national cohort study. Br. J. Cancer 114, 348–356 (2016).
Kohn, T. P., Kohn, J. R., Owen, R. C. & Coward, R. M. The prevalence of Y-chromosome microdeletions in oligozoospermic men: a systematic review and meta-analysis of European and North American studies. Eur. Urol. 76, 626–636 (2019).
Peña, V. N., Kohn, T. P. & Herati, A. S. Genetic mutations contributing to non-obstructive azoospermia. Best Pract. Res. Clin. Endocrinol. Metab. 34, 101479 (2020).
Liu, J. L., Peña, V., Fletcher, S. A. & Kohn, T. P. Genetic testing in male infertility – reassessing screening thresholds. Curr. Opin. Urol. 30, 317–323 (2020).
Kurinczuk, J. J. & Bhattacharya, S. Rare chromosomal, genetic, and epigenetic-related risks associated with infertility treatment. Semin. Fetal Neonatal Med. 19, 250–253 (2014).
Pinho, A., Barros, A. & Fernandes, S. Clinical and molecular characterization of Y microdeletions and X-linked CNV67 implications in male fertility: a 20-year experience. Andrology 8, 307–314 (2020).
Liu, X. G., Hu, H. Y., Guo, Y. H. & Sun, Y. P. Correlation between Y chromosome microdeletion and male infertility. Genet. Mol. Res. 15, gmr.15028426 (2016).
Bianco, S. D. & Kaiser, U. B. The genetic and molecular basis of idiopathic hypogonadotropic hypogonadism. Nat. Rev. Endocrinol. 5, 569–576 (2009).
Lee, P. A., O’Leary, L. A., Songer, N. J., Coughlin, M. T., Bellinger, M. F. & LaPorte, R. E. Paternity after bilateral cryptorchidism. A controlled study. Arch. Pediatr. Adolesc. Med. 151, 260–263 (1997).
Trsinar, B. & Muravec, U. R. Fertility potential after unilateral and bilateral orchidopexy for cryptorchidism. World J. Urol. 27, 513–519 (2009).
Mak, V. et al. Proportion of cystic fibrosis gene mutations not detected by routine testing in men with obstructive azoospermia. JAMA 281, 2217–2224 (1999).
Cai, Z. & Li, H. Congenital bilateral absence of the vas deferens. Front. Genet. 13, 775123 (2022).
Yu, J., Chen, Z., Ni, Y. & Li, Z. CFTR mutations in men with congenital bilateral absence of the vas deferens (CBAVD): a systemic review and meta-analysis. Hum. Reprod. 27, 25–35 (2012).
Sharma, H., Mavuduru, R. S., Singh, S. K. & Prasad, R. Increased frequency of CFTR gene mutations identified in Indian infertile men with non-CBAVD obstructive azoospermia and spermatogenic failure. Gene 548, 43–47 (2014).
Siwen, W., Wang, L. & Cheng, C. Y. in Infertility in the Male 5th Edn (eds Lipshultz, L. I., Howards, S. S., Niederberger, C. S. & Lamb, D. J.) Ch. 2 (Cambridge Univ. Press, 2023).
Schlegel, P. N. et al. Diagnosis and treatment of infertility in men: AUA/ASRM guideline part II. Fertil. Steril. 115, 62–69 (2021).
Mayerhofer, A. Peritubular cells of the human testis: prostaglandin E(2) and more. Andrology 8, 898–902 (2020).
Ruthig, V. A. & Lamb, D. J. Updates in Sertoli cell-mediated signaling during spermatogenesis and advances in restoring Sertoli cell function. Front. Endocrinol. 13, 897196 (2022).
Liebich, A. et al. The molecular signature of human testicular peritubular cells revealed by single-cell analysis. Cells 11, 3685 (2022).
Mayerhofer, A. Human testicular peritubular cells: more than meets the eye. Reproduction 145, R107–R116 (2013).
Brinster, R. L. & Zimmermann, J. W. Spermatogenesis following male germ-cell transplantation. Proc. Natl Acad. Sci. USA 91, 11298–11302 (1994).
Guan, K. et al. Pluripotency of spermatogonial stem cells from adult mouse testis. Nature 440, 1199–1203 (2006).
Abid, S. N. et al. A-single spermatogonia heterogeneity and cell cycles synchronize with rat seminiferous epithelium stages VIII–IX. Biol. Reprod. 90, 32 (2014).
Griswold, M. D. Spermatogenesis: the commitment to meiosis. Physiol. Rev. 96, 1–17 (2016).
Heller, C. G. & Clermont, Y. Spermatogenesis in man: an estimate of its duration. Science 140, 184–186 (1963).
Clermont, Y. The cycle of the seminiferous epithelium in man. Am. J. Anat. 112, 35–51 (1963).
Dohle, G. R., Smit, M. & Weber, R. F. Androgens and male fertility. World J. Urol. 21, 341–345 (2003).
Khodamoradi, K., Parmar, M., Khosravizadeh, Z., Kuchakulla, M., Manoharan, M. & Arora, H. The role of leptin and obesity on male infertility. Curr. Opin. Urol. 30, 334–339 (2020).
Coviello, A. D. et al. Low-dose human chorionic gonadotropin maintains intratesticular testosterone in normal men with testosterone-induced gonadotropin suppression. J. Clin. Endocrinol. Metab. 90, 2595–2602 (2005).
Jarow, J. P., Chen, H., Rosner, T. W., Trentacoste, S. & Zirkin, B. R. Assessment of the androgen environment within the human testis: minimally invasive method to obtain intratesticular fluid. J. Androl. 22, 640–645 (2001).
Rahnema, C. D., Lipshultz, L. I., Crosnoe, L. E., Kovac, J. R. & Kim, E. D. Anabolic steroid-induced hypogonadism: diagnosis and treatment. Fertil. Steril. 101, 1271–1279 (2014).
Meachem, S. J., Nieschlag, E. & Simoni, M. Inhibin B in male reproduction: pathophysiology and clinical relevance. Eur. J. Endocrinol. 145, 561–571 (2001).
Tsatsanis, C., Dermitzaki, E., Avgoustinaki, P., Malliaraki, N., Mytaras, V. & Margioris, A. N. The impact of adipose tissue-derived factors on the hypothalamic–pituitary–gonadal (HPG) axis. Hormones 14, 549–562 (2015).
Hammoud, A. O., Gibson, M., Peterson, C. M., Meikle, A. W. & Carrell, D. T. Impact of male obesity on infertility: a critical review of the current literature. Fertil. Steril. 90, 897–904 (2008).
Liu, P. Y., Swerdloff, R. S., Christenson, P. D., Handelsman, D. J. & Wang, C. Rate, extent, and modifiers of spermatogenic recovery after hormonal male contraception: an integrated analysis. Lancet 367, 1412–1420 (2006).
Kohn, T. P. et al. Age and duration of testosterone therapy predict time to return of sperm count after human chorionic gonadotropin therapy. Fertil. Steril. 107, 351–357 e351 (2017).
Gu, Y. et al. Multicenter contraceptive efficacy trial of injectable testosterone undecanoate in Chinese men. J. Clin. Endocrinol. Metab. 94, 1910–1915 (2009).
Ly, L. P., Liu, P. Y. & Handelsman, D. J. Rates of suppression and recovery of human sperm output in testosterone-based hormonal contraceptive regimens. Hum. Reprod. 20, 1733–1740 (2005).
Meistrich, M. L. Effects of chemotherapy and radiotherapy on spermatogenesis in humans. Fertil. Steril. 100, 1180–1186 (2013).
Nicholson, H. S. & Byrne, J. Fertility and pregnancy after treatment for cancer during childhood or adolescence. Cancer 71, 3392–3399 (1993).
Stahl, O. et al. Sperm DNA integrity in testicular cancer patients. Hum. Reprod. 21, 3199–3205 (2006).
Harman, S. M., Metter, E. J., Tobin, J. D., Pearson, J. & Blackman, M. R. Longitudinal effects of aging on serum total and free testosterone levels in healthy men. Baltimore Longitudinal Study of Aging. J. Clin. Endocrinol. Metab. 86, 724–731 (2001).
Frattarelli, J. L., Miller, K. A., Miller, B. T., Elkind-Hirsch, K. & Scott, R. T. Jr. Male age negatively impacts embryo development and reproductive outcome in donor oocyte assisted reproductive technology cycles. Fertil. Steril. 90, 97–103 (2008).
Wyrobek, A. J. et al. Advancing age has differential effects on DNA damage, chromatin integrity, gene mutations, and aneuploidies in sperm. Proc. Natl Acad. Sci. USA 103, 9601–9606 (2006).
Brandt, J. S., Cruz Ithier, M. A., Rosen, T. & Ashkinadze, E. Advanced paternal age, infertility, and reproductive risks: a review of the literature. Prenat. Diagn. 39, 81–87 (2019).
Penrose, L. S. Parental age and mutation. Lancet 269, 312–313 (1955).
Krooth, R. S. Comments on the estimation of the mutation rate for achondroplasia. Am. J. Hum. Genet. 5, 373–376 (1953).
Lorentz, C. P., Wieben, E. D., Tefferi, A., Whiteman, D. A. & Dewald, G. W. Primer on medical genomics part I: History of genetics and sequencing of the human genome. Mayo Clin. Proc. 77, 773–782 (2002).
Francioli, L. C. et al. Genome-wide patterns and properties of de novo mutations in humans. Nat. Genet. 47, 822–826 (2015).
Kong, A. et al. Rate of de novo mutations and the importance of father’s age to disease risk. Nature 488, 471–475 (2012).
Acuna-Hidalgo, R., Veltman, J. A. & Hoischen, A. New insights into the generation and role of de novo mutations in health and disease. Genome Biol. 17, 241 (2016).
Sharlip, I. D. et al. Best practice policies for male infertility. Fertil. Steril. 77, 873–882 (2002).
Rowe, P. J., Comhaire, F. H., Hargreave, T. B. & Mahmoud, A. M. WHO Manual for the Standardized Investigation and Diagnosis of the Infertile Male (Cambridge Univ. Press, 2000).
Cendron, M., Keating, M. A., Huff, D. S., Koop, C., Snyder, H. M. III & Duckett, J. W. Cryptorchidism, orchiopexy and infertility: a critical long-term retrospective analysis. J. Urol. 142, 559–562 (1989).
Goldstein, M. & Schlegel, P. N. (eds) Surgical and Medical Management of Male Infertility (Cambridge Univ. Press, 2013).
Kasman, A. M. et al. Association between preconception paternal health and pregnancy loss in the USA: an analysis of US claims data. Hum. Reprod. 36, 785–793 (2021).
Richmond, E. & Rogol, A. D. Traumatic brain injury: endocrine consequences in children and adults. Endocrine 45, 3–8 (2014).
Deforge, D. et al. Male erectile dysfunction following spinal cord injury: a systematic review. Spinal Cord 44, 465–473 (2006).
Ibrahim, E., Lynne, C. & Brackett, N. Male fertility following spinal cord injury: an update. Andrology 4, 13–26 (2016).
Hackett, G., Cole, N., Saghir, A., Jones, P., Strange, R. C. & Ramachandran, S. Testosterone undecanoate improves sexual function in men with type 2 diabetes and severe hypogonadism: results from a 30‐week randomized placebo‐controlled study. BJU Int. 118, 804–813 (2016).
DasGupta, R. & Fowler, C. J. Bladder, bowel and sexual dysfunction in multiple sclerosis. Drugs 63, 153–166 (2003).
Samplaski, M. K., Lo, K., Grober, E. & Jarvi, K. Finasteride use in the male infertility population: effects on semen and hormone parameters. Fertil. Steril. 100, 1542–1546 (2013).
Samplaski, M. K. & Nangia, A. K. Adverse effects of common medications on male fertility. Nat. Rev. Urol. 12, 401–413 (2015).
Amory, J. K. et al. The effect of 5alpha-reductase inhibition with dutasteride and finasteride on semen parameters and serum hormones in healthy men. J. Clin. Endocrinol. Metab. 92, 1659–1665 (2007).
Durairajanayagam, D., Agarwal, A. & Ong, C. Causes, effects and molecular mechanisms of testicular heat stress. Reprod. Biomed. Online 30, 14–27 (2015).
Holtmann, N. et al. Assessment of SARS-CoV-2 in human semen-a cohort study. Fertil. Steril. 114, 233–238 (2020).
Lundy, S. D. & Vij, S. C. Male infertility in renal failure and transplantation. Transl Androl. Urol. 8, 173 (2019).
Eckersten, D., Giwercman, A. & Christensson, A. Male patients with terminal renal failure exhibit low serum levels of antimüllerian hormone. Asian J. Androl. 17, 149 (2015).
Moody, J. A., Ahmed, K., Yap, T., Minhas, S. & Shabbir, M. Fertility managment in testicular cancer: the need to establish a standardized and evidence‐based patient‐centric pathway. BJU Int. 123, 160–172 (2019).
Michailov, Y., Lunenfeld, E., Kapelushnik, J. & Huleihel, M. Leukemia and male infertility: past, present, future. Leuk. Lymphoma 60, 1126–1135 (2019).
Costabile, R. A. The effects of cancer and cancer therapy on male reproductive function. J. Urol. 149, 1327–1330 (1993).
Wasilewski-Masker, K. et al. Male infertility in long-term survivors of pediatric cancer: a report from the childhood cancer survivor study. J. Cancer Survivorship 8, 437–447 (2014).
Harlev, A., Agarwal, A., Gunes, S. O., Shetty, A. & du Plessis, S. S. Smoking and male infertility: an evidence-based review. World J. Men’s Health 33, 143–160 (2015).
La Vignera, S., Condorelli, R. A., Balercia, G., Vicari, E. & Calogero, A. E. Does alcohol have any effect on male reproductive function? A review of literature. Asian J. Androl. 15, 221 (2013).
Greenberg, D. R. et al. ALDH2 expression, alcohol intake and semen parameters among East Asian men. J. Urol. 208, 406–413 (2022).
Jensen, T. K. et al. Habitual alcohol consumption associated with reduced semen quality and changes in reproductive hormones; a cross-sectional study among 1221 young Danish men. BMJ Open. 4, e005462 (2014).
Gundersen, T. D. et al. Association between use of marijuana and male reproductive hormones and semen quality: a study among 1,215 healthy young men. Am. J. Epidemiol. 182, 473–481 (2015).
Belladelli, F. et al. Effects of recreational cannabis on testicular function in primary infertile men. Andrology 10, 1172–1180 (2022).
Sermondade, N. et al. BMI in relation to sperm count: an updated systematic review and collaborative meta-analysis. Hum. Reprod. Update 19, 221–231 (2013).
Davidson, L. M., Millar, K., Jones, C., Fatum, M. & Coward, K. Deleterious effects of obesity upon the hormonal and molecular mechanisms controlling spermatogenesis and male fertility. Hum. Fertil. 18, 184–193 (2015).
Jóźków, P. & Rossato, M. The impact of intense exercise on semen quality. Am. J. Men’s Health 11, 654–662 (2017).
Minguez-Alarcon, L., Chavarro, J. E., Mendiola, J., Gaskins, A. J. & Torres-Cantero, A. M. Physical activity is not related to semen quality in young healthy men. Fertil. Steril. 102, 1103–1109 (2014).
Gaskins, A. J. et al. Physical activity and television watching in relation to semen quality in young men. Br. J. Sports Med. 49, 265–270 (2015).
Moxthe, L. C., Sauls, R., Ruiz, M., Stern, M., Gonzalvo, J. & Gray, H. L. Effects of bariatric surgeries on male and female fertility: a systematic review. J. Reprod. Infertil. 21, 71–86 (2020).
Andersen, E. et al. Sperm count is increased by diet-induced weight loss and maintained by exercise or GLP-1 analogue treatment: a randomized controlled trial. Hum. Reprod. 37, 1414–1422 (2022).
Sermondade, N. et al. Sperm parameters and male fertility after bariatric surgery: three case series. Reprod. Biomed. Online 24, 206–210 (2012).
Lazaros, L. et al. Dramatic reduction in sperm parameters following bariatric surgery: report of two cases. Andrologia 44, 428–432 (2012).
Carette, C. et al. Changes in total sperm count after gastric bypass and sleeve gastrectomy: the BARIASPERM prospective study. Surg. Obes. Relat. Dis. 15, 1271–1279 (2019).
Wijesekara, G. U. S., Fernando, D. M. S., Wijerathna, S. & Bandara, N. Environmental and occupational exposures as a cause of male infertility. Ceylon Med. 60, 52–56 (2015).
Guerrero-Bosagna, C. & Skinner, M. K. Environmentally induced epigenetic transgenerational inheritance of male infertility. Curr. Opin. Genet. Dev. 26, 79–88 (2014).
Rao, M. et al. Effect of transient scrotal hyperthermia on sperm parameters, seminal plasma biochemical markers, and oxidative stress in men. Asian J. Androl. 17, 668 (2015).
Sheynkin, Y., Jung, M., Yoo, P., Schulsinger, D. & Komaroff, E. Increase in scrotal temperature in laptop computer users. Hum. Reprod. 20, 452–455 (2005).
Nieschlag, E. & Vorona, E. Medical consequences of doping with anabolic androgenic steroids: effects on reproductive functions. Eur. J. Endocrinol. 173, 47 (2015).
Meriggiola, M. C., Bremner, W. J., Costantino, A., Pavani, A., Capelli, M. & Flamigni, C. An oral regimen of cyproterone acetate and testosterone undecanoate for spermatogenic suppression in men. Fertil. Steril. 68, 844–850 (1997).
Katz, N. & Mazer, N. A. The impact of opioids on the endocrine system. Clin. J. Pain 25, 170–175 (2009).
Amory, J. K. et al. The effect of 5α-reductase inhibition with dutasteride and finasteride on semen parameters and serum hormones in healthy men. J. Clin. Endocrinol. Metab. 92, 1659–1665 (2007).
Hellstrom, W. J., Giuliano, F. & Rosen, R. C. Ejaculatory dysfunction and its association with lower urinary tract symptoms of benign prostatic hyperplasia and BPH treatment. Urology 74, 15–21 (2009).
Bala, A., Nguyen, H. M. T. & Hellstrom, W. J. G. Post-SSRI sexual dysfunction: a literature review. Sex. Med. Rev. 6, 29–34 (2018).
Tanrikut, C., Feldman, A. S., Altemus, M., Paduch, D. A. & Schlegel, P. N. Adverse effect of paroxetine on sperm. Fertil. Steril. 94, 1021–1026 (2010).
O’moráin, C., Smethurst, P., Doré, C. J. & Levi, A. Reversible male infertility due to sulphasalazine: studies in man and rat. Gut 25, 1078–1084 (1984).
Gubatan, J. et al. Paternal medications in inflammatory bowel disease and male fertility and reproductive outcomes: a systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 21, 2222–2238 (2023).
Rovira, J., Diekmann, F., Ramírez-Bajo, M. J., Bañón-Maneus, E., Moya-Rull, D. & Campistol, J. M. Sirolimus-associated testicular toxicity: detrimental but reversible. Transplantation 93, 874–879 (2012).
Roa, J. et al. The mammalian target of rapamycin as novel central regulator of puberty onset via modulation of hypothalamic Kiss1 system. Endocrinology 150, 5016–5026 (2009).
Semet, M. et al. The impact of drugs on male fertility: a review. Andrology 5, 640–663 (2017).
Sansone, A., Romanelli, F., Sansone, M., Lenzi, A. & Di Luigi, L. Gynecomastia and hormones. Endocrine 55, 37–44 (2017).
Crawford, P. F. III & Crop, J. A. Evaluation of scrotal masses. Am. Fam. Physician 89, 723–727 (2014).
Charny, C. W. The spermatogenic potential of the undescended testis before and after treatment. J. Urol. 83, 697–705 (1960).
Bahk, J. Y., Jung, J. H., Jin, L. M. & Min, S. K. Cut-off value of testes volume in young adults and correlation among testes volume, body mass index, hormonal level, and seminal profiles. Urology 75, 1318–1323 (2010).
Lipshultz, L. I. & Corriere, J. N. Jr Progressive testicular atrophy in the varicocele patient. J. Urol. 117, 175–176 (1977).
Schlesinger, M. H., Wilets, I. F. & Nagler, H. M. Treatment outcome after varicocelectomy: a critical analysis. Urologic Clin. North. Am. 21, 517–529 (1994).
Chiba, K., Ramasamy, R., Lamb, D. J. & Lipshultz, L. I. The varicocele: diagnostic dilemmas, therapeutic challenges and future perspectives. Asian J. Androl. 18, 276 (2016).
Boeri, L. et al. Normal sperm parameters per se do not reliably account for fertility: A case–control study in the real‐life setting. Andrologia 53, e13861 (2021).
Keihani, S. et al. Semen parameter thresholds and time-to-conception in subfertile couples: how high is high enough?. Hum. Reprod. 36, 2121–2133 (2021).
Matin-du-Pan, R. & Bischof, P. Increased follicle stimulating hormone in infetile men: Is increased plasma FSH always due to damaged germinal epithelium? Hum. Reprod. 10, 1940–1945 (1995).
Clementini, E., Palka, C., Iezzi, I., Stuppia, L., Guanciali-Franchi, P. & Tiboni, G. Prevalence of chromosomal abnormalities in 2078 infertile couples referred for assisted reproductive techniques. Hum. Reprod. 20, 437–442 (2005).
VINCENT, M. C. et al. Cytogenetic investigations of infertile men with low sperm counts: a 25‐year experience. J. Androl. 23, 18–22 (2002).
Johnson, M. D. Genetic risks of intracytoplasmic sperm injection in the treatment of male infertility: recommendations for genetic counseling and screening. Fertil. Steril. 70, 397–411 (1998).
Colaco, S. & Modi, D. Genetics of the human Y chromosome and its association with male infertility. Reprod. Biol. Endocrinol. 16, 14 (2018).
Ferlin, A. et al. Molecular and clinical characterization of Y chromosome microdeletions in infertile men: a 10-year experience in Italy. J. Clin. Endocrinol. Metab. 92, 762–770 (2007).
De Boeck, K. Cystic fibrosis in the year 2020: a disease with a new face. Acta Paediatrica 109, 893–899 (2020).
Bieniek, J. M., Juvet, T., Margolis, M., Grober, E. D., Lo, K. C. & Jarvi, K. A. Prevalence and management of incidental small testicular masses discovered on ultrasonographic evaluation of male infertility. J. Urol. 199, 481–486 (2018).
Kolettis, P. N. & Sandlow, J. I. Clinical and genetic features of patients with congenital unilateral absence of the vas deferens. Urology 60, 1073–1076 (2002).
Donohue, R. E. & Fauver, H. E. Unilateral absence of the vas deferens. A useful clinical sign. JAMA 261, 1180–1182 (1989).
Boivin, J., Bunting, L., Collins, J. A. & Nygren, K. G. International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care. Hum. Reprod. 22, 1506–1512 (2007).
Aitken, R. J. Not every sperm is sacred; a perspective on male infertility. Mol. Hum. Reprod. 24, 287–298 (2018).
Turner, K. A. et al. Male infertility is a women’s health issue-research and clinical evaluation of male infertility is needed. Cells 9, 990 (2020).
Kolettis, P. N. & Sabanegh, E. S. Significant medical pathology discovered during a male infertility evaluation. J. Urol. 166, 178–180 (2001).
Honig, S. C., Lipshultz, L. I. & Jarow, J. Significant medical pathology uncovered by a comprehensive male infertility evaluation. Fertil. Steril. 62, 1028–1034 (1994).
Dubin, J. M., Greer, A. B., Kohn, T. P., Masterson, T. A., Ji, L. & Ramasamy, R. Men with severe oligospermia appear to benefit from varicocele repair: a cost-effectiveness analysis of assisted reproductive technology. Urology 111, 99–103 (2018).
Meng, M. V., Greene, K. L. & Turek, P. J. Surgery or assisted reproduction? A decision analysis of treatment costs in male infertility. J. Urol. 174, 1926–1931 (2005).
Schlegel, P. N. Is assisted reproduction the optimal treatment for varicocele-associated male infertility? A cost-effectiveness analysis. Urology 49, 83–90 (1997).
Stierman, B. et al. National Health and Nutrition Examination Survey 2017–March 2020 Prepandemic Data Files—Development of Files and Prevalence Estimates for Selected Health Outcomes. National Health Statistics Report No. 158 (CDC, 2021).
Craig, J. R., Jenkins, T. G., Carrell, D. T. & Hotaling, J. M. Obesity, male infertility, and the sperm epigenome. Fertil. Steril. 107, 848–859 (2017).
Eisenberg, M. L., Kim, S., Chen, Z., Sundaram, R., Schisterman, E. F., Buck & Louis, G. M. The relationship between male BMI and waist circumference on semen quality: data from the LIFE study. Hum. Reprod. 29, 193–200 (2014).
Gonzalez-Campoy, J. M. et al. Clinical practice guidelines for healthy eating for the prevention and treatment of metabolic and endocrine diseases in adults: cosponsored by the American Association of Clinical Endocrinologists/American College of Endocrinology and the Obesity Society. Endocr. Pract. 19 (Suppl. 3), 1–82 (2013).
Galdas, P. M., Cheater, F. & Marshall, P. Men and health help-seeking behaviour: literature review. J. Adv. Nurs. 49, 616–623 (2005).
Ramasamy, R., Bryson, C., Reifsnyder, J. E., Neri, Q., Palermo, G. D. & Schlegel, P. N. Overweight men with nonobstructive azoospermia have worse pregnancy outcomes after microdissection testicular sperm extraction. Fertil. Steril. 99, 372–376 (2013).
Hammoud, A. et al. Effect of Roux-en-Y gastric bypass surgery on the sex steroids and quality of life in obese men. J. Clin. Endocrinol. Metab. 94, 1329–1332 (2009).
Roth, M. Y., Amory, J. K. & Page, S. T. Treatment of male infertility secondary to morbid obesity. Nat. Clin. Pract. Endocrinol. Metab. 4, 415–419 (2008).
Moran, L. J. et al. Long-term effects of a randomised controlled trial comparing high protein or high carbohydrate weight loss diets on testosterone, SHBG, erectile and urinary function in overweight and obese men. PLoS ONE 11, e0161297 (2016).
Hayden, R. P., Flannigan, R. & Schlegel, P. N. The role of lifestyle in male infertility: diet, physical activity, and body habitus. Curr. Urol. Rep. 19, 56 (2018).
Salas-Huetos, A., Bullo, M. & Salas-Salvado, J. Dietary patterns, foods and nutrients in male fertility parameters and fecundability: a systematic review of observational studies. Hum. Reprod. Update 23, 371–389 (2017).
de Ligny, W., Smits, R. M. et al. Antioxidants for male subfertility. Cochrane Database Syst. Rev. 5, CD007411 (2022).
Creta, M. et al. Toxicity of antioxidant supplements in patients with male factor infertility: a systematic review and meta-analysis of randomized controlled trials. Antioxidants 11, 89 (2021).
Garolla, A. et al. Dietary supplements for male infertility: a critical evaluation of their composition. Nutrients 12, 1472 (2020).
Schisterman, E. F. Effect of folic acid and zinc supplementation in men on semen quality and live birth among couples undergoing infertility treatment: a randomized clinical trial. JAMA 323, 35–48 (2020).
Payne, K. S., Mazur, D. J., Hotaling, J. M. & Pastuszak, A. W. Cannabis and male fertility: a systematic review. J. Urol. 202, 674–681 (2019).
Pizzol, D. et al. Pollutants and sperm quality: a systematic review and meta-analysis. Env. Sci. Pollut. Res. Int. 28, 4095–4103 (2021).
Cannarella, R., Gül, M., Rambhatla, A. & Agarwal, A. Temporal decline of sperm concentration: role of endocrine disruptors. Endocrine 79, 1–16 (2023).
Knapke, E. T., Magalhaes, D. P., Dalvie, M. A., Mandrioli, D. & Perry, M. J. Environmental and occupational pesticide exposure and human sperm parameters: a navigation guide review. Toxicology 465, 153017 (2022).
Shefi, S., Tarapore, P. E., Walsh, T. J., Croughan, M. & Turek, P. J. Wet heat exposure: a potentially reversible cause of low semen quality in infertile men. Int. Braz. J. Urol. 33, 50–56 (2007).
Gautam, R., Priyadarshini, E., Nirala, J. & Rajamani, P. Impact of nonionizing electromagnetic radiation on male infertility: an assessment of the mechanism and consequences. Int. J. Radiat. Biol. 98, 1063–1073 (2022).
Shindel, A. W., Nelson, C. J., Naughton, C. K., Ohebshalom, M. & Mulhall, J. P. Sexual function and quality of life in the male partner of infertile couples: prevalence and correlates of dysfunction. J. Urol. 179, 1056–1059 (2008).
Lotti, F. & Maggi, M. Sexual dysfunction and male infertility. Nat. Rev. Urol. 15, 287–307 (2018).
Ding, J. et al. FDA-approved medications that impair human spermatogenesis. Oncotarget 8, 10714–10725 (2017).
Irfan, H. et al. Prolactinoma: clinical characteristics, management and outcome. Cureus 14, e29822 (2022).
Ko, E. Y., Siddiqi, K., Brannigan, R. E. & Sabanegh, E. S. Jr. Empirical medical therapy for idiopathic male infertility: a survey of the American Urological Association. J. Urol. 187, 973–978 (2012).
Thaker, H., Ko, E. Y., Sabanegh, E. S., Brannigan, R. E., Alukal, J. P. & Samplaski, M. K. Empirical medical therapy for idiopathic male infertility. FS Rep. 1, 15–20 (2020).
Keihani, S., Alder, N. J., Cheng, P. J., Stoddard, G. J., Pastuszak, A. W. & Hotaling, J. M. Obesity and baseline estradiol levels are independent predictors for initiation of anastrozole in hypogonadal men on clomiphene citrate. World J. Mens Health 38, 582–590 (2020).
Alder, N. J., Keihani, S., Stoddard, G. J., Myers, J. B. & Hotaling, J. M. Combination therapy with clomiphene citrate and anastrozole is a safe and effective alternative for hypoandrogenic subfertile men. BJU Int. 122, 688–694 (2018).
Halpern, J. A., Brannigan, R. E. & Schlegel, P. N. Fertility-enhancing male reproductive surgery: glimpses into the past and thoughts for the future. Fertil. Steril. 112, 426–437 (2019).
Chehval, M. J. & Purcell, M. H. Deterioration of semen parameters over time in men with untreated varicocele: evidence of progressive testicular damage. Fertil. Steril. 57, 174–177 (1992).
Schauer, I., Madersbacher, S., Jost, R., Hubner, W. A. & Imhof, M. The impact of varicocelectomy on sperm parameters: a meta-analysis. J. Urol. 187, 1540–1547 (2012).
Practice Committee of the American Society for Reproductive Medicine–Society for Male Reproduction and Urology. The management of obstructive azoospermia: a committee opinion. Fertil. Steril. 111, 873–880 (2019).
Esteves, S. C., Roque, M., Bradley, C. K. & Garrido, N. Reproductive outcomes of testicular versus ejaculated sperm for intracytoplasmic sperm injection among men with high levels of DNA fragmentation in semen: systematic review and meta-analysis. Fertil. Steril. 108, 456–467.e1 (2017).
Ibrahim, E., Aballa, T. C., Brackett, N. L. & Lynne, C. M. Electroejaculation in men with spinal cord injury: a step-by-step video demonstration. Fertil. Steril. 115, 1344–1346 (2021).
Di Bello, F. et al. Male sexual dysfunction and infertility in spinal cord injury patients: state-of-the-art and future perspectives. J. Pers. Med. 12, 873 (2022).
Belker, A. M., Thomas, A. J. Jr., Fuchs, E. F., Konnak, J. W. & Sharlip, I. D. Results of 1,469 microsurgical vasectomy reversals by the Vasovasostomy Study Group. J. Urol. 145, 505–511 (1991).
Marmar, J. L. Modified vasoepididymostomy with simultaneous double needle placement, tubulotomy and tubular invagination. J. Urol. 163, 483–486 (2000).
Farley, S. & Barnes, R. Stenosis of ejaculatory ducts treated by endoscopic resection. J. Urol. 109, 664–666 (1973).
Engin, G., Celtik, M., Sanli, O., Aytac, O., Muradov, Z. & Kadioglu, A. Comparison of transrectal ultrasonography and transrectal ultrasonography-guided seminal vesicle aspiration in the diagnosis of the ejaculatory duct obstruction. Fertil. Steril. 92, 964–970 (2009).
Turek, P. J., Magana, J. O. & Lipshultz, L. I. Semen parameters before and after transurethral surgery for ejaculatory duct obstruction. J. Urol. 155, 1291–1293 (1996).
Xu, B., Niu, X. & Wang, Z. et al. Novel methods for the diagnosis and treatment of ejaculatory duct obstruction. BJU Int. 108, 263–266 (2011).
Schlegel, P. N. Testicular sperm extraction: microdissection improves sperm yield with minimal tissue excision. Hum. Reprod. 14, 131–135 (1999).
Bernie, A. M., Mata, D. A., Ramasamy, R. & Schlegel, P. N. Comparison of microdissection testicular sperm extraction, conventional testicular sperm extraction, and testicular sperm aspiration for nonobstructive azoospermia: a systematic review and meta-analysis. Fertil. Steril. 104, 1099–1103.e3 (2015).
Ohlander, S., Hotaling, J., Kirshenbaum, E., Niederberger, C. & Eisenberg, M. L. Impact of fresh versus cryopreserved testicular sperm upon intracytoplasmic sperm injection pregnancy outcomes in men with azoospermia due to spermatogenic dysfunction: a meta-analysis. Fertil. Steril. 101, 344–349 (2014).
Mousavi, S. A., Masoumi, S. Z., Keramat, A., Pooralajal, J. & Shobeiri, F. Assessment of questionnaires measuring quality of life in infertile couples: a systematic review. J. Reprod. Infertil. 14, 110–119 (2013).
Duffy, J. M. N. et al. Top 10 priorities for future infertility research: an international consensus development study. Fertil. Steril. 115, 180–190 (2021).
Haraldstad, K. et al. A systematic review of quality of life research in medicine and health sciences. Qual. Life Res. 28, 2641–2650 (2019).
Koert, E., Takefman, J. & Boivin, J. Fertility quality of life tool: update on research and practice considerations. Hum. Fertil. 24, 236–248 (2021).
Pedro, J., Canavarro, M. C., Boivin, J. & Gameiro, S. Positive experiences of patient-centred care are associated with intentions to comply with fertility treatment: findings from the validation of the Portuguese version of the PCQ-Infertility tool. Hum. Reprod. 28, 2462–2472 (2013).
Peterson, B. D., Pirritano, M., Christensen, U., Boivin, J., Block, J. & Schmidt, L. The longitudinal impact of partner coping in couples following 5 years of unsuccessful fertility treatments. Hum. Reprod. 24, 1656–1664 (2009).
Sobral, M. P., Costa, M. E., Schmidt, L. & Martins, M. V. COMPI Fertility Problem Stress Scales is a brief, valid and reliable tool for assessing stress in patients seeking treatment. Hum. Reprod. 32, 375–382 (2017).
Ware, J. E. Jr. & Sherbourne, C. D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 30, 473–483 (1992).
World Health Organization. WHOQOL: measuring quality of life. WHO https://www.who.int/tools/whoqol (2012).
Boivin, J., Takefman, J. & Braverman, A. The fertility Quality of Life (FertiQoL) tool: development and general psychometric properties. Hum. Reprod. 26, 2084–2091 (2011).
Newton, C. R., Sherrard, W. & Glavac, I. The Fertility Problem Inventory: measuring perceived infertility-related stress. Fertil. Steril. 72, 54–62 (1999).
Boivin, J., Takefman, J. & Braverman, A. The Fertility Quality of Life (FertiQoL) tool: development and general psychometric properties. Fertil. Steril. 96, 409–415 e403 (2011).
Huppelschoten, A. G., van Dongen, A. J., Verhaak, C. M., Smeenk, J. M., Kremer, J. A. & Nelen, W. L. Differences in quality of life and emotional status between infertile women and their partners. Hum. Reprod. 28, 2168–2176 (2013).
Brandes, M. et al. When and why do subfertile couples discontinue their fertility care? A longitudinal cohort study in a secondary care subfertility population. Hum. Reprod. 24, 3127–3135 (2009).
Verberg, M. F. et al. Why do couples drop-out from IVF treatment? A prospective cohort study. Hum. Reprod. 23, 2050–2055 (2008).
Walschaerts, M., Bujan, L., Parinaud, J., Mieusset, R. & Thonneau, P. Treatment discontinuation in couples consulting for male infertility after failing to conceive. Fertil. Steril. 99, 1319–1323 (2013).
Chachamovich, J. R., Chachamovich, E., Ezer, H., Fleck, M. P., Knauth, D. & Passos, E. P. Investigating quality of life and health-related quality of life in infertility: a systematic review. J. Psychosom. Obstet. Gynaecol. 31, 101–110 (2010).
Shiraishi, K., Oka, S. & Matsuyama, H. Assessment of quality of life during gonadotrophin treatment for male hypogonadotrophic hypogonadism. Clin. Endocrinol. 81, 259–265 (2014).
Esteves, S. C. Evolution of the World Health Organization semen analysis manual: where are we? Nat. Rev. Urol. 19, 439–446 (2022).
Jayasena, C. N. et al. Burdens and awareness of adverse self-reported lifestyle factors in men with sub-fertility: a cross-sectional study in 1149 men. Clin. Endocrinol. 93, 312–321 (2020).
Olisa, N. P., Campo-Engelstein, L. & Martins da Silva, S. Male infertility: what on earth is going on? Pilot international questionnaire study regarding clinical evaluation and fertility treatment for men. Reprod. Fertil. 3, 207–215 (2022).
Lee, R. et al. Automated rare sperm identification from low-magnification microscopy images of dissociated microsurgical testicular sperm extraction samples using deep learning. Fertil. Steril. 118, 90–99 (2022).
Ito, Y. et al. A method for utilizing automated machine learning for histopathological classification of testis based on Johnsen scores. Sci. Rep. 11, 9962 (2021).
Ahrenfeldt, L. J. et al. Impaired fecundity as a marker of health and survival: a Danish twin cohort study. Hum. Reprod. 36, 2309–2320 (2021).
Eisenberg, M. L., Betts, P., Herder, D., Lamb, D. J. & Lipshultz, L. I. Increased cancer risk and azoospermia. Fertil. Steril. 100, e12 (2013).
Eisenberg, M. L., Betts, P., Herder, D., Lamb, D. J. & Lipshultz, L. I. Increased risk of cancer among azoospermic men. Fertil. Steril. 100, 681–685 (2013).
Eisenberg, M. L. et al. The relationship between anogenital distance and the androgen receptor CAG repeat length. Asian J. Androl. 15, 286–289 (2013).
Eisenberg, M. L. et al. Semen quality, infertility and mortality in the USA. Hum. Reprod. 29, 1567–1574 (2014).
Eisenberg, M. L., Li, S., Betts, P., Herder, D., Lamb, D. J. & Lipshultz, L. I. Testosterone therapy and cancer risk. BJU Int. 115, 317–321 (2015).
Eisenberg, M. L., Li, S., Cullen, M. R. & Baker, L. C. Increased risk of incident chronic medical conditions in infertile men: analysis of United States claims data. Fertil. Steril. 105, 629–636 (2016).
Eisenberg, M. L., Li, S., Herder, D., Lamb, D. J. & Lipshultz, L. I. Testosterone therapy and mortality risk. Int. J. Impot. Res. 27, 46–48 (2015).
Eisenberg, M. L., Murthy, L., Hwang, K., Lamb, D. J. & Lipshultz, L. I. Sperm counts and sperm sex ratio in male infertility patients. Asian J. Androl. 14, 683–686 (2012).
Hanson, B. M., Eisenberg, M. L. & Hotaling, J. M. Male infertility: a biomarker of individual and familial cancer risk. Fertil. Steril. 109, 6–19 (2018).
Kasak, L. et al. Actionable secondary findings following exome sequencing of 836 non-obstructive azoospermia cases and their value in patient management. Hum. Reprod. 37, 1652–1663 (2022).
Walsh, T. J. et al. Increased risk of high-grade prostate cancer among infertile men. Cancer 116, 2140–2147 (2010).
Hotaling, J. M. & Walsh, T. J. Male infertility: a risk factor for testicular cancer. Nat. Rev. Urol. 6, 550–556 (2009).
Ostrowski, K. A. & Walsh, T. J. Infertility with testicular cancer. Urol. Clin. North Am. 42, 409–420 (2015).
Rogers, M. J. & Walsh, T. J. Male Infertility and risk of cancer. Semin. Reprod. Med. 35, 298–303 (2017).
Walsh, T. J. Male reproductive health and prostate cancer risk. Curr. Opin. Urol. 21, 506–513 (2011).
Walsh, T. J., Croughan, M. S., Schembri, M., Chan, J. M. & Turek, P. J. Increased risk of testicular germ cell cancer among infertile men. Arch. Intern. Med. 169, 351–356 (2009).
Walsh, T. J. et al. Testosterone treatment and the risk of aggressive prostate cancer in men with low testosterone levels. PLoS ONE 13, e0199194 (2018).
Punjani, N. & Lamb, D. J. Male infertility and genitourinary birth defects: there is more than meets the eye. Fertil. Steril. 114, 209–218 (2020).
Tannour-Louet, M. et al. Identification of de novo copy number variants associated with human disorders of sexual development. PLoS ONE 5, e15392 (2010).
Tannour-Louet, M. et al. Increased gene copy number of VAMP7 disrupts human male urogenital development through altered estrogen action. Nat. Med. 20, 715–724 (2014).
Jorgez, C. J. et al. Genitourinary defects associated with genomic deletions in 2p15 encompassing OTX1. PLoS ONE 9, e107028 (2014).
Pryor, J. L. et al. Microdeletions in the Y chromosome of infertile men. N. Engl. J. Med. 336, 534–539 (1997).
Vogt, P., Chandley, A. C., Hargreave, T. B., Keil, R., Ma, K. & Sharkey, A. Microdeletions in interval 6 of the Y chromosome of males with idiopathic sterility point to disruption of AZF, a human spermatogenesis gene. Hum. Genet. 89, 491–496 (1992).
Ma, K. et al. Towards the molecular localisation of the AZF locus: mapping of microdeletions in azoospermic men within 14 subintervals of interval 6 of the human Y chromosome. Hum. Mol. Genet. 1, 29–33 (1992).
Haller, M., Au, J., O’Neill, M. & Lamb, D. J. 16p11.2 transcription factor MAZ is a dosage-sensitive regulator of genitourinary development. Proc. Natl Acad. Sci. USA 115, E1849–E1858 (2018).
Haller, M., Mo, Q., Imamoto, A. & Lamb, D. J. Murine model indicates 22q11.2 signaling adaptor CRKL is a dosage-sensitive regulator of genitourinary development. Proc. Natl Acad. Sci. USA 114, 4981–4986 (2017).
Punjani, N. & Lamb, D. J. Canary in the coal mine? Male infertility as a marker of overall health. Annu. Rev. Genet. 54, 465–486 (2020).
Punjani, N., Kang, C. & Lamb, D. J. Genetic implications of male-reproductive-health-associated comorbidities. Turk. J. Urol. 48, 363–374 (2020).
Medina-Martinez, O. et al. The transcription factor Maz is essential for normal eye development. Dis. Model. Mech. 13, dmm044412 (2020).
Guo, J. et al. The adult human testis transcriptional cell atlas. Cell Res. 28, 1141–1157 (2018).
Guo, J. et al. Chromatin and single-cell RNA-seq profiling reveal dynamic signaling and metabolic transitions during human spermatogonial stem cell development. Cell Stem Cell 21, 533–546.e6 (2017).
Blaurock, J., Baumann, S., Grunewald, S., Schiller, J. & Engel, K. M. Metabolomics of human semen: a review of different analytical methods to unravel biomarkers for male fertility disorders. Int. J. Mol. Sci. 23, 9031 (2022).
Ishikura, Y. et al. In vitro reconstitution of the whole male germ-cell development from mouse pluripotent stem cells. Cell Stem Cell 28, 2167–2179 (2021).
Brinster, R. L. Germline stem cell transplantation and transgenesis. Science 296, 2174–2176 (2002).
Sanou, I. et al. Spermatogonial stem cell-based therapies: taking preclinical research to the next level. Front. Endocrinol. 13, 850219 (2022).
Delessard, M. et al. Achievement of complete in vitro spermatogenesis in testicular tissues from prepubertal mice exposed to mono- or polychemotherapy. Sci. Rep. 12, 7407 (2022).
Skakkebaek, N. E. et al. Male reproductive disorders and fertility trends: influences of environment and genetic susceptibility. Physiol. Rev. 96, 55–97 (2016).
World Health Organization. WHO Laboratory Manual for the Examination of Human Semen and Sperm–Cervical Mucus Interaction 5th edn (Cambridge Univ. Press, 2010).
Roser, M. Fertility rate. OurWorldInData.org https://ourworldindata.org/fertility-rate (2017).
UN Department of Economic and Social Affairs, Population Division. World Population Prospects 2022. population.un.org https://population.un.org/wpp/ (2022).
GBD 2017 Population and Fertility Collaborators. Population and fertility by age and sex for 195 countries and territories, 1950-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392, 1995–2051 (2018).
GBD 2019 Demographics Collaborators. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1160–1203 (2020).
Aitken, R. J. The changing tide of human fertility. Hum. Reprod. 37, 629–638 (2022).
Levine, H. et al. Temporal trends in sperm count: a systematic review and meta-regression analysis. Hum. Reprod. Update 23, 646–659 (2017).
Skakkebæk, N. E. et al. Environmental factors in declining human fertility. Nat. Rev. Endocrinol. 18, 139–157 (2022).
Levine, H. et al. Temporal trends in sperm count: a systematic review and meta-regression analysis of samples collected globally in the 20th and 21st centuries. Hum. Reprod. Update 29, 157–176 (2023).
Cocuzza, M. & Esteves, S. C. Shedding light on the controversy surrounding the temporal decline in human sperm counts: a systematic review. ScientificWorldJournal 2014, 365691 (2014).
Priskorn, L. et al. Average sperm count remains unchanged despite reduction in maternal smoking: results from a large cross-sectional study with annual investigations over 21 years. Hum. Reprod. 33, 998–1008 (2018).
Sharma, R., Harlev, A., Agarwal, A. & Esteves, S. C. Cigarette smoking and semen quality: a new meta-analysis examining the effect of the 2010 World Health Organization Laboratory Methods for the Examination of Human Semen. Eur. Urol. 70, 635–645 (2016).
Glazer, C. H., Li, S., Zhang, C. A., Giwercman, A., Bonde, J. P. & Eisenberg, M. L. Racial and sociodemographic differences of semen parameters among US men undergoing a semen analysis. Urology 123, 126–132 (2019).
Paffoni, A., Somigliana, E., Boeri, L. & Viganò, P. The statistical foundation of the reference population for semen analysis included in the sixth edition of the WHO manual: a critical reappraisal of the evidence. Hum. Reprod. 37, 2237–2245 (2022).
Esteves, S. C. Clinical relevance of routine semen analysis and controversies surrounding the 2010 World Health Organization criteria for semen examination. Int. Braz. J. Urol. 40, 443–453 (2014).
Esteves, S. C., Zini, A., Aziz, N., Alvarez, J. G., Sabanegh, E. S. Jr & Agarwal, A. Critical appraisal of World Health Organization’s new reference values for human semen characteristics and effect on diagnosis and treatment of subfertile men. Urology 79, 16–22 (2012).
Acknowledgements
The authors thank V. Ruthig for helpful pre-review comments.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
M.L.E. is an adviser to Ro, Inc., Doveras, Next and VSeat. J.M.H. is an equity holder and co-founder of Paterna Biosciences, a consultant for Turtle Health and Carrot. K.H. is a medical director at Reprosource. D.J.L is an equity holder of Fellow Health, and serves on the Scientific Advisory Board for Ro, Inc. (stock options not executed and compensation). D.J.L. is supported in part by the Frederick J. and Theresa Dow Wallace Fund of the New York Community Trust and the Robert S. Dow Professorship in Urology. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Disease Primers thanks L. Björndahl, R. Henkel and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
GeneCards: https://www.genecards.org
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Eisenberg, M.L., Esteves, S.C., Lamb, D.J. et al. Male infertility. Nat Rev Dis Primers 9, 49 (2023). https://doi.org/10.1038/s41572-023-00459-w
Accepted:
Published:
DOI: https://doi.org/10.1038/s41572-023-00459-w
This article is cited by
-
Deleterious variant in FAM71D cause male infertility with asthenoteratospermia
Molecular Genetics and Genomics (2024)
-
The Effect of Carob (Ceratonia Siliqua) on Sperm Parameters of Infertile Men: Systematic Review and Meta-Analysis of Randomized Controlled Trials
Reproductive Sciences (2024)