Abstract
Obstructive sleep apnea (OSA) is a serious medical condition with a high prevalence, although diagnosis remains a challenge. Existing home sleep tests may provide acceptable diagnosis performance but have shown several limitations. In this retrospective study, we used 12,923 polysomnography recordings from six independent databases to develop and evaluate a deep learning model, called OxiNet, for the estimation of the apnea-hypopnea index from the oximetry signal. We evaluated OxiNet performance across ethnicity, age, sex, and comorbidity. OxiNet missed 0.2% of all test set moderate-to-severe OSA patients against 21% for the best benchmark.
Similar content being viewed by others
Introduction
Obstructive sleep apnea (OSA) is a highly prevalent condition. Benjafield et al.1 estimated moderate-to-severe OSA affects 425 million (95% CI 399–450) adults aged 30–69 years in a review including 17 studies. OSA is characterized by recurrent episodes of upper airway partial or complete upper airway obstruction associated with recurrent oxyhemoglobin desaturations (intermittent hypoxia) and arousals (sleep fragmentation). It is caused by upper airway collapse during sleep and is characterized by frequent awakenings caused by apnea and/or hypopnea. Several studies have shown that if untreated, OSA increases the risk of cardiovascular diseases, stroke, death, cancer, and other diseases2, which all bear high clinical and economical costs. The most common presenting symptom of OSA is excessive daytime sleepiness2, leading to accidents and less effective work. Currently, full-night polysomnography (PSG), is considered the gold standard for confirming the clinical suspicion of OSA, assessing its severity, and guiding therapeutic choices. It is a multi-channel monitoring technique that analyzes the electrophysiological and cardio-respiratory patterns of sleep.
In the past year, home sleep apnea tests (HSAT) have emerged as an alternative to in-lab PSG. Although HSAT became standard practice in some countries, a recent meta-analysis of 20 papers revealed a misdiagnosis rate of 39%3 in HSAT thus highlighting a gap in the performance of these alternative cost-efficient solutions and the more expensive gold standard in-lab PSG. Several factors have motivated the development of portable diagnostic technology such as those based on single channel oximetry analysis4,5,6,7,8: the growing awareness of the high prevalence of OSA, the high proportion of undiagnosed individuals9 but also low time, cost-effectiveness and low availability of PSG and the limited performance of existing HSAT. However, most previous studies4,5 focused on developing OSA screening tests with a binary classification task (OSA, non-OSA). In some cases6,8,10, a multiclass classification task was considered to take into account all degrees of severity of OSA, but failed to estimate the apnea–hypopnea index (AHI).
In this work, we develop and evaluate the robustness of a single-channel oximetry-based OSA diagnosis algorithm based on deep learning (DL), called OxiNet, in multiple distribution shifts. OxiNet is benchmarked against two state-of-the-art classical machine learning (ML) approaches in the field of oximetry analysis for OSA diagnosis. OxiNet, significantly outperformed benchmark algorithms on all external test datasets while missing 0.2% of all test sets moderate-to-severe patients against 21% for the best benchmark. The main drops in performance on external test sets were due to a distribution shift in ethnicity for Black participants and African American participants, and comorbidity for individuals with concomitant chronic obstructive pulmonary disease.
Results
We used 12,923 PSG recordings, totaling 115,866 h of continuous data, from 6 independent databases to develop and evaluate OxiNet for the regression task of AHI estimation from the oximetry signal. The AHI was defined as the average number of all apneas and hypopneas, according to the recommended rule, per hour of sleep following the American Academy of Sleep Medicine (AASM) 2012 rules11, and ICSD-3 guidelines12. Recordings with technical faults, with \(\widehat{TST} < 4\) (i.e. less than 4 h of sleep) and patients under 18 years old were excluded. We assess OxiNet performance across ethnicity, age, sex, and comorbidity. We benchmark OxiNet against an ML model using the oxygen desaturation index (ODI) as input and an ML model using digital oximetry biomarkers (OBM) as input.
Table 1 presents the size of each dataset before and after applying the exclusion criteria. SHHS1 and SHHS2 consist of the same cohort (longitudinal study) and thus in order to avoid information leakage, the recordings of the SHHS1 training set were discarded in SHHS2 yielding 621 recordings listed under the “original number of recordings” in SHHS2.
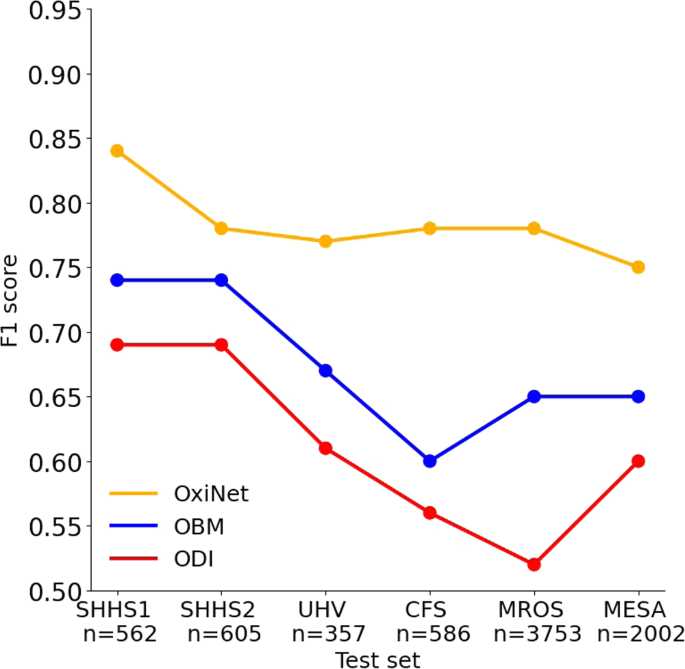
The model with the lowest loss in the validation set was saved for inference on the test sets. Table S1 presents the results of OxiNet trained on 90% of SHHS1. OxiNet achieved ICC = 0.96, F1,M = 0.84 for the SHHS1 test set and ICC = 0.95, F1,M = 0.83 for SHHS2. Performance was impaired but acceptable for UHV (ICC = 0.95, F1,M = 0.77), CFS (ICC = 0.92, F1,M = 0.78), MROS (ICC = 0.94, F1,M = 0.80) and MESA (ICC = 0.94, F1,M = 0.75). In all external databases, OxiNet performance was consistently and significantly better than the ODI and OBM benchmark models (Table S2). P-values of Wilcoxon rank-sum tests between OxiNet and OBM were below 0.05 for all databases. There was no statistical difference in performance between men and women. Table 2 presents the ICC and F1,M for all the databases and the different trained models. Figure 1 compares the estimated AHI against the actual AHI, for all the external databases.
Top (a–f): scatter plot of the computed and annotated AHI for all external databases. The dotted line represents the equation y = x. Bottom (g–l): Bland–Altman plot between the estimated and the annotated AHI. The error lines are positioned at ± 1.96 the standard deviation. From left to right: SHHS1, SHHS2, UHV, CFS, MROS, and MESA. R2 statistics are summarized in Table 2.
Discussion
Efforts focused on the analysis of respiratory pathologies based on oximetry time series have received considerable attention in the last few years13. Numerous studies have proposed oximetry biomarkers that describe patterns present in the oximetry signal, such as approximate entropy14, detrended fluctuation analysis15 or desaturations-based biomarkers16. Hang et al.4 proposed a support vector machine model which takes handcrafted features as input. They trained their model on a total of 699 patients with suspected OSA and reported a sensitivity of 0.89 for severe OSA and 0.87 for moderate-to-severe OSA. Behar et al.5 developed OxyDOSA, which is a linear regression model trained on oximetry biomarkers and three clinical features. They trained the model on a clinical PSG database of 887 individuals from a representative São Paulo (Brazil) population sample. They performed a binary classification of non-OSA versus OSA and obtained an AUROC of 0.94 ± 0.02, the sensitivity of 0.87 ± 0.04, 0.99, and 1.00 for the test set, moderate, and severe OSA respectively. Using the SHHS database, Deviaene et al.6 trained a random forest model based on 139 SpO2 features and 4 clinical features, with the aim of classifying 1-min segments as having or not a desaturation within them or not. They obtained an average sensitivity of 0.64 on the SHHS1 test set for the binary classification task and 67.0% for the multi-class classification task. When training an ensemble learning model based on features extracted from the oximetry signal, Gutierrez et al.8 achieved a kappa score between 0.45 and 0.66 when considering the four OSA severity categories, working on a database composed of 8,762 recordings. Previous studies mostly feature engineering-based models involving oximetry biomarkers and some clinical variables5,6,8,13. Mostafa et al.17 proposed a DL approach for the detection of sleep apnea using oximetry, but built their model on data from 33 patients only, achieving an accuracy of 0.97 and a sensitivity of 0.78. Despite the large number of studies focused on OSA diagnosis from oximetry data, they suffer critical limitations that have led to inconclusive beliefs regarding the viability of applying oximetry for OSA diagnosis. These limitations included the limited performance of the ML models developed, the experimental setting defining the challenge as a multi-class classification task thus preventing the assessment of such models for diagnostic purposes. In our contributions, we used a total of 12,923 PSG recordings, totaling 115,866 h of continuous data, from five independent databases to develop a robust DL model, denoted OxiNet, for the estimation of the AHI and to address research gaps in assessing the robustness of such an algorithm across ethnicity, age, sex, comorbidity, and medical guidelines. This research makes two main contributions. The first is the creation of OxiNet, a robust DL model for the estimation of the AHI from oximetry time series. The second is the performance assessment of OxiNet across different databases and distribution shifts.
The first main contribution of the research is the creation of OxiNet, a robust DL algorithm for the estimation of the AHI. OxiNet is shown to significantly outperform benchmark feature engineering based algorithms (ODI and OBM) on all test databases (Fig. 2 and Table 2). The baseline performance was determined by training a model taking the ODI as the sole oximetry feature. Indeed, ODI has been historically the most studied and used single oximetry based feature for OSA screening. The performance of the ODI based model on the SHHS1 test set was poor (ICC = 0.89, F1 = 0.69, Fig. 2) and would have led to 55 missed moderate to severe OSA diagnosis (21% of all moderate and severe). This demonstrates that using the ODI as the sole oximetry feature, i.e., only considering the average number of desaturations per hour, is not sufficient to enable robust AHI estimation and thus OSA diagnosis. When combining the set of 178 OBMs within a CatBoost model the performance increased significantly on the SHSH1 test set (ICC = 0.93, F1 = 0.74). Yet some important miss-classification errors remained with 971 missed moderate to severe OSA patients across all the databases (21% of all moderate and severe, Table 2). Our algorithm OxiNet performed significantly better on SHHS1 (ICC = 0.96, F1 = 0.84) and led to 11 missed moderate-to-severe OSA patients across all databases (0.2% of all moderate and severe). The learning curve (Fig. S1) of OxiNet performance on the SHHS1 test set demonstrated a monotonous increase as a function of the number of examples in the training set. This illustrates the importance of using a large training set (totaling thousands of recordings) in order to create a robust DL model for our task. Taken together, the results demonstrate the value of OxiNet in reaching performance that may be viable for medical diagnostic use.
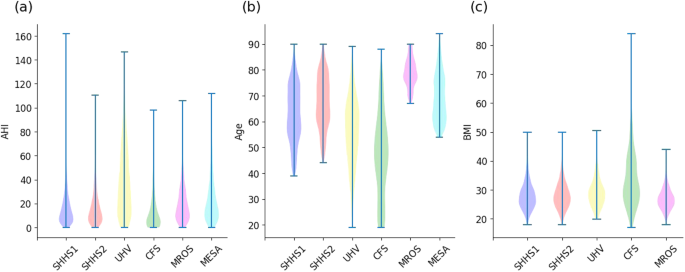
The second main contribution of the research was the assessment of the robustness of OxiNet performance by age, sex, ethnicity, and comorbidity. Our experimental results showed that the performance of OxiNet was robust in repetitive measurements (SHHS2, Table 2 and Figs. 1 and 2). Performance dropped when using the external test sets: the drop in performance was significant for a distribution shift relative to ethnicity (CFS) with F1 = 0.66 for the Black and African American participant subgroup against F1 = 0.80 for the white participant subgroup. An overall F1 score of 0.75 was obtained for the MESA database but there was a high variance across the different ethnicities with 0.72 for Hispanic participants, 0.71 for Black and African American participants, 0.78 for white participants and 0.77 for Chinese American participants (Table S3). Thus, while OxiNet performed well on white and Chinese American participants, it performed poorer on Hispanic, Black, and African American participants. These results are consistent with the melanin and typology angle levels used to characterize skin pigmentation in different ethnic groups18. It emphasizes the lack of inclusion or low prevalence of such minority groups in datasets traditionally used to train DL algorithms which inevitably leads to embedded biases and poorer diagnostic performance for these groups. Recent research19,20 has shown that pulse oximeter performance discrepancies have been shown to be affected by patients of different races and ethnicities, leading to poorer clinical management. This may explain the poorer performance of the model on Black and African American participants. The drop in performance in UHV was due to the presence of COPD comorbidity, which can lead to nocturnal desaturations13 and then mislead the model. Indeed, 58% of the misclassified patients in UHV had COPD whereas COPD had a prevalence of 20% in this database. Only two severe OSA were classified as non-OSA, in the MESA and UHV databases (0.1% of all 2017 severe cases), as shown in Fig. 3. Only 13 severe OSA cases were classified as mild OSA in the MESA and UHV databases (0.6% of all 2017 severe cases). The two misclassified severe-OSA from UHV had COPD with a global initiative for chronic obstructive lung diseases (GOLD) level three. None of the non-OSA was classified as severe, but an overall of two non OSA from MESA were classified as moderate. These two patients were Black and African American. A total of 15 patients were severe OSA and were classified as non OSA or mild OSA. For these recordings, the TST was <4 h (3.4 ± 0.4). These individuals probably had insomnia, which will affect our approximation \(\widehat{{{{{{\rm{TST}}}}}}}\) of the TST. Overall, the results illustrate that performance is impaired due to important distribution shifts. In particular, we found that distribution shifts due to ethnicity (CFS, MESA) and the presence of significant respiratory comorbidity with COPD (UHV) had an important impact on model performance.
For model explainability, Lregion was set to 120 s, which is the order of magnitude of the duration of one to a few apnea events (severe desaturations typically last 30–45 s, ref. 16). The importance score is calculated as the difference between the predicted AHI on the original signal and the predicted AHI on the signal with the corresponding window replaced by a baseline SpO2 value. In this study, the baseline SpO2 value was set to the mean value of the entire recording. Figure 4 presents examples of three different recordings. Figure 4a displays an overnight signal, where OxiNet identifies clusters of desaturations. OxiNet leverages the temporal context of desaturation events within the overnight time series. This is in opposition to a rule-based ODI detector that searches for desaturations as isolated events, i.e. independent of their temporal context. Figure 4b shows a signal segment with several apnea events. Although OxiNet assigned relatively high scores, there was no desaturation detected by the rule-based desaturation detector. This reflects that the desaturation detector is too constrained while OxiNet may learn a variety of SpO2 patterns associated with apnea and hypopnea events. Figure 4c shows a segment with no apnea or hypopnea respiratory event and, in agreement, relatively low OxiNet scores. The rule-based ODI detector, however, detected a desaturation that is not associated with a respiratory event. Overall, the explainability figures suggest that OxiNet provides added value over a simpler rule-based desaturation detector. This is because the data-driven approach enables to better learn the representation of SpO2 events during apnea and hypopnea across the high physiological variability of thousands of individuals used to train OxiNet. OxiNet also takes into account the temporal context of events while classical rule based ODI detectors look at an event in an isolated manner.
The three panels display the importance score for sections of three overnight recordings. The panels highlight the particular importance given a to desaturations clusters, b to apnea events where no desaturation was detected by the rule based desaturation detector, and c the low importance given to a section where no apnea or hypopnea event was annotated but where a desaturation was detected by the rule based desaturation detector.
This study proposed a DL algorithm for estimating the AHI from the oximetry time series and diagnose OSA. The DL OxiNet model outperformed the baseline models in all test databases (Fig. 2). Overall, this large retrospective multicenter study strongly supports the feasibility of single channel oximetry analysis for robust OSA diagnosis. The availability of a robust data driven model using input from a single pulse oximetry sensor may enable large scale diagnosis of OSA while reducing costs and waiting time. It may also enable multiple night testing and thereby even improve OSA diagnosis. Since 2017, the AASM guidelines recommend diagnosing OSA in uncomplicated patients with a single night sleep study21, which demands high test accuracy. In addition, the test must be low cost, almost fully (if not fully) automated, and, due to the shortage of hospital beds, must enable support testing in the home environment. Within this context, the high performance of OxiNet provide an exciting perspective in enabling remote diagnosis and monitoring of OSA.
The main limitation of this study is the absence of data from many underrepresented groups, ethnicity, or from developing countries. This is mainly due to the fact that despite the unprecedented initiative of sleepdata.org in open sourcing large databases of sleep data, the majority of the databases hosted on the platform are from the US. To drive health innovation that meets the needs of all and to democratize healthcare, there is a need for more databases from historically underrepresented populations. Beyond the practical and economical aspect of using home oximetry for the diagnosis of OSA, the test could also be repeated for a couple of nights. Indeed, there is evidence that there exists night to night variability of respiratory events in OSA patients22,23 and that this may lead to misdiagnosis if only a single night test is performed. Thus multiple night testing may be enabled by a home test powered by OxiNet. Some of the databases used in this study were collected at home. This includes the SHHS database. UHV, CFS, MROS and MESA were collected at the hospital. The performance was high for all databases with no particular trend observed between the oximetry data collected at home or at the hospital (see Fig. 2). For this reason, we do not expect much difference in performance given the usage of a similar clinical grade oximetry device. The same manufacturing company, Nonin, was used for the SHHS, UHV, CFS, MROS, and MESA databases, which were used to assess the performance of OxiNet according to input distribution shifts. Although Nonin has different oximeter products and versions, we believe that since most of the databases were recorded from oximeters from a single manufacturing company then this did not affect significantly the classification outcomes across our test sets. Previous research24,25 has reported variability in SpO2 measurements across different oximetry devices. Consequently, it will be valuable in future work to report on the performance of OxiNet for different oximeter manufacturers. We approximated the total sleep time (\(\widehat{{{{{{\rm{TST}}}}}}}\)) as being the time interval between sleep onset and sleep offset. In practice, this can be easily estimated using the photoplethysmography (PPG) signal recorded by the pulse oximeter. In previous research, we have demonstrated the feasibility of sleep staging from PPG, with a kappa score of 0.74 for 4-class classification (wake, light, deep, REM sleep) and an R squared of 0.92 in estimating TST26. Because the raw PPG signal was not available for most databases used in this research, we used the sleep stages provided instead in order to segment the onset and offset of the oximetry signal, as illustrated in Fig. S2. Another limitation of this work is that the datasets used for the analysis are relatively old. SHHS for instance was recorded between 1995 and 1998. Improvements have been made to oximetry technology since then. We do expect that some incremental improvement can be reached provided we had access to a dataset making use of state of the art oximeters and having a similar size to the SHHS. Indeed, although a relatively old dataset, the large size of SHHS was necessary to reach high model performance with OxiNet (Fig. S3). However, we do not expect a change in the relative performance of OxiNet versus the benchmarked models (ODI, OBM) and thus our main conclusions. In this work, we used Gaussian distributed noise for data augmentation. One avenue for further improvement of our approach would be to consider developing a simulator for the purpose of generating more biologically feasible sources of noise that are typical in oximetry measurement.
To conclude, this large, retrospective multicenter analysis provides strong support for the feasibility of single channel oximetry analysis for OSA diagnosis using OxiNet. In addition, it presented an approach to analyzing the performance of a machine learning model to specific population samples. Finally, this research provided a unique example of how large open access databases can enable the assessment of the robustness performance of ML algorithms across ethnicity, age, sex, and comorbidity to ensure the creation of robust and fair ML models.
Methods
Databases
The challenge of robustness is often raised in ML, especially for medical applications27. Indeed, there are many sources for distribution shifts, here defined as changes in the model input distribution, such as the difference across ethnicity groups. The model could learn a certain “bias” of the training set and generalize poorly on external test sets. We performed a large retrospective multicenter analysis including a total of 12,923 PSG recordings, totaling 115,866 hours of continuous data, from six independent databases. The databases include distribution shifts in age, sex, ethnicity, and comorbidity. The institutional review board from the Technion-IIT Rapport Faculty of Medicine was obtained under number 62-2019 to use the retrospective databases obtained from the open access sleepdata.org resource for this research. Table S4 provides summary statistics on demographics to describe the population samples for each of these databases.
Sleep Heart Health Study (SHHS)
SHHS28 is a multicenter cohort study conducted by the National Heart Lung & Blood Institute (ClinicalTrials.gov Identifier: NCT0000527) to determine the cardiovascular and other consequences of sleep-disordered breathing. Individuals were recruited to undergo a type II home PSG. The Nonin XPOD 3011 pulse oximeter (Nonin Medical, Inc., Plymouth, MI, USA) is used for recording. The signal is sampled at 1 Hz. In the first visit, denoted SHHS1, 6441 men and women, aged more than 40 years, are included in the database between November 1, 1995 and January 31, 1998. Recordings from 5793 subjects undergoing unattended full night PSG at baseline are available. A second visit has been performed from January 2001 to June 2003 and will be denoted as SHHS2. This second visit includes 3295 participants.
Río Hortega University Hospital of Valladolid (UHV)
UHV29 is composed of 369 oximetry recordings. The original database composed of 350 in lab PSG recordings is further described in Andres Blanco et al. and Levy et al.13,29. A total of 19 recordings were added to this research. The Nonin WristOx2 3150 was used to perform portable oximetry (simultaneously to PSG) and sampled at 1 Hz for the first 350 recordings, and 16 Hz for the additional 19. The UHV was the only database that was not part of the National Sleep Research Resource (available on sleepdata.org). However, the protocol for annotating the UHV PSG recordings also followed the AASM 2012 recommendations11, and scoring was formed by certified sleep technicians. The UHV database contains patients with suspected sleep disordered breathing and 78 patients with chronic obstructive pulmonary disease (COPD), which is a bias from the other databases. COPD is a lung pathology characterized by persistent airflow limitation that is usually progressive and an enhanced chronic inflammatory response to noxious particles or gases in the airways and the lungs30.
Cleveland Family Study (CFS)
The CFS database31 is made up of 2284 individuals from 361 families, one recording per patient. A subset of the original database, composed of 728 recordings, was available on NSRR and was used for this study. CFS is a large familial sleep apnea study designed to quantify the familial aggregation of sleep apnea. The oximetry was recorded using a Nonin 8000 sensor and sampled at 1 Hz. The database was acquired in the hospital when the patient underwent a type I PSG. Among the 728 recordings available, there are 427 (59%) Black and African American participants.
Osteoporotic Fractures in Men Study (MROS)
MROS32 is an ancillary study of the parent Osteoporotic Fractures in Men Study. Between 2000 and 2002, 5994 community dwelling men 65 years or older were enrolled in 6 clinical centers in a baseline examination. Between December 2003 and March 2005, 3135 of these participants were recruited to the sleep study when they underwent a type II home PSG and 3–5-day actigraphy studies. The objectives of the sleep study are to understand the relationship between sleep disorders and falls, fractures, mortality, and vascular disease. The oximetry signal was recorded with a Nonin 8000 sensor and sampled at of 1 Hz.
Multi Ethnic Study of Atherosclerosis (MESA)
MESA33 is a six-center collaborative longitudinal investigation of factors associated with the development of sub clinical cardiovascular disease. The study includes PSGs of 2056 individuals divided into four ethnic groups: Black and African American participants (n = 572), white participants (n = 743), Hispanic participants (n = 491), and Chinese American participants (n = 250) men and women ages 45–84 years, recorded between 2000 and 2002 with a type II home PSG. The oximetry signals were recorded using a Nonin 8000 sensor, with a sampling rate of 1 Hz.
Scoring rules
Figure 5 presents the distribution of actual AHI for each database. Table 3 summarizes the base demographic data and the AHI of each database. We ensured that the definitions of apnea and hypopnea events and thus the computation of the reference AHI were homogeneous across databases.
The databases SHHS, CFS, MROS and MESA provided by the NSSR were scored following the procedure described in Redline et al.28. Briefly, physiological recordings were originally scored in Compumedics Profusion where apnea and hypopnea respiratory events were scored according to drops in airflow that lasted more than 10 s without criteria of arousal or desaturation for hypopneas. After apneas and hypopneas were identified, the Compumedics Profusion software linked each event to data from the oxygen saturation and EEG channels. This allowed each event to be characterized according to various degrees of associated desaturation and associated arousals and/or combinations of these parameters. This top-down approach enabled the NSSR to generate AHI variables following different recommendations and rules (recommended/alternative). These AHI variables are available on the NSRR website. We used the ahi_a0h3a variable, which is consistent with AASM12 recommended rule as specified on the NSSR website and re-confirmed through private correspondence by the NSSR administrators. Data from the UHV were recorded after 2012 and followed the AASM 2012 guidelines. Annotations for all the NSRR databases (SHHS, CFS, MROS and MESA) as well as the UHV database were made by certified technicians.
Following the American Academy of Sleep Medicine (AASM) 2012 and ICSD-3 guidelines, the AHI was defined as the average number of apneas and hypopneas per hour of sleep. Apneas were scored if (i) there is a drop in the peak signal excursion by ≥90% of pre-event baseline using an oronasal thermal sensor (diagnostic study), positive airway pressure device flow (titration study), or an alternative apnea sensor; and (ii) the duration of the ≥90% drop in sensor signal is ≥10 s. In the same regard, following the recommended rule, hypopneas were defined as a ≥30% fall in an appropriate hypopnea sensor for ≥10 s and with a ≥3% desaturation or associated arousal.
Preprocessing and exclusion criteria
Recordings with technical faults (missing oximetry channel, or corrupted file) and patients under 18 years old, were excluded. Recordings from the UHV database were re-sampled at 1 Hz so that all databases had the same sampling rate. The Delta Filter34,35 was applied to the oximetry time series, to remove non physiological values due to the motion of the oximeter, or lack of proper contact between the finger and the probe. If there were fewer than three consecutive non-physiological values in the signal, a linear interpolation was performed, to fill in the missing values.
Initiating sleep may take some time and individuals with severe OSA may have numerous overnight awakenings. When computing the AHI in regular PSG examinations, the wake periods are excluded from the computation of the AHI, i.e., the cumulative number of apnea and hypopnea events is divided by the total sleep time. To partially account for this in our experiments, we have defined the sleep onset as the beginning of the first consecutive 5 min segments labeled and sleep offset as the end of the last consecutive 5 min segments labeled as sleep on the hypnogram provided for each recording. We approximated the total sleep time (\(\widehat{{{{{{\rm{TST}}}}}}}\)) as being the time interval between sleep onset and sleep offset. In practice, this can be easily estimated using the photoplethysmography (PPG) signal recorded by the pulse oximeter as we have demonstrated in our research work26.
Signals with \(\widehat{{{{{{\rm{TST}}}}}}} < 4\) (i.e., less than 4 h of sleep) were excluded28. All remaining signals were padded to 7 h. This enables us to handle signals of different lengths, from 4 to 7 h. Patients younger than 18 years were not considered in this study and were removed from the databases.
Baseline model
Two baseline classical ML models were implemented to benchmark against the DL approach. The first model included a single oximetry feature, which is the ODI with a threshold at 3%13. For the second model, SpO2 features were computed from the oximetry time series using the open source POBM toolbox35. These biomarkers are divided into five categories: (1) General Statistics: time based statistics describing the oxygen saturation data distribution. For example, Zero-Crossing36 and delta index37. (2) Complexity: quantifies the presence of long range correlations in non stationary time series. For example, Approximate Entropy38, or Detrended Fluctuation Analysis (DFA)39. (3) Periodicity: quantifies consecutive events to identify periodicity in the oxygen saturation time series. For example, Phase rectified signal averaging (PRSA)40 and power spectral density (PSD). (4) Desaturations: time based descriptive measures of the desaturation patterns occurring throughout the time series. For example, area, slope, length and depth of the desaturations. (5) Hypoxic Burden: time-based measures quantifying the overall degree of hypoxemia imposed on the heart and other organs during the recording period. For example, cumulative time under the baseline (CT)41. We have made open source on physiozoo.com the code for computing the digital oximetry features. In addition, the features are more extensively described, including their mathematical definition, in our previous work35.
A CatBoost regressor42 was trained, using a total of 178 engineered features. Further description of the features is available in the supplementary note 1. We used the maximum relevance minimum redundancy (mRMR) algorithm for feature selection. The model was optimized with fivefold cross-validation using Bayesian hyper parameter search. For both the ODI and OBM models, sex and age were added as two additional demographic features (Table S4).
OxiNet
Architecture
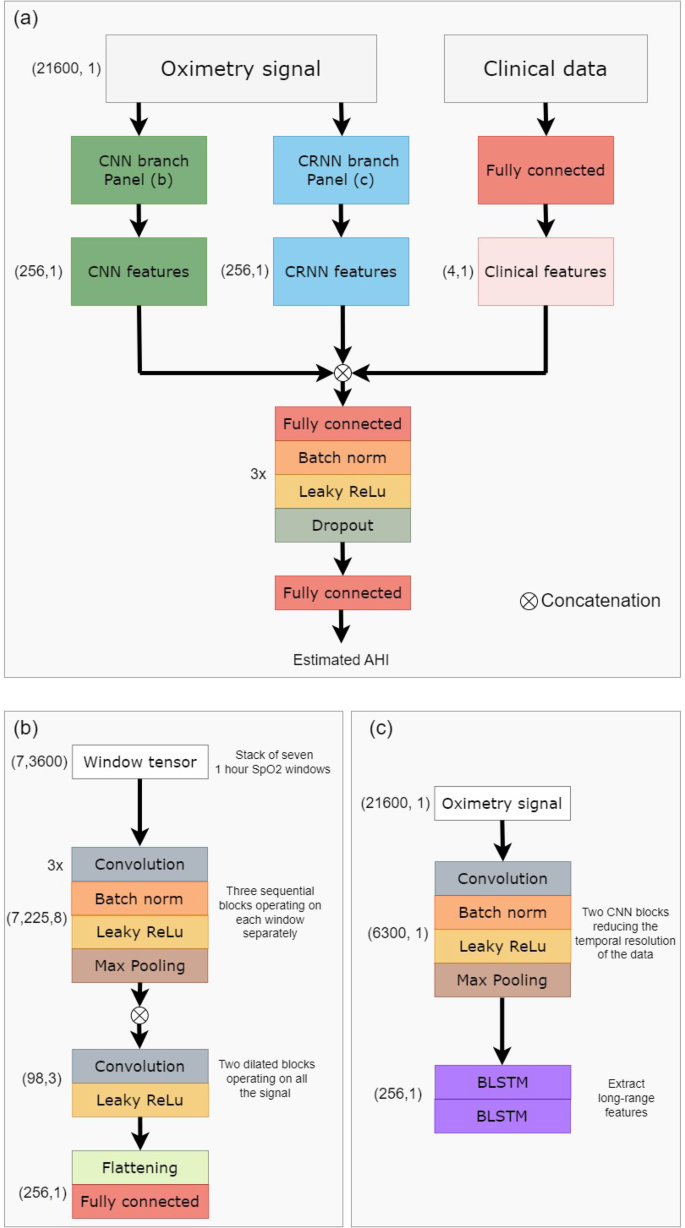
In contrast to classical ML approaches, DL techniques provide the ability to automatically learn and extract relevant features from the time series. The model takes as input the preprocessed overnight signal. Recordings with a \(\widehat{{{{{{\rm{TST}}}}}}}\) duration of over 4 h were included. Those with a \(\widehat{{{{{{\rm{TST}}}}}}}\) duration of 4–7 h were padded to 7 h. For those with a \(\widehat{{{{{{\rm{TST}}}}}}}\) duration of more than 7 h (less than 3% over all test set examples) only the first 7 h were included. The oximetry signal is independently processed by two branches as inspired by the architecture proposed by Interdonatoa et al.43. The first branch is based on convolutions, extracting useful patterns in the time series, and is called Convolutional Neural Network (CNN). The second branch, called Convolutional Recurrent Neural Network (CRNN), exploits the long range temporal correlation present in the time series.
For the CNN branch, the signals were split into overlapping windows of length Lwindow. The windows are fed to the first part of the branch, which extracts local features. This first part is composed of nB sequential blocks, which extract features from each window. One block is composed of nL 1D convolutional layers with kernel size 3, batch normalization, and Leaky ReLU activation followed by a maxpool layer of stride 2. There are skipped connections between each block. The local features of each window are then concatenated, and the second part of the model extracts long range temporal features, using dilated convolution. A total of nDB dilated blocks are sequentially used. A dilated block is made of nC 1D convolutional filters with kernel size Kdilated, followed by a Leaky ReLU activation. The dilation rate is progressively increased in order to increase the network’s field of view, beginning at ratedilation and being multiplied by 2 between each block. The CNN branch produces the feature vector \({V}_{{{{{{\rm{CNN}}}}}}}\in {{{{{{{{\mathcal{R}}}}}}}}}^{{N}_{{{{{{\rm{CNN}}}}}}}}\).
For the CRNN branch, a representation of the data is first created, to reduce the temporal resolution. This is done by using 2 CNN blocks when one block is composed of a convolutional layer with kernel size kCRNN, batch normalization, and Leaky ReLu activation followed by a maxpool layer of stride 2. Then, a total of two stacked layers of bidirectional Long Short Term Memory (LSTM) with nLSTM units is then applied. The CRNN branch produces the feature vector \({V}_{{{{{{\rm{CRNN}}}}}}}\in {{{{{{{{\mathcal{R}}}}}}}}}^{{N}_{{{{{{\rm{CRNN}}}}}}}}\).
The clinical metadata (META) is processed thanks to a fully connected layer, producing the feature vector \({V}_{{{{{{\rm{META}}}}}}}\in {{{{{{{{\mathcal{R}}}}}}}}}^{{N}_{{{{{{\rm{META}}}}}}}}\). The aggregated feature vector Vfinal = [VCNN, VCRNN, VMETA] is processed by nclassifier classifier blocks to give the final prediction. A classifier block is composed of a fully connected layer, batch normalization, Leaky Relu activation, and then dropout (with dropout rate dclassifier). Each classifier block reduces the dimensionality of the input by 2. A last fully connected layer is then applied, to output the predicted AHI.
This approach allows the model to learn complementary features and better exploit the information hidden in the time series. In order to enforce the discriminating power of the different subsets of features, we adopt the approach proposed by Hou et al.44. Two auxiliary regressors were created, working respectively on the VCNN and VCRNN vectors. These regressors were not involved in the final prediction of the model, but helped in the training process, by ensuring that each subset of the features was trained to be independently discriminative. Figure 6 presents the architecture of the resulting OxiNet model.
a Shows a high-level overview of the overall architecture. The raw data is independently processed by a CNN branch and a CRNN branch. The concatenation of CNN, CRNN, and clinical features is processed by a regressor that estimates the AHI. b Shows more in detail the CNN branch, while c presents the CRNN branch. BLSTM bidirectional long short term memory, CNN convolutional neural network, CRNN convolutional recurrent neural network.
The experiments were performed on a PowerEdge R740, 1 GPU NVIDIA Ampere A100, 40GB, 512 GB RAM. For our diagnostic objective, evenly distributed errors with low variance are preferable, as they might not change the final diagnosis of the model. For the above reason, the model was optimized using the Mean Squared Error (MSE) loss combined with L2 regularization. A total of two data augmentation techniques are used: moving window and jitter augmentation. More details about the loss and the data augmentation are available in the supplements.
Loss
For our diagnostic objective, evenly distributed errors with low variance are preferable, as they might not change the final diagnosis of the model. For the above reason, the model was optimized using the Mean Squared Error (MSE) loss combined with L2 regularization. This loss was computed three times: for the two auxiliary regressors, and for the final prediction. The final loss function used was:
When λCNN, λCRNN are two hyper parameters controlling the impact of \({{{{{{{{\mathcal{L}}}}}}}}}_{{{{{{\rm{CNN}}}}}}},{{{{{{{{\mathcal{L}}}}}}}}}_{{{{{{\rm{CRNN}}}}}}}\), respectively. At the beginning of the training process, λCRNN = λCNN = 1. Then every four epochs the two hyper parameters are multiplied by 80%, so the weight of the auxiliary classifiers in the final loss decreases. The intuition is that these regressors help the final model to converge, but are not part of it. That is why as long as the training process continues, their weight is decaying.
Data augmentation
The OxiNet model is composed of approximately 870,000 parameters, which is a few orders of magnitude larger than the number of examples contained in our training set. Data augmentation was used to increase the training set size, especially Jitter augmentation, adding white noise to the signal. The generated signal is:
where Xnew is the signal generated, X is the original signal and N is the noise added. σnoise is a hyperparameter of the model. Figure S4 presents the original and generated signals, with σnoise = 0.5. Although the generated signal may not be biologically feasible, this augmentation technique adds variance to the samples that are fed to the model and prevent overfitting the training set.
Training strategy
The SHHS1 database was split into a 90% training set and a 10% test set. All the hyperparameters of the model were optimized using Bayesian search, over 100 iterations. To this end, the SHHS1 training set was split into 70% training and 30% validation. In the first step, the model was trained on the SHHS1 train for 100 epochs. The Adam optimization algorithm was used, with a learning rate of 0.005. The set of hyperparameters leading to the smallest validation loss was retained. Then the performance measures were reported for the test set for each database, independently.
Explainability
Explainability is a critical aspect to ensure that the model is trustworthy and can be integrated into clinical practice. It enables the identification of the contributing factors and provides explanations for the predictions made by the model. Indeed, DL models are known for their black box nature, making it difficult to understand how they arrive at their predictions. To that end, we adapted the algorithm proposed by Zeiler et al.45, named Feature Occlusion (FO) and originally proposed for image recognition. The algorithm has already been used in the context of time series prediction several times46,47. The algorithm computes the importance score as the difference in output after replacing each contiguous region with a given baseline. We defined a region as a window of Lregion seconds in the oximetry signal and performed the occlusion with a sliding window of size Lregion/2, in order to have an importance score for each batch of Lregion/2 seconds. The baseline to replace with was set to be the overall mean of the signal.
Performance measures
The Kruskal–Wallis test was applied (p value cut-off of 0.05) to evaluate whether individual demographic features were discriminating between the four groups of OSA severity: non OSA (AHI < 5), mild (5 ≤ AHI < 15), moderate (15 ≤ AHI < 30) or severe (AHI ≥ 30) OSA. Table S4 presents the summary statistics for these variables and across the databases. Bland-Altman and correlation plots were generated to analyze the agreement and association between the estimated and reference AHI. The agreement was displayed as the median difference between \(\widehat{{{{{{\rm{AHI}}}}}}}\) and AHI and the 5th and 95th percentiles of their difference. For the regression task, the Intraclass Correlation Coefficient (ICC) was reported and is defined as follows:
where O is the number of observers (two, in this case, the real and predicted AHI), MSI is the instances mean square, MSE is the mean square error and MSO is the observers mean square.
After converting the AHI into the four levels of severity (i.e., non-OSA, mild, moderate, and severe OSA), the macro averaged F1 score was reported as the measure of diagnostic accuracy. The F1 score was computed as follows:
where, for a given class k, TPk is the number of true positives, TNk the number of true negatives, FPk the number of false positives, and FNk the number of false negatives. Additional performance measures are defined in the Supplementary Note.
We estimated the confidence interval for the F1 and ICC scores of the different models using bootstrapping, similar to the work of Biton et al.48. That is, the F1 and ICC scores were repeatedly computed on randomly sampled 80% of the test set (with replacement). The procedure was repeated 1000 times and used to obtain the intervals, which are defined as follows:
with \(\bar{x}\) as the bootstrap mean, z0.95 is the critical value found from the distribution table of normal CDF, and seboot is the bootstrap estimate of the standard error. Bootstrap was performed on each database separately. To determine if there was a statistical difference, the Wilcoxon rank-sum test was applied and a p value cut-off at 0.05 was used. The statistical test was also used to determine if there is a significant difference in performance measures for male vs female.
Data availability
The databases SHHS, CFS, MROS, and MESA are been achieved by the National Sleep Research Resource with appropriate deidentification. Permission and access for accessing these datasets were obtained via the online portal: https://www.sleepdata.org. In addition, the UHV database was contributed by co-author Prof. Felix Del Campo (fsas@telefonica.net) and access may be obtained on request.
Code availability
Our code and experiments can be reproduced by utilizing the details provided in the “Methods” section. For OxiNet, this includes the model architecture (section “Architecture” and Fig. 6), loss function (section “Loss”), data augmentation (section “Data augmentation”). Our trained model is also available at https://github.com/jeremy-levy/OxiNet/tree/main and is provided for academic research purpose and under a GNU GPL license. The source code used to engineer the oximetry biomarkers and train the ODI and OBM models has been made available at (https://oximetry-toolbox.readthedocs.io/en/latest/). Adam initialization was used https://www.tensorflow.org/api_docs/python/tf/keras/optimizers/Adam). For the data augmentation, we used the GaussianLayer (https://www.tensorflow.org/api_docs/python/tf/keras/layers/GaussianNoise). The code for explainability is adapted from the work of Zeiler et al.45 and is available at https://github.com/saketd403/Visualizing-and-Understanding-Convolutional-neural-networks.
References
Benjafield, A. V. et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir. Med. 7, 687–698 (2019).
Gottlieb, D. J. & Punjabi, N. M. Diagnosis and management of obstructive sleep apnea: a review. JAMA 323, 1389–1400 (2020).
Massie, F., Van Pee, B. & Bergmann, J. Correlations between home sleep apnea tests and polysomnography outcomes do not fully reflect the diagnostic accuracy of these tests. J. Clin. Sleep Med. 18, 871–876 (2022).
Hang, L.-W. et al. Validation of overnight oximetry to diagnose patients with moderate to severe obstructive sleep apnea. BMC Pulm. Med. 15, 1–13 (2015).
Behar, J. A. et al. Feasibility of single channel oximetry for mass screening of obstructive sleep apnea. EClinicalMedicine 11, 81–88 (2019).
Deviaene, M. et al. Automatic screening of sleep apnea patients based on the spo 2 signal. IEEE J. Biomed. Health Inform. 23, 607–617 (2018).
Behar, J. A. et al. Single-channel oximetry monitor versus in-lab polysomnography oximetry analysis: does it make a difference? Physiol. Meas. 41, 044007 (2020).
Gutiérrez-Tobal, G. C. et al. Ensemble-learning regression to estimate sleep apnea severity using at-home oximetry in adults. Appl. Soft Comput. 111, 107827 (2021).
Heinzer, R. et al. Prevalence of sleep-disordered breathing in the general population: the hypnolaus study. Lancet Respir. Med. 3, 310–318 (2015).
Behar, J. et al. Sleepap: an automated obstructive sleep apnoea screening application for smartphones. IEEE J. Biomed. Health Inform. 19, 325–331 (2014).
Thornton, A. T., Singh, P., Ruehland, W. R. & Rochford, P. D. Aasm criteria for scoring respiratory events: interaction between apnea sensor and hypopnea definition. Sleep 35, 425–432 (2012).
Sateia, M. J. International classification of sleep disorders. Chest 146, 1387–1394 (2014).
Levy, J., Álvarez, D., Del Campo, F. & Behar, J. A. Machine learning for nocturnal diagnosis of chronic obstructive pulmonary disease using digital oximetry biomarkers. Physiol. Meas. https://doi.org/10.1088/1361-6579/abf5ad (2021).
Pincus, S. M. Approximate entropy as a measure of system complexity. Proc. Natl Acad. Sci. USA 88, 2297–2301 (1991).
Peng, C.-K., Havlin, S., Stanley, H. E. & Goldberger, A. L. Quantification of scaling exponents and crossover phenomena in nonstationary heartbeat time series. Chaos 5, 82–87 (1995).
Kulkas, A., Duce, B., Leppänen, T., Hukins, C. & Töyräs, J. Gender differences in severity of desaturation events following hypopnea and obstructive apnea events in adults during sleep. Physiol. Meas. 38, 1490 (2017).
Mostafa, S. S., Mendonça, F., Morgado-Dias, F. & Ravelo-García, A. Spo2 based sleep apnea detection using deep learning. In 2017 IEEE 21st International Conference on Intelligent Engineering Systems (INES) 000091–000096 (IEEE, 2017).
Visscher, M. O. Skin color and pigmentation in ethnic skin. Facial Plast. Surg. Clin. 25, 119–125 (2017).
Gottlieb, E. R., Ziegler, J., Morley, K., Rush, B. & Celi, L. A. Assessment of racial and ethnic differences in oxygen supplementation among patients in the intensive care unit. JAMA Intern. Med. 182, 849–858 (2022).
Sjoding, M. W., Dickson, R. P., Iwashyna, T. J., Gay, S. E. & Valley, T. S. Racial bias in pulse oximetry measurement. N. Engl. J. Med. 383, 2477–2478 (2020).
Kapur, V. K. et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J. Clin. Sleep Med. 13, 479–504 (2017).
Meyer, T. J., Eveloff, S. E., Kline, L. R. & Millman, R. P. One negative polysomnogram does not exclude obstructive sleep apnea. Chest 103, 756–760 (1993).
Stöberl, A. S. et al. Night-to-night variability of obstructive sleep apnea. J. Sleep Res. 26, 782–788 (2017).
van Oostrom, J. H. & Melker, R. J. Comparative testing of pulse oximeter probes. Anesth. Analg. 98, 1354–1358 (2004).
Böhning, N. et al. Comparability of pulse oximeters used in sleep medicine for the screening of osa. Physiol. Meas. 31, 875 (2010).
Kotzen, K. et al. Sleepppg-net: a deep learning algorithm for robust sleep staging from continuous photoplethysmography. IEEE J. Biomed. Health Inform. 27, 924–932 (2022).
Celi, L. A. et al. Sources of bias in artificial intelligence that perpetuate healthcare disparities–a global review. PLoS Digit. Health 1, e0000022 (2022).
Redline, S. et al. Methods for obtaining and analyzing unattended polysomnography data for a multicenter study. Sleep 21, 759–767 (1998).
Andrés-Blanco, A. M. et al. Assessment of automated analysis of portable oximetry as a screening test for moderate-to-severe sleep apnea in patients with chronic obstructive pulmonary disease. PLoS ONE 12, e0188094 (2017).
Singh, D. et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD Science Committee Report 2019. Eur. Respir. J. 53, 1900164 (2019).
Redline, S. et al. The familial aggregation of obstructive sleep apnea. Am. J. Respir. Crit. Care Med. 151, 682–687 (1995).
Blackwell, T. et al. Associations between sleep architecture and sleep-disordered breathing and cognition in older community-dwelling men: the osteoporotic fractures in men sleep study. J. Am. Geriatr. Soc. 59, 2217–2225 (2011).
Chen, X. et al. Racial/ethnic differences in sleep disturbances: the multi-ethnic study of atherosclerosis (MESA). Sleep 38, 877–888 (2015).
Taha, B. et al. Automated detection and classification of sleep-disordered breathing from conventional polysomnography data. Sleep 20, 991–1001 (1997).
Levy, J. et al. Digital oximetry biomarkers for assessing respiratory function: standards of measurement, physiological interpretation, and clinical use. npj Digit. Med. 4, 1–14 (2021).
Xie, B. & Minn, H. Real-time sleep apnea detection by classifier combination. IEEE Trans. Inf. Technol. Biomed. 16, 469–477 (2012).
Pépin, J. L., Lévy, P., Lepaulle, B., Brambilla, C. & Guilleminault, C. Does oximetry contribute to the detection of apneic events?: mathematical processing of the sao2 signal. Chest 99, 1151–1157 (1991).
Pincus, S. M. Approximate entropy as a measure of system complexity. Proc. Natl Acad. Sci. USA 88, 2297–2301 (1991).
Peng, C., Havlin, S., Stanley, H. E. & Goldberger, A. L. Quantification of scaling exponents and crossover phenomena in nonstationary heartbeat time series. Chaos 5, 82–87 (1995).
Deviaene, M. et al. Automatic screening of sleep apnea patients based on the spo2 signal. IEEE J. Biomed. Health Inform. 23, 607–617 (2019).
Olson, L. G., Ambrogetti, A. & Gyulay, S. G. Prediction of sleep-disordered breathing by unattended overnight oximetry. J. Sleep Res. 8, 51–55 (1999).
Dorogush, A. V., Ershov, V. & Gulin, A. CatBoost: gradient boosting with categorical features support. Preprint at https://arxiv.org/abs/1810.11363 (2018).
Interdonato, R., Ienco, D., Gaetano, R. & Ose, K. Duplo: a dual view point deep learning architecture for time series classification. ISPRS J. Photogramm. Remote Sens. 149, 91–104 (2019).
Hou, S., Liu, X. & Wang, Z. Dualnet: Learn complementary features for image recognition. In Proc. IEEE International Conference on Computer Vision 502–510 (IEEE, 2017).
Zeiler, M. D. & Fergus, R. Visualizing and understanding convolutional networks. In Computer Vision–ECCV 2014: 13th European Conference, Zurich, Switzerland, September 6-12, 2014, Proceedings, Part I 13 818–833 (Springer, 2014).
Suresh, H. et al. Clinical intervention prediction and understanding using deep networks. Preprint at https://arxiv.org/abs/1705.08498 (2017).
Ismail, A. A., Gunady, M., Corrada Bravo, H. & Feizi, S. Benchmarking deep learning interpretability in time series predictions. Adv. Neural Inf. Process. Syst. 33, 6441–6452 (2020).
Biton, S. et al. Generalizable and robust deep learning algorithm for atrial fibrillation diagnosis across geography, ages and sexes. npj Digit. Med. 6, 44 (2023).
Acknowledgements
The Sleep Heart Health Study (SHHS) was supported by National Heart, Lung, and Blood Institute cooperative agreements U01HL53916 (University of California, Davis), U01HL53931 (New York University), U01HL53934 (University of Minnesota), U01HL53937 and U01HL64360 (Johns Hopkins University), U01HL53938 (University of Arizona), U01HL53940 (University of Washington), U01HL53941 (Boston University), and U01HL63463 (Case Western Reserve University). The National Sleep Research Resource was supported by the National Heart, Lung, and Blood Institute (R24 HL114473, 75N92019R002). The Cleveland Family Study (CFS) was supported by grants from the National Institutes of Health (HL46380, M01 RR00080-39, T32-HL07567, RO1-46380). The National Sleep Research Resource was supported by the National Heart, Lung, and Blood Institute (R24 HL114473, 75N92019R002). The National Heart, Lung, and Blood Institute provided funding for the ancillary MrOS Sleep Study, “Outcomes of Sleep Disorders in Older Men,” under the following grant numbers: R01 HL071194, R01 HL070848, R01 HL070847, R01 HL070842, R01 HL070841, R01 HL070837, R01 HL070838, and R01 HL070839. The National Sleep Research Resource was supported by the National Heart, Lung, and Blood Institute (R24 HL114473, 75N92019R002). The Multi-Ethnic Study of Atherosclerosis (MESA) Sleep Ancillary study was funded by NIH-NHLBI Association of Sleep Disorders with Cardiovascular Health Across Ethnic Groups (RO1 HL098433). MESA is supported by NHLBI funded contracts HHSN268201500003I, N01-HC-95159, N01-HC-95160, N01-HC-95161, N01-HC-95162, N01-HC-95163, N01-HC-95164, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168 and N01-HC-95169 from the National Heart, Lung, and Blood Institute, and by cooperative agreements UL1-TR-000040, UL1-TR-001079, and UL1-TR-001420 funded by NCATS. The National Sleep Research Resource was supported by the National Heart, Lung, and Blood Institute (R24 HL114473, 75N92019R002). J.A.B. and J.L. acknowledge the financial support of Israel PBC-VATAT and by the Technion Center for Machine Learning and Intelligent Systems (MLIS). D.Á. is supported by a “Ramón y Cajal” grant (RYC2019-028566-I) from the “Ministerio de Ciencia e Innovación - Agencia Estatal de Investigación” co-funded by the European Social Fund and in part by Sociedad Española de Neumología y Cirugía Torácica (SEPAR) under project 649/2018 and by Sociedad Española de Sueño (SES) under the project “Beca de Investigación SES 2019. In addition, D.Á. has been partially supported by “CIBER en Bioingeniería, Biomateriales y Nanomedicina (CIBERBBN)” through “Instituto de Salud Carlos III” co-funded with FEDER funds.
Author information
Authors and Affiliations
Contributions
J.A.B. conceived and designed the research, J.L. created OxiNet and cured and analyzed the data. D.Á. and F.C.M. provided statistical and clinical guidance on the interpretation of the results. J.A.B. and J.L. drafted the manuscript; J.L. prepared the figures; J.A.B., J.L., D.Á., and F.C.M. edited and revised the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
J.A.B. holds shares in SmartCare Analytics Ltd. The other authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Atul Malhotra, Amal Isaiah, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Levy, J., Álvarez, D., Del Campo, F. et al. Deep learning for obstructive sleep apnea diagnosis based on single channel oximetry. Nat Commun 14, 4881 (2023). https://doi.org/10.1038/s41467-023-40604-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-023-40604-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.