Abstract
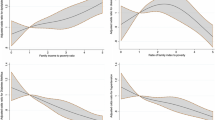
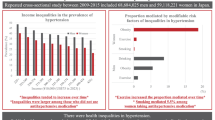
This cross-sectional study determined income disparities in age-adjusted prevalence and trends of 10-year high absolute cardiovascular disease (CVD) risk, metabolic syndrome, hypertension, diabetes, obesity, chronic kidney disease (CKD), leisure-time physical activity (LTPA), and current tobacco smoking within racial/ethnic groups in the US. National Health and Nutrition Examination Survey 2001–2016 data of 40–79-year-old people were analyzed. Survey periods were grouped as 2001–2006, 2007–2012, and 2013–2016. Race/ethnicity was grouped as non-Hispanic whites, non-Hispanic blacks, and other races/ethnicities. Three equal-sized strata (low-, middle-, and high income) were made from the family income-to-poverty ratio. Of the 25,777 participants (mean age: 55.6 years, 48% males), a majority of the studied prevalence was higher in most survey years among non-Hispanic blacks compared to non-Hispanic whites. Most studied prevalence was also higher among low-income people than middle-/high-income people. Within racial/ethnic groups, the prevalence also differed by income for high CVD risk, metabolic syndrome, hypertension, diabetes, obesity, CKD, LTPA, and tobacco smoking (P < 0.05) in most survey periods. After stratifying by race/ethnicity, the prevalence of many conditions remained disproportionately higher among low- and middle-income people, compared to those with high income during most survey periods in all racial/ethnic groups. These results reveal income in addition to race/ethnicity to be an important correlate of cardiovascular health and underscore the need to consider each when controlling for risk factors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Change history
01 April 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41371-021-00527-2
References
Heron M. National Vital Statistics Reports National Center for Health Statistics. Annual. Hyattsville, MD. 2018. https://www.cdc.gov/nchs/data/nvsr/nvsr67/nvsr67_06.pdf. Accessed 5 Dec 2018.
Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, Brauer M, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:2287–323.
GBD. DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2016;2017:1260–344.
Lottenberg SA, Glezer A, Turatti LA. Metabolic syndrome: identifying the risk factors. J de Pediatr. 2007;83:204–8.
Cassells HB, Haffner SM. The metabolic syndrome: risk factors and management. J Cardiovascular Nurs. 2006;21:306–13.
Qiao Q, Gao W, Zhang L, Nyamdorj R, Tuomilehto J. Metabolic syndrome and cardiovascular disease. Ann Clin Biochem. 2007;44:232–63.
Goff DC, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2935–59.
Ford ES. Trends in Predicted 10-year risk of coronary heart disease and cardiovascular disease among U.S. adults from 1999 to 2010. J Am Coll Cardiol. 2013;61:2249–52.
Dorans KS, Mills KT, Liu Y, He J. Trends in prevalence and control of hypertension according to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guideline. J Am Heart Assoc. 2018;7:e008888.
Pool LR, Ning H, Lloyd‐Jones DM, Allen NB. Trends in racial/ethnic disparities in cardiovascular health among US Adults from 1999–2012. J Am Heart Assoc. 2017;6. https://doi.org/10.1161/JAHA.117.006027.
Al Kibria GM. Racial/ethnic disparities in prevalence, treatment and control of hypertension among US adults following application of the 2017 American College of Cardiology/American Heart Association guideline. Prevent Med Rep. 2019;14:100850.
Aguilar M, Bhuket T, Torres S, Liu B, Wong RJ. Prevalence of the metabolic syndrome in the United States, 2003–2012. J Am Med Assoc. 2015;313:1973.
Moore JX, Chaudhary N, Akinyemiju T. Metabolic syndrome prevalence by race/ethnicity and sex in the United States, National Health and Nutrition Examination Survey, 1988–2012. Preventing Chronic Disease. 2017;14. https://doi.org/10.5888/pcd14.160287.
Odutayo A, Gill P, Shepherd S, Akingbade A, Hopewell S, Tennankore K, et al. Income disparities in absolute cardiovascular risk and cardiovascular risk factors in the United States, 1999–2014. JAMA Cardiol. 2017;2:782.
Jackson SL, Zhang Z, Wiltz JL, Loustalot F, Ritchey MD, Goodman AB, et al. Hypertension among youths—United States, 2001–2016. MMWR Morbidity Mortal Wkly Rep. 2018;67:758–62.
Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J. National health and nutrition examination survey: plan and operations, 1999–2010. Vital- Health Stat. 2013;1:1–37.
National Center for Health Statistics. National health and nutrition examination survey. 2020. https://wwwn.cdc.gov/nchs/nhanes/default.aspx. Accessed 26 Feb 2020.
Ostchega Y, Zhang G, Hughes JP, Nwankwo T. Factors associated with hypertension control in US adults using 2017 ACC/AHA guidelines: National Health and Nutrition Examination Survey 1999–2016. Am J Hypertens. 2018;31:886–94.
U.S. Department of Health & Human Services. Poverty Guidelines. 2019. https://aspe.hhs.gov/poverty-guidelines. Accessed 16 Feb 2019.
KGMM Alberti, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5.
Whelton PK, Carey RM, Aronow WS, Casey DEJ, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017:HYP.0000000000000065.
Khosla T, Lowe CR. Indices of obesity derived from body weight and height. Br J Prev Soc Med. 1967;21:122–8.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12.
U.S. Department of Health and Human Services. 2008 Physical activity guidelines for Americans. US; 2008. https://health.gov/paguidelines/pdf/paguide.pdf. Accessed 30 Jun 2018.
United States Census Bureau. Population distribution. 2019. https://www.census.gov/data/datasets/2017/demo/popest/nation-detail.html. Accessed 26 Feb 2020.
Kang H. The prevention and handling of the missing data. Korean J Anesthesiol. 2013;64:402.
Stata Corporation, College Station, Texas USA. StataCorp. 2017. 2017. https://www.stata.com/support/faqs/resources/citing-software-documentation-faqs/. Accessed 8 May 2017.
Jackson SL, Yang EC, Zhang Z. Income disparities and cardiovascular risk factors among adolescents. Pediatrics. 2018;142:e20181089 https://doi.org/10.1542/peds.2018-1089
Spatz ES, Beckman AL, Wang Y, Desai NR, Krumholz HM. Geographic variation in trends and disparities in acute myocardial infarction hospitalization and mortality by income levels, 1999–2013. JAMA Cardiol. 2016;1:255–65.
Bell CN, Thorpe RJ, Bowie JV, LaVeist TA. Race disparities in cardiovascular disease risk factors within socioeconomic status strata. Ann Epidemiol. 2018;28:147–52.
Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, et al. The association between income and life expectancy in the United States, 2001–2014. J Am Med Assoc. 2016;315:1750–66.
Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988–2012. J Am Med Assoc. 2015;314:1021.
Author information
Authors and Affiliations
Contributions
Concept and Design: GMAK. Analysis and interpretation of the data: GMAK, RC, and NR. First draft: GMAK, RC, CS, and MABC. Critical revision of the paper: RC, CS, MABC, and NR. Statistical analysis: GMAK.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Unfortunately, the spelling of the authors name Mohammad Abdul Baker Chowdhury was incorrect.
Supplementary information
Rights and permissions
About this article
Cite this article
Kibria, G.M.A., Crispen, R., Chowdhury, M.A.B. et al. Disparities in absolute cardiovascular risk, metabolic syndrome, hypertension, and other risk factors by income within racial/ethnic groups among middle-aged and older US people. J Hum Hypertens 37, 480–490 (2023). https://doi.org/10.1038/s41371-021-00513-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-021-00513-8
This article is cited by
-
The association of pre-cancer diagnosis cardiovascular risk factors with memory aging after a cancer diagnosis, overall and by race/ethnicity
Journal of Cancer Survivorship (2024)
-
Racial/Ethnic Discrimination and Cardiometabolic Diseases: A Systematic Review
Journal of Racial and Ethnic Health Disparities (2024)