Abstract
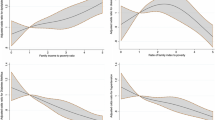
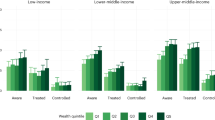
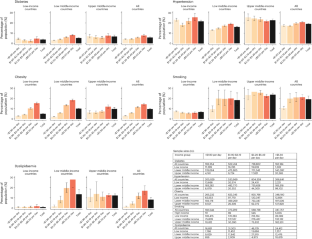
Evidence on cardiovascular disease (CVD) risk factor prevalence among adults living below the World Bank’s international line for extreme poverty (those with income <$1.90 per day) globally is sparse. Here we pooled individual-level data from 105 nationally representative household surveys across 78 countries, representing 85% of people living in extreme poverty globally, and sorted individuals by country-specific measures of household income or wealth to identify those in extreme poverty. CVD risk factors (hypertension, diabetes, smoking, obesity and dyslipidaemia) were present among 17.5% (95% confidence interval (CI) 16.7–18.3%), 4.0% (95% CI 3.6–4.5%), 10.6% (95% CI 9.0–12.3%), 3.1% (95% CI 2.8–3.3%) and 1.4% (95% CI 0.9–1.9%) of adults in extreme poverty, respectively. Most were not treated for CVD-related conditions (for example, among those with hypertension earning <$1.90 per day, 15.2% (95% CI 13.3–17.1%) reported taking blood pressure-lowering medication). The main limitation of the study is likely measurement error of poverty level and CVD risk factors that could have led to an overestimation of CVD risk factor prevalence among adults in extreme poverty. Nonetheless, our results could inform equity discussions for resource allocation and design of effective interventions.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
This study includes individual-level data from 105 surveys. Data are publicly available for 102 of these surveys. For data that are not publicly accessible and for which we have arranged specific data-use agreements, we are unable to share these data given the terms of our agreements.
Code availability
All data management and analysis code have been posted in a public repository available at https://github.com/LisaStehr/CVD-risk-factors-among-bottom-billion/tree/main. We calculated average marginal effects of Poisson regression models using R (v.4.1.3) margins package using complex survey design, with documentation available at https://cran.r-project.org/web/packages/margins/vignettes/Introduction.html.
References
Zuccala, E. & Horton, R. Reframing the NCD agenda: a matter of justice and equity. Lancet 396, 939–940 (2020).
Yach, D., Hawkes, C., Gould, C. L. & Hofman, K. J. The global burden of chronic diseases: overcoming impediments to prevention and control. J. Am. Med. Assoc. 291, 2616–2622 (2004).
Banerjee, A. V. & Duflo, E. The economic lives of the poor. J. Econ. Perspect. 21, 141–168 (2007).
Subramanian, S. & Deaton, A. The demand for food and calories. J. Political Econ. 104, 133–162 (1996).
Akhter, U. A. et al. The World’s Most Deprived: Characteristics and Causes of Extreme Poverty and Hunger (International Food Policy Research Institute, 2007).
Hickel, J. The true extent of global poverty and hunger: questioning the good news narrative of the Millennium Development Goals. Third World Q. 37, 749–767 (2016).
Svedberg, P. Poverty and Undernutrition: Theory, Measurement and Policy (Oxford Univ. Press, 2000).
Wanyama, R. N. Food security and dietary patterns among the urban poor in Africa. PhD thesis, Georg-August-University Göttingen (2019); https://doi.org/10.53846/goediss-7447
Hassen, I. W., Dereje, M., Minten, B. & Hirvonen, K. Diet Transformation in Africa: The Case of Ethiopia (International Food Policy Research Institute, 2016).
Daily meat consumption per person (Our World in Data, accessed 14 July 2022); https://ourworldindata.org/grapher/daily-meat-consumption-per-person
Share of energy from cereals, roots and tubers vs. GDP per capita (Our World in Data, accessed 14 July 2022); https://ourworldindata.org/grapher/share-of-energy-from-cereals-roots-and-tubers-vs-gdp-per-capita
Gindling, T. H. & Newhouse, D. Self-employment in the developing world. World Dev. 56, 313–331 (2014).
Collins, D., Morduch, J., Rutherford, S. & Ruthven, O. Portfolios of the Poor: How the World’s Poor Live on $2 a Day (Princeton Univ. Press, 2009); https://doi.org/10.1515/9781400829965
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J. Am. Coll. Cardiol. 76, 2982–3021 (2020).
Allen, L. et al. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: a systematic review. Lancet Glob. Health 5, e277–e289 (2017).
Williams, J. et al. A systematic review of associations between non-communicable diseases and socioeconomic status within low- and lower-middle-income countries. J. Glob. Health 8, 020409 (2018).
Rosengren, A. et al. Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income and high-income countries: the Prospective Urban Rural Epidemiologic (PURE) study. Lancet Glob. Health 7, e748–e760 (2019).
Gupta, R. et al. Socioeconomic factors and use of secondary preventive therapies for cardiovascular diseases in South Asia: the PURE study. Eur. J. Prev. Cardiol. 22, 1261–1271 (2015).
Steinert, J. I., Cluver, L. D., Melendez-Torres, G. J. & Vollmer, S. One size fits all? The validity of a composite poverty index across urban and rural households in South Africa. Soc. Indic. Res. 136, 51–72 (2018).
Poverty and Shared Prosperity 2018: Piecing Together the Poverty Puzzle (World Bank, 2018); http://elibrary.worldbank.org/doi/epdf/10.1596/978-1-4648-1330-6
Goyal, A. et al. Attained educational level and incident atherothrombotic events in low- and middle-income compared with high-income countries. Circulation 122, 1167–1175 (2010).
Yu, Z. Changes in cardiovascular risk factors in different socioeconomic groups: seven year trends in a Chinese urban population. J. Epidemiol. Community Health 54, 692–696 (2000).
Reddy, K. S. et al. Educational status and cardiovascular risk profile in Indians. Proc. Natl Acad. Sci. USA 104, 16263–16268 (2007).
Shavers, V. L. Measurement of socioeconomic status in health disparities research. J. Natl Med. Assoc. 99, 1013–1023 (2007).
Fomba, B. K., Talla, D. N. D. F. & Ningaye, P. Institutional quality and education quality in developing countries: effects and transmission channels. J. Knowl. Econ. 14, 86–115 (2022).
Altinok, N., Angrist, N. & Patrinos, H. A. Global Data Set on Education Quality (1965–2015) (World Bank, 2018); https://doi.org/10.1596/1813-9450-8314
Poverty Headcount Ratio at $1.90 a Day (2011 PPP) (% of Population) (World Bank, accessed 10 May 2022); https://data.worldbank.org/indicator/SI.POV.DDAY
Population, Total (World Bank, accessed 10 May 2022); https://data.worldbank.org/indicator/SP.POP.TOTL
Bukhman, G. et al. The Lancet NCDI Poverty Commission: bridging a gap in universal health coverage for the poorest billion. Lancet 396, 991–1044 (2020).
Member HDSSs. INDEPTH Network http://www.indepth-network.org/member-centres
Bukhman, G., Mocumbi, A. O. & Horton, R. Reframing NCDs and injuries for the poorest billion: a Lancet Commission. Lancet 386, 1221–1222 (2015).
Chomistek, A. K. et al. Healthy lifestyle in the primordial prevention of cardiovascular disease among young women. J. Am. Coll. Cardiol. 65, 43–51 (2015).
Heath, L., Jebb, S. A., Aveyard, P. & Piernas, C. Obesity, metabolic risk and adherence to healthy lifestyle behaviours: prospective cohort study in the UK Biobank. BMC Med. 20, 65 (2022).
Di Cesare, M. et al. Inequalities in non-communicable diseases and effective responses. Lancet 381, 585–597 (2013).
Kruk, M. E. et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Glob. Health 6, e1196–e1252 (2018).
Srinivas, A., Jalota, S., Mahajan, A. & Miller, G. Illness and wage loss: longitudinal evidence from India (and Implications for the Universal Health Coverage Agenda). Preprint at medRxiv https://doi.org/10.1101/2021.11.04.21265892 (2021).
Yusuf, S. et al. Cardiovascular risk and events in 17 low-, middle- and high-income countries. N. Engl. J. Med. 371, 818–827 (2014).
Dieleman, J. L. et al. Sources and focus of health development assistance, 1990–2014. J. Am. Med. Assoc. 313, 2359–2368 (2015).
Chang, A. Y. et al. Past, present and future of global health financing: a review of development assistance, government, out-of-pocket and other private spending on health for 195 countries, 1995–2050. Lancet 393, 2233–2260 (2019).
World Population Prospects 2022 (United Nations Department of Economic and Social Affairs, 2022); https://population.un.org/wpp/Download/Standard/Population/
Howe, L. D. et al. Measuring socio-economic position for epidemiological studies in low- and middle-income countries: a methods of measurement in epidemiology paper. Int. J. Epidemiol. 41, 871–886 (2012).
Alkire, S., Kanagaratnam, U., & Suppa, N. Global Multidimensional Poverty Index 2021: Unmasking Disparities by Ethnicity, Caste and Gender (OPHI & UNDP, 2021); https://ora.ox.ac.uk/objects/uuid:ce6a7338-9c0f-46e6-bbbd-2743e95563cb/files/s5q47rp795
Whelton, P. K. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation and management of high blood pressure in adults: a report of the American College of Cardiology/American heart association task force on clinical practice guidelines. Hypertension 71, 1269–1324 (2018).
American Diabetes Association. Professional Practice Committee. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2022. Diabetes Care 45, S17–S38 (2021).
World Bank Country and Lending Groups—World Bank Data Help Desk (World Bank, accessed 6 May 2022); https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
Unger, T. et al. International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 75, 1334–1357 (2020).
Sacks, D. B. et al. Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Clin. Chem. 57, e1–e47 (2011).
Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycaemia: Report of a WHO/IDF Consultation (World Health Organization & International Diabetes Federation, 2006).
Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation (WHO, 2000).
Friedewald, W. T., Levy, R. I. & Fredrickson, D. S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 18, 499–502 (1972).
National Cholesterol Education Program E. Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III)—Final Report (National Institutes of Health, 2001); https://www.nhlbi.nih.gov/files/docs/resources/heart/atp-3-cholesterol-full-report.pdf
Ahmad, O. B., Boschi-pinto, C., Lopez, A. D., Lozano, R. & Inoue, M. Age Standardization of Rates: A New WHO Standard (WHO, 2009).
WHO Package of Essential Noncommunicable (PEN) Disease Interventions for Primary Health Care (WHO, 2020); https://www.who.int/publications/i/item/9789240009226
The WHO CVD Risk Chart Working Group. World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. Lancet Glob. Health 7, e1332–e1345 (2019).
Poverty Headcount Ratio at $3.20 a day (2011 PPP) (% of population) (World Bank, accessed 19 July 2022); https://data.worldbank.org/indicator/SI.POV.LMIC
Poverty Headcount Ratio at $5.50 a day (2011 PPP) (% of population) (World Bank, accessed 19 July 2022); https://data.worldbank.org/indicator/SI.POV.UMIC
World Development Indicators. GDP per capita, PPP (constant 2011 international $) (World Bank, accessed 19 May 2022); https://data.worldbank.org/indicator/NY.GDP.PCAP.PP.KD
Poverty Gap at $1.90 a Day (2011 PPP) (%) (World Bank, accessed 18 July 2022); https://data.worldbank.org/indicator/SI.POV.GAPS
Acknowledgements
We would like to thank all participants in the household surveys that have been harmonized and analysed in this study. The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
P.G., R.L.T., R.A., T.B. and S.V. conceived this work. P.G., L.S., F.M., J.L., K.K.A., A.D., C.H., J.M.A.J., N.L., M.M., S.S.M., K.J.M., C.B., M.E.M., M.T., C.E., J.I.D., D.F., J.M.G., J.S., T.B. and S.V. were involved in data curation. P.G., L.S., F.M. and J.L. undertook formal analysis. P.G., L.S., F.M., J.L., M.E.M., T.B. and S.V. developed the methodology. P.G., L.S. and F.M. undertook visualization. P.G., R.L.T. and L.S. wrote the original draft. P.G., R.L.T., L.S., F.M., J.L., K.K.A., A.D., C.H., J.M.A.J., N.L., M.M., S.S.M., K.J.M., C.B., M.E.M., M.T., R.A., J.I.D., D.F., J.M.G., J.S., T.B. and S.V. were involved in reviewing and editing the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Human Behaviour thanks Anthony Etyang, Rajeev Gupta, Aditya Khetan, Vahé Nafilyan and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–28, Methods 1–5, Tables 1–54 and References.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Geldsetzer, P., Tisdale, R.L., Stehr, L. et al. The prevalence of cardiovascular disease risk factors among adults living in extreme poverty. Nat Hum Behav (2024). https://doi.org/10.1038/s41562-024-01840-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41562-024-01840-9