Abstract
The association between PM2.5 and non-respiratory infections is unclear. Using data from Medicare beneficiaries and high-resolution datasets of PM2.5 and its constituents across 39,296 ZIP codes in the U.S between 2000 and 2016, we investigated the associations between annual PM2.5, PM2.5 constituents, source-specific PM2.5, and hospital admissions from non-respiratory infections. Each standard deviation (3.7-μg m−3) increase in PM2.5 was associated with a 10.8% (95%CI 10.8–11.2%) increase in rate of hospital admissions from non-respiratory infections. Sulfates (30.8%), Nickel (22.5%) and Copper (15.3%) contributed the largest weights in the observed associations. Each standard deviation increase in PM2.5 components sourced from oil combustion, coal burning, traffic, dirt, and regionally transported nitrates was associated with 14.5% (95%CI 7.6–21.8%), 18.2% (95%CI 7.2–30.2%), 20.6% (95%CI 5.6–37.9%), 8.9% (95%CI 0.3–18.4%) and 7.8% (95%CI 0.6–15.5%) increases in hospital admissions from non-respiratory infections. Our results suggested that non-respiratory infections are an under-appreciated health effect of PM2.5.
Similar content being viewed by others
Introduction
It is estimated that 15% of all the deaths across the world are directly attributable to infectious disease each year1. While respiratory infections draw the most attention, non-respiratory infections are also an important health burden. For example, in 2015, it was estimated that the healthcare expenditure for intestinal infections was $6.4 billion in the United States2. There were around 10.5 million office visits for urinary tract infection, causing $3.5 billion in societal costs per year3,4.
Fine particulate matter (PM2.5) is a well-recognized risk factor for health and has been found to be associated with multiple adverse health outcomes such as cardiovascular disease and respiratory disease5,6. Previous studies suggested that PM2.5 has potential immunotoxicity and could be a risk factor for infection7,8,9. Various studies have found a positive association between PM2.5 exposure and risk for respiratory infections10,11,12,13. However, only limited studies have investigated the effect of PM2.5 on non-respiratory infections and there were conflicting results14,15,16,17. Due to the lack of consistent evidence, further study is required in this field.
PM2.5 is a complex mixture of multiple constituents that come from different sources18. Different chemical constituents likely have different immunotoxic profiles which could lead to different health impacts. Identifying the constituent-specific effects could help us understand the underlying pathways by which different components and sources of PM2.5 lead to adverse health outcomes and provide information for targeted interventions.
In this study, we investigated the associations between long-term exposure to PM2.5 and hospital admissions from non-respiratory infections among older adults in the US and identified the constituents and source specific PM2.5 which contribute most to the adverse health effects.
Here, we show that ZIP codes with higher PM2.5 concentration had higher rates of hospital admissions from non-respiratory infections. Across the 15 PM2.5 constituents we examined, sulfates, Nickel and Copper contributed most to the observed association between PM2.5 and the outcome. PM2.5 sourced from oil combustion, coal burning, traffic, dirt, and regionally transported nitrates had the strongest associations with admissions from different non-respiratory infection.
Results
ZIP code-level characteristics
Hospital admissions of non-respiratory infections from 39,296 ZIP codes between 2000 and 2016 were included in the analysis. In total, 13,724,218 admissions from non-respiratory infections were identified. This study included data from 67,005,279 Medicare beneficiaries, among whom 37,037,978 (55.3%) were female, 56,700,531 (84.6%) were White, 5,788,605 (8.6%) were Black and 11,837,647 (17.6%) were ever eligible for Medicaid. Among the 436,577 included ZIP code-years, the median number of beneficiaries was 536, while the median percentage of beneficiaries younger than 75 years-old was 55.2%, the median percentage of female beneficiaries was 55.6%, median percentage of White beneficiaries was 95.9%. Other ZIP code-level characteristics controlled for in the analysis, including percentage of smokers, SES, and meteorology are summarized in Table 1.
PM2.5 and non-respiratory infection
Across all the included ZIP code-years, the median level of PM2.5 was 9.7 μg m−3 (IQR 7.7–11.8). The median admission rate of non-respiratory infections was 25.1 (IQR 16.3–35.2) per 1000 person-years. The distribution of PM2.5 levels and rate of admission from non-respiratory infections in 2008 are shown in Figs. 1 and 2. After adjusting for the covariates, each standard deviation (3.7-µg m−3) increase in PM2.5 was associated with a 10.8% (95%CI 10.8–11.2%) increase in the admission rate from non-respiratory infection. PM2.5 was also significantly associated with increased admission rates for three sub-types of non-respiratory infection. The increases in admission rate associated with each standard deviation increase in PM2.5 were 6.8% (95%CI, 6.4–7.2%), 12.0% (95%CI, 11.6–12.0%) and 12.8% (95%CI, 12.4–13.2%) for intestinal infections, urinary tract infections and septicemia respectively (Table 2). When we restricted the analysis to ZIP code-years with PM2.5 ≤ 9 µg m−3, a standard deviation increase in PM2.5 was associated with 21.5% (95%CI 20.6–22.8%) increase in rate of hospital admissions from non-respiratory infections (Table 2).
Source data are provided as a Source Data file. The figure was created from ArcMap 10.7.
The rates of hospital admissions are indicated by the Source data are provided as a Source Data file. The figure was created from ArcMap 10.7.
Mixture effect of PM2.5 constituents
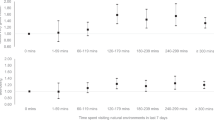
Each decile increase in the mixture was associated with a 10.3% (95%CI 10.2–10.4%) increase in admission rate of non-respiratory infection, while the constituents with the highest relative importance were SO4 (30.8%), Ni (22.5%) and Cu (15.3%) (Fig. 3). Similarly, each decile increase in the mixture was associated with 10.2% (95%CI 10.1–10.4%), 12.7% (95%CI 12.4–13.0%), and 12.0% (95%CI 11.8–12.3%) increases in admission rate for septicemia, intestinal infections and urinary tract infections, respectively. The constituents with the highest relative importance were Ni (19.7%), SO4 (17.4%) and Cu (15.6%) for septicemia; Cu (37.3%), Ni (20.0%) and SO4 (18.4%) for intestinal infections and SO4 (34.2%), Ni (14.2%), Fe (13.5%) for urinary tract infections. Each decile increase in the mixture was associated with 4.2% (95%CI 3.2–5.2%) increase in admission rate of CNS infections while the constituents with highest relative importance were Si (25.2%), OC (16.2%) and Ca (14.4%). Detailed relative importance of constituents for the four sub-types of non-respiratory infections are shown in Supplementary Fig. S1–4. All the results were adjusted for covariates mentioned above.
The dash line indicated the suggested threshold for the most influential constituents. Source data are provided as a Source Data file.
Source specific PM2.5 and non-respiratory infections
Geographical distributions for the clusters within which we conducted separate NMF are shown in Supplementary Fig. S5–7. The major sources of PM2.5 identified from our constituent data were coal burning, traffic, oil combustion, soil, biomass burning and regionally transported nitrates. Coal burning was identified in all of the nine strata while oil combustion was identified in eight strata; soil and traffic were identified in seven strata. Detailed results from NMF are shown in supplementary material (Figs. S8–S16).
After summarizing over all the strata, PM2.5 from five out of the six identified sources was significantly associated with increased admission rate from non-respiratory infections. The estimated increases in admission rate from non-respiratory infections for each one standard deviation increase in source specific PM2.5 were 14.5% (95%CI 7.6–21.8%), 18.2% (95%CI 7.2–30.2%), 20.6% (95%CI 5.6–37.9%), 8.9% (95%CI 0.3–18.4%), and 7.8% (95%CI 0.6–15.5%) for oil combustion, coal burning, traffic, soil and regionally transported nitrate respectively. PM2.5 from oil combustion and coal burning were associated with increased hospital admissions from intestinal infections, urinary tract infections and septicemia; while PM2.5 from traffic was associated with increased admission from all four subtypes of non-respiratory infections. Detailed effect estimates of each of the source-specific PM2.5 are shown in Table 3.
Discussion
In this study among older adults across the contiguous US, we observed that ZIP codes with higher PM2.5 concentrations had increased admission rates from total and different subtypes of non-respiratory infections including intestinal infections, urinary tract infections and septicemia. The associations were observed even at lower levels of PM2.5 including levels below the US EPA’s recently proposed standards, after adjusting for multiple confounders. When we examined PM2.5 constituents, SO4, Ni and Cu contributed most to the association between the constituent mixture and hospital admissions from non-respiratory infections. Based on our source apportionment analysis, PM2.5 sourced from oil combustion, coal burning and traffic had the strongest associations with admissions from different non-respiratory infections, which is generally consistent with the loadings in the mixture analyses, since Ni is a tracer for oil combustion, SO4 for coal combustion, and Cu for traffic particles.
Positive associations between PM2.5 and infections have been found in many studies, most of which focused on respiratory infections such as pneumonia and bronchiolitis6,13,19,20,21. However, associations between PM2.5 and non-respiratory infections have also been observed. A previous study among the US Medicare population found that each 1 µg m−3 increase in short-term PM2.5 was associated with 0.41%, 0.39%, 0.13% and 0.09% increases in hospital admission rates from septicemia, urinary tract infections, skin and subcutaneous tissue infections and intestinal infections20. However, that study examined short-term exposures to PM2.5 and not long-term exposures as we have done. A study from China observed that each 1 µg m−3 increase in short-term PM2.5 was associated with a 0.93% increase in rate of hospital admissions from bacterial infections of unspecified site and a 0.97% increase in the rate of hospital admissions from intestinal infections17. Our study further supports that PM2.5 is a risk factor for non-respiratory infections and is the first we know of to examine long-term exposures to particles, particle components, and particle sources. The potential pathways through which PM2.5 affects non-respiratory infections have not been thoroughly studied yet. An animal study suggested that exposure to PM2.5 down-regulated IL-1β and IFN-β, which led to increased susceptibility to viral infections22. Moreover, chronic exposure to PM2.5 could alter phagocytic activity and superoxide dismutase (SOD) activity, which affects immune response to pathogens23. The immunotoxicity potentially plays a key role in the observed association between PM2.5 and non-respiratory infections.
We observed that sulfate, Ni and Cu had the largest contribution to the effect of PM2.5 mixture on hospital admissions from non-respiratory infections. Ni is a heavy metal with high immunotoxicity. Previous studies suggested Ni exposure could increase production of reactive oxygen species, reduce the activity of SOD and catalase, and induce mitochondrial dysfunction, which are all interrelated with the function of the immune system24. Airborne Ni is predominantly from the combustion of heavy fuel oil, but other sources include metallurgy, stainless steel production and other industrial sources. An animal study found that the soluble Ni component could alter the immune defense in rats and increase their vulnerability to bacterial infections25. Similar to Ni, Cu is also a divalent cation that could affect the immune system and oxidative stress, including through Fenton chemistry. Exposure to high levels of Cu increases the production of pro-inflammatory cytokines and ROS26. An in vitro study found that copper could induce the apoptosis of monocytes. Airborne Cu is primarily a non-tailpipe traffic emission, primarily from brake wear. Other sources include industry and smelters. Sulfate particles derive primarily from coal combustion and have been observed to have the strongest association with mortality across different PM2.5 constituents in a number of studies27,28. However, evidence on the association between sulfate and infections is still lacking. A recent study observed that exposure to sulfate particles was associated with increased length of stay from hand-foot-mouth disease29. One potential mechanism for the observed effect could be that acidic sulfates turn the metal oxides from PM2.5 into metal ions which are soluble in the lung lining fluid, producing oxidative compounds and ultimately perturb the immune system30,31,32. It is plausible that sulfate interplays with metals such as nickel and copper and leads to the observed association between these PM2.5 constituents and non-respiratory infections.
PM2.5 sourced from coal burning, oil combustion, and traffic was identified in most of the strata and significantly associated with increased admission rate from total non-respiratory infections and most subtypes. These results are in accordance with our mixture analysis, given that sulfates, Nickel and Copper are the main constituents of PM2.5 sourced from coal burning, oil combustion and non-exhaust traffic. It was estimated that more than 80% of the PM2.5 in the US was from fossil fuel combustion including coal, petrol, and diesel and 0.36 million excess deaths in the country during 2012 were attributable to these sources33. Previous epidemiological studies suggested that, when compared to natural sources, PM2.5 from fossil fuel combustion has a greater adverse effect on mortality27,28,34. Thurston et al observed that coal combustion PM2.5 was associated with increased mortality from ischemic heart disease and that it showed a larger effect than overall PM2.5 in general28. Moreover, PM2.5 sourced from fossil fuel burning has also been found to be associated with multiple diseases including pneumonia, psychiatric disorders, and cancer33,35,36. Road traffic is another major contributor to the PM2.5 and has been found to be associated with many adverse health outcomes37,38,39. Traffic related PM can be categorized as exhaust and non-exhaust sources. Exhaust particles mainly come from tailpipe emissions while non-exhaust particles mainly come from the wear of tires and brakes, and also the abrasion of road surface40. A recent meta-analysis suggested that air pollution sourced from traffic emissions were associated with multiple adverse health outcomes including low birthweight, asthma onset, cardiovascular events, and mortality from multiple causes41. The results from our study provide further evidence for the harmful effect of PM2.5 sourced from fossil fuel and traffic on health, suggesting that regulations on PM2.5 could potentially focus on these sources.
The observed association between PM2.5 and its constituents and the outcomes were consistent across different subtypes of non-respiratory infections. However, the association between PM2.5 and CNS infection was much weaker when compared to other subtypes. One plausible explanation would be that the blood-brain barrier provides unique protection to the CNS and thus may be less affected by the environmental risk factors such as air pollution42. Related evidence is still sparse and, therefore, more studies are needed in order to elucidate the observed difference between CNS infections and other subtypes of non-respiratory infections.
This study has several strengths. First, this is the first study to comprehensively evaluate the impact of PM2.5 on non-respiratory infections. Second, using the data of PM2.5 constituents across the contiguous US, the study was able to identify the constituents and source-specific PM2.5 which had the strongest associations with different non-respiratory infection outcomes. These results could potentially help elucidate the potential mechanisms behind the immunotoxicity of PM2.5 and its constituents. Moreover, the results from mixture and source specific analysis are informative for targeted prevention strategies and policy making. Third, this study included more than 60 million participants, and most of the Medicare fee-for-service beneficiaries between 2000 and 2016 in the analysis, which is a representative sample of the older adults across the US, therefore, the results are likely to be generalizable to older population. The large sample size also provided enough power for us to evaluate the association between the exposures and multiple subtypes of non-respiratory infections.
The study also has limitations. First, the exposure data in this study are at ZIP code level instead of individual level. The participants’ individual exposure level within a same ZIP code could vary due to different factors. The exposure data were aggregated from grid cell level to ZIP code level. Therefore, the measurement error of the exposure could be affected by the size of ZIP code area and population, which is potentially non-differential. However, the within ZIP code coefficients of variation of the exposure data are small for the major PM2.5 components, suggesting that the potential measurement error arising from the aggregation was small. Moreover, previous studies suggested that ZIP code level air pollution is a valid proxy for individual level exposure and could avoid some of the impact of personal level confounding43. Second, the ZIP code level total PM2.5 and PM2.5 constituents in this study are not weighted by population. However, population-weighted exposure estimates could potentially lead to larger measurement error and further bias the result estimates. Third, the outcomes of this study were hospital admissions, which only captures the cases that were hospitalized or the most severe non-respiratory infection cases. It is unclear whether these results also apply to the milder cases. Further study which captures the outpatient cases are needed in the field. Fourth, this study was limited to Medicare beneficiaries who were 65 or older. Considering that older adults are more vulnerable to the adverse effect of air pollution, the results from this study might not be generalized to younger population. Moreover, since the metal components had substantial weights in contributing to the weighted quantile sum, but very small mass concentrations, the effect size estimate per weighted decile of the mixture cannot be directly compared to the effects per unit mass of PM2.5. However, these small mass components also contributed importantly to the source apportionment study, which may partially explain the larger effect size for sources, while this may also reflect the unimportance of other components of PM2.5 that were not included in our component mixture. Lastly, we are only able to obtain limited data on individual level confounders in this study. To reduce residual confounding, confounders such as smoking and SES were controlled at the contextual level.
In conclusion, higher ZIP code level PM2.5 exposure was associated with increased rate of hospital admissions from non-respiratory infections and the association remained robust even in areas with lower PM2.5, continuing below PM2.5 concentrations of 9 μg m−3. Sulfates, Nickel, and Copper play the most important role in the effect of the PM2.5 mixture on non-respiratory infections. PM2.5 sourced from fuel oil combustion, coal burning and traffic had larger effects on admission from non-respiratory infections when compared to PM2.5 from other sources. PM2.5 effects on non-respiratory infections has been understudied and this study provides evidence that this pathway could be an important additional impact from PM2.5 and should be considered in evaluating the adequacy of current PM2.5 standards.
Methods
Study population
We included all beneficiaries who enrolled in Medicare fee for service and were aged 65 and older between 2000 and 2016. Medicare is a national health insurance program in the U.S. which provides coverage mainly for those who are 65 years of age or older44. Beneficiaries entered the open cohort on January 1st 2000 or the first January 1st after their enrollment, which ever came later, and were followed until the date of death, or December 31st, 2016, whichever came earlier. This study is approved by the IRB of the Harvard T.H. Chan School of Public Health. Informed consent was waived because this study conducted secondary analysis of deidentified data.
Outcome
The outcomes of this study were hospital admissions from non-respiratory infections, and its subtypes including central nervous system (CNS) infections, intestinal infections, urinary tract infections and septicemia. Data on hospital admissions including ICD (International Classification of Diseases) Diagnosis codes at discharge and date of admissions among Medicare beneficiaries between 2000-2016 were extracted from the Medicare Provider Analysis and Review (MEDPAR) data file. Hospital admission data could include multiple diagnosis codes for each admission record. In this study, we defined the outcome as having a principal discharge diagnosis code of non-respiratory infections.
For hospital admission records with ICD-9 diagnosis codes, we applied the categorizing scheme from the Clinical Classification Software for ICD-9-CM (CCS) to categorize over 14,000 ICD-9 diagnosis codes into 280 clinically meaningful and mutually exclusive diagnosis groups45. For hospital admission records with ICD-10 diagnosis code, we applied the categorizing scheme from the Clinical Classification Software Refined for ICD-10-CM (CCSR) to categorize over 70,000 ICD-10 diagnosis codes into 530 clinically meaningful diagnosis groups46. Based on CCS and CCSR, ICD diagnosis from hospital admission records were categorized into total non-respiratory infections, CNS infections, intestinal infections, urinary tract infections and septicemia.
For admission records with ICD-9 diagnosis codes, non-respiratory infection was defined as diagnosis code being within one of group 2–9, 76–78, 90, 135, 159, 197, 201 and 248 of CCS scheme; CNS infection was defined as diagnosis code being within one of group 76–78; intestinal infection was defined as diagnosis code being within group 135; urinary tract infection was defined as diagnosis code being within group 159; septicemia was defined as diagnosis code being within group 2.
For CCSR scheme, each ICD-10 diagnosis code could exist in more than one diagnosis group. Therefore, for admission records with ICD-10 diagnosis codes, non-respiratory infection was defined as being in group INF002-004, INF006-011, MUS001-002, MUS027, NVS001-NVS003, GEN001, SKN001 and DIG001 but not in group RSP002-006. CNS infection was defined as diagnosis code being within either one of group NVS001-003; intestinal infection was defined as diagnosis code being in group DIG001; urinary tract infection was defined as diagnosis code being in group GEN001; septicemia was defined as diagnosis group being in group INF002.
The number of hospital admissions from non-respiratory infections and its subtypes were calculated for each year within each ZIP code.
Environmental exposure data
Levels of ambient PM2.5 and its constituents across the contiguous US between 2000 and 2016 were estimated from validated ensemble machine learning models developed by our grouped previously. Details of the exposure modeling are described elsewhere47,48,49. Daily PM2.5 at a 1 km*1 km grid cell level was estimated by combining predictions from random forest, gradient boosting, and neural network models in a geographically weighted regression ensemble. Predictors of the model for PM2.5 included aerosol optical depth, meteorology data, chemical transport model simulations and land-use data47. The cross-validated (CV) R2 of the annual PM2.5 prediction model was 0.89.
Annual mean levels of 15 PM2.5 constituents [elemental carbon (EC), ammonium (NH4+), nitrate (NO3-), organic carbon (OC), and sulfate (SO42-), bromine (Br), calcium (Ca), copper (Cu), iron (Fe), potassium (K), nickel (Ni), lead (Pb), silicon (Si), vanadium (V), and zinc (Zn)] were estimated at a 50 m*50 m grid cell level in urban areas and at a 1 km*1 km level in rural areas. The estimates incorporated predictions from multiple machine-learning models including random forest (RF), stochastic gradient boosting (GBM), extreme gradient boosting (XGB), cubist, and K-nearest neighbors (KNN) models. These were ensembled using a support vector machine (SVM). Like the prediction models for PM2.5, models for PM2.5 constituents included a large number of predictors which included satellite observations, meteorology data and novel land use covariates48,49. The CV R2 ranged from 0.80 to 0.96 across different constituents. The constituents predicted comprise most, but not all of the total mass of PM2.5.
Grid cell level PM2.5 and constituent concentrations were then aggregated to the ZIP code level based on previously described methods50. The coefficient of variation for each of the exposure within ZIP codes are provided in supplementary table 1.
Covariates
We obtained demographic information (age, sex, race), ZIP code of residence and Medicaid eligibility of the Medicare beneficiaries from the Medicare denominator file. Sex information in Medicare data was obtained from multiple sources including self-reported at enrollment, claims data or Electronic Health Records. Information on beneficiaries’ ZIP code, age, and Medicare eligibility were updated annually. ZIP code level socioeconomic status (SES) data including percentage of Hispanics, percentage of population that had less than high school education, median household income, percentage of population who were on public assistance and percentage of population living in poverty were directly obtained from American Community Survey 5-year estimates between 2011 and 201651 or linearly interpolated from the 2000 and 2010 US Decennial Census52. Data on the percentage of smokers within a ZIP code was obtained from Behavioral Risk Factor Surveillance System. Annual percent of Medicare enrollees having at least one ambulatory visit to a primary care clinician and distance to nearest hospital at ZIP code level were obtained or calculated from data from the Dartmouth Atlas of Healthcare website53. ZIP code-level maximal daily temperature in the summer and maximal daily temperature in the winter was calculated from the Gridded Surface Meteorological (gridMET) Dataset54. To account for potential temporal trends, we also included indicatory variables of calendar year as covariates.
Statistical analysis
Individual level data of Medicare beneficiaries were first aggregated to counts of events by ZIP code and year and merged with the ZIP code-level covariates. Within each ZIP code-year stratum, we calculated the total counts of non-respiratory infections as well as its subtypes, total number of Medicare beneficiaries, percent of female beneficiaries, percent of Black beneficiaries, and percent of beneficiaries who were also eligible for Medicaid. In our analysis, we only included ZIP codes which had more than 100 beneficiaries.
Associations between PM2.5 and the admission rates of our five outcomes, namely total non-respiratory infections, central nervous system (CNS) infections, intestinal infections, urinary tract infections, and septicemia were investigated using multivariable quasi-Poisson regression models below.
Where i indicates the ith ZIP code, j indicates the jth year, k indicates the kth outcome (total non-respiratory infection and its subtypes), Z indicates the matrix of covariates mentioned above. Admission counts indicates the number of hospital admissions for the corresponding outcome while beneficiary count indicates the number of Medicare beneficiaries aged 65 or older who were alive on January 1st of the corresponding year within the ZIP code. Quasi-Poisson regression was used because the outcome of the study was counts data and the variance of the outcome was larger than the mean of the outcome.
The US Environmental Protection Agency is considering lowering the standard of annual PM2.5 to 9–10 µg m−3. To evaluate the effect of PM2.5 at levels below the proposed standards, we conducted the same analysis restricted to ZIP code-years where PM2.5 ≤ 9 µg m−3.
Given that PM2.5 is a mixture of multiple constituents, within which correlations exist, we used weighted quantile sum regression to investigate the mixture effects of the different constituents. Weighted quantile sum regression is a modeling technique which can identify the association between mixtures and the outcome of interest while reducing the impact of high collinearity. A detailed description of the weighted quantile sum method is provided in the supplementary information. Briefly, weighted quantile sum regression estimates the relative contribution of each constituent and generates a mixture index as a linear combination of different constituents. It assumes each quantile increase in the mixture index is linearly and unidirectionally associated with the outcome55. Using weighted quantile sum regression with a quasi-Poisson link, we estimated the association between each one decile increase in the PM2.5 mixture and our five outcomes of interest while estimating the relative contribution from each of the components within the PM2.5 mixture. The weighted quantile sum regression was run with 100 bootstrap samples and all the weights were constrained to be positive.
To identify source specific effects of PM2.5, we used non-negative matrix factorization (NMF) to conduct source apportionment on our ZIP code-level PM2.5 constituent data. Similar to principal component analysis, NMF is a method for dimensionality reduction which explains the observed multidimensional data using limited number of bases56. However, NMF constrains the matrix components and the mixture coefficients to non-negative values, which is more appropriate for mass concentrations57. The regulations for the sources of air pollution varied differently over time, and hence the proportion of each component’s contribution to each source was likely to also vary over time. Therefore, we conducted source apportionment separately by time periods. To ensure enough sample size for NMF, we separated our data by three time periods (2000–2005, 2006–2010 and 2011–2016). The contribution of different sources of PM2.5 also vary across regions. Therefore, within each time period, we summarized the ZIP code mean concentration for each constituent. Using Ward’s hierarchical clustering, the contiguous US was categorized into three clusters with similar patterns of PM2.5 constituents for each of the time periods. Within each of the nine stratum (3 clusters * 3 time periods), NMF was conducted to identify 4–5 independent factors which accounted for most of variance of the PM2.5 constituent data and the source factors levels for each observation35. Based on the factor loadings of the constituents and our prior knowledge on the trace elements of PM2.5, we identified the source for each factor58 (details are provided in the supplementary information). The units of source factor levels were first converted to µg m−3 and rescaled by the standard deviation of each source factor (see supplementary methods). Within each stratum, associations between source specific factors and non-respiratory infection outcomes were estimated using quasi-Poisson regression models, and all the source factors were mutually adjusted. The total effect for each source was estimated by combining the stratum specific effects using random effect meta-analysis (flowchart is shown in Fig. 4). Details of the random effect meta-analysis are provided in the supplementary information.
All the analyses were adjusted for the confounders listed in the covariate section. To account for the autocorrelations within ZIP codes across years, we incorporated robust standard error in all of the effect estimates. Statistical analyses were conducted using R 4.1.359. The analytic code for this project is available in Supplementary Code published alongside with this manuscript.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The data of the Medicare beneficiaries are available under restricted access due to the requirements from the Center for Medicare and Medicaid Services (CMS). Researchers can submit their data request to CMS and the request will be forwarded to the CMS dissemination contractor for processing. Processing of the data takes approximately 2–4 weeks (depending on the number and years of files being requested). However, the data use agreement prevents us from sharing that data and so are not publicly available. According to the DUA, our group could only access the data on the level 3 cluster of Harvard University with controlled access and cannot download the data. The air pollution data used in this study are publicly available on the SEDAC website: https://sedac.ciesin.columbia.edu/data/set/aqdh-pm2-5-component-ec-nh4-no3-oc-so4-50m-1km-contiguous-us-2000-2019 and https://sedac.ciesin.columbia.edu/data/set/aqdh-pm2-5-component-trace-elements-50m-1km-contiguous-us-2000-2019 and https://sedac.ciesin.columbia.edu/data/set/aqdh-pm2-5-o3-no2-concentrations-zipcode-contiguous-us-2000-2016. The data from American Community Survey and US census are available at https://data.census.gov/. Data from BFRSS are available at https://www.cdc.gov/brfss/annual_data/annual_data.htm. Data from Dartmouth Healthcare Atlas are available at https://data.dartmouthatlas.org/. Source data of the figures are provided with this paper. Source data are provided with this paper.
Code availability
The analytic codes of this study are publicly available from https://github.com/yatkan/PM2.5_nonrespiratoryInfection_NC/tree/main. Code is also available in Supplementary Code published alongside this manuscript.
References
World Health Organization. Deaths by Cause, Age, Sex, by Country and by Region, 2000-2016.2018. Available from: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates.
Peery, A. F. et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the united states: update 2018. Gastroenterology 156, 254–72.e11 (2019).
Schappert, S. M. & Rechtsteiner, E. A. Ambulatory medical care utilization estimates for 2007. Vital. Health Stat. 169, 1–38 (2011).
Flores-Mireles, A. L., Walker, J. N., Caparon, M. & Hultgren, S. J. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat. Rev. Microbiol. 13, 269–284 (2015).
U.S. EPA. Integrated Science Assessment (ISA) for Particulate Matter (Final Report, Dec 2019). U.S. Environmental Protection Agency, Washington, DC; 2019.
Pun, V. C., Kazemiparkouhi, F., Manjourides, J. & Suh, H. H. Long-Term PM2.5 exposure and respiratory, cancer, and cardiovascular mortality in older US adults. Am. J. Epidemiol. 186, 961–969 (2017).
Calderon-Garciduenas, L. et al. Long-term air pollution exposure is associated with neuroinflammation, an altered innate immune response, disruption of the blood-brain barrier, ultrafine particulate deposition, and accumulation of amyloid beta-42 and alpha-synuclein in children and young adults. Toxicol. Pathol. 36, 289–310 (2008).
Dai, L. et al. Differential DNA methylation and PM2.5 species in a 450K epigenome-wide association study. Epigenetics 12, 139–148 (2017).
Fossati, S. et al. Ambient particulate air pollution and microRNAs in elderly men. Epidemiology 25, 68–78 (2014).
Liang, Y. et al. PM2.5 in Beijing - temporal pattern and its association with influenza. Environ. Health 13, 102 (2014).
Zhi, W. et al. Respiratory syncytial virus infection in children and its correlation with climatic and environmental factors. J. Int. Med. Res. 49, 3000605211044593 (2021).
Chen, M. J. et al. Machine learning to relate PM2.5 and PM10 concentrations to outpatient visits for upper respiratory tract infections in Taiwan: a nationwide analysis. World J. Clin. Cases 6, 200–206 (2018).
Chen, P. C. et al. Roles of ambient temperature and PM(2.5) on childhood acute bronchitis and bronchiolitis from viral infection. Viruses 14, 1932 (2022).
Wang, Y. et al. Sepsis-related hospital admissions and ambient air pollution: a time series analysis in 6 Chinese cities. BMC Public Health 21, 1182 (2021).
Honda, T. J., Kazemiparkouhi, F., Henry, T. D. & Suh, H. H. Long-term PM(2.5) exposure and sepsis mortality in a US medicare cohort. BMC Public Health 22, 1214 (2022).
Sarmiento, E. J. et al. Fine particulate matter pollution and risk of community-acquired sepsis. Int. J. Environ. Res. Public Health 15, 818 (2018).
Gu, J. et al. Ambient air pollution and cause-specific risk of hospital admission in China: a nationwide time-series study. PLoS Med. 17, e1003188 (2020).
Kelly, F. J. & Fussell, J. C. Size, source and chemical composition as determinants of toxicity attributable to ambient particulate matter. Atmos. Environ. 60, 504–526 (2012).
Guo, C. et al. Habitual exercise, air pollution, and pneumonia mortality: a longitudinal cohort study of approximately 0.4 million adults. Am. J. Epidemiol. 191, 1732–1741 (2022).
Wei, Y. et al. Short term exposure to fine particulate matter and hospital admission risks and costs in the Medicare population: time stratified, case crossover study. BMJ 367, l6258 (2019).
Feng, Y. et al. Ambient air pollution and posttransplant outcomes among kidney transplant recipients. Am. J. Transpl. 21, 3333–3345 (2021).
Tao, R. J. et al. PM2.5 compromises antiviral immunity in influenza infection by inhibiting activation of NLRP3 inflammasome and expression of interferon-beta. Mol. Immunol. 125, 178–186 (2020).
Lee, A., Kinney, P., Chillrud, S. & Jack, D. A systematic review of innate immunomodulatory effects of household air pollution secondary to the burning of biomass fuels. Ann. Glob. Health 81, 368–374 (2015).
Genchi, G., Carocci, A., Lauria, G., Sinicropi, M. S. & Catalano, A. Nickel: human health and environmental toxicology. Int, J. Environ. Res, Public Health 17, 679 (2020).
Roberts, J. R., Young, S. H., Castranova, V. & Antonini, J. M. The soluble nickel component of residual oil fly ash alters pulmonary host defense in rats. J. Immunotoxicol. 6, 49–61 (2009).
Figliuzzi, M. et al. Copper-dependent biological effects of particulate matter produced by brake systems on lung alveolar cells. Arch. Toxicol. 94, 2965–2979 (2020).
Crouse, D. L. et al. A new method to jointly estimate the mortality risk of long-term exposure to fine particulate matter and its components. Sci. Rep. 6, 18916 (2016).
Thurston, G. D. et al. Ischemic heart disease mortality and long-term exposure to source-related components of U.S. fine particle air pollution. Environ. Health Perspect. 124, 785–794 (2016).
Li, W. et al. Association of PM(2.5) and its components with lengths of hospital stay for hand foot and mouth disease in children. Environ. Sci. Pollut. Res. Int. 29, 50598–50607 (2022).
Meng, X. et al. A satellite-driven model to estimate long-term particulate sulfate levels and attributable mortality burden in China. Environ. Int. 171, 107740 (2023).
Brehmer, C. et al. The oxidative potential of personal and household PM2.5 in a rural setting in Southwestern China. Environ. Sci. Technol. 53, 2788–2798 (2019).
Fang, T. et al. Highly acidic ambient particles, soluble metals, and oxidative potential: a link between sulfate and aerosol toxicity. Environ. Sci. Technol. 51, 2611–2620 (2017).
Vohra, K. et al. Global mortality from outdoor fine particle pollution generated by fossil fuel combustion: results from GEOS-Chem. Environ. Res. 195, 110754 (2021).
Chen, Y. et al. The prospective effects of long-term exposure to ambient PM(2.5) and constituents on mortality in rural East China. Chemosphere 280, 130740 (2021).
Qiu, X. et al. Fine particle components and risk of psychiatric hospitalization in the U.S. Sci. Total Environ. 849, 157934 (2022).
Dherani, M. et al. Indoor air pollution from unprocessed solid fuel use and pneumonia risk in children aged under five years: a systematic review and meta-analysis. Bull. World Health Organ. 86, 390–8C (2008).
Fan, Z. T. et al. Acute exposure to elevated PM2.5 generated by traffic and cardiopulmonary health effects in healthy older adults. J. Expo. Sci. Environ. Epidemiol. 19, 525–533 (2009).
Hart, J. E. et al. Long-term ambient residential traffic-related exposures and measurement error-adjusted risk of incident lung cancer in the netherlands cohort study on diet and cancer. Environ. Health Perspect. 123, 860–866 (2015).
Heck, J. E. et al. Childhood cancer and traffic-related air pollution exposure in pregnancy and early life. Environ. Health Perspect. 121, 1385–1391 (2013).
Thorpe, A. & Harrison, R. M. Sources and properties of non-exhaust particulate matter from road traffic: a review. Sci. Total Environ. 400, 270–282 (2008).
Boogaard, H. et al. Long-term exposure to traffic-related air pollution and selected health outcomes: a systematic review and meta-analysis. Environ. Int. 164, 107262 (2022).
Mastorakos, P. & McGavern, D. The anatomy and immunology of vasculature in the central nervous system. Sci. Immunol. 4, eaav0492 (2019).
Weisskopf, M. G. & Webster, T. F. Trade-offs of personal versus more proxy exposure measures in environmental epidemiology. Epidemiology 28, 635–643 (2017).
Hoffman, E. D. Jr, Klees, B. S. & Curtis, C. A. Overview of the medicare and medicaid programs. Health Care Financ. Rev. 50, 1–378 (2002).
Healthcare Cost and Utilization Project (HCUP). HCUP CCS, March 2017. [Available from: www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp.
Healthcare Cost and Utilization Project (HCUP). Clinical Classifications Software Refined (CCSR). December 2022. [Available from: www.hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp.
Di, Q. et al. An ensemble-based model of PM(2.5) concentration across the contiguous United States with high spatiotemporal resolution. Environ. Int. 130, 104909 (2019).
Amini, H. et al. Annual Mean PM2.5 Components (EC, NH4, NO3, OC, SO4) 50m Urban and 1km Non-Urban Area Grids for Contiguous U.S., 2000-2019 v1. Palisades, New York: NASA Socioeconomic Data and Applications Center (SEDAC); 2023.
Amini, H., et al. Hyperlocal super-learned PM2.5 components across the contiguous US. 2022 [Available from: Research Square https://doi.org/10.21203/rs.3.rs-1745433/v2.
Wei, Y. et al. Causal effects of air pollution on mortality rate in Massachusetts. Am. J. Epidemiol. 189, 1316–1323 (2020).
American Community Survey (ACS) [Available from: https://www.census.gov/programs-surveys/acs.
Census Bureau Data [Available from: https://data.census.gov/.
The Dartmouth Atlas of Health Care [Available from: https://www.dartmouthatlas.org/.
Abatzoglou, J. T. Development of gridded surface meteorological data for ecological applications and modelling. Int. J. Climatol. 33:121–131 (2013).
Carrico, C., Gennings, C., Wheeler, D. C., Factor-Litvak, P. Characterization of weighted quantile sum regression for highly correlated data in a risk analysis setting. J. Agric. Biol. Environ. Stat. 20:100–120 (2015).
Wang, Y. X. & Zhang, Y. J. Nonnegative matrix factorization: a comprehensive review. IEEE Trans. Knowl. Data Eng. 25, 1336–1353 (2013).
Gaujoux, R. & Seoighe, C. A flexible R package for nonnegative matrix factorization. BMC Bioinforma. 11, 367 (2010).
Thurston, G. D., Ito, K. & Lall, R. A source apportionment of U.S. fine particulate matter air pollution. Atmos. Environ. 45, 3924–3936 (2011).
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing. (2022).
Acknowledgements
This study was funded by JS’s National Institute of Environmental Health Science (NIEHS) grant RO1 ES023418 and NIEHS P30-000002.
Author information
Authors and Affiliations
Contributions
YF contributed to conceptualization, methodology, data analysis and writing original draft. EC contributed to data compiling, methodology and manuscript editing & reviewing. YW, XQ and TJ contributed to methodology and manuscript editing & reviewing. FD contributed to manuscript editing & reviewing. JS contributed to funding, conceptualization, methodology and manuscript editing & reviewing.
Corresponding author
Ethics declarations
Competing interests
J.S. has been an expert witness for the United States Department of Justice on cases involving violations of the Clean Air Act. The other authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Amber Hackstadt and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Feng, Y., Castro, E., Wei, Y. et al. Long-term exposure to ambient PM2.5, particulate constituents and hospital admissions from non-respiratory infection. Nat Commun 15, 1518 (2024). https://doi.org/10.1038/s41467-024-45776-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-024-45776-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.